Introduction
Antituberculosis drug-induced liver injury (ATDILI)
is one of the most common adverse reactions to drugs used to treat
tuberculosis (TB), frequently resulting in the discontinued or
interrupted use of drugs, and thus contributing to the
socio-economic burden of the disease (1). The majority of patients with TB with
DILI develop irreversible liver failure and eventually require a
liver transplant due to a poorly defined pathogenesis and delayed
diagnosis (2). Therefore, an improved
understanding of the causes underlying hepatotoxicity induced by
anti-TB drugs may result in the identification of novel markers and
novel therapeutic targets for preventing and slowing the
progression of DILI. Although the exact aetiology of DILI is not
completely understood, it is considered a multifactorial disease
which stems from a range of risk factors, including drugs used for
treatment of TB and the dose, duration, hepatic metabolism and
lipophilicity of those drugs, and other factors including sex, age
and metabolism (2). Genetics has been
proposed as a critical contributor to the pathogenesis of DILI
(3). Thus, a focus has been placed on
the potential influence of genetic factors in the development of
ATDILI, in which a variety of genetic polymorphisms including in
N-acetyltransferase 2 (NAT2), cytochrome P450 family 2
subfamily E member 1 (CYP2E1) and glutathione S-transferases
[glutathione S-transferase mu 1 (GSTM1) and glutathione
S-transferase theta 1 (GSTT1)] have been reported to be
associated with an increased risk of ATDILI (4).
Of the various genes known to be associated with
ATDILI, GSTs are gaining increasing interest as potential
mediators of hepatotoxicity. GSTs are essential phase II
metabolizing enzymes for detoxification, which are responsible for
mitigating the cellular damage resulting from oxidative stress via
conjugating glutathione to substrates including reactive oxygen
species (ROS) in response to liver injury, and have been implicated
in hepatotoxicity (5). Thus, they
exert a protective effect against cellular damage, and one study
revealed that gene deletions caused by the homozygous null
mutations of GSTM1 and GSTT1, which are two major
GSTs involved in the isoniazid metabolism pathway, were
significantly associated with an elevated risk of DILI in patients
with TB (6). A number of clinical
studies have demonstrated a potential significant association
between GSTM1 or GSTT1 and susceptibility to ATDILI
and DILI (7-21);
however, the results obtained from these studies are inconsistent.
For example, Rana et al (14)
revealed that GSTM1 was associated with an increased risk of
ATDILI; however, in a study by Chatterjee et al (7), an association was not observed. A
meta-analysis is a valuable tool for deriving meaningful
conclusions from data and may help resolve inconsistencies in
research, and may thus assist in clarifying the association between
polymorphisms of GSTM1 or GSTT1 and ATDILI.
Numerous meta-analyses have revealed an association
between GSTM1 and GSTT1 null genotypes and
susceptibility to ATDILI (6,22-24);
nevertheless, there remain important gaps in our knowledge.
Firstly, previous meta-analyses have included publications with
confounding factors, including patients with hepatitis virus
infection or human immunodeficiency virus (HIV) (23,25).
Furthermore, since a large number of studies have been published,
it is necessary to perform an updated meta-analysis to assess the
association of genetic polymorphisms with ATDILI. Additionally,
although genetic data derived from numerous meta-analyses are based
on a large multi-ethnic population, the association between
polymorphisms and individuals of South Asian descent require
further validation. To address the aforementioned limitations of
previous meta-analyses, the present meta-analysis was designed with
a more stringent selection criteria to verify the precise
associations between GSTM1 and GSTT1 with
susceptibility to ATDILI. Therefore, the aim of the present
analysis was to summarize and analyse the body of available data
regarding the pharmacogenomics associated with ATDILI using a
systematic review and meta-analysis approach, along with network
analysis in order to gain insight into the molecular interactions
between these pharmacogenes, their genetic polymorphisms and
association with a susceptibility to ATDILI based on genetics and
ethnicity.
Materials and methods
Identification of genes associated
with ATDILI
The PubMed (https://www.ncbi.nlm.nih.gov/pubmed) and
Scopus (https://www.scopus.com/) databases were searched using the
following terms: ‘drug-induced liver injury’ OR ‘hepatitis’ OR
‘drug-induced hepatitis’ OR ‘drug-induced hepatotoxicity’ OR
‘hepatotoxicity’ OR ‘liver injury’ AND ‘pharmacogenomic OR
pharmacogenetic*’ OR ‘genetic polymorphism’ OR
‘polymorphism*’ AND ‘antituberculosis OR antitubercular’
OR ‘tuberculosis treatment’. Original articles examining the
association between genetic polymorphisms and ATDILI with a cut-off
date of October 30, 2018, were gathered. The frequencies of each
gene associated with ATDILI were counted and the top five most
frequent genes were and analysed using the STRING online software
(26). STRING integrated and ranked
protein/gene associations were benchmarked based on reference data
which consisted of experimental and predicted interactions between
each protein. The interaction network was considered relevant if
the confidence score was >0.7(26). In the protein-protein interaction
(PPI) network, each node represented a protein, and each edge
indicated a physical or theoretical interaction between two
proteins in the network.
Search strategy for literature on
GSTM1 and GSTT1
Searches for original publications were performed in
PubMed, Scopus and Web of Science (https://www.webofknowledge.com/)
databases with a cut-off date of December 25, 2018. The process was
performed using the PICO strategy (27). The PICO in this study was set as
follows: Population (P), tuberculosis patient; Intervention (I),
GSTM1 or GSTT1 polymorphisms; Comparator (C), gene
deletion and wild type; and Outcomes (O), liver injury or
hepatotoxicity. The search strategies were constructed by combining
search terms using Boolean operators, including ‘OR’ within the
same domain and ‘AND’ amongst domains (28).
Study selection for meta-analysis of
GSTM1 and GSTT1
For inclusion of a study, it had to satisfy the
specific inclusion and exclusion criteria. The inclusion criteria
were: i) case-control or cohort study investigating the association
between GSTM1 or GSTT1 and susceptibility to ATDILI
susceptibility; and ii) study participants were patients with TB
receiving isoniazid, rifampicin, pyrazinamide or ethambutol. The
exclusion criteria were: i) case report, secondary or tertiary
publications including reviews, systematic review and
meta-analysis; ii) articles not available in English; iii) studies
using healthy volunteers as the control group; iv) studies using a
duplicated set of subjects and/or data; and v) studies which
included participants with confounding factors of hepatotoxicity,
including those co-infected with hepatitis virus or human
immunodeficiency virus, excessive consumption of alcoholic
beverages or concomitant administration of other potential
hepatotoxic medication.
Assessment of the quality of the
study
To assess the quality of each study, two reviewers
independently evaluated the quality of the publications according
to the Newcastle-Ottawa scale (29).
The score from the Newcastle-Ottawa scale ranges from 0-9.
Publications were included and designated as ‘pass’ if the
publication assessment score was >5.
Data extraction for meta-analysis
Data from all the eligible studies were extracted
into a data sheet. The following data were extracted: First author,
publication year, study design, ethnicity, sample size, sex, age,
body mass index (BMI), observed medication and the number of
cases/controls for each GST (M1, T1 and
M1/T1) genotype with their odds ratio (OR) and 95%
confidence intervals (CI). If any disagreement between data
extraction results by two reviewers were revealed, it was resolved
by discussion and consensus with a third reviewer.
Statistical analysis
The extracted data such as age and BMI are presented
as the mean. Meta-analysis of the effects of GSTM1 and
GSTT1 genes were performed using Review Manager Version 5.3
(Nordic Cochrane Centre, Copenhagen, Denmark). The Mantel-Haenszel
fixed-effects model was used for the overall calculation of the OR,
95% CI and P-value calculations. All data are represented as
estimated OR with 95% CI. Subgroup analyses were performed by
stratifying patients according to ethnicity as follows: East Asian,
South Asian, South East Asian, European and South American.
P<0.05 was considered to indicate a statistically significant
difference. Heterogeneity among studies was estimated using a
χ2 test or if the I2 value was >50%
(30). Subgroup analysis was utilized
for the meta-analysis where a χ2 P-value <0.05 or an
I2 value >50% was considered significant (31). Finally, publication bias was
investigated using a funnel plot.
Results
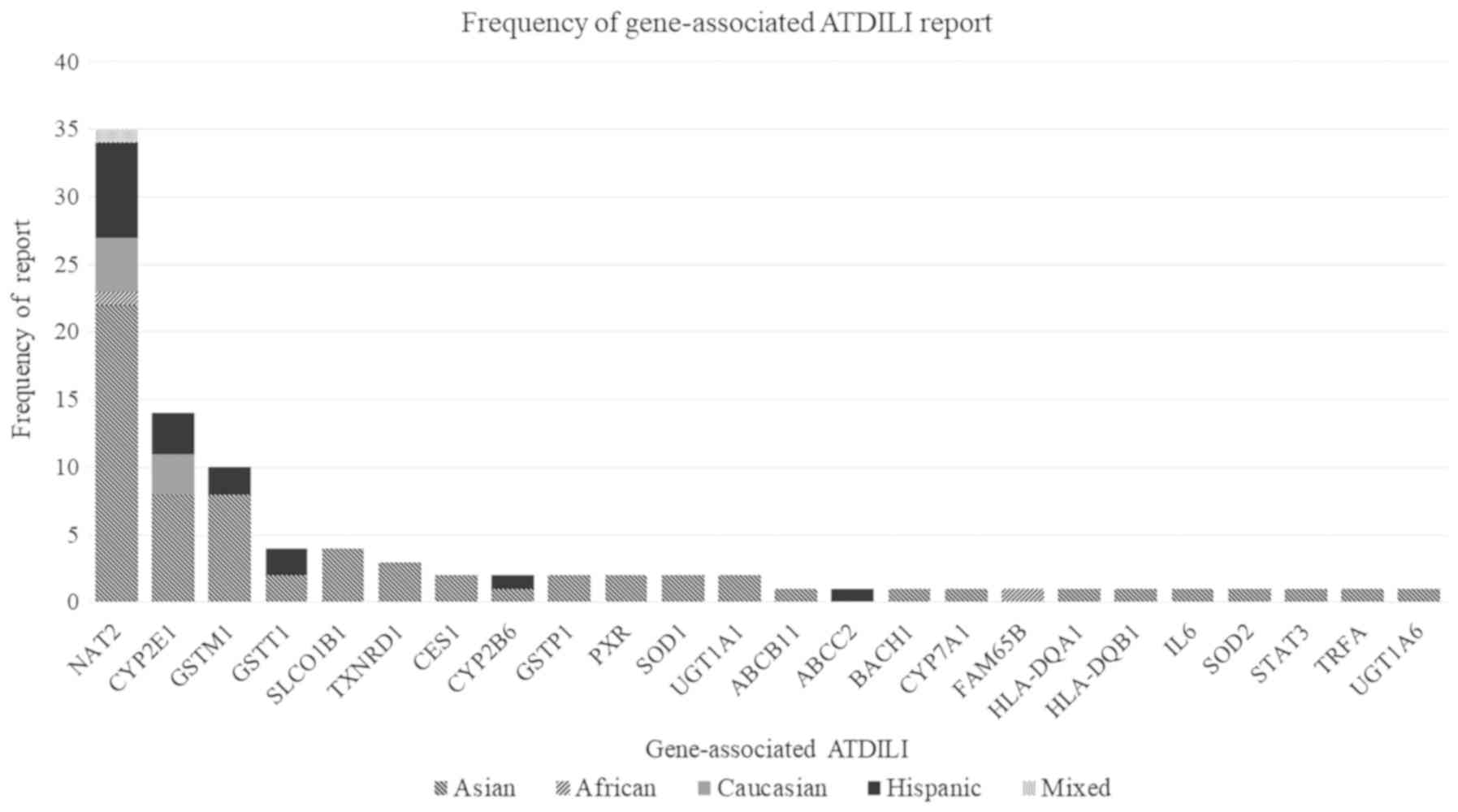
Genes associated with ATDILI
A total of 973 studies were obtained from PubMed and
Scopus databases based on the aforementioned search criteria. Of
these, 91 were duplicates and excluded. Subsequent to refining the
data using the exclusion criteria, 788 publications were excluded
as follows: irrelevant (n=695); studies in non-human models (n=54);
secondary publications (n=30); and studies where healthy volunteers
were used as the control group (n=9). Therefore, 94 publications
were included in this analysis. However, only 77 publications
identified a statistically significant gene associated with ATDILI.
There were 94 reports of genes in the 77 publications. The top five
most frequently reported genes were NAT2 (35 reports),
CYP2E1 (14 reports), GSTM1 (10 reports), GSTT1
(4 reports) and solute carrier organic anion transporter family
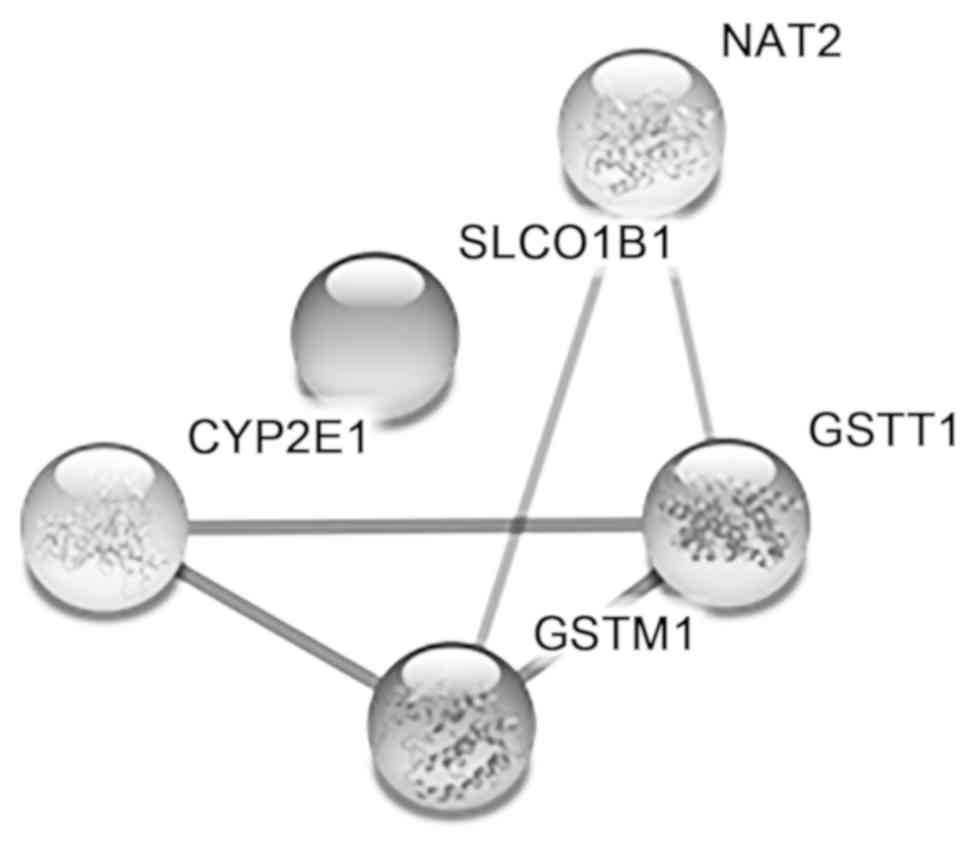
member 1B1 (SLCO1B1; 4 reports) (Fig. 1). The PPI analysis of these five genes
revealed interactions amongst GSTM1, GSTT1,
CYP2E1 and NAT2. Interestingly, according to STRING
analysis, associations between GSTM1 or GSTT1 with
CYP2E1 or NAT2 enzymes were observed in the PPI
network (Fig. 2).
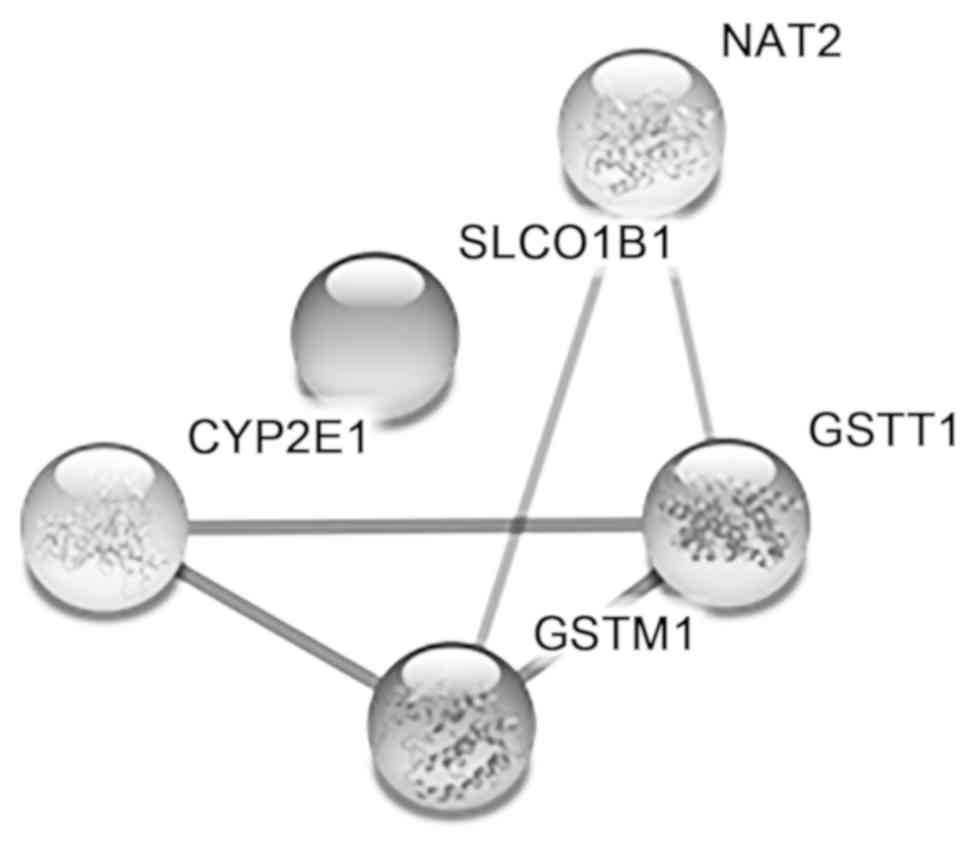 | Figure 2.Protein-protein interaction network
of NAT2, CYP2E1, GSTM1, GSTT1 and SLCO1B1 with an interaction score
of >0.7. Each node represents each protein in this pathway.
There are three types of edge. The yellow edge represents the
interaction by textmining, while the cyan egde demonstrates the
interaction in curated databases, and the black edge represents
co-expression. NAT2, N-acetyltransferase 2; CYP2E1, cytochrome P450
family 2 subfamily E member 1; GSTM1, glutathione S-transferase mu
1; GSTT1, glutathione S-transferase θ1; SLCO1B1, solute carrier
organic anion transporter family member 1B1. |
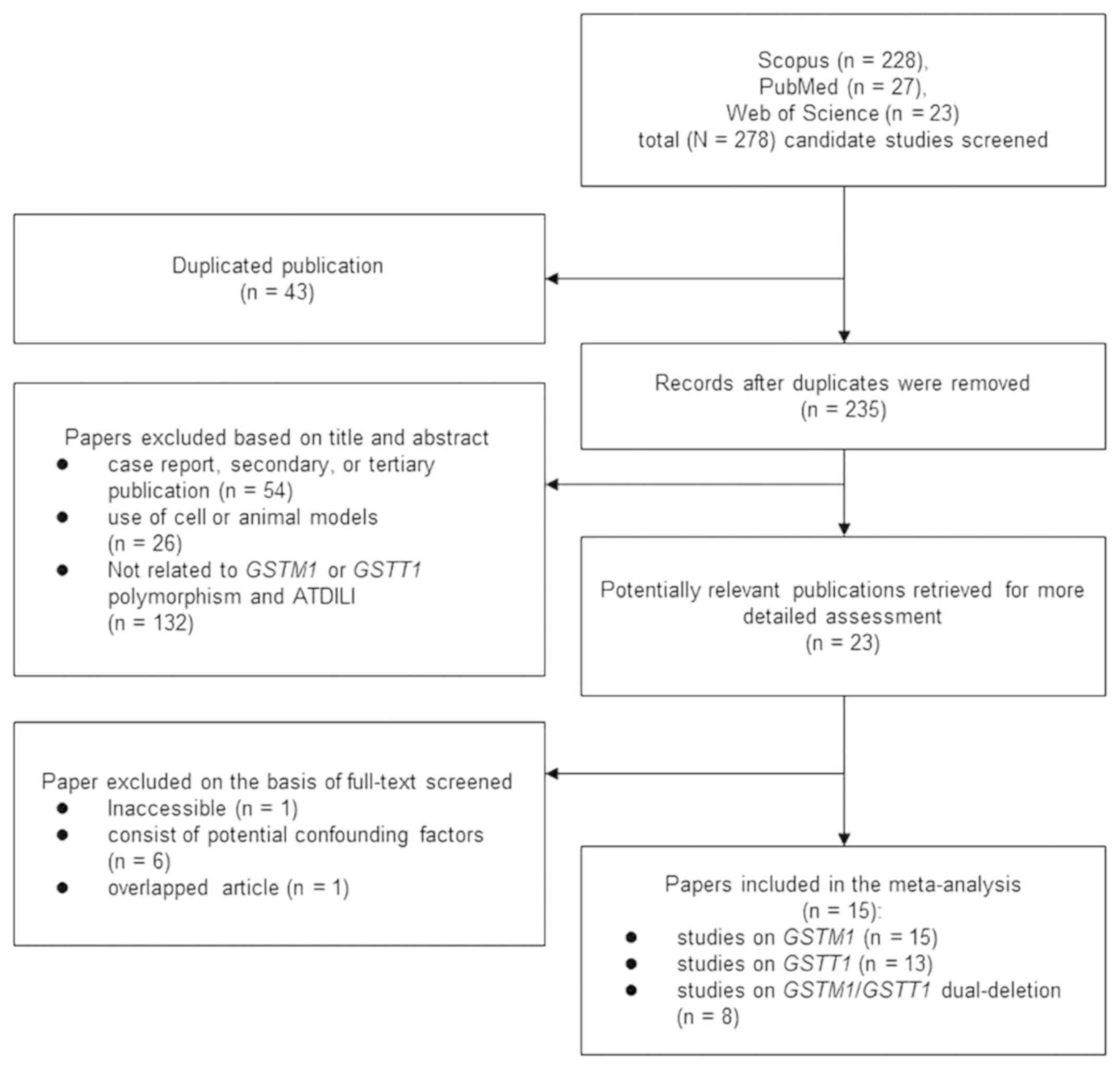
Study selection for meta-analysis of
the association between GSTM1 or GSTT1 with ATDILI
The selection process of the included studies is
illustrated in Fig. 3. Initially, a
total of 278 publications were used, and 15 publications were
selected with 905 cases of ATDILI from a total of 3,785 patients
with TB. All included publications were qualified according to the
Newcastle-Ottawa scale for case-control and cohort studies.
Study characteristics of the
meta-analyses
The studies used were published between 2001 and
2018 and are presented in Table I.
The majority of the studies were performed on East Asian (9,12,18,20,21) and
South Asian (7,8,10,14-17)
patients. Other studies were performed on South East Asian
(13), South American (19) and European patients (11).
 | Table IMain characteristics of the eligible
publications in the present updated meta-analysis. |
Table I
Main characteristics of the eligible
publications in the present updated meta-analysis.
| | | | Sample size
case/control | Sex
(male/female) | Age (mean) | BMI (mean) | |
|---|
| Author, year | Ethnicity | Study design | Case | Control | Total | Case | Control | Case | Control | Case | Control | (Refs.) |
|---|
| Perwitasari et
al 2018 | South East
Asian | Cohort | 136 | 71 | 207 | NA | NA | NA | NA | NA | NA | (13) |
| Xiang et al
2014 | East Asian | Cohort | 89 | 1,858 | 1,947 | 60/29 | 1,012/846 | 37 | 46 | 20.3 | 21.4 | (21) |
| Singla et al
2014 | South Asian | Cohort | 17 | 391 | 408 | 11/7 | 241/150 | 48 | 33 | NA | NA | (17) |
| Sharma et al
2014 | South Asian | Cohort | 113 | 201 | 314 | 63/50 | 145/56 | 28 | 35 | 17.1 | 17.1 | (16) |
| Rana et al
2014 | South Asian | Case-control | 50 | 245 | 295 | 33/22 | 152/93 | 44 | 42 | 19.23 | 23.1 | (14) |
| Liu et al
2014 | East Asian | Case-control | 20 | 143 | 163 | 12/8 | 85/58 | 4 | 6 | NA | NA | (12) |
| Gupta et al
2013 | South Asian | Case-control | 50 | 246 | 296 | 24/26 | 139/107 | 37 | 37 | 21.0 | 21.0 | (8) |
| Tang et al
2012 | East Asian | Case-control | 89 | 356 | 445 | 65/24 | 260/96 | 44 | 44 | 19.5 | 19.4 | (18) |
| Teixeira et
al 2011 | South American | Case-control | 26 | 141 | 167 | 16/10 | 74/67 | 48 | 43 | NA | NA | (19) |
| Wang et al
2010 | East Asian | Case-control | 104 | 111 | 215 | 70/34 | 75/36 | 49 | 45 | 19.8 | 20.2 | (20) |
| Kim et al
2010 | East Asian | Case-control | 57 | 190 | 247 | 34/27 | 129/61 | 47 | 42 | NA | NA | (10) |
| Chatterjee et
al 2010 | South Asian | Case-control | 51 | 100 | 151 | 25/26 | 63/37 | 37 | 33 | 16.2 | 17.5 | (7) |
| Leiro et al
2008 | European | Case-control | 35 | 60 | 95 | 14/21 | 25/35 | 34 | 31 | 23.1 | 22.1 | (11) |
| Huang et al
2007 | East Asian | Case-control | 63 | 63 | 126 | 42/22 | NA | 62 | NA | NA | NA | (9) |
| Roy et al
2001 | South Asian | Case-control | 33 | 33 | 66 | 15/18 | NA | 30 | NA | NA | NA | (15) |
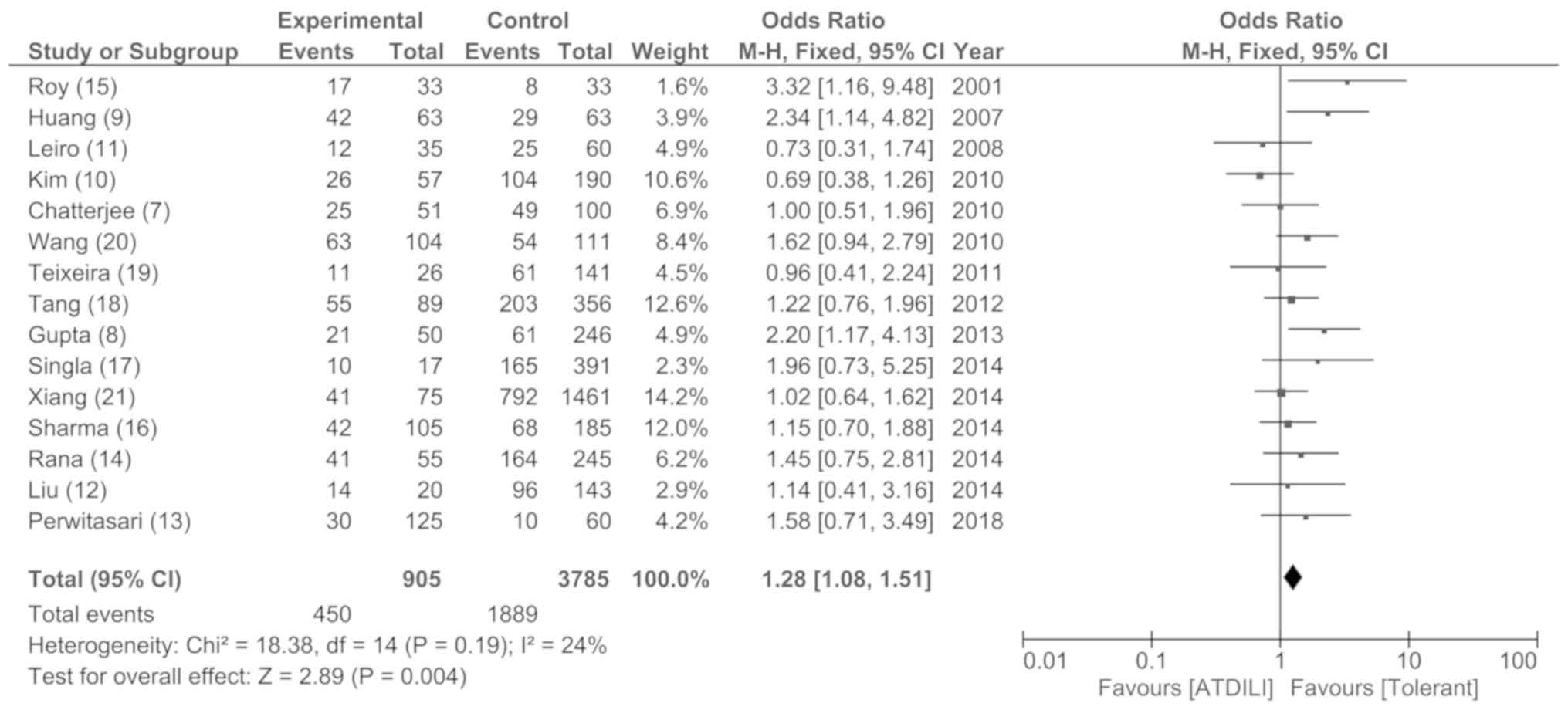
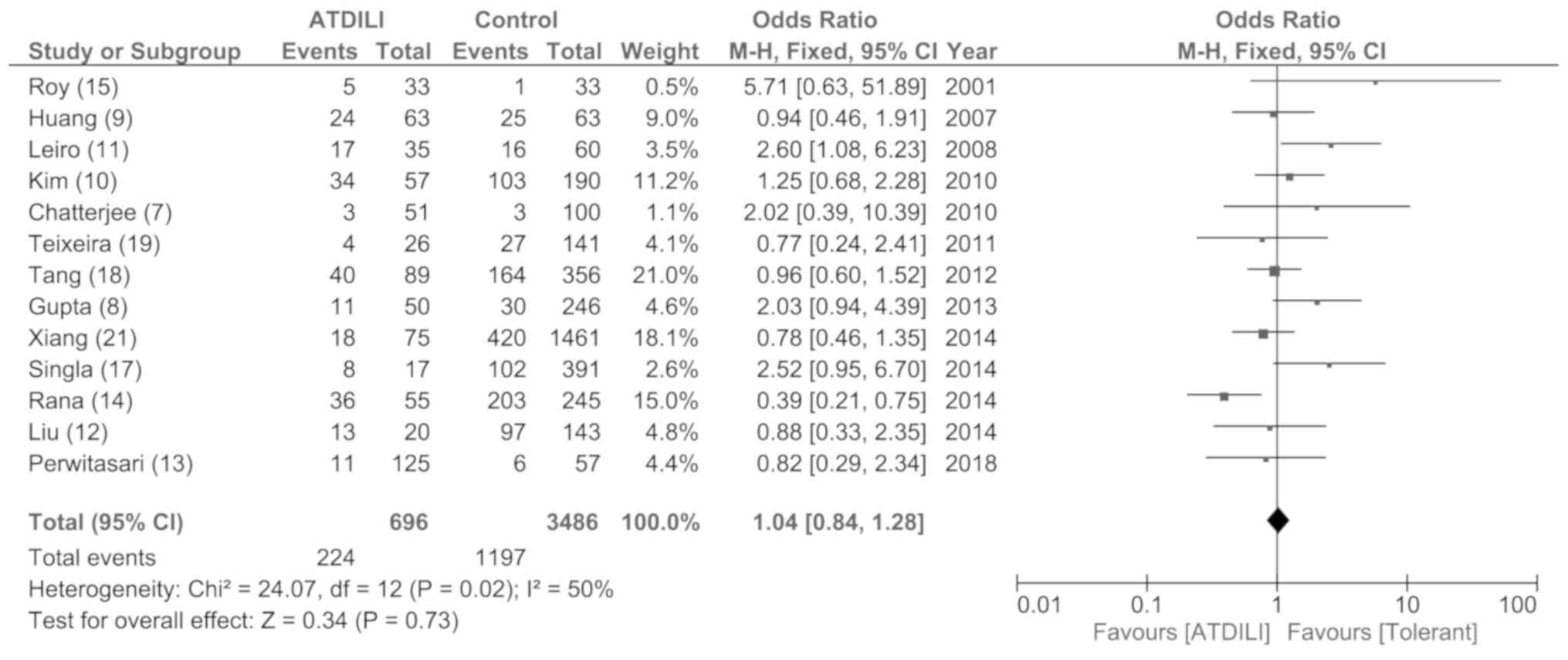
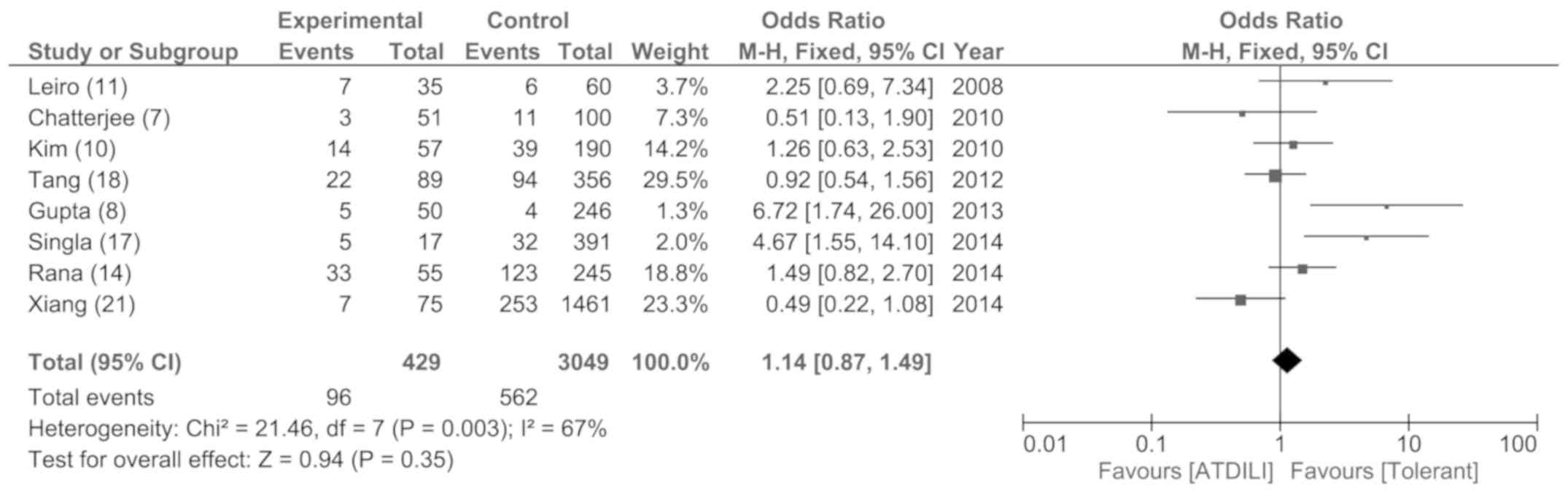
Meta-analysis of results
The associations between GSTM1, GSTT1
and GSTM1/GSTT1 dual-deletions with the
susceptibility of ATDILI in patients with TB are summarized in
Figs. 4-6. The results suggested that GSTM1 was
significantly associated with a susceptibility of ATDILI with an OR
of 1.28 (95% CI, 1.08-1.51; P<0.05; Fig. 4). However, there was no significant
difference between the cases and controls on the influence of the
dual gene deletions, the deletion of GSTT1 (Fig. 5) or GSTM1/GSTT1 (Fig. 6).
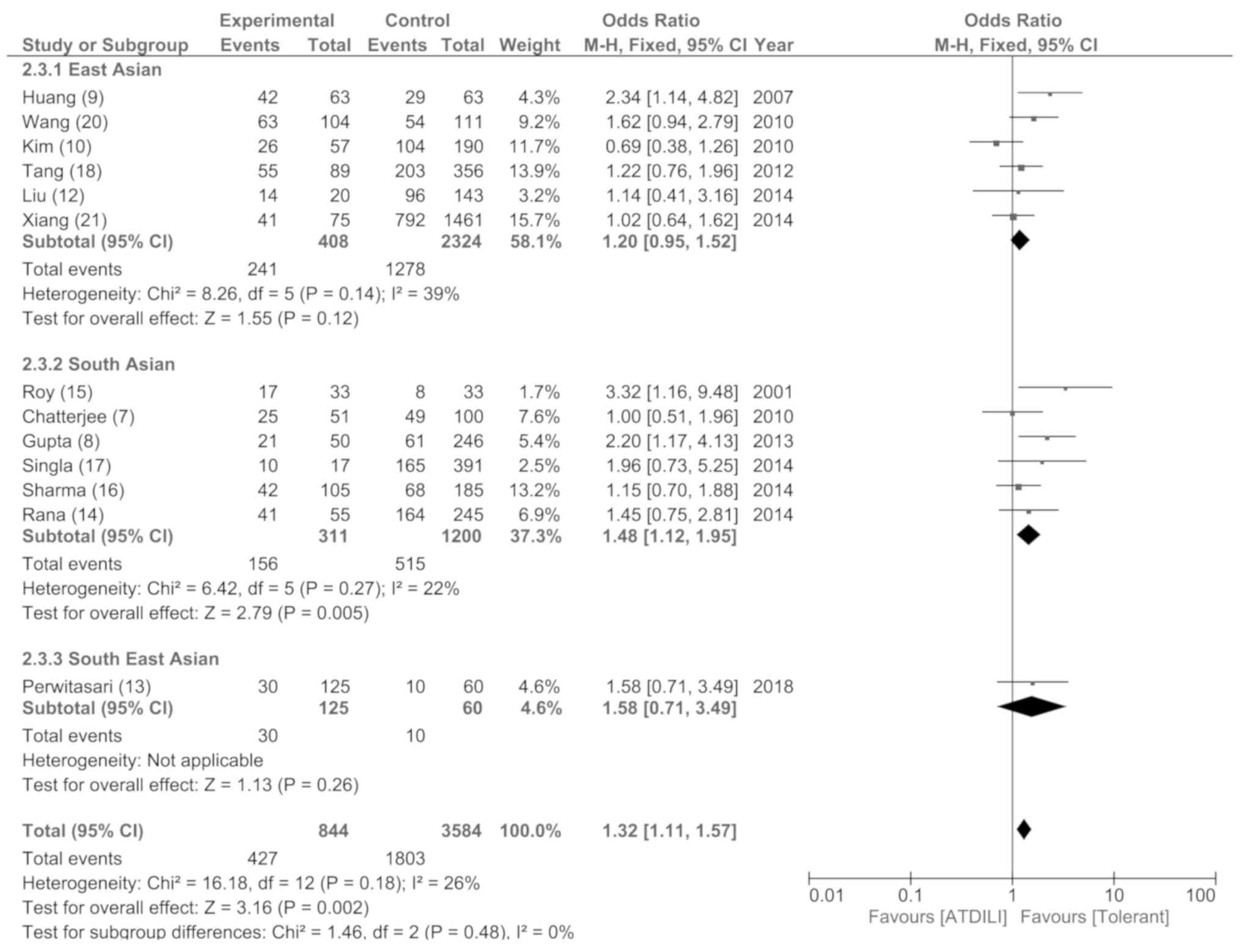
Meta-analysis sensitivity,
heterogeneity and publication bias analyses
Sensitivity analysis was performed by removing a
single study at a time to assess the effect of each study on the
overall estimate. The results demonstrated that the meta-analysis
of the GSTM1 deletion genotype passed the sensitivity
analysis. Heterogeneity was not observed in the GSTM1
deletion genotype studies (data not shown). Subgroup analysis was
used to explain the heterogeneity by subgrouping the studies
according to ethnicity as follows; East Asian, South Asian and
South East Asian (Fig. 7).
Publication bias was investigated using a funnel plot. In the
funnel plots, a condensed plot presented at the top of the 95% CI
triangle indicated a publication bias for studies with a large
number of enrolled patients. However, the plots were symmetrical
between each of the sides within the triangle which demonstrated
that publication bias was not revealed to be a negative or positive
result.
Results of subgroup meta-analysis
The subgroup analyses based on the ethnicity of
patients with TB were performed for the GSTM1 gene deletion
(Fig. 7). The results demonstrated
that the GSTM1 deletion was significantly associated with
ATDILI in South Asian patients with an OR of 1.48 (95% CI,
1.12-1.95; P<0.01). On the contrary, there was no significant
association between GSTM1 with ATDILI in any of the other
ethnicities.
Discussion
Despite extensive research efforts, current
understanding of the mechanisms which regulate the progression of
hepatotoxicity progression during the treatment of TB remains
unclear. As such, the majority of the patients with hepatotoxicity
induced by anti-TB drugs will develop end-stage liver injury due to
a lack of reliable and specific biomarkers for ATDILI (32). Genetic variations associated with
ATDILI have been extensively studied, and may be used as genetic
biomarkers for identifying patients who may be at increased risk of
ATDILI, prior to the prescription of therapeutics which may
aggravate the risk (33). In the
present analysis, previous studies on the association of genetic
variations in patients with ATDILI were analysed and the top five
most frequently reported genes were NAT2, CYP2E1,
GSTM1, GSTT1 and SLCO1B1. In addition, PPI
network analysis of these genes illustrated that there were direct
links between NAT2, CYP2E1, GSTM1 and
GSTT1 enzymes, and GSTs were indicated as serving as
a key molecule in this PPI network. Supporting this hypothesis,
alternative results from a PPI network delineated that GSTM1
was functionally associated with CYP2E1 and GSTT1 in
drug metabolism in Kyoto Encyclopedia of Genes and Genomes pathway
analysis (34) and was frequently
reported alongside the NAT2 enzyme in numerous studies
(8,14,17). Based
on the metabolism pathway of isoniazid, NAT2, CYP2E1,
GSTM1 and GSTT1 enzymes functionally associate with
each other to metabolize isoniazid, and GSTM1 and
GSTT1 enzymes function to detoxify the toxic metabolites
formed following the metabolism of isoniazid by NAT2 and
CYP2E1 (35). Based on the
data on the genes associated with ATDILI NAT2, CYP2E1, GSTM1
and GSTT1, polymorphisms of these genes may together
contribute to the risk of ATDILI. Thus, further investigation is
required to determine the effects of polymorphisms of these genes,
and how they may contribute to the risk of ATDILI. To the best of
our knowledge, there are no publications which have investigated
the influence of the multi-genetic contribution on the risk of
ATDILI. Therefore, the present study was not able to perform a
meta-analysis to demonstrate the association of the multi-gene
effect on the risk of ATDILI. A meta-analysis was performed to
verify the association between polymorphisms of GSTM1 and
GSTT1 and ATDILI risk. There was an association between a
GSTM1 null genotype with an increased risk of ATDILI in
patients with TB. This result supports the hypothesis that genetic
variation in genes encoding proteins responsible for managing
oxidation may increase the risk of ATDILI, and genetic
polymorphisms of GSTM1 and GSTT1 may serve as novel
genetic markers for predicting which patients with TB are at a
higher risk of ATDILI.
As the GST enzymes are fundamental for the
elimination of ROS through the conjugation of glutathione to
substrates including xenobiotics and ROS (4), it is not surprising that they exert
protective effects on numerous different types of cells from the
oxidative stress induced by anti-TB drugs, and an absence of
GST activity leaves the liver more susceptible to ATDILI
(2). The two major GST enzymes
which conjugate isoniazid metabolites are GSTM1 and
GSTT1, and an absence of their activity caused by homozygous
null mutations has been implicated in liver injury owing to a lack
of protection from oxidant species (5). Supporting this, the results of the
present meta-analysis revealed that a null GSTM1 genotype
was significantly associated with a higher risk of ATDILI
(P<0.05), in agreement with a number of previous meta-analyses
(5,6,21-23).
Previously, GSTM1 was reported to be significantly
correlated with a susceptibility to develop ATDILI only in East
Asian individuals, although in the present analysis, an association
between GSTM1 polymorphisms and South Asian individuals was
observed. The reason for this inconsistency is unknown, but may be
attributed to the lesser number of included publications due to the
more stringent inclusion and exclusion criteria. Therefore, further
investigation is required to determine the association between
GSTM1 deletion and ATIDILI risk in East Asian, South East
Asian, Caucasian and African individuals.
It has been demonstrated that the homozygous null
mutation of GSTT1 may result in the loss of detoxification
activity of hepatotoxic reactive metabolites in hepatocytes
(36). Thus, it seems plausible that
a GSTT1 null genotype may result in an increased risk of
ATDILI. Nonetheless, in the present study, no significant
association between a null GSTT1 genotype and ATDILI was
observed, consistent with previous meta-analyses (6,22-24).
A potential explanation for this result may be due to the small
sample sizes. In the present study, although 905 ATDILI cases and
2,880 controls were pooled, the number of subjects was still
insufficient. Tang et al (6)
suggested that a cohort of >10,000 patients is required to
determine the significance of a polymorphism when the risk of a
polymorphism is moderate (37).
Alternatively, Bao et al (4)
illustrated that there are multiple factors, including genetic and
environmental factors, which influence the pathogenesis of ATDILI.
In the present analysis, confounding environmental factors
including viral hepatitis, HIV infection and alcohol consumption
were excluded, but other factors including age, sex and BMI were
included, which may have thus resulted in an inaccurate
association. Altogether, it was not possible to ascertain whether a
null GSTT1 genotype was associated with the risk of ATDILI,
for which a multi-centre genetic association study with larger
sample sizes and well-characterized subjects is required.
Whether combined GSTM1 and GSTT1 null
genotypes are associated with an elevated risk of ATDILI remains
yet to be determined. Lucena et al (38) focused on investigating the potential
association between a combination of GSTM1 and GSTT1
polymorphisms with DILI and demonstrated a significant association
between GSTM1 and GSTT1 dual-null polymorphisms and
an increased risk of ATDILI. In the present analysis, no
significant association between GSTM1/GSTT1 dual-null
genotypes and ATDILI risk was observed. This contrasting result may
be attributable to differences in the pathophysiology of
hepatoxicity, ethnicity and the type of drugs prescribed between
studies. Supporting the observation that there was no association
between GSTM1/GSTT1 dual-null genotypes and ATDILI risk,
Ginsberg et al (39)
investigated the genotypic frequency and distribution of
GSTM1 and GSTT1 null genotypes in a wide spectrum of
the human populations, and they revealed that GSTM1 or
GSTT1 null genotypes were highly prevalent in Asian patients
compared with GSTM1/GSTT1 dual-null polymorphisms.
If there is a direct link between a null
GSTM1 genotype and an increased risk of ATDILI in patients
with TB, it may be hypothesized that a homozygous deletion of
GSTM1 results in a loss of GSTM1 enzyme activity
contributing to the pathogenesis of hepatoxicity influenced by
anti-TB drugs. Hepatotoxicity induced by anti-TB drugs,
particularly isoniazid, is mediated through toxic intermediaries,
including hydrazine and acetyldiazine, in addition to ROS (40,41). An
increase in ROS production results in increased oxidative stress,
which in turn induces organ failure, particularly of the liver
(40), in which NAT2 and
CYP2E1 have been revealed to be responsible for a
biotransformation pathway of isoniazid-induced increased ROS
generation (34). In a NAT2-
and CYP2E1-mediated detoxification of an isoniazid-mediated
increase in ROS levels, GST enzymes are known to serve a
protective function against oxidative stress-induced cellular
injury (4), suggesting that
GSTs may serve a function in the detoxification of anti-TB
drugs. This hypothesis is supported by the results from the PPI
network analysis, in which a functional association between
GSTs with NAT2 and CYP2E1 was observed, and
the centrality of GST enzymes in the interactions between
molecules was established. Although results from the present
meta-analysis along with PPI network analysis provide support for
an association between GSTM1 deletion and an increased risk
of ATDILI in patients with TB, the function of genetic variations
of GSTs genes and the risk of ATDILI remains yet to be
determined, and additional research is required to determine their
function in the detoxification of oxidative intermediates which
results from the metabolism of anti-TB drugs.
There are certain limitations in the present study.
The major limitation of the present study is that it only
illustrated the association of ATDILI with GSTT1
polymorphisms using the previous case-control and cohort study
results; however, the exact function of GSTT1 in the
pathogenesis of ATDILI was unable to be determined. To address the
cause and effect association, further experimental studies using
in vivo models need to be performed. Another limitation is
that the present study only included publications which were
published in the English language, thus a language bias was
unavoidable. In addition, pooling data from different types of
study designs, including case-controlled and cohort studies, may
provide a higher number of studies compared with previous
meta-analyses; however, these may contribute to significant
heterogeneity. On the other hand, the strength of the present study
is that all publications with confounding factors were excluded to
better mitigate the effect of the confounding factors, providing
more reliable results.
In conclusion, the meta-analysis revealed that a
GSTM1 null genotype was significantly associated with the
susceptibility of ATDILI, particularly in South Asian individuals.
However, there was no association between a null GSTT1 or a
dual-null GSTM1/GSTT1 genotype and risk of ATDILI. STRING
analysis revealed that GSTs interact with other proteins
associated with ATDILI, including NAT2 and CYP2E1,
and thus may exert a protective function. Additional studies are
required with larger sample sizes, well-characterized subjects and
various ethnicities including South East Asian, Caucasian and
African individuals to draw a more precise conclusion and support
the use of these genetic markers for predicting the risk of ATDILI
in patients with TB.
Acknowledgements
The authors would like to thank The International
Research Network team for their grant, encouragement, and technical
support and Dr Supharat Suvichapanich (Department of Biochemistry,
Faculty of Pharmacy, Mahidol University) and Mrs. Saowalak
Turongkaravee (Department of Pharmacy, Faculty of Pharmacy, Mahidol
University) for their constructive comments and suggestions.
Funding
The present study was supported by The International
Research Network of The Thailand Research Fund (grant no.
IRN60W003) and Medical Scholar Program of Mahidol University
(Thailand).
Availability of data and materials
The data analysed and generated during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JJ, UC, SM and SW conceived and designed the study.
NC and WU performed literature review. NC retrieved the data. JJ
and NC reviewed the assessment of the quality of the study. NC
performed the meta-analyses. NC, JJ, and WU wrote the manuscript.
All authors edited and revised the manuscript. All authors approved
the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tostmann A, Boeree MJ, Aarnoutse RE, de
Lange WC, van der Ven AJ and Dekhuijzen R: Antituberculosis
drug-induced hepatotoxicity: Concise up-to-date review. J
Gastroenterol Hepatol. 23:192–202. 2008.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ramappa V and Aithal GP: Hepatotoxicity
related to anti-tuberculosis drugs: Mechanisms and management. J
Clin Exp Hepatol. 3:37–49. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Clare KE, Miller MH and Dillon JF: Genetic
factors influencing drug-induced liver injury: Do they have a role
in prevention and diagnosis? Curr Hepatol Rep. 16:258–264.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bao Y, Ma X, Rasmussen TP and Zhong XB:
Genetic variations associated with anti-tuberculosis drug-induced
liver injury. Curr Pharmacol Rep. 4:171–181. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Eaton DL and Bammler TK: Concise review of
the glutathione S-transferases and their significance to
toxicology. Toxicol Sci. 49:156–164. 1999.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tang N, Deng R, Wang Y, Lin M, Li H, Qiu
Y, Hong M and Zhou G: GSTM1 and GSTT1 null
polymorphisms and susceptibility to anti-tuberculosis drug-induced
liver injury: A meta-analysis. Int J Tuberc Lung Dis. 17:17–25.
2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chatterjee S, Lyle N, Mandal A and Kundu
S: GSTT1 and GSTM1 gene deletions are not associated
with hepatotoxicity caused by antitubercular drugs. J Clin Pharm
Ther. 35:465–470. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gupta VH, Singh M, Amarapurkar DN, Sasi P,
Joshi JM, Baijal R, H R PK, Amarapurkar AD, Joshi K and Wangikar
PP: Association of GST null genotypes with anti-tuberculosis
drug induced hepatotoxicity in western indian population. Ann
Hepatol. 12:959–965. 2013.PubMed/NCBI
|
|
9
|
Huang YS, Su WJ, Huang YH, Chen CY, Chang
FY, Lin HC and Lee SD: Genetic polymorphisms of manganese
superoxide dismutase, NAD(P)H: Quinone oxidoreductase, glutathione
S-transferase M1 and T1, and the susceptibility to drug-induced
liver injury. J Hepatol. 47:128–134. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kim SH, Kim SH, Yoon HJ, Shin DH, Park SS,
Kim YS, Park JS and Jee YK: GSTT1 and GSTM1 null
mutations and adverse reactions induced by antituberculosis drugs
in koreans. Tuberculosis (Edinb). 90:39–43. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Leiro V, Fernandez-Villar A, Valverde D,
Constenla L, Vázquez R, Piñeiro L and González-Quintela A:
Influence of glutathione S-transferase M1 and T1 homozygous null
mutations on the risk of antituberculosis drug-induced
hepatotoxicity in a Caucasian population. Liver Int. 28:835–839.
2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liu F, Jiao AX, Wu XR, Zhao W, Yin QQ, Qi
H, Jiao WW, Xiao J, Sun L, Shen C, et al: Impact of glutathione
S-transferase M1 and T1 on anti-tuberculosis drug-induced
hepatotoxicity in Chinese pediatric patients. PLoS One.
9(e115410)2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Perwitasari DA, Darmawan E, Mulyani UA,
Vlies PV, Alffenaar JC, Atthobar J and Wilffert B: Polymorphisms of
NAT2, CYP2E1, GST, and HLA related to
drug-induced liver injury in indonesian tuberculosis patients. Int
J Mycobacteriology. 7:380–386. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rana SV, Sharma SK, Ola RP, Kamboj JK,
Malik A, Morya RK and Sinha SK: N-Acetyltransferase 2, cytochrome
P4502E1 and glutathione S-transferase genotypes in antitubercular
treatment-induced hepatotoxicity in North Indians. J Clin Pharm
Ther. 39:91–96. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Roy B, Chowdhury A, Kundu S, Santra A, Dey
B, Chakraborty M and Majumder PP: Increased risk of
antituberculosis drug-induced hepatotoxicity in individuals with
glutathione S-transferase M1 ‘null’ mutation. J Gastroenterol
Hepatol. 16:1033–1037. 2001.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sharma SK, Jha BK, Sharma A, Sreenivas V,
Upadhyay V, Jaisinghani C, Singla R, Mishra HK and Soneja M:
Genetic polymorphisms of CYP2E1 and GSTM1 loci and
susceptibility to anti-tuberculosis drug-induced hepatotoxicity.
Int J Tuberc Lung Dis. 18:588–593. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Singla N, Gupta D, Birbian N and Singh J:
Association of NAT2, GST and CYP2E1
polymorphisms and anti-tuberculosis drug-induced hepatotoxicity.
Tuberculosis (Edinb). 94:293–298. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tang SW, Lv XZ, Zhang Y, Wu SS, Yang ZR,
Xia YY, Tu DH, Deng PY, Ma Y, Chen DF and Zhan SY: CYP2E1,
GSTM1 and GSTT1 genetic polymorphisms and
susceptibility to antituberculosis drug-induced hepatotoxicity: A
nested case-control study. J Clin Pharm Ther. 37:588–593.
2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Teixeira RL, Morato RG, Cabello PH, Muniz
LM, Moreira Ada S, Kritski AL, Mello FC, Suffys PN, Miranda AB and
Santos AR: Genetic polymorphisms of NAT2, CYP2E1 and GST enzymes
and the occurrence of antituberculosis drug-induced hepatitis in
Brazilian TB patients. Mem Inst Oswaldo Cruz. 106:716–724.
2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wang T, Yu HT, Wang W, Pan YY, He LX and
Wang ZY: Genetic polymorphisms of cytochrome P450 and glutathione
S-transferase associated with antituberculosis drug-induced
hepatotoxicity in Chinese tuberculosis patients. J Int Med Res.
38:977–986. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Xiang Y, Ma L, Wu W, Liu W, Li Y, Zhu X,
Wang Q, Ma J, Cao M, Wang Q, et al: The incidence of liver injury
in uyghur patients treated for TB in xinjiang uyghur autonomous
region, China, and its association with hepatic enzyme
polymorphisms NAT2, CYP2E1, GSTM1 and GSTT1. PLoS One.
9(e85905)2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Cai Y, Yi J, Zhou C and Shen X:
Pharmacogenetic study of drug-metabolising enzyme polymorphisms on
the risk of anti-tuberculosis drug-induced liver injury: A
meta-analysis. PLoS One. 7(e47769)2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Li C, Long J, Hu X and Zhou Y:
GSTM1 and GSTT1 genetic polymorphisms and risk of
anti-tuberculosis drug-induced hepatotoxicity: An updated
meta-analysis. Eur J Clin Microbiol Infect Dis. 32:859–868.
2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sun F, Chen Y, Xiang Y and Zhan S:
Drug-metabolising enzyme polymorphisms and predisposition to
anti-tuberculosis drug-induced liver injury: A meta-analysis. Int J
Tuberc Lung Dis. 12:994–1002. 2008.PubMed/NCBI
|
|
25
|
Cai L, Cai MH, Wang MY, Xu YF, Chen WZ,
Qin SY, Wan CL and He L: Meta-analysis-based preliminary
exploration of the connection between ATDILI and schizophrenia by
GSTM1/T1 gene polymorphisms. PLoS One.
10(e0128643)2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Szklarczyk D, Franceschini A, Wyder S,
Forslund K, Heller D, Huerta-Cepas J, Simonovic M, Roth A, Santos
A, Tsafou KP, et al: STRING v10: Protein-protein interaction
networks, integrated over the tree of life. Nucleic Acids Res.
43:D447–D452. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Aslam S and Emmanuel P: Formulating a
researchable question: A critical step for facilitating good
clinical research. Indian J Sex Transm Dis AIDS. 31:47–50.
2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Grewal A, Kataria H and Dhawan I:
Literature search for research planning and identification of
research problem. Indian J Anaesth. 60:635–639. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wells G, Shea B, O'Connell D, Robertson J,
Peterson J, Welch V, Losos M and Tugwell P: The Newcastle-Ottawa
Scale (NOS) for assessing the quality of nonrandomised studies in
meta-analyses. Ottawa Hospital Research Institute. 2019.
|
|
30
|
Higgins JP and Thompson SG: Quantifying
heterogeneity in a meta-analysis. Stat Med. 21:1539–1558.
2002.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Higgins JP, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003.PubMed/NCBI View Article : Google Scholar
|
|
32
|
McGill MR and Jaeschke H: Biomarkers of
drug-induced liver injury: Progress and utility in research,
medicine, and regulation. Expert Rev Mol Diagn. 18:797–807.
2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Saukkonen JJ, Cohn DL, Jasmer RM, Schenker
S, Jereb JA, Nolan CM, Peloquin CA, Gordin FM, Nunes D, Strader DB,
et al: An official ATS statement: Hepatotoxicity of
antituberculosis therapy. Am J Respir Crit Care Med. 174:935–952.
2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kanehisa M and Goto S: KEGG: Kyoto
encyclopedia of genes and genomes. Nucleic Acids Res. 28:27–30.
2000.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wang P, Pradhan K, Zhong XB and Ma X:
Isoniazid metabolism and hepatotoxicity. Acta Pharm Sin B.
6:384–392. 2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Roy PD, Majumder M and Roy B:
Pharmacogenomics of anti-TB drugs-related hepatotoxicity.
Pharmacogenomics. 9:311–321. 2008.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Ioannidis JP, Trikalinos TA and Khoury MJ:
Implications of small effect sizes of individual genetic variants
on the design and interpretation of genetic association studies of
complex diseases. Am J Epidemiol. 164:609–614. 2006.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Lucena MI, Andrade RJ, Martínez C,
Ulzurrun E, García-Martín E, Borraz Y, Fernández MC, Romero-Gomez
M, Castiella A, Planas R, et al: Glutathione S-transferase m1 and
t1 null genotypes increase susceptibility to idiosyncratic
drug-induced liver injury. Hepatology. 48:588–596. 2008.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ginsberg G, Smolenski S, Hattis D, Guyton
KZ, Johns DO and Sonawane B: Genetic polymorphism in glutathione
transferases (GST): Population distribution of GSTM1,
T1, and P1 conjugating activity. J Toxicol Environ
Health B Crit Rev. 12:389–439. 2009.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Chowdhury A, Santra A, Bhattacharjee K,
Ghatak S, Saha DR and Dhali GK: Mitochondrial oxidative stress and
permeability transition in isoniazid and rifampicin induced liver
injury in mice. J Hepatol. 45:117–126. 2006.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zhai Q, Lu SR, Lin Y, Yang QL and Yu B:
Oxidative stress potentiated by diallylsulfide, a selective CYP2E1
inhibitor, in isoniazid toxic effect on rat primary hepatocytes.
Toxicol Lett. 183:95–98. 2008.PubMed/NCBI View Article : Google Scholar
|