Introduction
Pulmonary osseous metaplasia or ossification of the
lung is the presence of mature bone tissue within the lung
parenchyma; it is a rare entity and is usually associated with some
other form of chronic pulmonary disease, such as bronchiectasis,
pneumonia or pulmonary fibrosis (1,2).
Pulmonary osseous metaplasia is mostly observed as a post-mortem
finding in autopsies of patients who were not diagnosed during
their lifetime (3). The bone
metastases could be localized or spread throughout the lungs
(1). Unless associated with other
diseases, they usually tend to be asymptomatic, and various imaging
techniques (such as chest radiography and computed tomography) and
bone scans are required for their diagnosis (2). Disseminated ossification of the lung
generally seems to have two main patterns, namely the dendriform
and nodular patterns. Branching along the terminal airway with
marrow islands is observed in the dendriform pattern; however, the
nodular pattern is more often found in the alveolar space and is
usually more localized (4). A study
found that in autopsies, diffuse pulmonary ossification occurs at a
rate of 1.63 per 1,000 cases. Nevertheless, there is an absence of
information concerning the occurrence of both types in living cases
(3).
The pathophysiology of the condition is not well
known, but there have been some associations reported in the
literature, such as the association with other lung diseases
(2). As the disease tends to be
extremely rare in living patients, little knowledge is available on
whether or not it has a sexual predominance or even its preferred
age group. With this in mind, it is worth noting that in one study,
among 10,426 autopsy cases of diffuse pulmonary ossification, there
was a predilection for males (88%) (3).
The aim of the current study is to present a case of
pulmonary osseous metaplasia recorded in a 64-year-old female. The
present report discusses the diagnosis and treatment of such a rare
entity that was initially suspected to be a metastatic
condition.
Case report
Patient information
A 64-year-old woman who had previously been
diagnosed with transitional cell carcinoma (TCC) of the lower
ureter was referred to Smart Health Tower (Sulaymaniyah, Iraq) in
July 2023 for the management of a pulmonary nodule found during a
routine check-up [chest-abdomen-pelvic computed tomography (CT)
scan]. The patient was asymptomatic.
Clinical findings
Cardiovascular, respiratory and genitourinary
examinations were normal. All vital signs were within the normal
ranges. There were no signs of tuberculosis (TB) and the past
medical history for TB was negative.
Diagnostic assessment
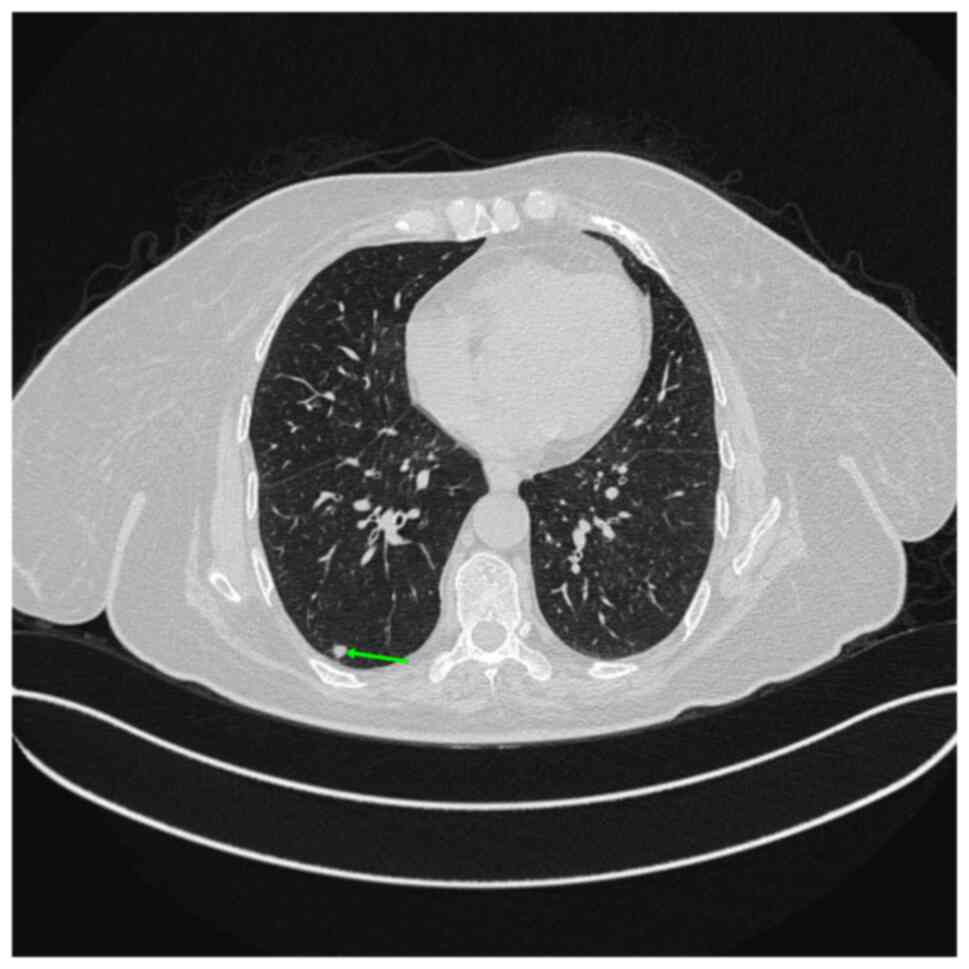
A CT scan of the chest revealed a well-demarcated
pleural-based solid hyperdense nodule measuring 4x4 mm in the
posterior segment of the right lower lobe of the lung. After 6
weeks, the CT scan was repeated and showed a slight increase in the
nodule size to 5 mm. The radiologist suspected a metastasis
(Fig. 1).
Therapeutic intervention
The patient was prepared for general anesthesia, in
the lateral position, and the nodule was resected through uniport
video-assisted thoracoscopic surgery (VATS). Four enlarged
mediastinal lymph nodes were also resected, with the largest lymph
node being 1 cm in size. The histopathological examination of the
nodule and nodal specimens revealed myeloid-osseous metaplasia of
the lung (Fig. 2). Specimens were
fixed in 10% neutral buffered formalin at room temperature for 24
h, section to a 4-µm thickness, and stained using hematoxylin and
eosin for 1-2 min at room temperature. Slides were observed under a
light microscope (x400 magnification).
Follow-up and outcomes
The patient remained in the hospital for 2 days
receiving intravenous antibiotic (400 mg ciprofloxacin twice per
day) and oral analgesics (1 g acetaminophen and 1 g ketorolac, both
three times per day). The post-operative period was uneventful. The
patient has been followed up for 3 months, and the prognosis
remains good.
Discussion
The finding of well-developed bone tissue within the
parenchyma of the lung is not a common phenomenon (5). If the pulmonary ossification is seen
to be diffuse and not localized, then it is more likely a
protective mechanism arising to shield the lung from chronic
irritation and injury (6). Despite
its association with pulmonary infections, in a previous study,
diffuse dendriform ossification of the lung was observed in only 5
out of 75 patients with previously diagnosed interstitial pneumonia
proven by biopsy (7). The nodular
pattern of osseous metaplasia, such as that in the present case,
tends to be even rarer, with no statistics recorded.
Due to the limited information available in the
literature with regard to osseous metaplasia, its exact etiology
and pathophysiology remain unclear. Ossification has been reported
in avascular bronchial cartilage along with other abnormalities
such as calcification and fibrovascular ingrowth in patients who
have undergone a lung transplantation (8). Osseous metaplasia has also been
suggested to be induced by bacterial infections that arise due to
cystic fibrosis, which also eliminates the bronchial cartilage
(9). Pulmonary bone metaplasia has
also been reported in patients with TB infection (10). Previous lung injury, hypercalcemia
and an environment with elevated pH are other factors involved in
the etiology (2). The alkaline
environment due to scar tissue injury facilitates the precipitation
of calcium (11).
A definite diagnosis requires histopathological
confirmation, while a high-resolution CT scan might suggest the
condition (1). The dendriform
pattern is observed as branching shadows of dense calcification
usually appearing similar to bronchiectasis and fibrosis formed
from a scar, whereas the subpleural nodular pattern with more than
one nodule smaller than 1 cm is characteristic of a previous
infection (4). The current patient
had the nodular subtype with an enhancing basal lung nodule that
appeared to be <5 mm in diameter. The diagnosis was confirmed by
histopathological examination, which revealed small calcified
nodules in the parenchymal tissue consisting of mature bone
trabeculae with elements of the marrow found within their medullary
spaces.
Due to the rarity of the disease, no consensus has
been found in the literature regarding its management (1). In the current case, after waiting for
6 weeks, repeating the CT scan and discussing the condition with
the tumor board, uniport VATS resection was recommended, as the
provisional diagnosis was pulmonary metastasis from the TCC
(12).
The primary limitations of this report include the
absence of data on the TNM stage and previous management of the
urinary tract tumor, which was handled at another medical center.
This absence prevents the investigation of the potential emergence
of pulmonary calcification as a side effect of the treatment.
Additionally, the case lacks data on blood calcium and vitamin D
levels, and a blood gas analysis of pH.
In conclusion, myeloid osseous metaplasia of the
lung is a rare finding. Based on this report, it may be associated
with TCC.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
FHK was a major contributor to the conception of the
study, as well as to the literature search for related studies. ASA
and PMK were involved in the literature review, study design and
writing the manuscript. SHT, RJR, JIH and BJHA were involved in the
literature review, the design of the study, the critical revision
of the manuscript and the processing of the figures. FHK and PMK
confirm the authenticity of all the raw data. AMA was the
pathologist who performed the histopathological diagnosis. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Eum SY, Kong JH, Jeon BY, Cho SN, Kim J,
Via LE, Barry Iii CE and Koh WJ: Metaplastic ossification in the
cartilage of the bronchus of a patient with chronic multi-drug
resistant tuberculosis: a case report. J Med Case Rep.
4(156)2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chan ED, Morales DV, Welsh CH, McDermott
MT and Schwarz MI: Calcium deposition with or without bone
formation in the lung. Am J Respir Crit Care Med. 165:1654–1669.
2002.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tseung J and Duflou J: Diffuse pulmonary
ossification: An uncommon incidental autopsy finding. Pathology.
38:45–48. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fraser RG: Diagnosis of diseases of the
chest. 3rd edition. Philadelphia: Saunders, 1988.
|
|
5
|
Mier OJM, Lemus MLR, Cuevas BRA, Gómez NG,
Jorge LD, Jafif M and Cervantes Ó: Bone metastasis in lung and
pulmonary emphysema in a healthy individual with chronic cough and
weight loss. Acta Med. 20:358–360. 2022.
|
|
6
|
Poon C: Pulmonary osseous metaplasia
associated with UI. Chest. 140 (Suppl)(134A)2011.
|
|
7
|
Kim TS, Han J, Chung MP, Chung MJ and Choi
YS: Disseminated dendriform pulmonary ossification associated with
usual interstitial pneumonia: Incidence and thin-section
CT-pathologic correlation. Eur Radiol. 15:1581–1585.
2005.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yousem SA, Dauber JH and Griffith BR:
Bronchial cartilage alterations in lung transplantation. Chest.
98:1121–1124. 1990.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Haraguchi M, Shimura S and Shirato K:
Morphometric analysis of bronchial cartilage in chronic obstructive
pulmonary disease and bronchial asthma. Am J Respir Crit Care Med.
159:1005–1013. 1999.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shuangshoti S: Metaplasia of bone in lungs
and bronchi: Report of 2 cases. J Med Assoc Thai. 78:103–107.
1995.PubMed/NCBI
|
|
11
|
Peros-Golubicić T and Tekavec-Trkanjec J:
Diffuse pulmonary ossification: An unusual interstitial lung
disease. Curr Opin Pulm Med. 14:488–492. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kareem PM, Karim SO, Sofi HA, Fuad FE,
Kakamad SH, Abdullah HO, Abdalla BA, Hussein SM, Rahim HM, Hassan
MN, et al: Uniport versus multiport video assisted thoracoscopic
surgery (VATS): Comparisons and outcomes; a review article. Barw
Med J. 1:1–3. 2023.
|