1. Introduction
Clostridium difficile (C. difficile)
is a Gram-positive, anaerobic, toxin-producing germ first isolated
from the stool of healthy newborns in 1935(1). It is the most common cause of
antimicrobial therapy-associated diarrhea and is a common
healthcare-associated pathogen (2).
In recent years, there has been an increase in the incidence of
community-acquired infection in subjects without known risk factors
(3,4), such as previous exposure to
antibiotics, patients with chronic gastrointestinal pathology or
inflammatory bowel disease (IBD).
C. difficile may be considered a constituent
of the normal microbiota, but under specific conditions that
disrupt the normal intestinal microbiota, it colonizes the large
intestine causing, through the action of its toxins, varying
degrees of colonic damage, ranging from mild diarrhea to toxic
megacolon (5).
In recent years, there have been substantial changes
in its diagnostic and therapeutic management (6). However, there is a lack of research on
C. difficile infection (CDI) in children, with much of the
data being extrapolated from studies of adult patients (7).
The aim of the present review was to provide the
pediatrician with up-to-date information and recommendations on CDI
in pediatric patients.
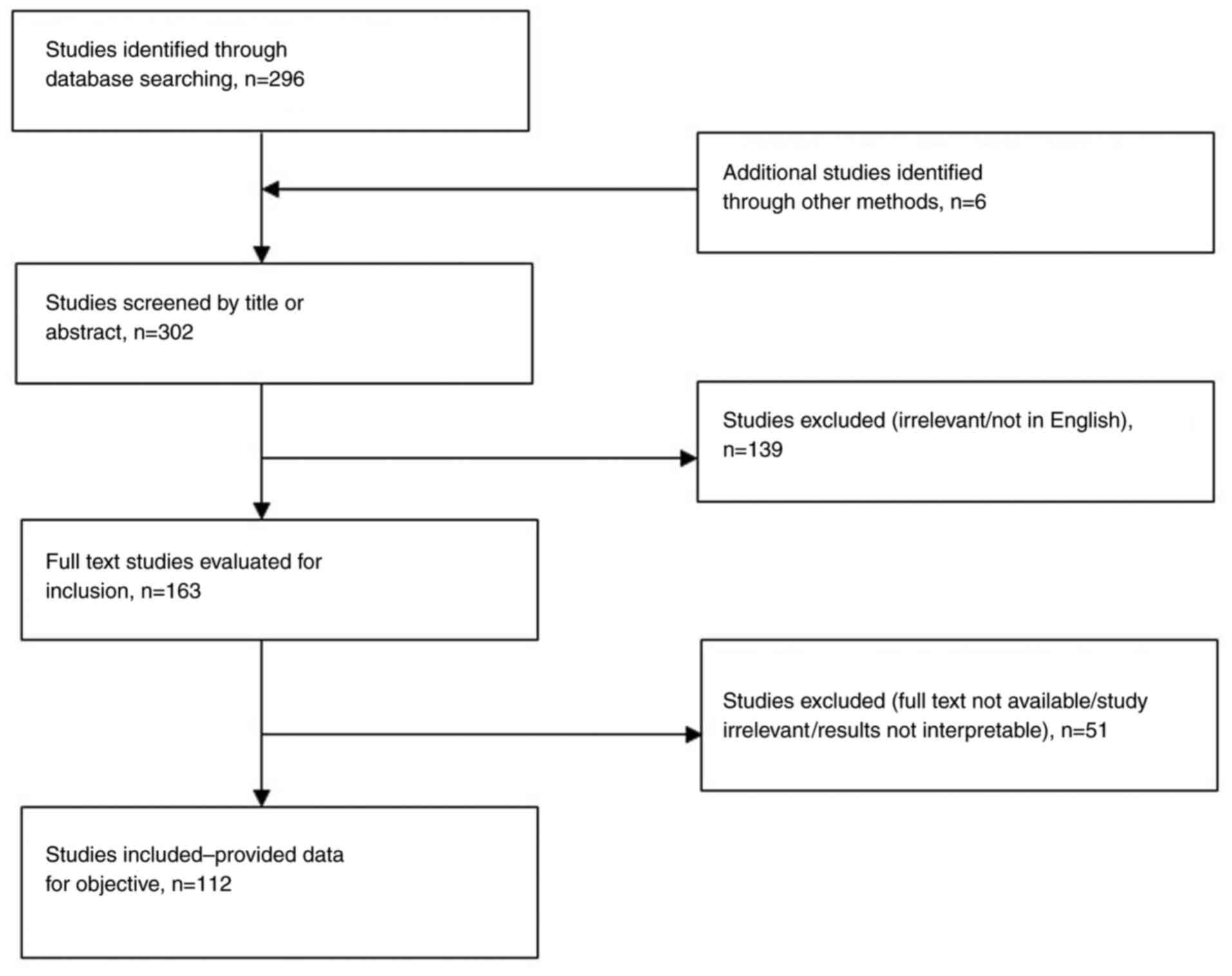
2. Materials and methods
The Cochrane (https://www.cochrane.org/), MEDLINE (https://www.nlm.nih.gov/) and EMBASE (https://www.embase.com/) databases were explored from
January 2000 to September 2023, using the terms ‘Clostridium
difficile neonates’, ‘Child, pediatric, Clostridium
difficile’; a total of 112 studies containing relevant data
were selected and checked. Studies were excluded if they were not
published in English or French, if the pediatric population was not
treated separately from the adult population or if the study did
not contain original data (Fig. 1).
Studies that included adult groups were also selected for the
pathogenesis and epidemiology chapter.
3. Epidemiology
C. difficile
is a Gram-positive anaerobic bacterium that can
exist in both toxigenic and non-toxigenic form (8). It is widespread in the natural
environment, in human and animal feces and is part of the normal
intestinal flora with the mode of transmission being fecal-oral or
by direct contact (9).
The epidemiology of C. difficile in children
is relatively unknown due to limited surveillance. Zilberberg et
al (10) reported that the
annual rate of pediatric hospitalization with CDI in the United
States increased from 7.24 to 12.8/10,000 hospitalizations between
1997 and 2006. Another multicenter study of 22 pediatric hospitals
in the United States found that the annual incidence of C.
difficile-associated disease in hospitalized children nearly
doubled over a five-year period (from 26 to 40 per 10,000
hospitalizations between 2001 and 2006) (11).
A study conducted between 2003 and 2012 revealed an
increase from 24 to 58 per 10,000 discharges per year in all age
groups, with the largest increases observed in patients >15
years of age (12). Most
importantly, an increase in the incidence of CDI is observed in
generally healthy children with no risk factors, such as recent
exposure to antimicrobial drugs or repeated hospitalizations
(1,13).
In Italy, a 5-year study (2014-2018) showed an
increase from 0.75 to 9.80 per 1,000 hospitalizations of patients
with community-acquired CDI (2).
A recent study including 23,052 children with C.
difficile in the United States identified a decrease in
hospitalized children, from 7.09 cases per 10,000 patients in 2013
to 4.89 cases per 10,000 patients in 2019. This decreasing trend is
secondary to a decrease in antibiotic prescribing in both community
and hospital settings, effective sterilization protocols, disease
prevention policies, decreased specific testing for C.
difficile, changing diagnostic algorithms over the past 10
years and increased recognition of C. difficile
colonization, especially in children <1 year of age (14).
Asymptomatic C. difficile colonization is
frequent in early childhood; the carrier rate is reported to be 1
to 84% in healthy newborns and infants (15), but it decreases to less than 5% by 8
years of age (6). The most likely
source in infants is environmental contamination rather than
maternal-fetal contamination (vaginal birth, premature rupture of
membranes and prior administration of antimicrobial agents) and is
favored by artificial feeding, gut immaturity and lack of
protective gut microbiota (1,9). The
gut of the newborn is sterile, but by 12 months of age, the gut of
the infant has a flora similar to that of an adult (16).
Although infants have high carrier rates, they
rarely develop clinical infection due to immunoglobulin fractions
in breast milk that inhibit the binding of toxin A to its
intestinal receptor, the absence in the newborn intestine of the
intestinal receptor that binds to toxin A of C. difficile
because of the immaturity of the intestinal mucosa and the nature
and composition of the infant gut microflora that protects against
C. difficile overgrowth (6,17).
Although infant testing is not recommended, recent
data revealed that 26% of children hospitalized with CDI were
infants younger than 1-year-old and 5% were newborns. What cannot
be determined from this data is whether hospitalization rates for
CDI represent true disease or asymptomatic carriers (18).
According to most studies, the incidence of CDI in
children is increasing even in the community setting, similar to
adult cases, but the severity of cases has not increased (6,19).
This is due to a low percentage of cases with virulent North
American pulsed field type 1 (NAP1) strains in children, 19.4%
compared with >50% of cases in adults (20). This strain is characterized by
deletions of the tcdC gene, resistance to fluoroquinolones,
production of C. difficile transferase (CDT) or binary
toxin, intensive spore production and increased production of
toxins A and B (1,21). The detection of the NAP1 strain of
C. difficile is not possible in most laboratories and, in
most situations, it would not influence the clinical care of a
patient (16). Further studies are
needed to determine the role of the NAP1 strain in severe forms of
C. difficile infection in the pediatric population.
4. Risk factors
Recognized risk factors for older children that
acquire C. difficile have included the use of antibiotics
and proton pump inhibitors (PPIs) for prolonged periods,
immunosuppressive treatments, repeated enemas, the use of diapers,
prolonged nasogastric tube insertion, gastrointestinal tract
surgery, renal failure, the presence of IBD and impaired humoral
immunity (1,6,22).
A previous study of pediatric C. difficile
cases reported as risk factors the antibiotic treatment in 92% of
children, the immunosuppressive treatment in 60%, a malignancy or
organ transplant in 39%, while 13% had IBD (23). Among the antibiotics, the most
commonly associated with increased risk of C. difficile
infection are the combinations of antibiotics, cephalosporins,
fluoroquinolones, penicillins, carbapenems and cotrimoxazole
(14).
While a study conducted in 2020 found that
clindamycin is associated with higher odds of community-acquired
CDI in pediatrics [odds ratio (OR), 14.9; 95% confidence interval
(CI), 5.2-42.3], followed by amoxicillin-clavulanate (OR, 2.2; 95%
CI, 1.2-3.9) and cephalosporin (OR, 2; 95% CI, 1.1-3.6) (22), a different study reported an
association between community-acquired CDI and cephalosporins (OR,
1.95; 95% CI, 0.68-4.95; P=0.16), exposure to clindamycin (OR,
2.70; 95% CI, 0.70-10.39; P=0.15) and the presence of a
gastrointestinal feeding device (OR, 2.27; 95% CI, 0.92-5.60;
P=0.08) (24), while a study
conducted by Adams et al (25) reported an association between
community-acquired CDI and clindamycin (OR, 73.00; 95% CI,
13.85-384.68) and third-generation cephalosporins (OR, 16.32; 95%
CI, 9.11-29.26).
Chemotherapy is associated with an increased risk of
CDI, possibly due to the antimicrobial properties of
chemotherapeutic agents, the effects of immunosuppression and
neutropenia, and changes in intestinal mucosa (26). Hypogammaglobulinemia is also
associated with an increased risk of CDI.
While a number of studies suggest that drugs that
suppress gastric acidity, particularly PPIs (27), cause the alteration of the gut
microbiota, allowing pathogens including C. difficile to
increase, in a previous pediatric study the H2 receptor antagonists
have actually been associated with decreased colonization by C.
difficile (28).
The presence of frequent and prolonged
hospitalizations among children with C. difficile is
highlighted by numerous studies; this is due to the exposure to an
environmental reservoir of C. difficile, with the possible
transmission of this pathogen, and is indirectly associated with
other risk factors such as the use of antibiotics and PPIs
(1).
Inflammation of the intestinal epithelium secondary
to viral gastroenteritis (noroviruses and caliciviruses), may
facilitate adhesion and colonization by C. difficile and the
occurrence of infection (1).
Comorbidities (especially chronic gastrointestinal
and neurological diseases) are associated with CDI, due to the
numerous associated risk factors that trigger disturbances of the
gut microbiota such as: i) Prolonged hospitalization, ii) the use
of antibiotics or PPIs and iii) immunosuppression (1,29).
Thus, according to studies, IBD (OR, 3.72; 95% CI, 1.52-9.12),
renal failure (OR, 2.64; 95% CI, 1.23-5.68), hematologic cancer
(OR, 1.75; 95% CI, 1.02-5.68) and diabetes mellitus (OR, 1.15; 95%
CI, 1.05-1.27) were associated with CDI (30). A study conducted in 2018
demonstrated that other conditions identified as risk factors for
CDI included coagulopathy (OR, 3.07; 95% CI, 1.34-7.06), pneumonia
(OR, 2.37; 95% CI, 1.73-3.25), female pelvic infection (OR, 2.01;
95% CI 1.21-3.37), IBD (OR, 1.96; 95% CI, 1.36-2.81), irritable
bowel syndrome (OR, 1.66; 95% CI, 1.23-2.24), iron deficiency
anemia (OR, 1.55; 95% CI, 1.02-2.33), viral infections (OR, 1.51;
95% CI, 1.06-2.15), depression (OR, 1.45; 95% CI, 1.06-1.98) and
stroke (OR 1.43, 95% CI 1.00-2.03) (31).
5. Pathogenesis
The incubation period from exposure to onset of
symptomatic CDI (CSI) is two to three days. The reservoir for C.
difficile spores is represented by toilets, furniture in the
clinic, telephones and medical devices (thermometers,
stethoscopes).
Important pathophysiological characteristics of
C. difficile include the resistance to heat of the spore
(which allows its persistence in the environment for several
months), the resistance to acids, antibiotics and the production of
toxins (28).
Once in the gut, bile acids play an important role
in inducing the germination of C. difficile spores (1). Colonization does not necessarily mean
symptomatic infection, only 25-30% of asymptomatic colonized
patients develop diarrhea (32).
The microbial intestinal ecosystem, rich in the
anaerobic Bacteroides and Firmicutes species, plays
an important role in the regulation of host physiology, especially
in the defense against pathogens, in the stimulation of
angiogenesis or in the nutrition process (1).
C. difficile begins to dominate and colonize
the large intestine when the balance of intestinal microorganisms
is disturbed, which is the first step of infection.
C. difficile is not invasive, virulence is
due mainly to enzymes such as collagenase, hyaluronidase,
chondroitin sulfatase, as well as toxins A and B, which damage the
cytoskeleton of epithelial cells, leading to disruption of tight
junctions and loss of mucosal functionality (32). Toxin A (enterotoxin) can disrupt
neuronal function and cause aberrant calcium release (33). Toxin B (cytotoxin) exerts its effect
on white blood cells by altering neutrophil chemotaxis and
activating mast cells and macrophages, which leads to the release
of inflammatory mediators (26,33).
There is also a third toxin, CDT, a binary toxin that is produced
by certain C. difficile strains, including the PCR027
ribotypes, which theoretically could have clinical impact, however
its role is unclear. The end result of toxin activity in the gut is
fluid secretion, mucosal damage and interstitial inflammation
(1).
In more severe forms, microulcerations covered with
pseudo-membranes (composed of destroyed intestinal cells,
neutrophils and fibrin) begin to appear on the surface of the
intestinal mucosa (32).
6. Clinical picture
A case definition of CDI includes the presence of
symptoms (usually watery diarrhea) and either one stool test result
that is positive for C. difficile toxin or colonoscopy
findings demonstrating pseudomembranous colitis.
The clinical picture of CDI is very heterogeneous
and ranges from asymptomatic carrier state, mild or moderate
diarrhea, to fulminant life-threatening colitis (34). Although the incubation period is not
precisely defined, recent studies revealed that it is longer than 3
days and is highly dependent on the individual.
The symptomatic illness can be mild, moderate or
severe. The mild and moderate form is usually characterized by
watery diarrhea (<4 stools/day in the mild form and more in the
moderate form), low-grade fever and mild abdominal pain, without
phenomena of systemic toxicity. Other clinical manifestations
include nausea, weakness and loss of appetite. Fecal occult blood
testing is often positive, although active bleeding is rarely
present (32). The severe form
involves high fever, intense abdominal pain, abdominal distension,
vomiting food, numerous watery stools with mucus and blood leading
to significant dehydration, hypoalbuminemia with peripheral edema
and subsequent circulatory shock (32).
Other severe complications of CDI include toxic
megacolon, intestinal paralysis, small bowel infiltration, colonic
perforation, reactive arthritis, renal failure, systemic
inflammatory response syndrome, sepsis and death (35).
Complications are more likely to occur among
children with hematological malignancies or those treated with
hematopoietic stem cell transplantation, infants with
Hirschsprung's disease or patients with IBD (1).
The mortality rate due directly to CDI is estimated
at 5%, while mortality associated with complications reaches 15-25%
and up to 34% in intensive care units (32).
7. Diagnostic tests
The diagnosis of CDI is based on the association
between medical history, clinical presence of >3 semi-consistent
stools/24 h or bloody stools and laboratory tests (9). Because of the slow turnaround time,
isolation of the organism from stool is not a clinically useful
diagnostic test, nor is stool testing of asymptomatic patients.
Cell culture cytotoxicity neutralization assay
(CCCA) has been replaced by more sensitive diagnostics, the most
common test method used today for C. difficile toxins is the
enzyme immunoassay (EIA), which detects toxins A and/or B. It is
preferred due to the rapid turnaround time, the ease of testing and
the high specificity (1).
Detection of glutamine dehydrogenase, an antigen
present on C. difficile, although very sensitive, only
indicates the presence of the pathogen. It should only be used as
part of a 2-step algorithm, with confirmation of positive results
using either an EIA for toxin A/B or a CCCA.
Molecular tests using nucleic acid amplification
tests (NAATs) are now preferred by numerous laboratories because
they have high sensitivity and specificity, comparable turnaround
times to EIA and do not need to be part of a 2- or 3-step algorithm
(14). In a previous study, the
sensitivities of PCR tests with high sensitivity and specificity
for toxins A and B compared with the EIA test were higher (95 vs.
35%, respectively), and the specificity was equal to 100% (36). Using PCR tests, positivity rates for
stool samples doubled, from 7.9 to 8.3% with EIA and from 14.9 to
18.1% with PCR (9).
Stool testing in newborns and infants <1 year of
age is not recommended except in the presence of risk factors such
as Hirschsprung-associated enterocolitis or primary
immunodeficiency, surgery on the gastrointestinal tract or the
presence of an infectious outbreak; the presence of C.
difficile is considered colonization (1). In children aged 1 to 2 years
presenting with diarrhea, testing for C. difficile may be
considered after testing for other causes of diarrhea, especially
viral infection. In children >2 years of age, testing is similar
to adult testing and is recommended for patients with prolonged or
worsening diarrhea, especially if combined with relevant risk
factors or exposures.
The presence of pseudo-membranes and hyperemic,
friable rectal mucosa on colonoscopy suggests pseudomembranous
colitis and establishes the diagnosis of CDI, regardless of the age
of the child (1,14).
Since C
difficile toxin excretion lasts up to 4 weeks
after healing, it is recommended that testing for possible relapse
has to be conducted later than 4 weeks after therapy, using the
more sensitive NAAT test (9).
8. Treatment
The treatment of CDI in children is based on
clinical data from adults and is determined by the number and
severity of episodes (37). The
therapeutic recommendations in CDI are the following: i) General
principles, ii) etiological treatment, iii) surgery, iv) supportive
treatment, v) fecal microbiota transplantation, vi) upcoming
treatment and vii) prevention.
General principles
It is very important to: Eliminate favoring factors
whenever possible (interruption of antibiotics and gastric
anti-secretory drugs); eliminate aggravating factors (no
administration of antiperistalsis drugs); initiate etiological
therapy and adopt measures in order to limit human transmission as
quickly as possible after the diagnostic suspicion has been
made.
Etiological treatment of the first
episode
For children with their first episode of mild to
moderate CDI, metronidazole and vancomycin are recommended, while
oral vancomycin is preferred over metronidazole for children with a
first episode of severe CDI (Table
I) (38).
 | Table ISummary of therapies for children
with Clostridium difficile infection. |
Table I
Summary of therapies for children
with Clostridium difficile infection.
| Initial
episode | |
|---|
| Mild to moderate
infection | Oral metronidazole
(7,5 mg/kg per dose-up to 500 mg qid) for 10 to 14 days |
| | Or |
| | Oral vancomycin (10
mg/kg per dose-up to 125 mg qid) for 10 days |
| Severe
infection | Oral vancomycin (10
mg/kg per dose-up to 500 mg qid) for 10 days |
| | ± |
| | Iv metronidazole
(10 mg/kg per dose-up to 500 mg tid) for 10 days (if ileus, toxic
megacolon, shock is present) |
| Recurrence | |
| First
recurrence | Oral metronidazole
(7,5 mg/kg per dose-up to 500 mg qid) for 10 to 14 days |
| | Or |
| | Oral vancomycin (10
mg/kg per dose-up to 125 mg qid) for 10 days |
| Second
recurrence | Oral vancomycin (10
mg/kg per dose-up to 125 mg qid) for 10 days (if not used
previously) |
| | Or |
| | Tapered or pulsed
regimens of vancomycin: |
| | Vancomycin 10 mg/kg
per dose qid (max 125 mg) for 10 days, followed by vancomycin 10
mg/kg per dose bid (max 125 mg) for 7 days followed by vancomycin
10 mg/kg per dose once daily (max 125 mg) for 7 days followed by
vancomycin 10 mg/kg per dose every 2 to 3 days (max 125 mg) for 2
to 8 weeks |
| Other options for
recurrent infection | Oral fidaxomicin
(16 mg/kg per dose-up to 400 mg bid) for 10 days |
| (more than 2
recurrences) | Fecal microbiota
transplantation |
| Progressive or
fulminant colitis | Surgery-colectomy
should be considered in such patients |
Metronidazole should be administered in a dose of
7,5 mg/kg three times a day orally; indicative duration: 10 days
(should not be extended to >14 days because of the increased
risk of neurotoxicity) (39); it is
no longer effective if the colonic inflammation has improved,
therefore it is not administered more than 3-4 days after the
remission of symptoms.
Vancomycin should be administered in a dose of 10
mg/kg every 6 h orally, for 10-14 days. In special situations such
as toxic megacolon or ileus, it is recommended to increase the
doses and administer simultaneously by several routes: Vancomycin
10 mg/kg every 6 h orally, to which vancomycin 10 mg/kg every 6-12
h by therapeutic enema (in 100-500 ml saline) should be added and
intravenous metronidazole 10 mg/kg every 8 h for 10 days.
In adults, based on the improved clinical cure rates
and lower recurrence risk, fidaxomicin and vancomycin are now
recommended as preferred first line therapies (40).
In children, there have recently been studies that
indicated an increase in the use of vancomycin to the detriment of
metronidazole (41). A study
published in 2020, which followed 192 patients with moderate CDI,
treated with oral metronidazole or oral vancomycin, concluded that
patients treated with vancomycin had a faster resolution of
symptoms, while recurrence at 12 weeks was similar in both groups
(42).
Fidaxomicin is a registered macrocyclic antibiotic
in clinical practice for the treatment of CDI, which achieves very
high fecal concentrations with minimal systemic absorption; a
previous study revealed that the efficacy of fidaxomicin is similar
to vancomycin and it is more active in vitro against C.
difficile strains including NAP1/BI/027(43). Moreover, it is effective at
achieving clinical cure and preventing recurrent infections and it
is well tolerated in pediatric patients (44). A multicenter Phase III SUNSHINE
study, which investigated the efficacy of fidaxomicin therapy in
pediatric patients with CDI, compared with oral vancomycin,
concluded that fidaxomicin is well tolerated and has an improved
sustained response rate than vancomycin at 30 days from the end of
the treatment (45).
Fidaxomicin is a newly United States FDA approved
option for treatment in children >6 months of age and who weigh
>4 kg; the weight-based dosing is 16 mg/kg per dose (max 200 mg
per dose), orally, twice daily for 10 days, available as tablets
and liquid formulations (46).
There is no proper treatment for the fulminant forms of
Clostridium infection, therefore additional studies are
needed to improve the prognosis in these forms (47).
Etiological treatment of relapses
For the first relapse, the guidelines recommend the
same options and doses as for the initial episode, oral
metronidazole or oral vancomycin in children.
Starting with the second relapse, patients may
benefit from tapering and pulsed oral vancomycin: 10 mg/kg every 6
h (max 125 mg) for 10 days; subsequently 10 mg/kg every 12 h (max
125 mg) for 7 days; then 10 mg/kg once daily (max 125 mg) for 7
days and finally 10 mg/kg every 2-3 days for 14-56 days (47).
Secondary prophylaxis with oral vancomycin in
pediatric patients with a history of CDI, while receiving systemic
antibiotics, may reduce the risk of recurrences (48).
Surgery
The criteria for surgical treatment are: Colon
perforations; a worsening of the condition of the patient despite
adequate drug therapy; toxic megacolon or severe ileus; the
occurrence of shock and CDI in the recovery period after a colonic
intervention.
The types of surgery are: Total or subtotal
colectomy with terminal ileostomy-preferred choice; less aggressive
interventions are rarer, in cases where total colectomy is not
accepted.
Effectiveness of the interventions: Reducing the
risk of death by 2-3 times, from 35-80 to 12-35%, if the
intervention takes place early, especially before the colon is
severely damaged; lactate <5 mmol/l and the number of white
blood cells <50,000/mm3 (49-50).
Supportive treatment must include hydro-electrolytic
rebalancing; correction of hypoproteinemia; prevention of deep
thrombosis and correction of organ dysfunctions.
Fecal microbiota transplantation
(FMT)
FMT is the process of implanting intestinal
microbiota, using a special filtration method, from a healthy donor
into the gastrointestinal tract of the patient, in order to restore
the intestinal flora of the recipient and help to achieve an
optimal function of the intestinal system. Delivery methods include
gastrostomy, colonoscopy, nasogastric tube, nasoduodenal catheters,
retention enema or capsule. FMT has demonstrated great efficacy in
the treatment of severe and recurrent CDI in adults (51), but in pediatric patients, the
implications of altering the microbiome at such an early age in
development raises numerous question marks and requires further
research.
In adults, after FMT there have been reports of
infectious and non-infectious complications, including the
development of flares of IBD, potential metabolic disorders or
nutritional deficiencies (51,52).
A multicenter retrospective study that included 335
pediatric and young adult patients (ages ranging from 11 months to
23 years), demonstrated the very favorable efficacy of FMT in the
treatment of CDI, with no episodes of recurrence in 81% of the
patients (51). Among the
independent predictors of FMT success, the use of fresh stool vs.
frozen stool, the lack of a feeding tube, delivery by colonoscopy
and a lower number of CDI episodes before FMT were identified. A
total of 4.7% of the patients had a severe adverse event during the
3-month follow-up period: Aspiration pneumonia, vomiting and
dehydration and inflammatory bowel syndrome flare.
FMT has been demonstrated to be relatively safe in
immunocompromised adult patients and patients with IBD, but the
long-term safety of FMT still needs to be established. Because of
that, the North American Society for Pediatric Gastroenterology,
Hepatology and Nutrition, as well as the European Society for
Gastroenterology, Hepatology and Nutrition recommend performing FMT
in established centers, where long-term side effects can be
monitored and which have rigorous donor screening (53).
Probiotics
No published guide recommends the use of probiotics
for the prevention or treatment of CDI in children, because of the
lack of the evidence (54).
Upcoming treatment
The Clinical Practice Guideline, issued by the
Infectious Diseases Society of America, recommends the use of
bezlotoxumab in addition to standard of care antibiotics for adult
patients with a recurrence of CDI within the past 6 months
(40). Bezlotoxumab is an IgG
monoclonal antibody against C. difficile that binds to toxin
B and neutralizes its effects on mammalian cells (55). It is not approved in patients under
18 years of age.
Recently, a multicenter, double-blind,
placebo-controlled study (MODIFY III) of bezlotoxumab in 111
children (between 1 and <18 years of age) receiving
antibacterial treatment for CDI, showed a safety profile similar to
that observed in studies in adults and was generally well tolerated
(56).
In adult patients with CDI, there are numerous
ongoing studies that follow clinical efficacy, pharmacokinetics,
pharmacodynamics, safety and tolerability of new molecules
including a DNA polymerase inhibitor (ibezapolstat) (57), ridinilazole (58) and a novel topoisomerase inhibitor
(59).
Prevention
The transmission of CDI occurs via the fecal-oral
route, through contact with the patient or patients in the
contaminated environment. Controlling the spread of C.
difficile into the environment is essential in healthcare
facilities.
Washing the hands with soap and water, the use of
gloves in symptomatic patients and decontamination using
chlorine-based products are measures that prevent the transmission
of CDI.
People with C. difficile-associated diarrhea
should be placed in isolation for the duration of treatment.
Given that exposure to antibiotics is the main risk
factor for CDI, programs to reduce inappropriate use of antibiotics
in children, especially in outpatient settings, need to be
implemented (47).
9. Conclusions
Although the incidence of CDI is not really known,
all data in the literature indicated an increase in community
cases. Clinicians should be more responsible for recommending
outpatient antibiotic therapy.
The diagnosis must take into account both the
presence of risk factors and the presence of clinical signs and
follow specific diagnostic testing algorithms. Further studies are
needed to evaluate different treatment strategies for children with
a poor response to classic treatment.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the RIPLU TARGOVISTE
S.R.L. (Targoviste, Romania) Research Grant of the University of
Medicine and Pharmacy of Craiova (grant no.
26/721/2/21.07.2023).
Availability of data and materials
Not applicable.
Authors' contributions
DD, IRM, VP, DCC, RP, SAN and CEN contributed
equally to the acquisition, analysis and systematization of the
data, manuscript writing and critical revision for important
intellectual content. All authors read and approved the final
version of the manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Borali E and De Giacomo C: Clostridium
difficile infection in children: A review. J Pediatr
Gastroenterol Nutr. 63:e130–e140. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Borali E, Ortisi G, Moretti C, Stacul EF,
Lipreri R, Gesu GP and De Giacomo C: Community-acquired
Clostridium difficile infection in children: A retrospective
study. Dig Liver Dis. 47:842–846. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ananthakrishnan AN: Clostridium
difficile infection: Epidemiology, risk factors and management.
Nat Rev Gastroenterol Hepatol. 8:17–26. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kuntz JL, Johnson ES, Raebel MA, Petrik
AF, Yang X, Thorp ML, Spindel SJ, Neil N and Smith DH: Epidemiology
and healthcare costs of incident Clostridium difficile
infections identified in the outpatient healthcare setting. Infect
Control Hosp Epidemiol. 33:1031–1038. 2012.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Rupnik M, Wilcox MH and Gerding DN:
Clostridium difficile infection: New developments in
epidemiology and pathogenesis. Nat Rev Microbiol. 7:526–536.
2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Shim JO: Clostridium difficile in
children: To treat or not to treat? Pediatr Gastroenterol Hepatol
Nutr. 17:80–84. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
van Dorp SM, Smajlović E, Knetsch CW,
Notermans DW, de Greeff SC and Kuijper EJ: Clinical and
microbiological characteristics of Clostridium difficile
infection among hospitalized children in the Netherlands. Clin
Infect Dis. 64:192–198. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lamont JT and Theodore E: Woodward award.
How bacterial enterotoxins work: Insights from in vivo studies.
Trans Am Clin Climatol Assoc. 113:167–180. 2002.PubMed/NCBI
|
|
9
|
Schutze GE and Willoughby RE: Committee on
infectious disease, American Academy of Pediatrics. Clostridium
difficile infection in infants and children. Pediatrics.
131:196–200. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zilberberg MD, Tillotson GS and McDonald
C: Clostridium difficile infections among hospitalized
children, United States, 1997-2006. Emerg Infect Dis. 16:604–609.
2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kim J, Smathers SA, Prasad P, Leckerman
KH, Coffin S and Zaoutis T: Epidemiological features of
Clostridium difficile-associated disease among inpatients at
children's hospitals in the United States, 2001-2006. Pediatrics.
122:1266–1270. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pant C, Deshpande A, Gilroy R, Olyaee M
and Donskey CJ: Rising incidence of Clostridium difficile
related discharges among hospitalized children in the United
States. Infect Control Hosp Epidemiol. 37:104–106. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sandora TJ, Fung M, Flaherty K, Helsing L,
Scanlon P, Potter-Bynoe G, Gidengil CA and Lee GM: Epidemiology and
risk factors for Clostridium difficile infection in
children. Pediatr Infect Dis J. 30:580–584. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Edwards PT, Thurm CW, Hall M, Busing JD,
Kahn SA, Kellermayer R, Kociolek LK, Oliva-Hemker MM, Sammons JS,
Weatherly M, et al: Clostridioides difficile infection in
hospitalized pediatric patients: Comparisons of epidemiology,
testing, and treatment from 2013 to 2019. J Pediatr.
252:111–116.e1. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bryant K and McDonald LC: Clostridium
difficile infections in children. Pediatr Infect Dis J.
28:145–146. 2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jangi S and Lamont JT: Asymptomatic
colonization by Clostridium difficile in infants:
Implications for disease in later life. J Pediatr Gastroenterol
Nutr. 51:2–7. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lees EA, Miyajima F, Pirmohamed M and
Carrol ED: The role of Clostridium difficile in the
paediatric and neonatal gut-a narrative review. Eur J Clin
Microbiol Infect Dis. 35:1047–1057. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Adams DJ, Barone JB and Nylund CM:
Community-associated Clostridioides difficile infection in
children: A review of recent literature. J Pediatric Infect Dis
Soc. 10 (Suppl_3):S22–S26. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nylund CM, Goudie A, Garza JM, Fairbrother
G and Cohen MB: Clostridium difficile infection in
hospitalized children in the United States. Arch Pediatr Adolesc
Med. 165:451–457. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Toltzis P, Kim J, Dul M, Zoltanski J,
Smathers S and Zaoutis T: Presence of the epidemic North American
Pulsed Field type 1 Clostridium difficile strain in
hospitalized children. J Pediatr. 154:607–608. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Loo VG, Poirier L, Miller MA, Oughton M,
Libman MD, Michaud S, Bourgault AM, Nguyen T, Frenette C, Kelly M,
et al: A predominantly clonal multi-institutional outbreak of
Clostridium difficile-associated diarrhea with high
morbidity and mortality. N Engl J Med. 353:2442–2449.
2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Miranda-Katz M, Parmar D, Dang R,
Alabaster A and Greenhow TL: Epidemiology and risk factors for
community associated clostridioides difficile in children. J
Pediatr. 221:99–106. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
El Feghaly RE, Stauber JL, Tarr PI and
Haslam DB: Viralco-infections are common and are associated with
high er bacterial burden in children with Clostridium
difficile infection. J Pediatr Gastroenterol Nutr. 57:813–816.
2013.
|
|
24
|
Crews JD, Anderson LR, Waller DK, Swartz
MD, DuPont HL and Starke JR: Risk Factors for Community-associated
Clostridium difficile-associated diarrhea in children.
Pediatr Infect Dis J. 34:919–923. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Adams DJ, Eberly MD, Rajnik M and Nylund
CM: Risk factors for community-associated Clostridium
difficile infection in children. J Pediatr. 186:105–109.
2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Allen UD: Canadian Paediatric Society,
Infectious Diseases, Immunization Committee. Clostridium
difficile in paediatric populations. Paediatr Child Health.
19:43–48. 2014.PubMed/NCBI
|
|
27
|
Dial S, Delaney JA, Barkun AN and Suisse
S: Use of gastric acid-suppressive agents and the risk of
community-acquired Clostridium difficile-associated disease.
JAMA. 294:2989–2995. 2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Rexach CE, Tang-Feldman Y, Cantrell MC and
Cohen SH: Epidemiologic surveillance of Clostridium
difficile diarrhea in a freestanding pediatric hospital and a
pediatric hospital at a university medical center. Diagn Microbiol
Infect Dis. 56:109–114. 2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sammons JS, Toltzis P and Zaoutis TE:
Clostridium difficile infection in children. JAMA Pediatr.
167:567–573. 2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Furuya-Kanamori L, Stone JC, Clark J,
McKenzie SJ, Yakob L, Paterson DL, Riley TV, Doi SA and Clements
AC: Comorbidities, exposure to medications, and the risk of
community-acquired Clostridium difficile Infection: A
systematic review and Meta-analysis. Infect Control Hosp Epidemiol.
36:132–141. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Oh SH and Kang HY: Identification of
target risk groups for population-based Clostridium
difficile infection prevention strategies using a population
attributable risk approach. Int J Infect Dis. 66:107–112.
2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Czepiel J, Dróżdż M, Pituch H, Kuijper EJ,
Perucki W, Mielimonka A, Goldman S, Wultańska D, Garlicki A and
Biesiada G: Clostridium difficile infection: Review. Eur J
Clin Microbiol Infect Dis. 38:1211–1221. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kelly CP and LaMont JT: Clostridium
difficile-more difficult than ever. N Engl J Med. 59:1932–1940.
2008.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Cohen SH, Gerding DN, Johnson S, Kelly CP,
Loo VG, McDonald LC, Pepin J and Wilcox MH: Society for Healthcare
Epidemiology of America; Infectious Diseases Society of America.
Clinical practice guidelines for Clostridium difficile
infection in adults: 2010 update by the Society for Healthcare
Epidemiology of America (SHEA) and the Infectious Diseases Society
of America (IDSA). Infect Control Hosp Epidemiol. 31:431–455.
2010.PubMed/NCBI View
Article : Google Scholar
|
|
35
|
McDonald LC, Gerding DN, Johnson S, Bakken
JS, Carroll KC, Coffin SE, Dubberke ER, Garey KW, Gould CV, Kelly
C, et al: Clinical practice guidelines for Clostridium
difficile infection in adults and children: 2017 update by the
Infectious Diseases Society of America (IDSA) and Society for
Healthcare Epidemiology of America (SHEA). Clin Infect Dis.
66:e1–e48. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Luna RA, Boyanton BL Jr, Mehta S, Courtney
EM, Webb CR, Revell PA and Versalovic J: Rapid stool-based
diagnosis of Clostridium difficile infection by real-time
PCR in a children's hospital. J Clin Microbiol. 49:851–857.
2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Li Z, Dong N, Hao J, Ouyang Z, Qiang C,
Yang Y, Mi C, Niu Y, Yang J, Wen B, et al: Clostridioides difficile
infection in infants: A case report and literature review. Gut
Pathog. 29(31)2023.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Gnocchi M, Gagliardi M, Gismondi P, Gaiani
F, De' Angelis GL and Esposito S: Updated Management guidelines for
clostridioides difficile in paediatrics. Pathogens.
9(291)2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Stanescu GL, Nedelcuta RM, Dop D, Diaconu
R, Calin G, Niculescu EC, Gheonea C, Stanescu R, Anghelina L and
Stanescu MR: Brain abscess of unknown etiology in a 2-year-old
child: A case report. Rom J Morphol Embryol. 56:1201–1204.
2015.PubMed/NCBI
|
|
40
|
Johnson S, Lavergne V, Skinner AM,
Gonzales-Luna AJ, Garey KW, Kelly CP and Wilcox MH: Clinical
practice guideline by the Infectious Diseases Society of America
(IDSA) and Society for Healthcare Epidemiology of America (SHEA):
2021 focused update guidelines on management of Clostridioides
difficile infection in adults. Clin Infect Dis. 73:e1029–e1044.
2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Stultz JS, Hopp J, Orndahl CM, Omecene NE
and Pakyz AL: Changes in metronidazole and vancomycin utilization
for nonsevere Clostridioides difficile infection among institutions
caring for children. Pediatr Infect Dis J. 40:634–636.
2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Yin J, Kociolek LK, Same RG, Hsu AJ, Amoah
J and Tamma PD: Oral vancomycin may be associated with earlier
symptom resolution than metronidazole for hospitalized children
with nonsevere Clostridiodes difficile infections. Open Forum
Infect Dis. 6(ofz492)2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Cornely OA, Crook DW, Esposito R, Poirier
A, Somero MS, Weiss K, Sears P and Gorbach S: OPT-80-004 Clinical
Study Group. Fidaxomicin versus vancomycin for infection with
Clostridium difficile in Europe, Canada, and the USA: A
double-blind, non-inferiority, randomised controlled trial. Lancet
Infect Dis. 12:281–289. 2012.PubMed/NCBI View Article : Google Scholar
|
|
44
|
D'Ostroph AR and So TY: Treatment of
pediatric Clostridium difficile infection: A review on
treatment efficacy and economic value. Infect Drug Resist.
10:365–375. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Wolf J, Kalocsai K, Fortuny C, Lazar S,
Bosis S, Korczowski B, Petit A, Bradford D, Croos-Dabrera R, Incera
E, et al: Safety and efficacy of fidaxomicin and vancomycin in
children and adolescents with Clostridioides (Clostridium)
difficile infection: A phase 3, multicenter, randomized,
single-blind clinical trial (SUNSHINE). Clin Infect Dis.
71:2581–2588. 2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Food and Drug Administration: DIFICID.
(Fidaxomicin) [package insert]. Whitehouse Station, NJ, Merck,
2020.
|
|
47
|
Shirley DA, Tornel W, Warren CA and Moonah
S: Clostridioides difficile infection in children: Recent updates
on epidemiology, diagnosis, therapy. Pediatrics.
152(e2023062307)2023.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Bao H, Lighter J, Dubrovskaya Y, Merchan
C, Siegfried J, Papadopoulos J and Jen SP: Oral vancomycin as
secondary prophylaxis for Clostridioides difficile infection.
Pediatrics. 148(e2020031807)2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Lamontagne F, Labbé AC, Haeck O, Lesur O,
Lalancette M, Patino C, Leblanc M, Laverdière M and Pépin J: Impact
of emergency colectomy on survival of patients with fulminant
Clostridium difficile colitis during an epidemic caused by a
hypervirulent strain. Ann Surg. 245:267–272. 2007.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Olivas AD, Umanskiy K, Zuckerbraun B and
Alverdy JC: Avoiding colectomy during surgical management of
fulminant Clostridium difficile colitis. Surg Infect
(Larchmt). 11:299–305. 2010.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Nicholson MR, Mitchell PD, Alexander E,
Ballal S, Bartlett M, Becker P, Davidovics Z, Docktor M, Dole M,
Felix G, et al: Efficacy of fecal microbiota transplantation for
Clostridium difficile infection in children. Clin
Gastroenterol Hepatol. 18:612–619.e1. 2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Shin JH, Chaplin AS, Hays RA, Kolling GL,
Vance S, Guerrant RL, Archbald-Pannone L and Warren CA: Outcomes of
a multidisciplinary clinic in evaluating recurrent Clostridioides
difficile infection patients for fecal microbiota transplant: A
retrospective cohort analysis. J Clin Med. 8(1036)2019.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Davidovics ZH, Michail S, Nicholson MR,
Kociolek LK, Pai N, Hansen R, Schwerd T, Maspons A, Shamir R,
Szajewska H, et al: Fecal microbiota transplantation for recurrent
Clostridium difficile infection and other conditions in
children: A joint position paper from the North American Society
for Pediatric Gastroenterology, Hepatology, and Nutrition and the
European Society for Pediatric Gastroenterology, Hepatology, and
Nutrition. J Pediatr Gastroenterol Nutr. 68:130–143.
2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Malhotra S and Mohandas S: Updates and
opinions in diagnosis and treatment of clostridiodes difficile in
pediatrics. Curr Treat Options Peds. 7:203–216. 2021.
|
|
55
|
Gerding DN, Kelly CP, Rahav G, Lee C,
Dubberke ER, Kumar PN, Yacyshyn B, Kao D, Eves K, Ellison MC, et
al: Bezlotoxumab for prevention of recurrent Clostridium
difficile infection in patients at increased risk for
recurrence. Clin Infect Dis. 67:649–656. 2018.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Sferra TJ, Merta T, Neely M, Murta de
Oliveira C, Lassaletta A, Fortuny Guasch C, Dorr MB, Winchell G, Su
FH, Perko S, et al: Double-blind, placebo-controlled study of
bezlotoxumab in children receiving antibacterial treatment for
clostridioides difficile infection (MODIFY III). J Pediatric Infect
Dis Soc. 12:334–341. 2023.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Garey KW, McPherson J, Dinh AQ, Hu C, Jo
J, Wang W, Lancaster CK, Gonzales-Luna AJ, Loveall C, Begum K, et
al: Efficacy, safety, pharmacokinetics, and microbiome changes of
ibezapolstat in adults with Clostridioides difficile infection: A
phase 2a multicenter clinical trial. Clin Infect Dis. 75:1164–1170.
2022.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Carlson TJ, Endres BT, Bassères E,
Gonzales-Luna AJ and Garey KW: Ridinilazole for the treatment of
Clostridioides difficile infection. Expert Opin Investig Drugs.
28:303–310. 2019.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Hind C, Clifford M, Woolley C, Harmer J,
McGee LMC, Tyson-Hirst I, Tait HJ, Brooke DP, Dancer SJ, Hunter IS,
et al: Insights into the spectrum of activity and mechanism of
action of MGB-BP-3. ACS Infect Dis. 8:2552–2563. 2022.PubMed/NCBI View Article : Google Scholar
|