Introduction
Bone metastases are a frequent problem in patients
affected by cancer, and the oncological treatment of these tumors
includes surgery, radiotherapy and chemotherapy. The spine is the
most common site of tumor metastasis, and metastatic tumors of the
spine are a common type of malignant spinal tumors. In total,
12–20% of patients with malignant tumor initially showed
characteristics of spinal metastasis (1). In particular, surgery is indicated in
cases of spinal instability, cord compression, failure of previous
radiotherapy and when the diagnosis is in doubt. In recent years,
with the development of operation and spinal reconstruction
technology, the operation treatment of vertebral metastases
strategy emphasize that based on the specific metastasis position,
nerve compression and decompression should be directly performed in
these positions, and should perform spinal stability reconstruction
(1). Posterior vertebral column
resection is an effective technique that has been widely applied to
treat severe rigid spinal deformities and tumors (2–4). The
surgery is able to radically resect the regional lesions; however,
it requires complex skills, and the associated complications should
not be neglected. The majority of previous studies (5–7) have
focused on the efficacy of this surgery, omitting any systemic
review of the complications. The present study summarizes the
complications of 40 consecutive cases of posterior vertebral column
resection and systematically analyses the complications of this
procedure in 40 patients with spinal tumors.
Patients and methods
Patient characteristics
Patients who underwent routine vertebral column
resection were included in this retrospective study. The inclusion
criteria were as follows: Patients were aged ≥18 years and had a
diagnosis of primary, secondary or metastatic spinal tumor. The
exclusion criteria were patients who: i) were not surgical
candidates for spine tumor removal, as determined by the surgical
team; ii) had undergone previous spinal surgery for tumor removal;
iii) in the opinion of the investigator may not have been able to
comply with the safety monitoring requirements of the study.
The study was approved by the ethics committee of
the Peking Union Medical College Hospital (Beijing, China). The
ethics committee approved the associated treatment, data collection
and follow-up of these patients. Written informed consent was
obtained from all the subjects between August 2005 and December
2011.
Surgical procedure
Briefly, following general anesthesia, the patients
were placed in a prone position. A mid-line linear incision was
created and the ligamentous attachments and muscle were dissected
to the tips of the transverse process over the levels of
decompression and posterior fixation. During the process, great
care was taken to avoid the transmission of pressure to the spinal
cord.
In the thoracic spine, a bilateral
costotransversectomy of 5–6 cm of the medial ribs associated with
the resection level was performed. Resections were later performed
either piecemeal or en bloc. The pleura were protected carefully.
The dura was cautiously elevated posteriorly, and the epidural
veins were pre-cauterized by bipolar cautery. The lateral cortex of
the vertebra was then exposed by blunt dissection. A pre-contoured
rod was connected to the screws on the opposite side to stabilize
the spine prior to removing the vertebral body. Osteotomies were
used to remove the vertebral body along the cartilage endplate. A
bone knife or wire saw was used to cut off the vertebral pedicle.
The upper and lower discs, including the cartilage endplate, were
completely removed until the resected bone was exposed, and the
other side of the vertebra was then removed using the same
procedure. Subsequently, anterior reconstruction with a titanium
mesh cage or artificial vertebral body was used for vertebral body
replacement. Posterolateral fusion was performed, and during the
surgical process, controlled hypotension was used and the vertebra
was resected as quickly as possible to minimise blood loss.
Postoperative management
Antibiotics were infused intravenously between the
first and third postoperative days (the duration was normally
limited to 48 h but was prolonged to six days in one case due to
pneumonia). The drainage was removed within 24–48 h after the
surgery. The patients were allowed to sit up and gradually walk
three days after the surgery with a brace. If the patient recovered
well, the brace was removed 24 weeks after the surgery.
Outcome assessment
The intra- and postoperative complications, resected
segment, duration of surgery, intraoperative blood loss,
transfusion volume, serum levels of hemoglobin and platelets
between post- and preoperation, preoperational pulmonary function
test results, postoperative liver and renal function, and timing of
extubation were recorded. Estimated blood loss was recorded at the
end of the surgery by a single staff member from the anesthesia
department. An X-ray was applied to evaluate the subsidence and
excursion of the replaced spinal segment. In the present study the
complications were classified as major or minor (8). Major complications were those that
may affect or change the expected recovery, and the others were
designated as minor complications. The complications were
classified as intraoperative and early and late postoperative.
Early complications were those occurring within the first 30 days
after surgery, and late complications were those occurring after 30
days. These three types of complications were further classified as
major or minor.
Statistical analysis
Normally distributed continuous data are presented
as the mean ± standard deviation and were compared using Student’s
t-tests. Non-normally distributed continuous data were compared
using the Mann-Whitney U test. Qualitative data are expressed as
frequencies and percentages. The Fisher’s exact or χ2
tests were used to examine the correlations between the qualitative
variables. Differences were considered statistically significant
when P<0.05. SPSS software version 12.0 (SPSS, Inc., Chicago,
IL, USA) was used to conduct the data analysis.
Results
Patient information
A total of 22 males and 18 females were selected for
inclusion in the present study. The median age of these patients
was 52 years (range, 20–78 years). Primary bone tumors accounted
for 13 cases (32.5%) and metastatic lesions in bone for 27 cases
(67.5%). A total of 40 tumors were detected through X-ray or
magnetic resonance imaging examination. Representative images are
shown in Fig. 1. It was observed
that 10 tumors were located at the lumbar vertebrae and the
remaining 30 tumors were located at the thoracic vertebrae.
Two adjacent thoracic vertebrae were resected in
four patients, and single vertebral resection was performed in the
other patients. No cases of mortality occurred, but two cases
survived for <6 months. The neurological function of the
patients was evaluated pre- and postoperatively using the five-tier
Frankel grading scale (9). One
patient exhibited complete motor and sensory loss (Frankel Grade
A); two had complete motor loss with some sensation preserved
(Frankel Grade B); 22 had an incomplete loss of motor function
(including three patients of Frankel Grade C and 19 of Frankel
Grade D) and 15 retained normal motor and sensory functions
(Frankel Grade E).
Duration of surgery, blood transfusion
and follow-up period
The ranges and medians of these parameters were as
follows: Duration of surgery, range 135–470 min and mean±standard
deviation, 305.8±78.2 min; blood loss volume, range 600–11,000 ml,
median 2,400 ml; blood transfusion volume, range 0–26,200 ml,
median 2,600 ml; and follow-up time, range 4–78 months, median 14
months.
Intraoperative and early and late
postoperative complications
A total of two major and 34 minor complications
occurred (Table I). The
intraoperative and early and late postoperative complications
included: two cases of intraoperative cerebral-spinal leakage; 10
of transient thrombocytopenia; one, acute renal failure and liver
dysfunction; one of drainage tube retention due to allergy to the
allograft bone with the allergy being controlled following the
administration of anti-allergic drugs; one of infective shock due
to pneumonia (a major complication); five of late tracheal
extubation; two of hemothorax; one of pneumothorax; one of acute
enteritis; one of transient cardiac ischemia following surgery; six
of hardware subsidence; one of regional recurrence (a major
complication, Fig. 2); and two
patients who expected to ambulate normally following surgery but
the Frankel grade was still C postoperatively, thus they felt
dissatisfied with the limited motor function improvement.
 | Table IClassification and types of
complications. |
Table I
Classification and types of
complications.
| Classification | Complication | n |
|---|
| Intraoperative |
| Major | – | 0 |
| Minor | Cerebral-spinal
leakage | 2 |
| Early
postoperative |
| Major | Infective shock | 1 |
| Minor | Acute liver
dysfunction and renal failure | 1 |
| Drainage tube
retention | 1 |
| Late tracheal
extubation | 5 |
| Transient
thrombocytopenia | 10 |
| Hemothorax | 2 |
| Pneumothorax | 1 |
| Acute enteritis | 1 |
| Transient cardiac
ischemia | 1 |
| Dissatisfied with the
limited motor function improvement | 2 |
| Late
postoperative |
| Major | Regional
recurrence | 1 |
| Minor | Hardware
subsidence | 6 |
Late tracheal extubation is associated
with higher intraoperative bleeding volume, and lower preoperative
forced vital capacity (FVC) and forced expiratory volume in 1 sec
(FEV1%)
The parameters that could result in late tracheal
extubation following surgery were analyzed. The Mann-Whitney U test
indicated that transient late tracheal extubation was associated
with a higher intraoperative bleeding volume (Z=−2.367, P=0.018;
Table II). The Student’s t-test
indicated that late tracheal extubation was associated with lower
preoperative FVC (t=2.864, P=0.007) and FEV1% (t=2.563, P=0.015;
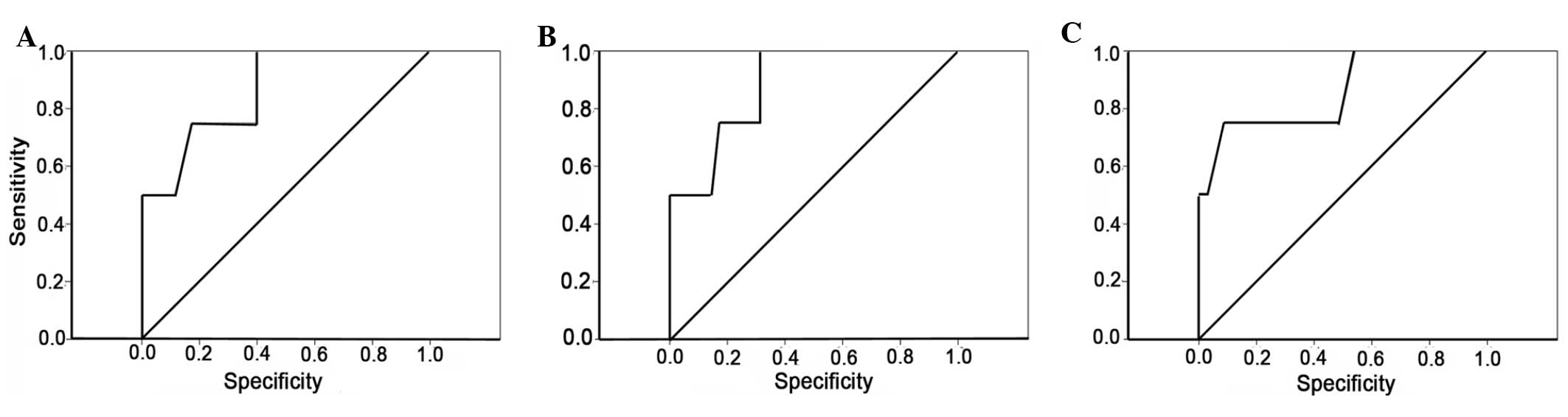
Table III). A receiver operating
characteristic (ROC) curve was drawn to analyze the correlation of
late tracheal extubation with blood loss and preoperative FVC and
FEV1% (Fig. 3).
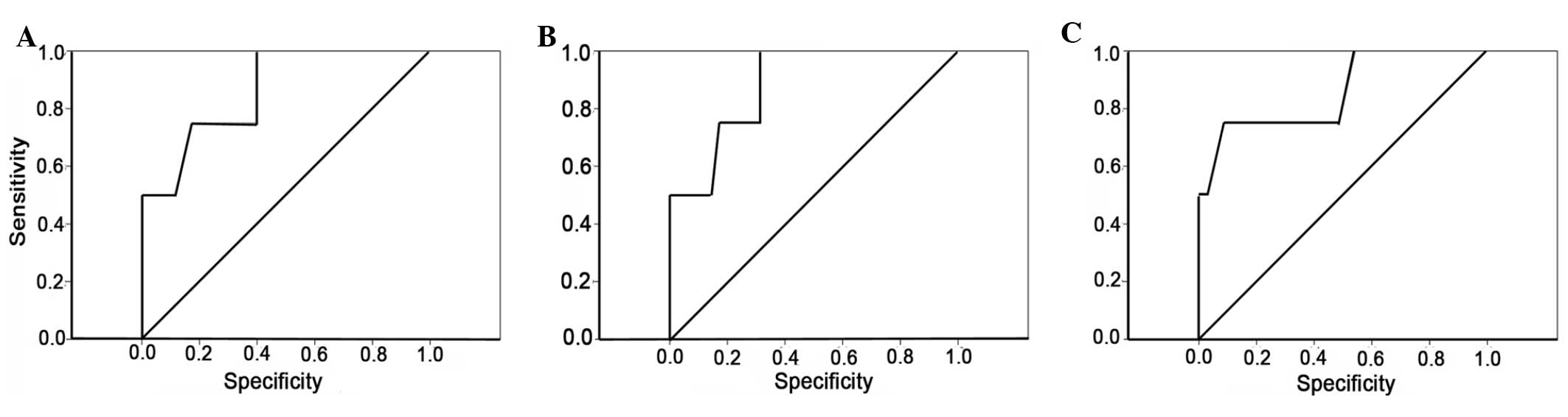 | Figure 3Receiver operating characteristic
curves of intraoperative bleeding volume, FVC and FEV1% for late
tracheal extubation. The highest diagnostic values and clinical
significance were as follows: (A) When the blood loss was >4,100
ml, sensitivity and specificity were 75 and 82.9.2%, respectively;
(B) when the preoperative FVC was <77.45, sensitivity and
specificity were 100 and 68.6%, respectively. (C) when the
preoperative FEV1% was <63.4, sensitivity and specificity were
75 and 91.4%, respectively. FVC, forced vital capacity; FEV1%,
forced expiratory volume in 1 sec. |
 | Table IICorrelation of late tracheal
extubation with intraoperative bleeding volume. |
Table II
Correlation of late tracheal
extubation with intraoperative bleeding volume.
| Tracheal extubation
timing | Mean intraoperative
bleeding volume, ml (range) |
|---|
| Late | 7500
(3200–10750) |
| Normal | 2000 (1500–3200) |
 | Table IIICorrelation of late tracheal
extubation with preoperative FVC and FEV1%. |
Table III
Correlation of late tracheal
extubation with preoperative FVC and FEV1%.
| Parameter | FVC | FEV1% |
|---|
| Late tracheal
extubation | 59.00±12.35 | 61.65±14.54 |
| Normal tracheal
extubation | 80.26±14.20 | 80.91±14.21 |
| t-value | 2.864 | 2.563 |
| P-value | 0.007 | 0.015 |
Replaced spinal segment subsidence is
associated with longer duration of surgery
The Mann-Whitney U test indicated that hardware
subsidence was associated with increased duration of surgery
(Z=−2.158, P=0.031), intraoperative bleeding volume (Z=−2.895,
P=0.004) and total blood transfusion volume (Z=−3.295, P=0.001,
Table IV); and that
thrombocytopenia was associated with increased operation duration
(Z=−2.719, P=0.007) and total blood transfusion volume (Z=−2.273,
P=0.023, Table V). The other
factors were not statistically associated with late tracheal
extubation, hardware subsidence and transient thrombocytopenia.
 | Table IVCorrelation of replaced spinal segment
subsidence with duration of surgery, intraoperative bleeding volume
and total blood transfusion volume. |
Table IV
Correlation of replaced spinal segment
subsidence with duration of surgery, intraoperative bleeding volume
and total blood transfusion volume.
| Parameter | Surgery duration, min
(range) | Intraoperative
bleeding volume, ml (range) | Total blood
transfusion volume, ml (range) |
|---|
| With subsidence | 380
(281.3–418.8) | 6600 (2575–9550) | 6700 (3250–9950) |
| Without
subsidence | 295
(245.0–335.0) | 2000 (1300–3000) | 2400 (1200–3600) |
| Z | −2.158 | −2.895 | −3.295 |
| P-value | 0.031 | 0.004 | 0.001 |
 | Table VCorrelation of thrombocytopenia with
duration of surgery and total blood transfusion volume. |
Table V
Correlation of thrombocytopenia with
duration of surgery and total blood transfusion volume.
| Parameter | Duration of surgery,
min (range) | Total blood
transfusion volume, ml (range) |
|---|
| Thrombocytopenia | 380.0
(282.5–436.3) | 3700 (2800–6800) |
| No
thrombocytopenia | 290.0
(242.5–330) | 2400 (1200–3800) |
| Z | −2.719 | −2.273 |
| P-value | 0.007 | 0.023 |
Discussion
Previous studies have demonstrated that the general
incidence of complications of spinal surgery is relatively high
(10–12). The posterior vertebral column
resection for spinal tumors is a widely used approach. The surgery
requires the performing of extralesional or en bloc resection;
therefore, additional anatomical structures may be resected
(13), including the thoracic
pleura, dura, muscle, nerve root and vessels. The resection may
lead to a higher incidence of complications. En bloc resection may
decrease tumor spread and recurrence; however, it is highly
skillful and time-consuming, requiring the separation of the
lateral and front sides of the vertebral body, bisection of the
intervertebral disc and removal of the vertebrae surrounding the
spinal cord. This surgery takes time to avoid causing injuries to
the blood vessels and nerve roots; however, the incidence of nerve
root stretching is high. Piecemeal resection removes the lesion
gradually, and the individual performing the surgery is able to
observe the front of the vertebra directly (14); therefore, the incidence of injuries
of the vessels and nerves is relatively low. Since en bloc
resection is highly challenging and risky, it should be performed
with caution in appropriate patients, and certain associated
factors should be considered, including the general condition,
Tomita score, Weinstein-Boriani-Biagini stage, metastatic lesions
and survival time. If the patient is not able to tolerate vertebral
column resection, or the life expectancy is less than half a year,
posterior or anterior decompression is a preferable option.
One case of pneumonia-induced shock occurred in the
present study, in which the patient was old, exhibited poor general
condition, had a long time of bed rest and were unable to
expectorate. The shock was induced by pneumonia and was finally
cured following active treatment. This indicates that it is
necessary to avoid and manage pulmonary complications particularly
for elderly patients who are weak and require a long period of bed
rest (15).
FVC was used to evaluate the pulmonary volume and
airway resistance. The FEV1% represents the proportion of the vital
capacity that an individual is able to expire in the first second
of expiration. In clinical practice, obstruction is defined as an
FEV1% <70%. Although no chronic obstructive pulmonary disease or
asthma was diagnosed in the present study, poor pulmonary function
may decrease the compensation ability of the lungs and cause late
tracheal extubation.
In the present study, the blood loss associated with
the vertebral column resection was relatively high. This may have
affected the hemodynamic stability. The statistical analysis
revealed that late tracheal extubation was associated with the
increase of blood loss, which indicated that an excessive discharge
of blood could affect the oxygen supply of the patients. There were
four cases of late tracheal extubation with a 2 h delay following
surgery and one case with a 24 h delay, for whom the blood loss
volume reached 11,000 ml. In addition, the ROC curve indicated that
when the blood loss was >4,100 ml, the blood oxygen level should
be monitored, which may lead to late tracheal extubation.
In addition, transient thrombocytopenia was found in
10 patients in this study, and the statistical analysis indicated
that this was associated with an increased duration of surgery and
total transfusion volume. No explanation for this connection has
been found in the literature; however, one conclusion is that this
may be caused by blood dilution following the application of a
large amount of colloidal solution during the long surgery. Higher
total transfusion volume also indicates that these patients
required greater amounts of colloidal solution. Following the
transfusion of red blood cells and plasma, the platelet count is
likely to recover within three days, which should not affect the
prognosis.
Hemodynamic disturbances may lead to transient
ischemia of the vital organs. Thus, it may be speculated that the
following complications were due to this cause: one case of cardiac
ischemia, one case of liver dysfunction and one case of renal
dysfunction. Since the renal dysfunction existed prior to the
surgery, it was difficult to clarify the correlation with blood
loss. Due to the limited number of samples, statistical analysis
was not available. In addition, the blood loss of giant cell
carcinomas was significantly higher than that of other tumors,
indicating that the type of tumor may be associated with the level
of blood loss.
Careful intraoperative manipulations and good
protection of the surrounding tissues could avoid life-threatening
complications, including inferior vena cava injuries (16). Two cases of cerebrospinal leakage
occurred in the present study, and instant repair was performed.
The drainage tube was subsequently removed 72 h after the surgery
and the wound healed well without infection. Boriani et al
(16) reported that delayed aortic
dissection may be caused by the severe adherence of the aorta with
the tumor. However, timely treatment, such as with aortic bypass
surgery, may prevent this complication. Orthopedists should
therefore be aware of the possible severe complications induced by
intraoperative injuries of the surrounding tissues and ensure that
they treat these problems in a timely manner.
The incidence of hemothorax is relatively lower in
posterior compared with anterior surgeries. Hemothorax may be
caused by a number of factors (17), including the inappropriate
positioning of hooks and screws, which may penetrate the lungs and
blood vessels, or the ribs penetrating the lungs and blood vessels
during thoracoplasty, or occasionally the central venous
catheterization may also penetrate the lungs and vessels (18). However, hemothorax can occur
without definitive reasons. Modi et al (19) reported that three cases of
hemothorax occurred within one week after surgery in 27 cases of
scoliosis with Duchenne muscular atrophy; however, computed
tomography scans did not find any inappropriate positioning of the
fixation apparatus. Modi hypothesized that the hemothorax may have
been caused by the cortex penetrating the lateral or front side of
the vertebrae during tapping or placing of the screws. In the
present study, no abnormalities of the screw paths or injuries of
the pulmonary tissues or vessels were found; therefore the
incidence of hemothorax may be interpreted using the theory by
Modi.
Posterior one-stage vertebral column resection has
been increasingly adapted by spine surgeons (20). The greatest advantage of this
surgery is that the surgeon is able to observe the spinal cord
directly to decrease the risks of spinal injuries, and reduce the
duration of surgery at the same time. Titanium mesh is a good
choice for reconstruction of the spine, due to the varieties of
shape, length and diameter that are available. The most common
complications of titanium mesh are subsidence and shift (21). Six cases of mild subsidence
occurred in the present study, which did not require revision.
Subsidence of the replaced spinal segment was associated with
increased duration of surgery, intraoperative bleeding volume and
total blood transfusion volume. No available explanation for this
connection was identified in the literature. However, X-rays showed
that when the upper or lower end plates were partially resected,
the exposure and bearing loss of the spongy bone could cause
subsidence of the replaced spinal segment. This leads to the
conclusion that the increased duration of surgery, intraoperative
bleeding volume and total blood transfusion volume may indicate the
spinal segment that is replaced during the surgery, and in such
surgeries the end plate cannot be preserved well due to unclear
visibility. However, once the prosthesis is fixed in position by
the vertebral pedicle screws, it should not sink any further, and
so should not lead to severe local kyphosis. Therefore, it is
important to increase the extraversion angle of the screws to stop
subsidence of the titanium mesh, which is a key process to avoid
this type of complication. Artificial vertebral bodies were used in
two cases without subsidence. They are expandable and easy to place
during the surgery, and the risks of spinal cord injury are
decreased; thus, from this point of view, they exhibits greater
advantages than the mesh cage.
In addition, increased drainage volume caused by the
allergic reactions to the allograft bone occurred in one case.
Great attention was paid to this complication and it was considered
to be associated with the immunogenicity of the allograft bone. In
certain previous cases, removal of the allograft bone was
necessary, and continuous drainage and antibiotic treatment were
recommended subsequently (22);
infection did not occur in these cases. However, in the present
study, the drainage volume increased for 4 days after surgery and
began to decrease gradually from postoperative day 5. Therefore, it
was decided to retain the drainage and use antibiotics, to ensure
that no infection occurred. This indicates that whether or not it
is beneficial to remove the allograft bone depends on the
individual case.
One case of acute enteritis was observed in the
present study, and it was concluded that this may have been caused
by unclean food. The patient subsequently healed following
administration of antibiotics orally for three days. Two
preoperative paraplegia patients suffered sensory decrease, but
remained at Frankel Grade B, and two cases survived for <6
months. However, these four patients were satisfied with the
outcome of the surgeries in terms of significant pain relief and
improved life quality; therefore, the surgery indicators should
also be individualized.
Univariate instead of multivariate analyses were
used in the present study, due to the small number of patients
recruited. This may have increased data deviations and influenced
the accuracy of the result. Thus, further study and the collection
of more data are required to improve the quality of the study. In
conclusion, the present study demonstrates that the majority of the
complications were minor and did not affect the prognosis of the
patients. Active prevention is necessary to reduce the incidence of
complications, in particular major ones.
Acknowledgements
This study was supported by the National Natural
Science Foundation for the Youth (no. 81101382).
References
|
1
|
Feiz-Erfan I, Rhines LD and Weinberg JS:
The role of surgery in the management of metastatic spinal tumors.
Semin Oncol. 35:108–117. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hamzaoglu A, Alanay A, Ozturk C, et al:
Posterior vertebral column resection in severe spinal deformities:
a total of 102 cases. Spine (Phila Pa 1976). 36:E340–E344.
2011.PubMed/NCBI
|
|
3
|
Jandial R, Kelly B and Chen MY:
Posterior-only approach for lumbar vertebral column resection and
expandable cage reconstruction for spinal metastases. J Neurosurg
Spine. 19:27–33. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Eleraky M, Setzer M and Vrionis FD:
Posterior transpedicular corpectomy for malignant cervical spine
tumors. Eur Spine J. 19:257–262. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kaltoft B, Kruse A, Jensen LT and Elberg
JJ: Reconstruction of the cervical spine with two osteocutaneous
fibular flap after radiotherapy and resection of osteoclastoma: a
case report. J Plast Reconstr Aesthet Surg. 65:1262–1264. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhu Y, Zhao H, Qiu GX, et al: Single-stage
posterior spondylectomy, circumferential decompression and
reconstruction using mesh cage for spinal tumors. Chin Med Sci J.
24:172–177. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Naito Y, Akeda K, Kasai Y, et al: Lumbar
metastasis of choriocarcinoma. Spine (Phila Pa 1976). 34:E538–E543.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McDonnell MF, Glassman SD, Dimar JR II,
Puno RM and Johnson JR: Perioperative complications of anterior
procedures on the spine. J Bone Joint Surg Am. 78:839–847.
1996.PubMed/NCBI
|
|
9
|
Frankel HL, Hancock DO, Hyslop G, et al:
The value of postural reduction in the initial management of closed
injuries of the spine with paraplegia and tetraplegia. I
Paraplegia. 7:179–192. 1969. View Article : Google Scholar
|
|
10
|
Schwab FJ, Lafage V, Farcy JP, et al:
Predicting outcome and complications in the surgical treatment of
adult scoliosis. Spine (Phila Pa 1976). 33:2243–2247. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Weiss HR and Goodall D: Rate of
complications in scoliosis surgery-a systematic review of the Pub
Med literature. Scoliosis. 3:92008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wise JJ, Fischgrund JS, Herkowitz HN,
Montgomery D and Kurz LT: Complication, survival rates, and risk
factors of surgery for metastatic disease of the spine. Spine
(Phila Pa 1976). 24:1943–1951. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Biagini R, Casadei R, Boriani S, et al: En
bloc vertebrectomy and dural resection for chordoma: a case report.
Spine (Phila Pa 1976). 28:E368–E372. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen N, Li XL, Dong J, et al: En bloc
spondylectomy for thoracolumbar spinal malignant tumors via
posterior approach. Chinese Journal of Spine and Spinal Cord.
20:624–628. 2010.(In Chinese).
|
|
15
|
McCormick WE, Will SF and Benzel EC:
Surgery for thoracic disc disease. Complication avoidance: overview
and management. Neurosurg Focus. 9:e132000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Boriani S, Bandiera S, Donthineni R, et
al: Morbidity of en bloc resections in the spine. Eur Spine J.
19:231–241. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Modi HN, Suh SW, Yang JH, et al: Surgical
complications in neuromuscular scoliosis operated with
posterior-only approach using pedicle screw fixation. Scoliosis.
4:112009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shapiro G, Green DW, Fatica NS and
Boachie-Adjei O: Medical complications in scoliosis surgery. Curr
Opin Pediatr. 13:36–41. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Modi HN, Suh SW, Hong JY, et al: Treatment
and complications in flaccid neuromuscular scoliosis (Duchenne
muscular dystrophy and spinal muscular atrophy) with posterior-only
pedicle screw instrumentation. Eur Spine J. 19:384–393. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tomita K, Kawahara N, Murakami H and
Demura S: Total en bloc spondylectomy for spinal tumors:
improvement of the technique and its associated basic background. J
Orthop Sci. 11:3–12. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Alfieri A, Gazzeri R, Neroni M, et al:
Anterior expandable cylindrical cage reconstruction after cervical
spinal metastasis resection. Clin Neurol Neurosurg. 113:914–917.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jin XH, LH and Niu HF: Rejection after
posterior lumbar lateral fusion in 6 patients undergoing allogeneic
bone transplantation. Journal of Clinical Rehabilitative Tissue
Engineering Research. 12:10497–10499. 2008.(In Chinese).
|