Introduction
Due to the limited self-healing capacity of the
articular cartilage, knee osteoarthritis (OA) has become one of the
most common causes of pain and disability in middle-aged and older
patients (1). The majority of mild
and moderate cases of OA can be successfully managed with
conservative interventions, including drugs, such as non-steroidal
analgesics, weight control and lifestyle changes (2). Intra-articular injections of
hyaluronic acid (HA) are commonly used to treat knee OA (3). The exact mechanism of HA action is
unclear. Restoration of the elastoviscous properties of synovial
fluid seems to be the most logical explanation of the function of
HA, while other mechanisms include possible anti-inflammatory and
antinociceptive properties or stimulation of in vivo HA
synthesis by the exogenously injected HA (3). Although HA is effective at reducing
adverse symptoms, it does not modify the biochemical environment of
the joint or promote cartilage healing (4). Therefore, further clinical and
laboratory research are focused on developing novel biological
methods for repairing damaged cartilage.
In previous years, the biological effects of growth
factors (GFs) on cartilage repair have been well documented both
in vivo and in vitro (5-8).
In particular, platelet-rich plasma (PRP) is a fraction of the
plasma containing platelets and GF at concentrations above baseline
that can be produced by centrifugal separation of whole blood
(9,10). PRP has been indicated to exhibit a
positive effect on the local environment, reducing intra-articular
synovial hyperplasia and adjusting the synovial fluid concentration
of IL-1 receptor antagonist (11).
PRP has been used to successfully treat chronic elbow tendinosis
and refractory wounds (12-14),
such that a number of studies have previously reported its
effectiveness for the treatment of knee OA (15-18).
However, there remains to be a lack of clinical research into the
cost and treatment time of PRP administration and its potential use
as a therapeutic option for articular cartilage injuries.
The present study aimed to compare the clinical and
economic benefits of PRP intra-articular injections with those of
HA intra-articular injections in Chinese patients with mild knee
OA. In addition, frequency, proportion, pain score, duration and
prognosis of adverse reactions were also recorded.
Patients and methods
Patients
The present study was a retrospective comparative
study using HA as the control. The PRP procedure was approved by
the Ethics Committee of Ningbo No. 6 Hospital (Ningbo, China) prior
to study commencement. Between March 2017 and December 2018, 101
patients with knee OA receiving PRP or HA injections in the
Department of Joint Surgery of Ningbo No. 6 Hospital, were
recruited. There were 25 female and 17 male patients in the PRP
group and 27 female and 17 male patients in the control group. The
age of patients ranged from 43 to 72 years, with a mean of
57.57±5.87 in the PRP group and 59.66±5.21 in the control group,
with no significant difference (P=0.08) (Table I). All patients with knee OA in the
associated study period were screened for inclusion. The inclusion
criteria were as follows: i) Patients were aged between 18 and 75
years old; ii) chronic knee pain or swelling lasting >3 months;
and iii) X-ray findings of degenerative joint changes
[Kellgren-Lawrence score (19),
grade I-III]. The exclusion criteria included: i) Kellgren-Lawrence
scores of grade 0 or IV; ii) pregnant or lactating women; iii)
diabetes; iv) rheumatoid arthritis; v) gout; vi) blood diseases;
vii) severe cardiovascular diseases; viii) infections; ix)
immunodepression; x) patients receiving anticoagulant therapy; and
xi) patients with hemoglobin values >11 g/dl and platelet values
>150,000/mm3. Patients who did not complete three
injections or 6 months of follow-up were also excluded from the
study.
 | Table IBasal characteristics of patients in
the two groups. |
Table I
Basal characteristics of patients in
the two groups.
| Parameter | Platelet-rich
plasma | Hyaluronic acid | P-value |
|---|
| No. of
patients/knees | 42/42 | 44/47 | |
| Age (years) | 57.57±5.87 | 59.66±5.21 | 0.08 |
| Male sex, n (%) | 17 (40.48%) | 17 (38.64%) | |
| Female sex, n
(%) | 25 (59.52%) | 27 (61.36%) | |
| Body mass index
(kg/m2) | 23.74±2.87 | 24.31±2.82 | 0.35 |
| Kellgren-Lawrence
grade | | | |
|
I | 15 | 16 | |
|
II | 19 | 22 | |
|
III | 8 | 9 | |
Treatment, preparation and clinical
evaluation
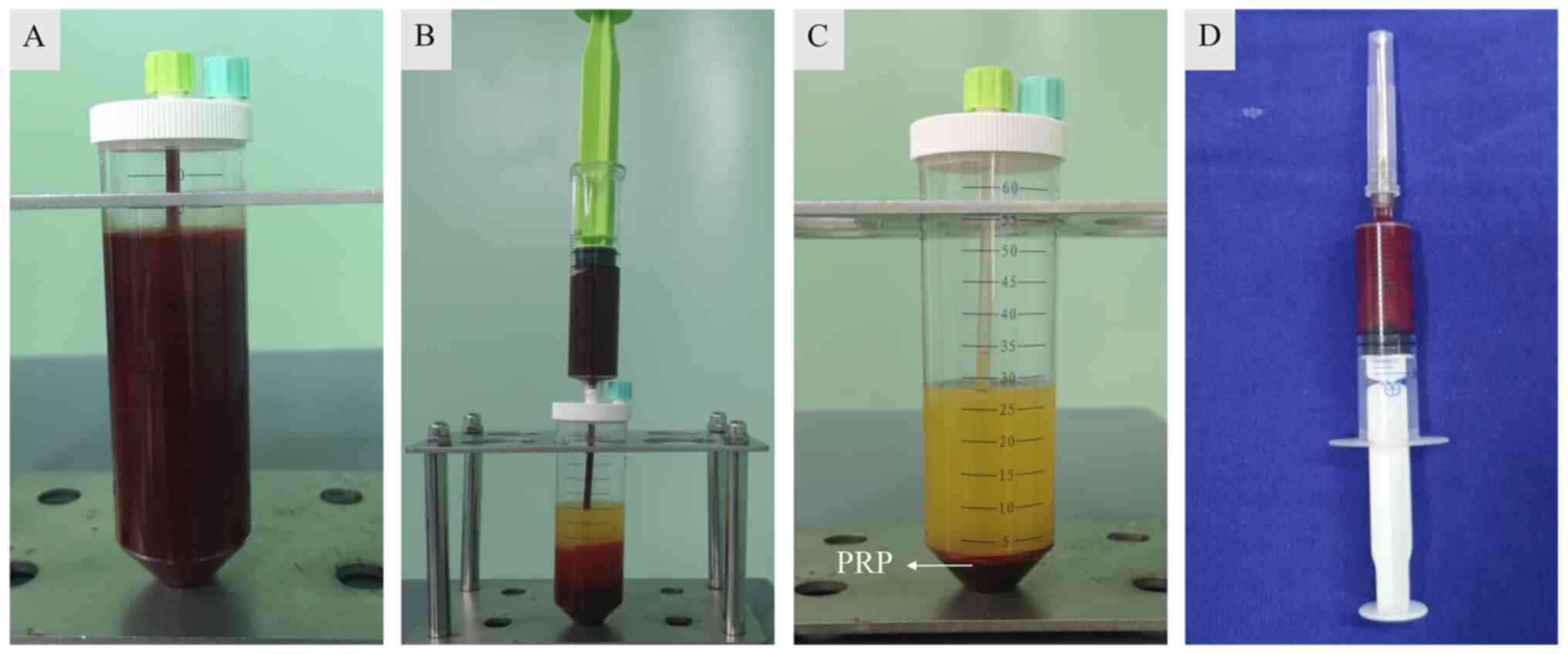
For each injection, a 50-ml blood sample was
collected from the median elbow vein using a 50-G needle, such that
the ratio of blood to anticoagulant reached 9:1. The blood samples
collected were then transferred to a separation tube (Weigao New
Polymer Materials Co., Ltd.), centrifuged twice to first separate
erythrocytes and then to concentrate platelets (378 x g for 10 min
each; Fig. 1); this resulted in a
unit of 4.5 ml PRP (Fig. 1). All
procedures were performed in the same therapeutic office at room
temperature (25˚C). A total of 3.5 ml PRP was immediately
transported to the injection room whereas the remainder was sent to
the laboratory of Ningbo No. 6 Hospital for platelet concentration
analysis. The PRP platelet and leukocyte counts were found to be
819.47±136.32x109/l and 32.2±10.42x1012/l,
respectively, which were 6.40±1.10 and 6.10±1.93 times greater than
those in the preoperative peripheral blood.
The patients received three PRP or HA
intra-articular injections at 1-week intervals. Following
iodopovidone-based disinfection, a 21-gauge needle with a 10-ml
syringe was used for knee injections, following which the skin was
sterilely dressed and excess effusion fluid was extracted before
intra-articular injection of 3.5 ml PRP or 2.5 ml HA (ARTZ;
Seikagaku Corporation) into the knee joint (Video S1). At the end of the procedure,
the injection site was covered with a sterile dressing and patients
were asked to bend and extend the knee several times. The patients
were then given the following instructions: i) No showering for 3
days; ii) ipsilateral joint activities should be limited over the
next 24 h; iii) symptoms such as pain and swelling are normal; iv)
and ice on the knee helps to reduce pain and swelling.
Outcome assessments were performed by SCW blinded to
the treatment groups. The patients were clinically evaluated 1 h
before injection and at 1- and 6-month post-injection intervals.
During each evaluation, International Knee Documentation Committee
(IKDC) subjective scores (20),
Western Ontario and McMaster Universities (WOMAC) scores (21) and the visual analogue scale (VAS)
were evaluated (22). These three
scales are used to assess joint pain, activity and instability.
Joint infection, deep vein thrombosis and hematoma were defined as
major adverse events, whilst joint pain and swelling were defined
as mild adverse reactions. Frequency, proportion, pain score, start
time, end time and duration of these reactions were also observed.
Average cost, treatment time and patient satisfaction in the two
groups were also recorded. Patient satisfaction referred to whether
the patient was satisfied with the treatment, which was divided
into satisfaction and dissatisfaction.
Statistical analysis
The data are expressed as the mean ± SD unless
otherwise indicated. Two-way ANOVA was performed to assess the
differences between groups at different follow-up times. Friedman's
test followed by Wilcoxon signed rank test with Bonferroni
correction was used to evaluate the data at different time points
within a single group. Mann-Whitney U test was used to compare the
numerical parameters between HA and PRP groups, including
post-injection VAS scores, treatment time and average cost per
person. Statistical analyses were performed using SPSS version 23.0
(IBM Corp.), where P<0.05 was considered to indicate a
statistically significant difference.
Results
Basal information
Due to incomplete treatment data, 15 of these
patients were excluded from the present study. In total, 86
patients (89 knees; 3 patients with OA in both knees) met the study
criteria (PRP group, 42 patients and 42 knees; HA group, 44
patients and 47 knees) and completed 6 months of follow-up
examinations. No differences in basal characteristics were observed
between the two groups (Table
I).
Clinical scores
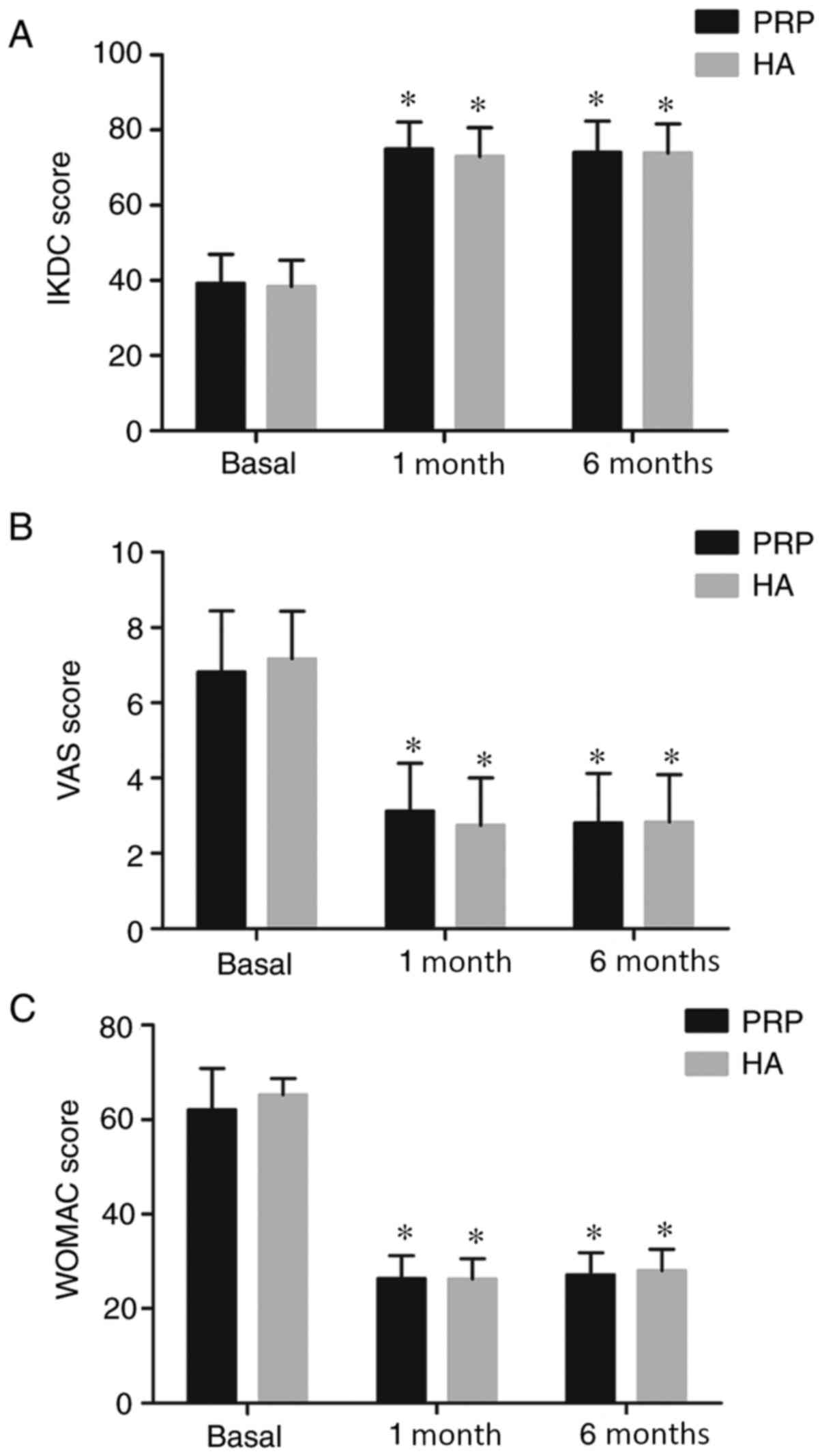
Preliminary analysis of patients in the PRP and HA
groups demonstrated a statistically significant improvement in the
three clinical scores from pre-injection to the 1- and 6-month
follow-up assessments (P<0.05). However, no significant
inter-group differences were observed in the clinical scores
between the two follow-up time points. In the PRP group, the IKDC
score increased from 39.21±7.71 at basal evaluation to 74.95±7.15
after 1 month and 74.00±8.42 after 6 months (Fig. 2A), the VAS score decreased from
6.80±1.62 at basal evaluation to 3.12±1.27 after 1 month and
2.81±1.31 after 6 months (Fig. 2B)
and the WOMAC score decreased from 62.09±8.74 at basal evaluation
to 26.35±4.90 after 1 month and 27.14±4.66 after 6 months (Fig. 2C). In the HA group, the IKDC score
increased from 38.40±6.95 at the basal evaluation to 72.96±7.64
after 1 month and then 73.87±7.76 after 6 months evaluation
(Fig. 2A), the VAS score decreased
from 7.17±1.26 at basal evaluation to 2.74±1.26 after 1 month and
2.83±1.25 after 6 months (Fig. 2B)
and the WOMAC score decreased from 65.28±3.49 at basal evaluation
to 26.31±4.27 after 1 month and 28.00±4.55 after 6 months (Fig. 2C).
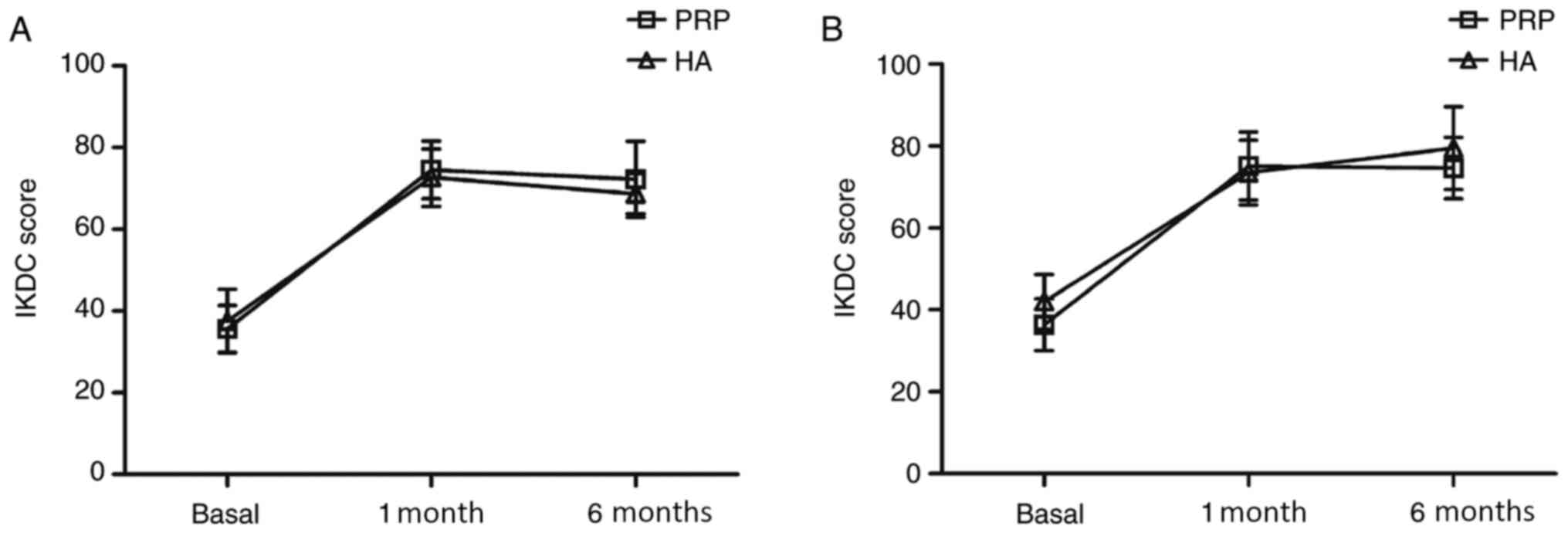
No significant differences in the Kellgren-Lawrence
grade I, II or III scores were observed between the PRP and HA
groups (P>0.05). However, further analysis revealed slightly
different results in patients affected by varying degrees of
cartilage degeneration. At the 6-month follow-up assessment,
patients in the PRP group who were affected by Kellgren-Lawrence
grade I lesions exhibited higher IKDC scores (72.00±9.30) compared
with that in the HA group (68.63±4.93) (P=0.20; Fig. 3A). HA appeared to improve the IKDC
score (79.55±10.16) of patients with Kellgren-Lawrence grade III
degenerative joint changes compared with that in the PRP group
(74.60±7.52), though this did not reach statistical significance
(P=0.28; Fig. 3B).
Complications and adverse
reactions
Complications, including infection, deep vein
thrombosis, hematoma or other major adverse events were not
observed during treatment itself. However, compared with HA, PRP
was associated with more post-injection pain and swelling (33.33
vs. 10.64%) and significantly more severe pain (P<0.01; Table II). The start time of adverse
reactions in the PRP group was 0.33±0.42 h after injection,
compared with 0.10±0.21 h in the HA group, though this difference
was not statistically significant (Table II). Furthermore, mild reactions
subsided significantly later in the PRP group (45.71±18.41)
compared with that in the HA group (31.20±23.04) (P=0.02; Table II), suggesting that the duration
time was significantly longer in the PRP group (49.00±18.27) than
that in the HA group (31.10±23.11) (P=0.02; Table II). However, all reactions were
self-limiting and did not require further treatment.
 | Table IIMild adverse reactions of the two
groups. |
Table II
Mild adverse reactions of the two
groups.
| Parameter | Platelet-rich
plasma | Hyaluronic acid | P-value |
|---|
| Total injections
(n) | 126 | 141 | |
| Frequency, n (%) | 42 (33.33) | 15 (10.64) | |
| Pain score (visual
analogue scale) | 3.59±2.24 | 1.93±0.80 | <0.01 |
| Start time (h) | 0.33±0.42 | 0.10±0.21 | 0.05 |
| End time (h) | 45.71±18.41 | 31.20±23.04 | 0.02 |
| Duration (h) | 49.00±18.27 | 31.10±23.11 | 0.02 |
Treatment time and preparation
cost
The cost of PRP treatment (4,996.00±12.00 renminbi)
included the PRP kit and associated preparation costs, which
significantly exceeded the cost of HA administration (219.00±5.50
renminbi) (P<0.01; Table III).
PRP preparation also included two centrifugation steps, which also
markedly prolonged the total treatment time in the PRP group
(30.00±5.12 min) than that in the control group (6.00±1.30 min)
(P<0.01; Table III). The
average cost of PRP treatment per patient was 22.81 times that of
HA treatment, whereas the average treatment time was 5 times that
of HA (Table III). However, at
the 6-month follow-up, patient satisfaction rates reached 71.43 and
70.21% for the PRP and HA groups, respectively (Table III), indicating no significant
difference between the two treatment options.
 | Table IIIThe cost and satisfaction rates of
the two groups. |
Table III
The cost and satisfaction rates of
the two groups.
| Parameter | Platelet-rich
plasma | Hyaluronic
acid | P-value |
|---|
| Average cost per
person (Renminbi) | 4,996.00±12.00 | 219.00±5.50 | <0.01 |
| Treatment time
(min) | 30.00±5.50 | 6.00±1.30 | <0.01 |
| Satisfaction rate,
n (%) | 30 (71.43%) | 33 (70.21%) | |
Discussion
The positive biological effects of GFs on cartilage
repair have been well documented both in vivo and in
vitro (5,6). The present study was designed to
obtain preliminary data on the short-term clinical efficacy and
safety of PRP intra-articular injections. The results indicate that
PRP treatment reduces pain and improves patient knee function after
6 months, but the three clinical scores of PRP injections are
ultimately not better compared with HA administration. PRP was also
associated with higher incidences and more serious post-injection
pain and swelling, though these reactions were self-limiting and
required no further treatment.
Over the past decade, numerous studies have
demonstrated advantages of intra-articular PRP injections (15-18).
Since OA is an intra-articular lesion, intra-articular PRP
administration is a direct and minimally invasive treatment that is
well tolerated by patients (18).
PRP is derived from autologous peripheral blood, meaning that it
has good biocompatibility, is not associated with immune rejection
or disease transmission and potentially confers anti-infection
effects (23).
Previous studies have demonstrated the positive
effects of PRP on knee OA (15-18).
Lisi et al (15) previously
reported a phase II randomized controlled trial where 50 patients
received three PRP (n=28) or HA (n=22) intra-articular injections
at 4-week intervals. Using MRI scanning, PRP was concluded to
reduce articular damage in as soon as 6 months after treatment,
which was better than that by HA. Sánchez et al (16) treated patients with OA using
intra-articular injections of autologous platelet-rich growth
factors (PRGFs), with those receiving hyaluronan injections serving
as the control group. Each group included 30 patients. After 5
weeks, the success rate for the pain subscale reached 33.4 and 10%
for the PRGF and hyaluronan groups, respectively. These results
were encouraging, though due to short follow-up times (5 weeks) and
small sample sizes, this previous study (16) included the same limitations as the
aforementioned study by Lisi et al (15). Furthermore, calcium chloride was
used as a PRP activator in both of these previous studies.
Following activation by calcium chloride, PRP is transformed into
liquid PRGF and solid PRP gels (24,25).
PRGF injection alone causes GF loss from the PRP gel. However,
applying PRP with calcium chloride results in the rapid formation
of the PRP gel in the joint, which is not conducive to the
distribution of GF in the damaged cartilage (26). Wang-Saegusa et al (17) published a prospective study of 261
patients with knee OA. The patients received three injections of
PRP before clinical evaluations were conducted after 6 months using
the WOMAC score, VAS, Lequesne Index and the Short Form 36 Health
Survey (SF-36). Statistical analysis revealed significant results
with an improvement in all clinical scores, though the study did
not include a control group. Furthermore, Kon et al
(18) reported that PRP resulted in
a better clinical outcome compared with those of low molecular
weight HA (LWHA) and high molecular weight HA (HWHA), where 150
patients (50 in each group) were treated with three injections of
either PRP, LWHA or HWHA.
However, a number of studies have also reported
negative effects of PRP injection therapy (27,28).
In 2016, Filardo et al (27)
reported the results of a randomized, blinded and controlled trial
with 12 months of follow-up, which included 192 patients with knee
OA (96 treated with HA and 96 with PRP). The patients received
three weekly intra-articular injections and corresponding clinical
evaluations. The patients in both the PRP and HA groups exhibited
improved IKDC scores, which did not differ at any of the follow-up
points. It was therefore concluded that PRP injections were no more
beneficial than HA treatment. In addition, a concern was also
highlighted in this study. PRP preparation involves harvesting 150
ml peripheral blood followed by two centrifugation steps, which
yields 20 ml PRP (27). After the
first injection of 4-5 ml, the remaining PRP was frozen for 2 weeks
and then thawed for the second and third injections. It was
suggested that storing PRP at -20˚ and then thawing for subsequent
use may significantly decrease the levels of GFs, including
epidermal growth factor, vascular endothelial growth factor,
platelet-derived growth factor, insulin-like growth factor 1 and
transforming growth factor (29),
which may subsequently alter the clinical efficacy of PRP.
Using the results of previous studies, the present
study proposes an improved method of PRP administration. To
activate PRP more slowly and thus prolong GF activity, calcium
chloride was not used before injection. Instead, pure PRP was
directly injected to enable even distribution within the joint. To
avoid freezing, PRP was produced from fresh peripheral blood prior
to each injection, which not only ensured the freshness of the PRP,
but also reduced the possibility of exogenous contamination.
Generally speaking, previous studies have reported
that treatment with PRP causes more adverse reactions compared with
HA (27,28). In the present study, adverse
reactions were recorded in more detail, which included frequency,
proportion, pain score and duration of these events. More frequent
and severe pain reactions were observed following PRP, compared
with that after HA injection. The duration of the adverse reactions
in the PRP group was also longer compared with that in the HA
group, which may be associated with stimulation of the joint
synovium by components within the PRP, such as red and white blood
cells.
The cost of PRP treatment is primarily determined by
the price of the PRP kit in China. There are currently >10 types
of PRP preparation kits available at varying prices, though the PRP
kit from Weigao New Polymer Materials Co., Ltd. is one of the few
currently approved kits for intra-articular injections in China.
Therefore, the cost of PRP treatment may decrease as novel PRP kits
are approved for clinical use. Additionally, centrifugal
preparation of PRP greatly prolongs treatment time. Filardo et
al (27) proposed freezing a
single PRP sample, which could be thawed for subsequent injections.
However, this may reduce the levels of available GFs, thus reducing
the clinical benefits of PRP treatment.
There are a number of limitations to the present
study, including the non-randomized double-blind design, small
sample size and short follow-up time, in addition to a lack of
direct evidence of cartilage repair, including data from
arthroscopic or radiological examinations. After outlining the
different effects of PRP and HA injections, the patients were
allowed to select their preferred method of treatment, which may
also have introduced bias to the study results.
These preliminary results indicated that although
PRP injections could significantly improve clinical outcome after 6
months in patients with knee OA, PRP is not more effective compared
with HA. PRP was also associated with higher incidence rates and
more serious post-injection pain and swelling compared with HA,
although these reactions were self-limiting and required no further
treatment. Furthermore, PRP injections were associated with higher
costs and treatment times compared with HA. Therefore, additional
clinical studies are required before PRP injections can be
considered as a first-line treatment option for knee OA.
Supplementary Material
Intra-articular injection of
platelet-rich plasma. Following iodopovidone-based disinfection,
the skin was sterilely dressed, and 3.5 ml PRP was slowly injected
into the knee joint through a 21-gauge needle.
Supplementary Data
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by grants from the
Ningbo Natural Science Foundations (grant no. 2018A610261) and
Zhejiang Provincial Key Laboratory of Pathophysiology (grant no.
201911).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HL and ML conceived and designed the study; HL, ML,
ZYH and SCW performed the literature search; HL, ML, ZLD and JHZ
performed the quality assessment of the screened literature; ZYH
and SCW were involved in PRP production and patient follow-up
evaluation; ZLD and JHZ were responsible for patient enrollment and
PRP administration; HL and ML were responsible for confirming the
authenticity of all the raw data, writing the manuscript and
performing the final revision. All authors have read and approved
the final version of the manuscript, and due care has been taken to
ensure the integrity of the work.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Ningbo No. 6 Hospital (Ningbo, China). The
participating patients had complete clinical data, and written
informed consent was obtained from the patients or their
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Robinson DL, Kersh ME, Walsh NC, Ackland
DC, de Steiger RN and Pandy MG: Mechanical properties of normal and
osteoarthritic human articular cartilage. J Mech Behav Biomed
Mater. 61:96–109. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zhang W, Moskowitz RW, Nuki G, Abramson S,
Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty
M, et al: OARSI recommendations for the management of hip and knee
osteoarthritis, Part II: OARSI evidence-based, expert consensus
guidelines. Osteoarthritis Cartilage. 16:137–162. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Brzusek D and Petron D: Treating knee
osteoarthritis with intra-articular hyaluronans. Curr Med Res Opin.
24:3307–3322. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Maricar N, Callaghan MJ, Felson DT and
O'Neill TW: Predictors of response to intra-articular steroid
injections in knee osteoarthritis - A systematic review.
Rheumatology (Oxford). 52:1022–1032. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shah NJ, Geiger BC, Quadir MA, Hyder MN,
Krishnan Y, Grodzinsky AJ and Hammond PT: Synthetic nanoscale
electrostatic particles as growth factor carriers for cartilage
repair. Bioeng Transl Med. 1:347–356. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Medeiros Da Cunha CM, Perugini V,
Bernegger P, Centola M, Barbero A, Guildford AL, Santin M, Banfi A,
Martin I and Marsano A: Vascular endothelial growth factor
sequestration enhances in vivo cartilage formation. Int J Mol Sci.
18(2478)2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Li M, Zhang J, Jin Q, Li J, He Z and Di Z:
Role of platelet-rich plasma in articular cartilage lesions. Chin
Med J (Engl). 127:3987–3992. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mascarenhas R, Saltzman BM, Fortier LA and
Cole BJ: Role of platelet-rich plasma in articular cartilage injury
and disease. J Knee Surg. 28:3–10. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Masuki H, Okudera T, Watanebe T, Suzuki M,
Nishiyama K, Okudera H, Nakata K, Uematsu K, Su CY and Kawase T:
Growth factor and pro-inflammatory cytokine contents in
platelet-rich plasma (PRP), plasma rich in growth factors (PRGF),
advanced platelet-rich fibrin (A-PRF), and concentrated growth
factors (CGF). Int J Implant Dent. 2(19)2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mussano F, Genova T, Munaron L, Petrillo
S, Erovigni F and Carossa S: Cytokine, chemokine, and growth factor
profile of platelet-rich plasma. Platelets. 27:467–471.
2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Frisbie DD, Kawcak CE, Werpy NM, Park RD
and McIlwraith CW: Clinical, biochemical, and histologic effects of
intra-articular administration of autologous conditioned serum in
horses with experimentally induced osteoarthritis. Am J Vet Res.
68:290–296. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Alessio-Mazzola M, Repetto I, Biti B,
Trentini R, Formica M and Felli L: Autologous US-guided PRP
injection versus US-guided focal extracorporeal shock wave therapy
for chronic lateral epicondylitis: A minimum of 2-year follow-up
retrospective comparative study. J Orthop Surg (Hong Kong).
26(2309499017749986)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Karaduman M, Okkaoglu MC, Sesen H,
Taskesen A, Ozdemir M and Altay M: Platelet-rich plasma versus open
surgical release in chronic tennis elbow: A retrospective
comparative study. J Orthop. 13:10–14. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rainys D, Samulėnas G, Kievišas M,
Samulėnienė E, Pilipaitytė L and Rimdeika R: Platelet biology and
the rationale of PRP therapy in chronic wounds. Eur J Plast Surg.
40:1–10. 2017.
|
|
15
|
Lisi C, Perotti C, Scudeller L, Sammarchi
L, Dametti F, Musella V and Di Natali G: Treatment of knee
osteoarthritis: Platelet-derived growth factors vs. hyaluronic
acid. A randomized controlled trial. Clin Rehabil. 32:330–339.
2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sánchez M, Anitua E, Azofra J, Aguirre JJ
and Andia I: Intra-articular injection of an autologous preparation
rich in growth factors for the treatment of knee OA: A
retrospective cohort study. Clin Exp Rheumatol. 26:910–913.
2008.PubMed/NCBI
|
|
17
|
Wang-Saegusa A, Cugat R, Ares O, Seijas R,
Cuscó X and Garcia-Balletbó M: Infiltration of plasma rich in
growth factors for osteoarthritis of the knee short-term effects on
function and quality of life. Arch Orthop Trauma Surg. 131:311–317.
2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kon E, Mandelbaum B, Buda R, Filardo G,
Delcogliano M, Timoncini A, Fornasari PM, Giannini S and Marcacci
M: Platelet-rich plasma intra-articular injection versus hyaluronic
acid viscosupplementation as treatments for cartilage pathology:
From early degeneration to osteoarthritis. Arthroscopy.
27:1490–1501. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kellgren JH and Lawrence JS: Radiological
assessment of osteoarthrosis. Ann Rheum Dis. 16:494–502.
1957.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Agel J and LaPrade RF: Assessment of
differences between the modified Cincinnati and International Knee
Documentation Committee patient outcome scores: A prospective
study. Am J Sports Med. 37:2151–2157. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bellamy N: WOMAC: A 20-year experiential
review of a patient-centered self-reported health status
questionnaire. J Rheumatol. 29:2473–2476. 2002.PubMed/NCBI
|
|
22
|
Dones I, Messina G, Nazzi V and Franzini
A: A modified visual analogue scale for the assessment of chronic
pain. Neurol Sci. 32:731–733. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Bielecki TM, Gazdzik TS, Arendt J,
Szczepanski T, Król W and Wielkoszynski T: Antibacterial effect of
autologous platelet gel enriched with growth factors and other
active substances: An in vitro study. J Bone Joint Surg Br.
89:417–420. 2007.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wu W, Chen F, Liu Y, Ma Q and Mao T:
Autologous injectable tissue-engineered cartilage by using
platelet-rich plasma: Experimental study in a rabbit model. J Oral
Maxillofac Surg. 65:1951–1957. 2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sun Y, Feng Y, Zhang CQ, Chen SB and Cheng
XG: The regenerative effect of platelet-rich plasma on healing in
large osteochondral defects. Int Orthop. 34:589–597.
2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Li M and Zhang CQ: Clinical application
and biomaterial properties of platelet-rich plasma. J Clin Rehabil
Tissue Eng Res. 8:1445–1448. 2011.(In Chinese).
|
|
27
|
Filardo G, Di Matteo B, Di Martino A,
Merli ML, Cenacchi A, Fornasari P, Marcacci M and Kon E:
Platelet-rich plasma intra-articular knee injections show no
superiority versus viscosupplementation: A randomized controlled
trial. Am J Sports Med. 43:1575–1582. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Filardo G, Kon E, Di Martino A, Di Matteo
B, Merli ML, Cenacchi A, Fornasari PM and Marcacci M: Platelet-rich
plasma vs hyaluronic acid to treat knee degenerative pathology:
Study design and preliminary results of a randomized controlled
trial. BMC Musculoskelet Disord. 13(229)2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Hosnuter M, Aslan C, Isik D, Caliskan G,
Arslan B and Durgun M: Functional assessment of autologous
platelet-rich plasma (PRP) after long-term storage at -20 ˚C
without any preservation agent. J Plast Surg Hand Surg. 51:235–239.
2017.PubMed/NCBI View Article : Google Scholar
|