Introduction
It is difficult to expose the sphenoid sinus
considering its location deep inside the sphenoid bone and adjacent
to the basis cranii. The sphenoid sinus is close to important
anatomical structures, such as the optic nerve, internal carotid
artery and sella turcica, which makes the management of sphenoid
sinus lesions challenging (1). The
blood vessels and olfactory nerve endings are widely distributed in
the surgical field, thus bleeding during or post-surgery and
postoperative olfactory hypofunction are prone to occur (2,3).
Moreover, these characteristics may give rise to challenging
surgical operations, incomplete cleaning of sphenoid sinus lesions,
diverse surgical complications and rapid recurrence of lesions
after operation (4,5).
Primary functional endoscopic sinus surgery is
effective in treating medically refractory chronic rhinosinusitis,
with ~5-15% of patients requiring revision, endoscopic sinus
surgery (6), which indicates that
a marked proportion of patients will require >1 revision sinus
surgery. Surgery of the sphenoid sinus is always affected by nasal
anatomy, surgical instruments, lesion characteristics and the
experience of the operator, which means that the revision rate may
be higher (5).
It was observed that, in clinical practice, the rate
of orifice re-closing after sphenoid sinus surgery, especially
refractory sphenoid sinusitis, was high (4). Refractory sphenoid sinusitis refers
to patients in whom sphenoid sinusitis has not been effectively
controlled >3 months post standard nasal endoscopic surgery and
comprehensive treatment, with persistent chronic inflammation in
the operative cavity as well as prolonged symptoms and signs for
>6 months after follow-up (7).
Most patients with refractory sphenoid sinusitis are characterized
by sphenoid sinus stenosis, small sinus cavity volume, heavy
mucosal inflammation in the sinus cavity, peripheral bone
hyperplasia and easy recurrence after surgery (8). Sphenoid sinus scar stenosis or
sphenoid sinus atresia after surgery, which are difficult to deal
with in the clinic, commonly appear when routine sphenoid sinus
surgery is performed using a nasal endoscope. Furthermore, local
recurrence is also a problem for patients with sphenoidal tumor
(1,4,5).
Currently, approaches to transnasal endoscopic
sphenoid sinus surgery can be grouped as follows: The Messerklinger
approach, the Wingand approach, Transphenoidal septum into the
contralateral sphenoid sinus approach and trans-medial plate of
pterygoid process approach (9-12).
The principles common to the aforementioned approaches are to fully
open the sphenoid sinus, completely remove the lesion and to
maintain drainage. The more traditional and the most widely used
surgical approaches in the sphenoid sinus are via the
trans-superior meatus or the transethmoidal sinus and other
contralateral or lateral approaches (both on the lateral side of
nasal septum) (11,12). There are seldom reports of
sphenoidal surgery through the nasal septum mucoperiosteal
incision. In the present study, the new methodological application
of expanding bilateral sphenoid sinus plasty was evaluated. The
surgical outcomes of 42 cases of sphenoid sinus diseases treated
using expanding bilateral sphenoid sinus plasty using the nasal
endoscope and the postoperative curative effects in patients were
observed.
Materials and methods
Clinical data
The present study was performed at The Medical
School of Nanjing University Affiliated Jinling Hospital (Nanjing,
China). Each patient signed an informed consent before surgery. The
study was approved by the Ethics Committees of The Medical School
of Nanjing University Affiliated Jinling Hospital (approval no.
2012NKY011). A total of 42 patients with sphenoid sinus lesions,
confirmed during the first surgical operation and reoperation
pathology, from December 2012 to December 2018 were included in the
study. The group included 26 males and 16 females, with mean age of
45.7 years (range 22-75 years). The sphenoid sinus lesions included
15 patients with refractory sphenoid sinusitis (with 3 patients
with postoperative complications of pituitary adenoma), 9 patients
with sphenoidal mucoceles, 8 patients with fungal sphenoid
sinusitis (with 1 patient having intracranial infection and fever),
3 patients with sphenoid sinus papilloma, 2 patients with posterior
sphenoid nostril polyps, 2 patients with sphenoid sinus carcinoma,
1 patient with sphenoid sinus chordoma, 1 patient with pituitary
adenoma and 1 patient with olfactory neuroblastoma with sphenoid
sinus and intracranial invasion. The clinical symptoms were as
follows: Headache (36 patients), purulent runny nose (23 patients),
nosebleed or bloody runny nose (18 patients), nasal obstruction (16
patients), hyposmia (6 patients), diplopia (3 patients), vision
decline (2 patients), exophthalmos or distended pain (2 patients),
fever (1 patient) and vomiting (1 patient). The disease course
ranged from 6 months to 11 years, with a median of 2.6 years. A
total of 21 patients underwent a second surgical operation,
including refractory sphenoid sinusitis (15 patients), sphenoidal
mucoceles (2 patients), sphenoid sinus papilloma (2 patients),
fungal sphenoid sinusitis (1 patient), and sphenoid sinus carcinoma
(1 patient).
Preoperative examination
All patients underwent routine physical examinations
prior to surgery. There were no apparent surgical
contraindications. Nasal endoscopy and 64-slice computerized
tomography (CT) scan of the sinuses were performed using the
coronal, axial and sagittal positions. A total of 21 patients
underwent MRI examination, including 3 patients with refractory
sphenoid sinusitis and postoperative complications of pituitary
adenoma, 9 patients with sphenoid mucoceles, 1 patients with fungal
sphenoid sinusitis and having intracranial infection and fever, 3
patients with sphenoid sinus papilloma, 2 patients with sphenoid
sinus carcinoma, 1 patient with sphenoid sinus chordoma, 1 patient
with pituitary adenoma and 1 patient with olfactory neuroblastoma
with sphenoid sinus and intracranial invasion. MRI was only
performed for patients with sphenoid sinus tumors and when MRI was
of great significance in the diagnosis, scope and surgical guidance
of sphenoid sinus lesions. The development, location and expansion
of the sphenoid sinus were respectively determined. The operative
risk and the surgical plan for all patients were assessed.
Surgical procedure
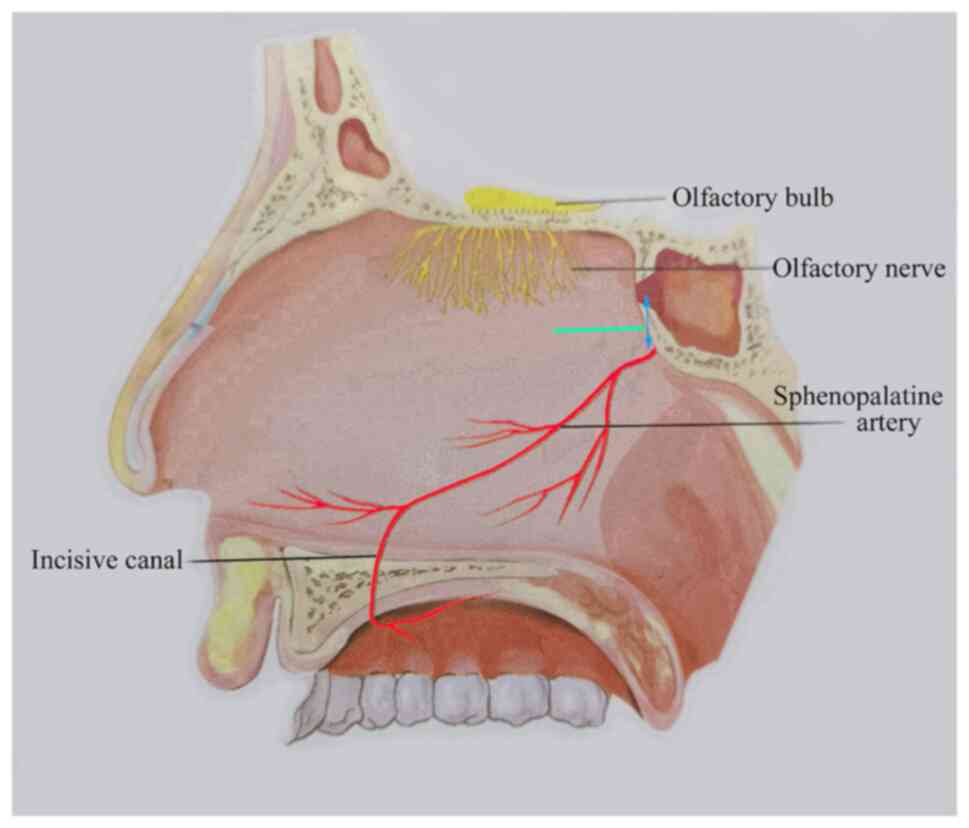
All patients underwent expanding bilateral sphenoid
sinus plasty under general anesthesia. Surgery was performed as
follows: With a 30˚ nasal endoscope (Karl Storz SE & Co. KG),
having conducted the external transfer of middle turbinate without
resection, the superior meatus, the nasal septum and the recessus
sphenoethmoidalis were fully exposed. After local
electrocauterization with the bipolar coagulation, an incision ~2
cm long (indicated by a green line in Fig. 1) was formed on the root mucosa of
the nasal septum 2 mm below the recessus sphenoethmoidalis or the
natural opening of sphenoid sinus. The mucoperiosteum was separated
and cotton pads were applied to protect the mucosal flaps. The
nasal septum fracture was separated but the contralateral nasal
mucosa was kept intact. The sphenoid ridge and exposed posterior
nasal septum were fully removed using a drill and the sphenoidal
intersinus septum was removed. The opening of sphenoid sinus was
ground to its bottommost part and the bilateral sphenoid sinus was
integrated into a single cavity. The intact nasal septum flaps were
reset to the sphenoidal cavity and the middle turbinate was
repositioned anatomically after complete removal of sphenoid sinus
lesions.
Improvements of surgical operation: A unilateral
incision or bilateral approach can be used. Tumors should be
thoroughly resected. The contralateral side may not need a
transverse incision. Insertion into the surgical operation cavity
through the recessus sphenoethmoidalis is suitable, which can fully
expose the lesions and is minimally invasive. When removing the
lateral lesions of the sphenoid sinus, a 30˚ or 45˚ endoscope can
be placed in the contralateral cavity to expose and operate in a
safe and convenient way. To reduce the surgical trauma, a bilateral
transverse incision can be avoided. We have adopted the above
methods on patients with sphenoid sinus tumors.
Patient follow-up
Patients were followed up for 6-53 months, with a
median follow-up time of 16.5 months. The first nasal cleaning was
performed 1 week post-surgery. Local cleaning using a nasal
endoscopic was performed at an interval of 1-2 weeks according to
the local recovery of the surgical cavity until a complete
regeneration of the mucosal epithelization in the sphenoid sinus
and the opening.
Statistical analysis
SPSS 19.0 (IBM Corp.) was used for statistical
analysis. Continuous variables were expressed as mean (range) or
median (range) and compared using Student's t-test or the Wilcoxon
rank-sum test. Categorical variables were expressed as frequency
(percentage) and analyzed using the χ2 test or, where
the expected count in >20% of cells was <5. Fisher's exact
test was used to analyze categorical variables. P<0.05 was
considered to indicate a statistically significant difference.
Results
A total of 15 patients with refractory sphenoid
sinusitis were considered to be cured with a well opened sphenoid
sinus orifice and clean cavity. The sphenoidal lesions were
completely removed in 9 patients with sphenoidal mucoceles, 8
patients with fungal sphenoid sinusitis (including 1 patient whose
treatment was complicated by intracranial infection and fever as
well as receiving postoperative antifungal therapy for 3 months,
with intracranial lesion absorption observed), 3 patients with
sphenoidal papilloma, 2 patients with post-sphenoidal nostril polyp
and 1 patient with hypophysoma. Two patients with sphenoidal
carcinoma and one patient with sphenoidal chordoma were treated
using endoscopic resection and postoperative radiotherapy. A
patient with olfactory neuroblastoma with sphenoid sinus and
intracranial invasion was treated with combined neurosurgery,
lesion resection and postoperative radiotherapy.
In the 42 patients, symptoms were relieved after
operation except preoperative hyposmia in 2 patients and impaired
vision in 1 patient with no obvious improvement. There were no
complications, such as arterial nosebleed, olfactory decline or
perforation of the nasal septum. The postoperative mucosal
epithelization of the operation cavity regenerated well. The total
time for regeneration and epithelization was 6-14 weeks (mean, 8.6
weeks). Patients with sphenoid sinus carcinoma and sphenoid sinus
chordoma underwent radiotherapy after surgical operation. Two
patients with sphenoid sinus carcinoma were followed up for 10 and
14 months, with no recurrence. One patient with sphenoid chordoma
was followed up for 10 months, without recurrence. One patient with
olfactory neuroblastoma with sphenoid sinus and intracranial
invasion was followed up for 8 months, without recurrence.
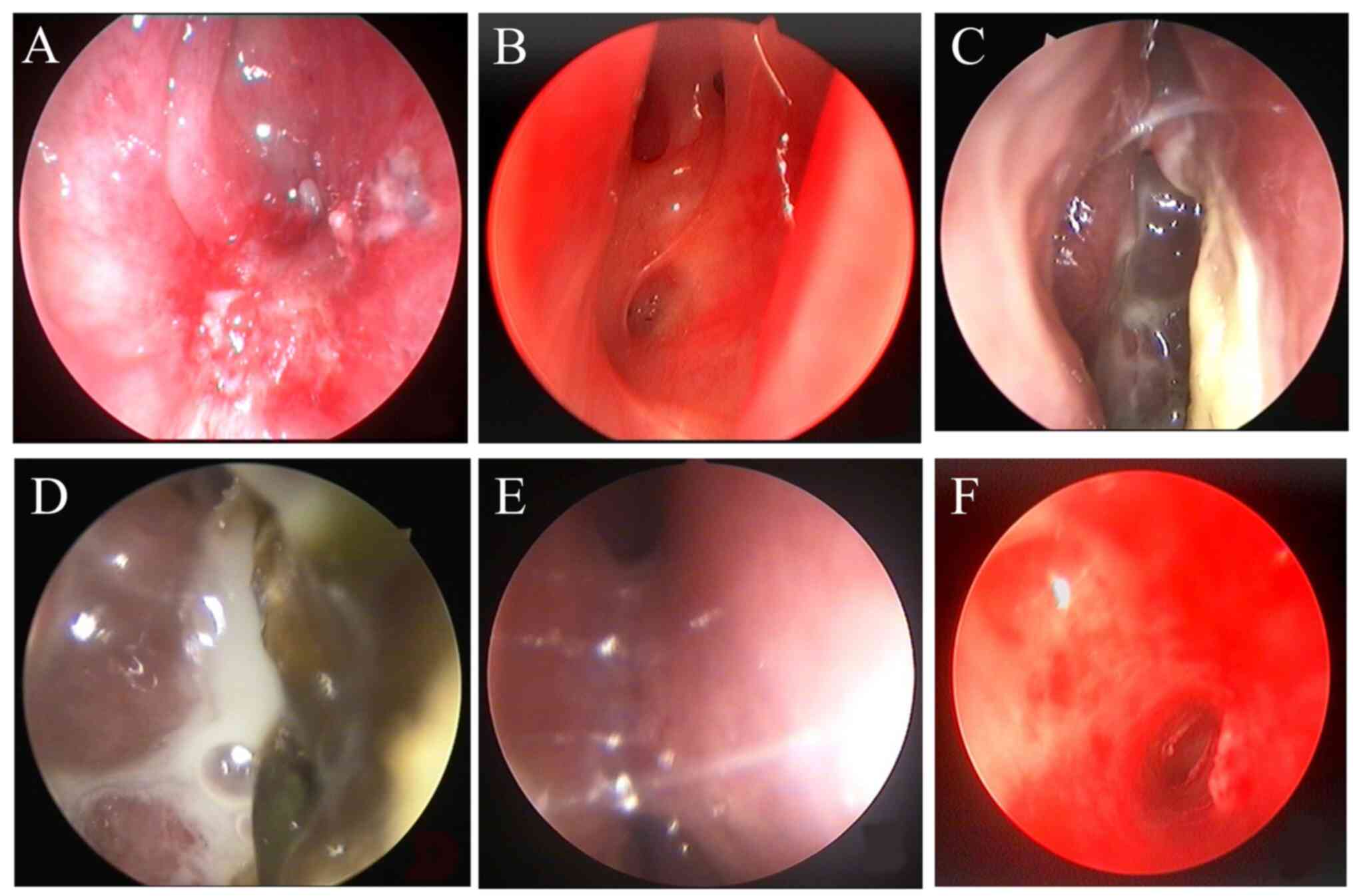
Endoscopic sinus reexamination demonstrated that the
sphenoid sinus orifice was well opened and no sphenoid sinus
orifice closure was observed in any of the 42 patients. The data
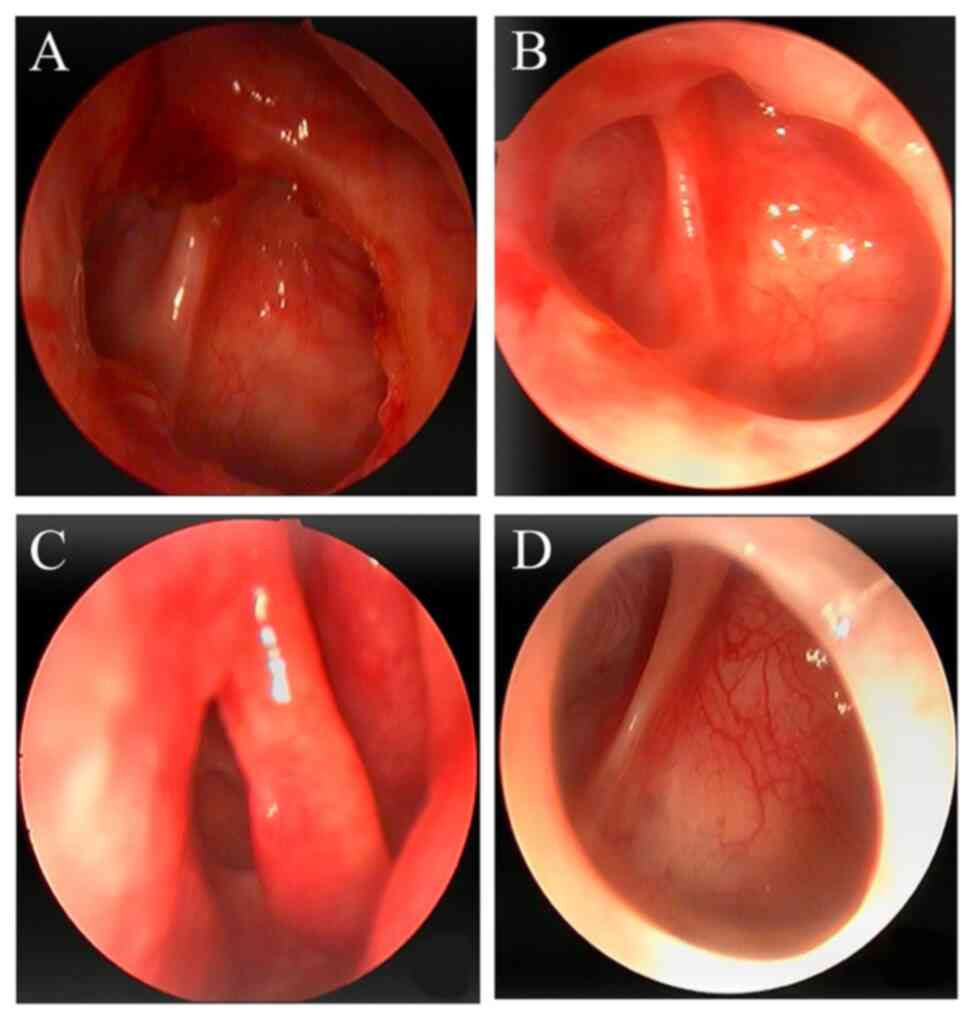
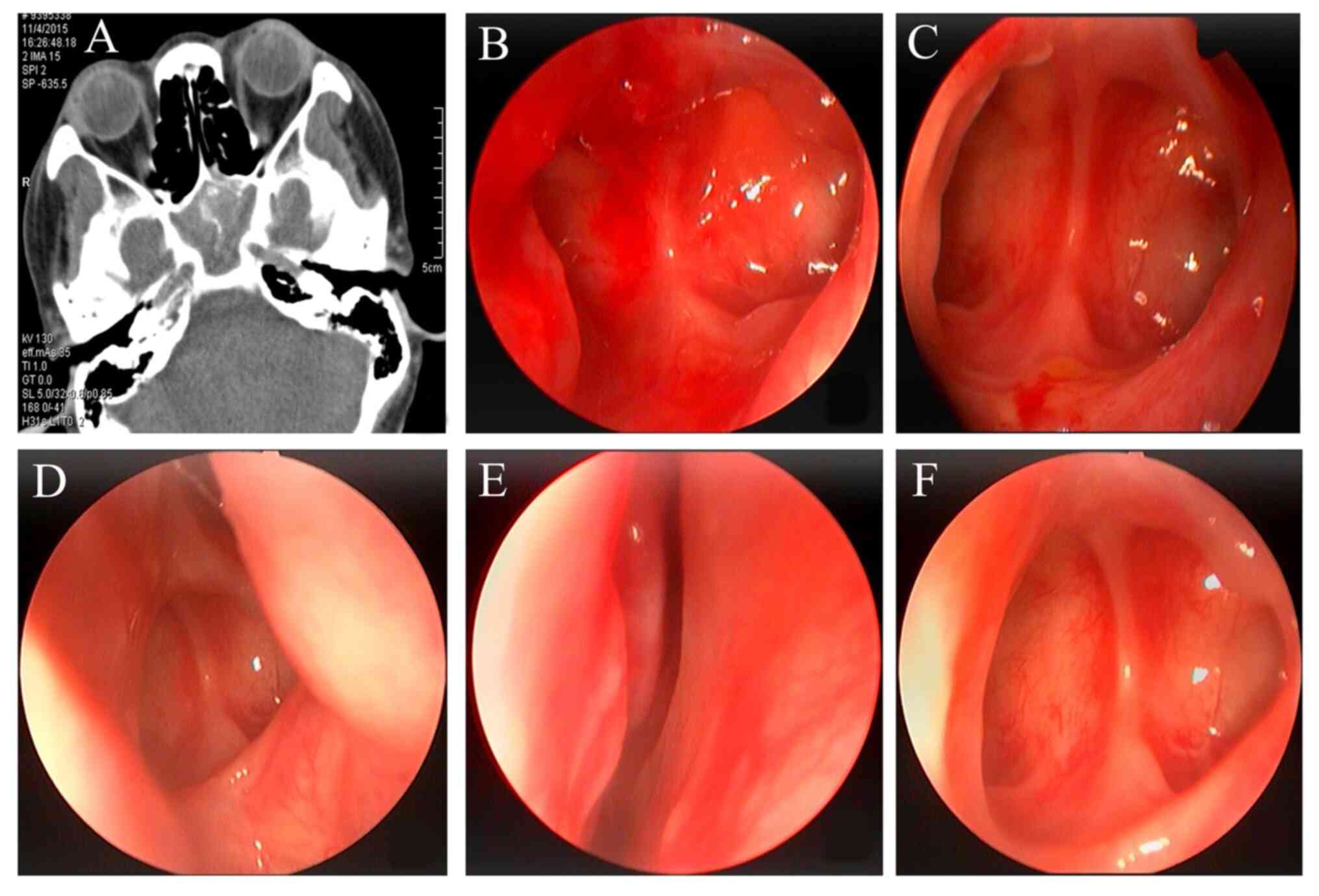
before and after surgical operation and the follow-up results were
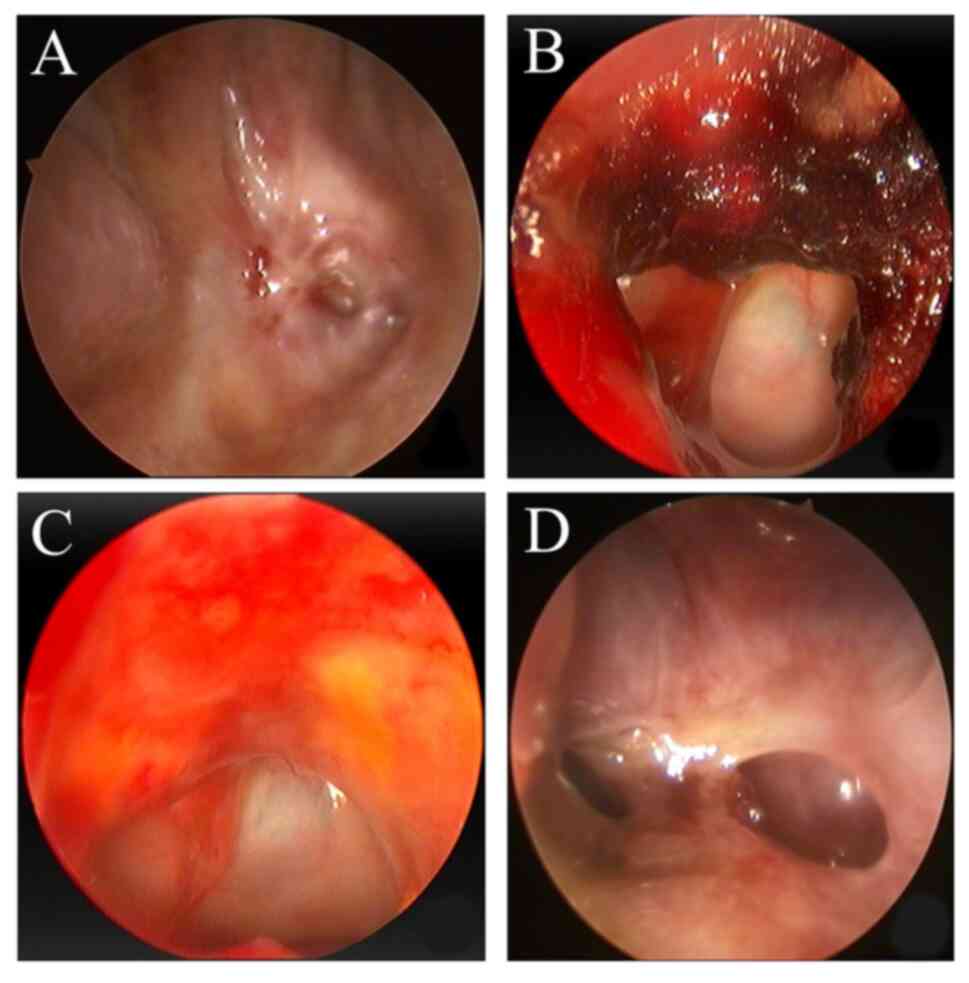
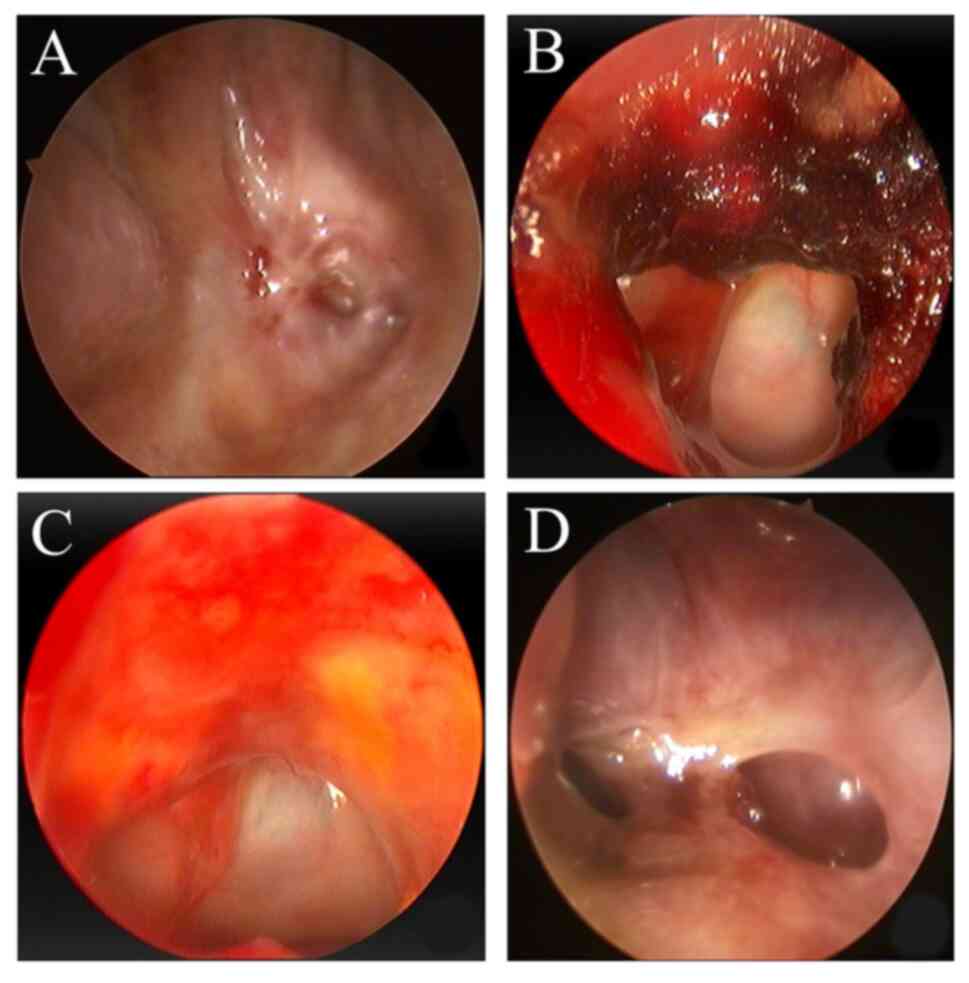
presented in the figures. Fig. 2
showed the nasal endoscopic images of sphenoid sinus opening
failure. The endoscopic follow-up of a patient with sphenoidal
mucocele was shown in Fig. 3,
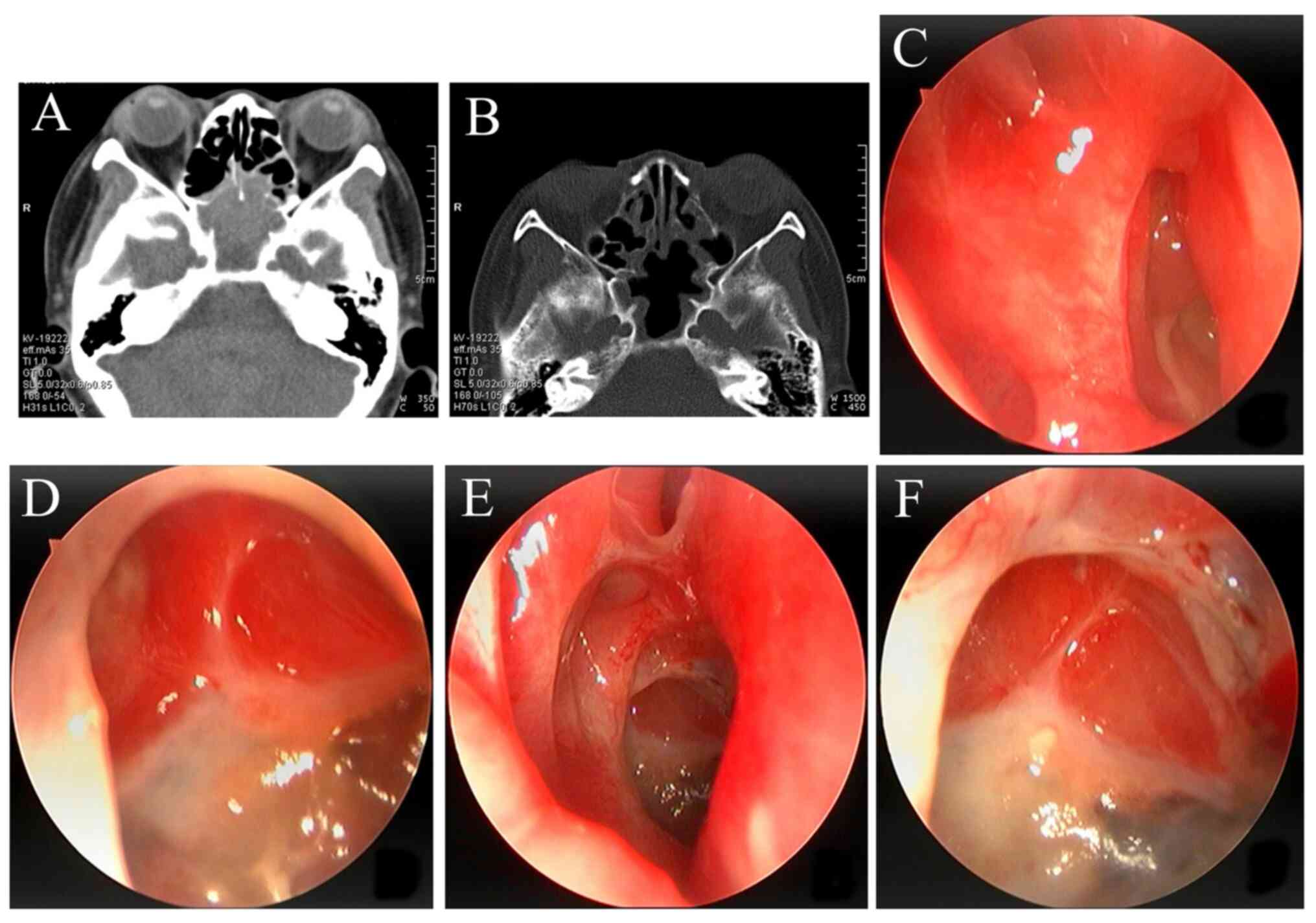
follow-up of a patient with fungal sphenoid sinusitis with CT and
nasal endoscopy was shown in Fig.
4 and the follow-up results of a patient with refractory
sphenoid sinusitis were shown in Fig.
5. The benign lesions were treated with the one-sided approach.
The bilateral exposure and surgery were applied for sphenoid sinus
tumor lesions, and the follow-up results of a patient with sphenoid
sinus carcinoma using CT and nasal endoscopy were shown in Fig. 6.
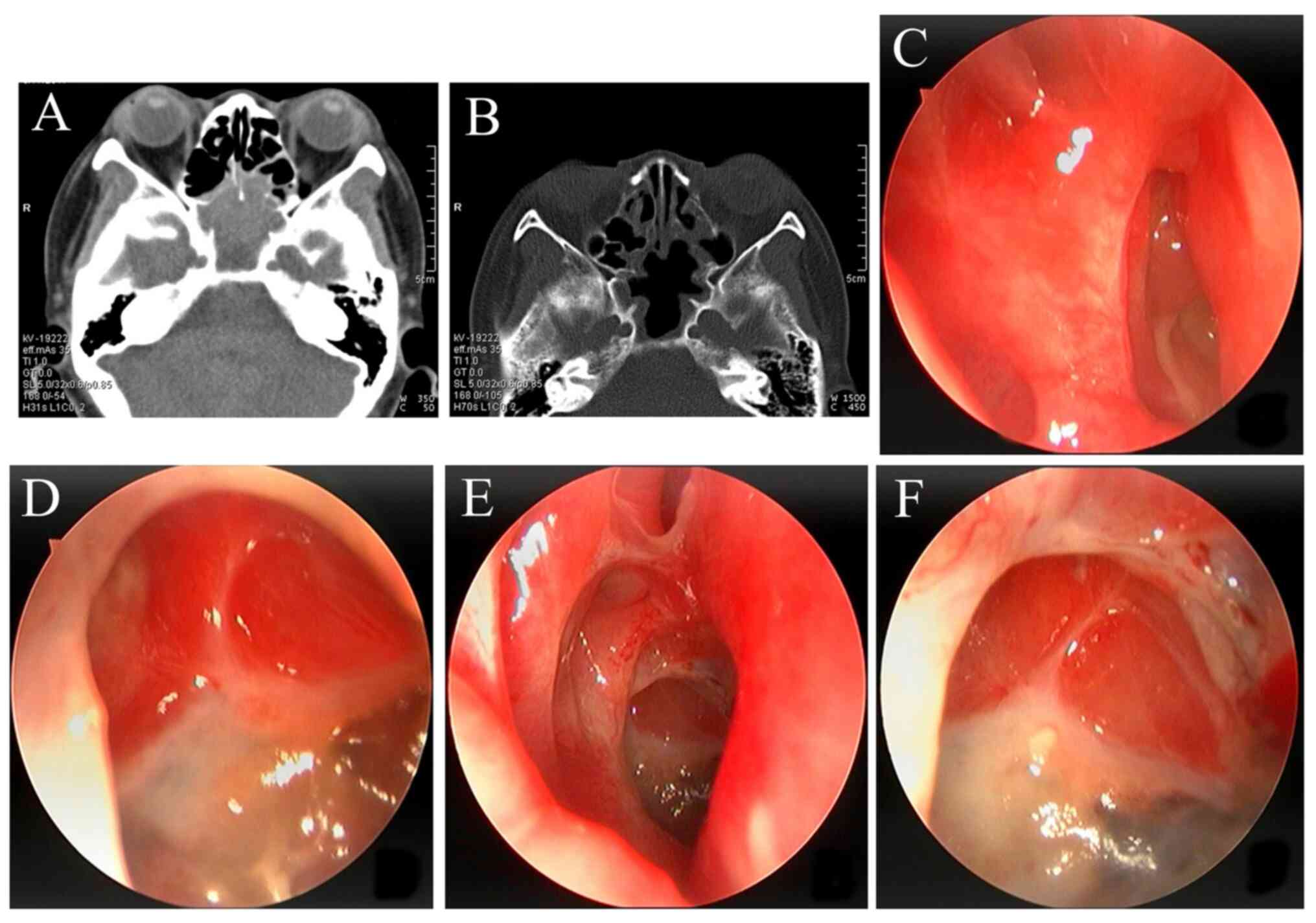
 | Figure 3Endoscopic follow-up of 1 patient with
sphenoidal mucocele. (A) Image 2 weeks after surgery, demonstrating
bilateral sphenoid sinus cavity fusion, good opening, a clean sinus
cavity, mild hyperemia and edema. (B) Image 4 weeks after surgery,
demonstrating bilateral sphenoid sinuses which were well opened,
that the opening of the ostium was low enough, the sinus cavity was
clean, the mucosa was smooth and there were no obvious hyperemia
and edema. (C) Image 8 weeks after surgery, demonstrating that the
sphenoid sinus was well opened and the nasal structure was well
preserved. (D) Image 15 months after surgery, demonstrating
bilateral sphenoid sinus cavity fusion, good opening, and a clean
sinus cavity and epithelial mucosa. |
 | Figure 4Follow-up of 1 patient with fungal
sphenoid sinusitis with CT and nasal endoscopy. (A) Preoperative
CT, demonstrating bilateral thickening of bone wall and plaque or
cord shaped calcification. (B) Endoscopy image 2 weeks after
surgery, demonstrating bilateral sphenoid sinus cavity fusion, good
opening, a clean sinus cavity, mucosal congestion and edema. (C)
Endoscopy image 4 weeks after surgery, demonstrating bilateral
sphenoid sinuses which were well opened, that the opening of the
ostium was low enough and that the mucosa was smooth. (D) Endoscopy
image 8 weeks after surgery (left sinus), demonstrating bilateral
sphenoid sinus cavity fusion, good opening, and a clean sinus
cavity and epithelial mucosa. (E) Endoscopy image 8 weeks after
surgery (right sinus), demonstrating that the right mucosa of the
nasal septum was intact and the right nasal cavity structure had no
disturbance. (F) Endoscopy image 12 months after surgery,
demonstrating local epithelization, a clean cavity and the lowest
point of the sphenoid sinus opening being basically flush with its
bottommost part. There was no apparent narrowing of the ostium. |
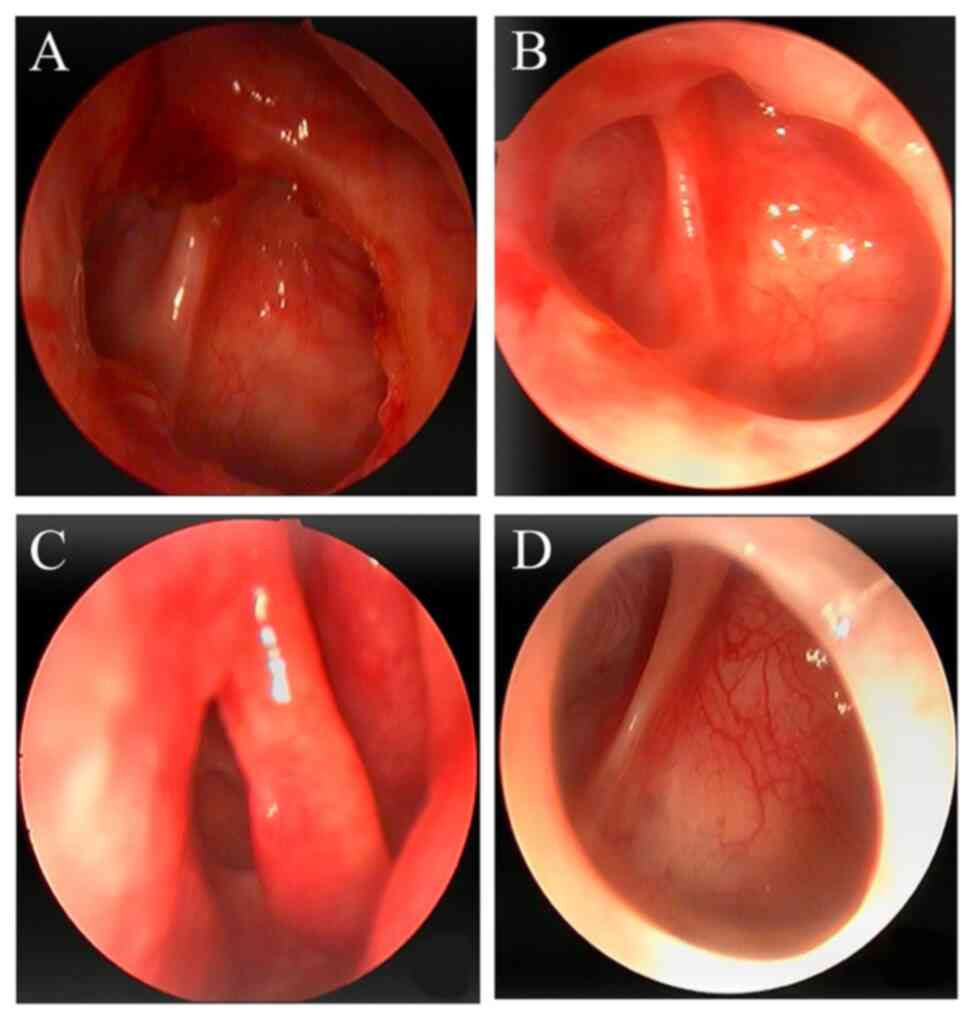
 | Figure 5Follow-up results of 1 patient with
refractory sphenoid sinusitis. (A) Pre-operation sphenoid sinus
orifice atresia. (B) Image 2 weeks after surgery, demonstrating
that the cavity was attached to a small amount of NasoPore at the
expanding apertura sinus sphenoidalis, which was not removed, to
avoid interfering with the regenerating process of the mucosa. (C)
Image 6 weeks after surgery, demonstrating that the operation
cavity and bilateral sphenoid sinuses were well opened, the opening
of the ostium was low enough, the operation cavity was clean, the
mucosa was smooth, slight hyperemia and edema. (D) Image 53 months
after surgical operation, demonstrating apertura sinus
sphenoidalis, bilateral sphenoid sinuses were still open, the sinus
cavity was clean and the mucosa was epithelialized. |
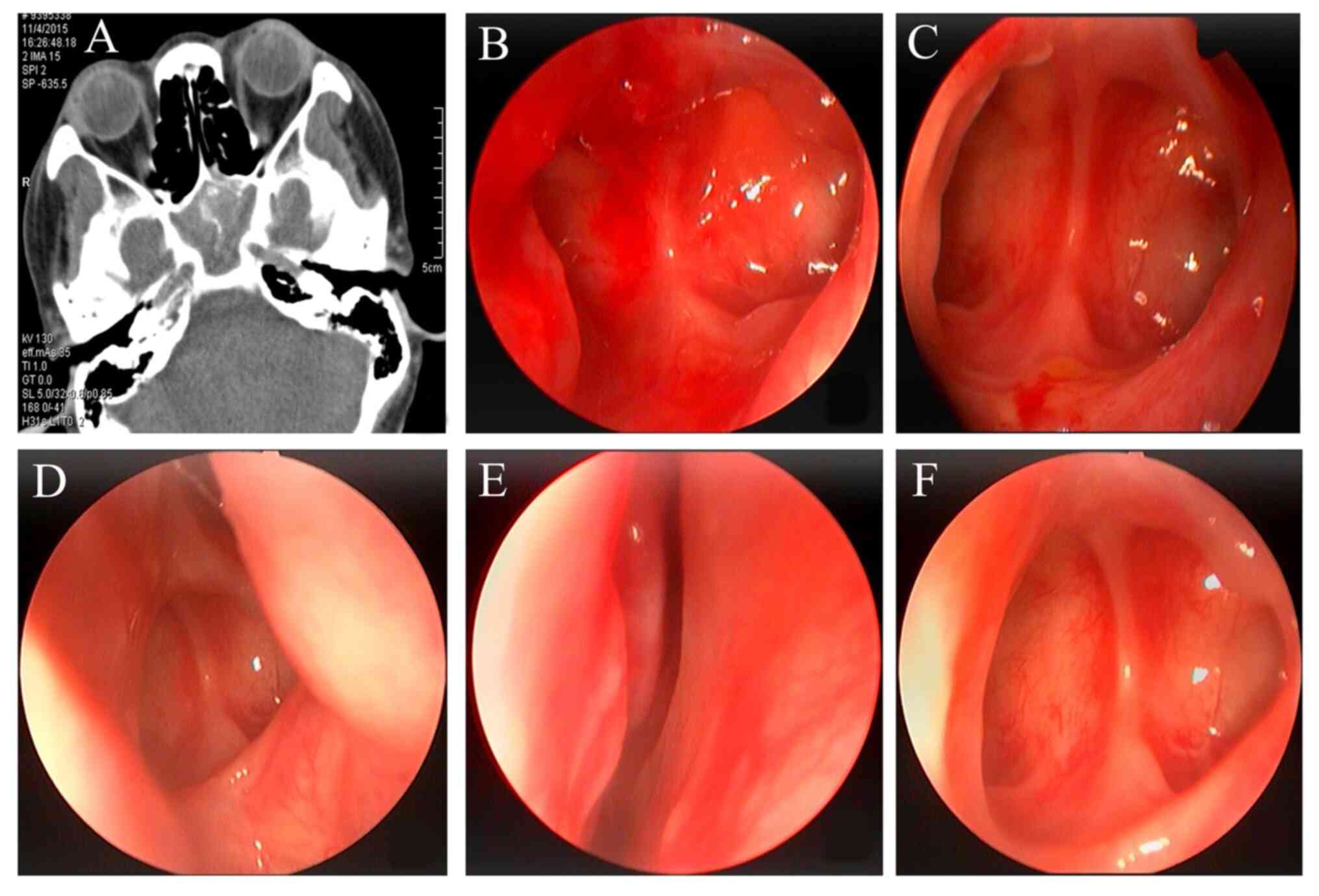
 | Figure 6Follow-up of 1 patient with sphenoid
sinus carcinoma using CT and nasal endoscopy. (A) Preoperative CT,
demonstrating That the sphenoid sinus cavity was filled with soft
tissue. (B) CT image 12 weeks after surgery, demonstrating slight
swelling of nasal sinus mucosa and no obvious tumor residue. (C)
Endoscope image 12 weeks after surgery (right sinus, during
radiotherapy), demonstrating that the right sphenoid sinus was
open, the mucosa of the sinus cavity was obviously congested and
edematous, and that no obvious tumor remained. (D) Endoscopy image
12 weeks after surgery (left sinus, during radiotherapy),
demonstrating that the left sphenoid sinus was well opened, the
sinus mucosa was congested and swollen, and that no obvious tumor
remained. (E) Endoscope image 12 months after postoperative
radiotherapy (right sinus), demonstrating that the right sphenoid
sinus was well opened, the sinus mucosa was slightly congested and
swollen, and no obvious tumor remained. (F) Endoscope image 12
months after postoperative radiotherapy (left sinus), demonstrating
that the left sphenoid sinus was well opened, the sinus mucosa was
slightly congested and swollen, and no obvious tumor remained. |
The characteristics of patients treated with
expanding bilateral sphenoid sinus plasty and traditional sphenoid
sinus plasty were compared (Table
I). The data demonstrated that procedure length was
significantly longer and hospital stay was significantly shorter
observed in patients treated using expanding bilateral sphenoid
sinus plasty compared with those treated using traditional sphenoid
sinus plasty. There was no significant difference in intraoperative
bleeding volume. With regards complications, the occurrence rate of
arterial nosebleed (0 vs. 5), nasal cavity adhesion (2 vs. 8),
olfactory decline (0 vs. 5) and perforation of nasal septum (0 vs.
2) were markedly reduced in patients with expanding bilateral
sphenoid sinus plasty compared with the traditional group; however,
no statistical significance was demonstrated. Moreover, no sphenoid
sinus orifice closures were observed postoperatively, no revision
operations were performed and the epithelialization time was
significantly shorter in patients treated using expanding bilateral
sphenoid sinus plasty compared with the traditional group.
 | Table IComparing expanding bilateral sphenoid
sinus plasty with traditional sphenoid sinus plasty. |
Table I
Comparing expanding bilateral sphenoid
sinus plasty with traditional sphenoid sinus plasty.
| Characteristic | Expanding bilateral
sphenoid sinus plasty (n=42) | Traditional sphenoid
sinus plasty (n=64) | P-value |
|---|
| Age, mean (range),
years | 45.7 (22-75) | 43.4 (18-78) | NA |
| Sex, n (%) | | | 0.563 |
|
Male | 26 (61.9) | 36 (56.3) | |
|
Female | 16 (38.1) | 28 (43.7) | |
| Duration of
follow-up, median (range), months | 16.5 (6-53) | 20.1 (4-62) | NA |
| Length of the
procedure, mean (range), min | 116 (80-242) | 90 (60-281) | 0.001 |
| Average bleeding
volume, mean (range), ml | 165 (90-550) | 127 (70-860) | 0.071 |
| Hospital stay, mean
(range), days | 4.3 (3-9) | 5.5 (3-12) | <0.001 |
| Complications, n
(%) | | | 0.567 |
|
Arterial
nosebleed | 0 (0.0) | 5 (7.8) | |
|
Nasal cavity
adhesion | 2 (4.8) | 8 (12.5) | |
|
Olfactory
decline | 0 (0.0) | 5 (7.8) | |
|
Perforation
of nasal septum | 0 (0.0) | 2 (3.1) | |
| Sphenoid sinus
orifice closure postoperative, n (%) | 0 (0.0) | 8 (12.5) | 0.021 |
| Revision operations,
n (%) | 0 (0.0) | 6 (9.3) | 0.079 |
| Epithelialization
time, mean (range), weeks | 8.6 (6-14) | 11. 2(8-16) | <0.001 |
Discussion
The anatomical position of the sphenoid sinus is
considered special in view of its proximity to vital anatomical
structures, such as the internal carotid artery, sella turcica,
pituitary, optic nerve, sinus cavernosus, visual cross and the
third to the sixth cranial nerve (13-15).
This poses a challenge for the clinical diagnosis and treatment of
sphenoidal disease. In the present study, a conventional nasal
endoscopic examination was carried out and the imaging pictures
were carefully analyzed. The scope of the lesion in relation to
surrounding tissues was assessed. Blind operation was avoided
during surgical procedures and the sphenoid sinus lesion was
removed as thoroughly as possible.
Recurrence of refractory sphenoid sinusitis is the
most common side effect encountered in sphenoidal disease after
surgical operation (4). Patients
commonly have characteristics such as stenosis of the sphenoid
sinus orifice, small volume of chamber, severe inflammation of the
sinus mucosa and easy recurrence after surgery (16). It is essential to fully open the
apertura sinus sphenoidalis and protect the mucosa of the surgical
cavity during surgical operation, to avoid postoperative scar
stenosis of the sinus orifice (8).
In the present study, expanding bilateral sphenoid sinus plasty was
used to open the sphenoid sinus orifice while protecting the mucosa
of the surgical cavity. The apertura sinus sphenoidalis was higher
than the bottom wall of the sinus; therefore, the posterior of the
nasal septum and the anterior inferior wall of sphenoid sinus were
removed during surgery and the opening of the sphenoid sinus was
drilled to its bottommost part, which enabled the bilateral
sphenoid sinus to be completely opened to facilitate drainage.
Furthermore, in the long-term post-nasal endoscopic treatment, it
was observed that the sphenoid sinus opening frequently appeared in
various degrees of annular reduction post-surgery. Based on the
present study, it is suggested that the fenestration should not be
too small. Meanwhile, after the bilateral sphenoid sinus was fully
opened, the well-preserved nasal septum mucosal flaps could be
reset to the sphenoidal cavity, which promoted the rapid
epithelization of the mucous membrane in the sphenoid cavity,
avoided local scar formation and reduced postoperative recurrence
or fenestration atresia.
Safety during surgical operation must be considered
during the treatment of sphenoid sinus lesions (17). Hence, to avoid serious surgical
complications, the surgeon must not blindly clamp and drag the
lesion of the lateral wall or scratch the mucous membrane of the
lateral wall (18,19). In the present study, angle nasal
endoscopy was combined with expanding bilateral sphenoid sinus
plasty to address sphenoid sinus lesions. The surgical field was
fully exposed and clearly visible, which allowed operators to avoid
accidental injuries of important anatomical structures. Most
surgical operations were performed in the midline or medial, which
features high security, and thus, damage to the lateral internal
carotid artery and optic nerve of sphenoid sinus could be avoided
(20). A transverse incision of
the mucoperiosteum at the root of the nasal septum was adopted to
preserve the sphenopalatine artery pedicle and its nasal septum
branches and to maintain the integrity of olfactory epithelium,
especially the mucosa of the septal olfactory strip (21,22).
This also reduced the risk of postoperative nosebleed, perforation
of the nasal septum and olfactory disturbance. So, the expanding
bilateral sphenoid sinus plasty is mainly characterized by avoiding
the medial olfactory band, sphenopalatine artery and lateral
internal carotid artery, and optic nerve, and improving the safety
of the operation while reducing postoperative complications.
The most important aspect of this surgical method is
to achieve full exposure of the operative field and create a better
condition for the full-treatment of the sphenoid sinus lesion,
which can reduce the recurrence probability of the lesion. For
better gasification of the sphenoid sinus, some of the air chambers
can be extended to the root of the pterygoid process to form the
lateral recess of the sphenoid sinus (23). Usually, to enable a clear exposure
and ensure safer and more convenient surgical operation, a 30˚ or
45˚ endoscope is used to clear the lateral lesions of the sphenoid
sinus (24). The present study
made a preliminary evaluation of how to improve the surgical
procedure, which is mainly embodied in a one-sided or double-sided
approach. The bilateral approach is mainly applicable for sphenoid
sinus tumors. It follows the principle of completely resecting the
tumor and minimizing surgical trauma. The operation space increases
with the full exposure of the sphenoid sinus cavity. The operating
assistant can help aspirate the blood and expose the surgical field
from another side, which enables the surgeon to operate with both
hands simultaneously. Surgeons need to master local anatomy and
surgical approach, as well as specialize in analyzing sphenoid
sinus lesions and the imaging of morphological changes (25-27).
In the present study, the normal and healthy mucous
membranes of the nasal cavity, the sphenoid sinus, and the nasal
septum were retained as much as possible (28). The mucosal flap technique was
applied to protect the mucosa of the nasal septum; the nasal septum
mucosal flaps were reset to the sphenoidal cavity; the nasal mucosa
of the opposite side was kept intact; the minimum amount of the
mucosa of the sphenoid sinus was removed and the turbinate was
kept; and the excessive electrocauterization of the bleeding
mucosa, particularly the mucosal margins, was avoided. The incision
and separation of the nasal septum mucoperiosteum should be kept
neat so as to not damage the vascular pedicle and nasal septum
olfactory band. This method can form sufficiently large mucosal
flaps to retain the anatomical structure of the nasal cavity and
sphenoid sinus, and boost the healing of the mucous membrane after
surgery. The contralateral nasal mucosa is not easily damaged once
the osseous nasal septum is broken. Keeping the contralateral nasal
mucosa intact can avoid the disturbance of its nasal cavity and
sinus function. Furthermore, subperiosteal peeling anatomy is
beneficial for the protection of the nasal mucosa and it can
improve the long-term healing ability of nasal cavity, which can
reduce the forming of scab and shorten the process of epithelial
transformation of the nasal cavity and sinuses. It is necessary to
examine and clear the postoperative cavity under the endoscope
periodically for quick recovery post-surgical operation (29). Regular endoscopic follow-up was
performed after the operation. If the operational areas under the
nasal endoscope are smooth, there is no obvious hyperemia and edema
in the mucosa, no obvious residual lesion and the ostium of the
sinus is well opened, then it is considered that epithelialization
was successful. In the present study, the mean time of mucosa
epithelial transformation for patients was ~8.6 weeks post-surgery,
which was significantly shorter compared with traditional sphenoid
sinus plasty-treated patients.
For certain simple cases with better gasification of
the sphenoid sinus and no obvious anatomical variation, the trauma
using this surgical method may be larger. The incision and the
particular method used here may produce excessive damage. However,
expanding bilateral sphenoid sinus plasty is necessary for patients
with refractory sphenoid sinusitis, especially for malignant tumors
of the sphenoid sinus (30). The
present study is a case series, thus certain limitations and
shortcomings exist. A larger study population recruited in a
prospective or randomized fashion with validated outcome measures
would allow for a more conclusive analysis of the benefits of
expanding bilateral sphenoid sinus plasty for sphenoid sinus
diseases.
In summary, the advantages of the expanding
bilateral sphenoid sinus plasty, as indicated by the present study,
are as follows: i) It enables a fully exposed and clear surgical
field, which leads to the complete removal of lesions in the
sphenoid sinus; ii) it can fully open the apertura sinus
sphenoidalis and protect the mucous membrane of the operation
cavity to reduce recurrence; iii) it can promote rapid
epithelization of the mucosa of the sphenoid sinus cavity and the
opening postoperatively; iv) higher safety and no injury of
internal carotid artery and optic nerve; v) postoperative
complications are minimal, thus the risk of postoperative
nosebleed, perforation of nasal septum and olfactory disorder is
reduced; and vi) the follow-up treatment is intuitionistic and
convenient. In the present study, no sphenoid sinus orifice closure
was identified in patients during follow-up. The results of the
present study indicated that this procedure is suitable for use in
most cases of sphenoid sinus lesions. The same surgical incision
and sphenoid sinus exposure also provides sufficient surgical
exposure for transsphenoid pituitary adenoma surgery and
transsphenoid treatment of suprasaddle and parasellar lesions.
Currently, preliminary adoption of this method has been achieved in
the Neurosurgery Department of our hospital (5).
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the China
Postdoctoral Science Foundation (grant no. 2017M613438) and by the
Medical School of Nanjing University Affiliated Jinling Hospital
(grant no. 2017001).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
FX, YC and RW contributed to the study design and
performed the funding acquisition. FX, XY and YC contributed to
data collection and wrote the manuscript. MW and JJ performed data
validation and retouched the manuscript. XF, YC and MW confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committees of
the Medical School of Nanjing University Affiliated Jinling
Hospital (approval no. 2012NKY011). Written informed consent was
obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen L, Jiang L, Yang B and Subramanian
PS: Clinical features of visual disturbances secondary to isolated
sphenoid sinus inflammatory diseases. BMC Ophthalmol.
17(237)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
De Los Reyes KM, Gross BA, Frerichs KU,
Dunn IF, Lin N, Rincon-Torroella J, Annino DJ and Laws ER:
Incidence, risk factors and management of severe
post-transsphenoidal epistaxis. J Clin Neurosci. 22:116–122.
2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
ZA Lang, HB Sheng and AW B: Long-term
olfactory dysfunction after single-nostril endoscopic transnasal
transsphenoidal pituitary adenoma surgery. J Clin Neurosci.
82:166–172. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Van Zele T, Pauwels B, Dewaele F, Gevaert
P and Bachert C: Prospective study on the outcome of the sphenoid
drill out procedure. Rhinology. 56:178–182. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cheng Y, Xue F, Wang TY, Ji JF, Chen W,
Wang ZY, Xu L, Hang CH and Liu XF: Analyses and treatments of
postoperative nasal complications after endonasal transsphenoidal
resection of pituitary neoplasms. Medicine (Baltimore).
96(e6614)2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Leight WD and Leopold DA: Sphenoid
‘drill-out’ for chronic sphenoid rhinosinusitis. Int Forum Allergy
Rhinol. 1:64–69. 2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Subspecialty Group of Rhinology, Editorial
Board of Chinese Journal of Otorhinolaryngology Head and Neck
Surgery; Subspecialty Group of Rhinology, Society of
Otorhinolaryngology Head and Neck Surgery, Chinese Medical
Association. Guidelines for diagnosis and treatment of chronic
rhinosinusitis (2012, Kunming). Zhonghua Er Bi Yan Hou Tou Jing Wai
Ke Za Zhi. 48:92–94. 2013.PubMed/NCBI(In Chinese).
|
|
8
|
Eloy JA, Marchiano E and Vázquez A:
Extended endoscopic and open sinus surgery for refractory chronic
rhinosinusitis. Otolaryngol Clin North Am. 50:165–182.
2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Stammberger H and Posawetz W: Functional
endoscopic sinus surgery. Concept, indications and results of the
Messerklinger technique. Eur Arch Otorhinolaryngol. 247:63–76.
1990.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Toffel PH, Aroesty DJ and Weinmann RH IX:
Secure endoscopic sinus surgery as an adjunct to functional nasal
surgery. Arch Otolaryngol Head Neck Surg. 115:822–825.
1989.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lubbe DE, Douglas-Jones P, Wasl H, Mustak
H and Semple PL: Contralateral precaruncular approach to the
lateral sphenoid Sinus-A case report detailing a new, multiportal
approach to lesions, and defects in the lateral aspect of
well-pneumatized sphenoid sinuses. Ear Nose Throat J. 99:62–67.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Huang Q, Zhou B, Cui SJ and Li YC: The
application of endoscopic strategy and approaches to treat sphenoid
sinus inflammatory diseases. Lin Chuang Er Bi Yan Hou Tou Jing Wai
Ke Za Zhi. 30:1265–1270. 2016.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
13
|
Burke MC, Taheri R, Bhojwani R and Singh
A: A practical approach to the imaging interpretation of sphenoid
sinus pathology. Curr Probl Diagn Radiol. 44:360–370.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Turkdogan FT, Turkdogan KA, Dogan M and
Atalar MH: Assessment of sphenoid sinus related anatomic variations
with computed tomography. Pan Afr Med J. 27(109)2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Liu J, Liu S, Heng X, Fei C, Wei Y, Zhang
J, Zhang Z and Tang Y: The values of thin sections and
three-dimensional reconstruction in the sellar region. World
Neurosurg. 78:510–515. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cingi C, Bayar Muluk N and Lee JT: Current
indications for balloon sinuplasty. Curr Opin Otolaryngol Head Neck
Surg. 27:7–13. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Samandouras G, Kerr RS and Milford CA:
Minimally invasive biopsy of parasellar lesions: Safety and
clinical applications of the endoscopic, transnasal approach. Br J
Neurosurg. 19:338–344. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dehdashti AR, Ganna A, Karabatsou K and
Gentili F: Pure endoscopic endonasal approach for pituitary
adenomas: Early surgical results in 200 patients and comparison
with previous microsurgical series. Neurosurgery. 62:1006–1017.
2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Laury AM, Oyesiku NM, Hadjipanayis CG,
Delgaudio JM and Wise SK: Incidental sinonasal findings identified
during preoperative evaluation for endoscopic transsphenoidal
approaches. Am J Rhinol Allergy. 27:202–205. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wormald PJ and McDonogh M: ‘Bath-plug’
technique for the endoscopic management of cerebrospinal fluid
leaks. J Laryngol Otol. 111:1042–1046. 1997.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ng YH and Sethi DS: Isolated sphenoid
sinus disease: Differential diagnosis and management. Curr Opin
Otolaryngol Head Neck Surg. 19:16–20. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Eravcı FC, Ceylan A, Göcek M, İlerı F,
Uslu SS, Yılmaz M and Kızıl Y: Isolated sphenoid sinus pathologies:
A series of 40 cases. Turk J Med Sci. 47:1560–1567. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Özer CM, Atalar K, Öz II, Toprak S and
Barut Ç: Sphenoid sinus in relation to age, gender, and
cephalometric indices. J Craniofac Surg. 29:2319–2326.
2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Orhan I, Ormeci T, Bilal N, Sagiroglu S
and Doganer A: Morphometric analysis of sphenoid sinus in patients
with nasal septum deviation. J Craniofac Surg. 30:1605–1608.
2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Yilmaz N, Kose E, Dedeoglu N, Colak C,
Ozbag D and Durak MA: Detailed anatomical analysis of the sphenoid
sinus and sphenoid sinus ostium by cone-beam computed tomography. J
Craniofac Surg. 27:e549–e552. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ahmadipour Y, Lemonas E, Maslehaty H,
Goericke S, Stuck BA, El Hindy N, Sure U and Mueller O: Critical
analysis of anatomical landmarks within the sphenoid sinus for
transsphenoidal surgery. Eur Arch Otorhinolaryngol. 273:3929–3936.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gibelli D, Cellina M, Gibelli S, Cappella
A, Oliva AG, Termine G, Dolci C and Sforza C: Relationship between
sphenoid sinus volume and protrusion of internal carotid artery and
optic nerve: A 3D segmentation study on maxillofacial CT-scans.
Surg Radiol Anat. 41:507–512. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kimple AJ, Leight WD, Wheless SA and
Zanation AM: Reducing nasal morbidity after skull base
reconstruction with the nasoseptal flap: Free middle turbinate
mucosal grafts. Laryngoscope. 122:1920–1924. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kasle DA, Torabi SJ, Narwani V and Manes
RP: Medicare reimbursement for balloon catheter dilations among
surgeons performing high volumes of the procedures to treat chronic
rhinosinusitis. JAMA Otolaryngol Head Neck Surg. 146:264–269.
2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Hong HY, Li YN, Fan YP, Feng SY and Gao
JB: Management of sphenoidal sinus lesions by septal-assisted
approach: Surgical skills and advantages. J Huazhong Univ Sci
Technolog Med Sci. 35:558–562. 2015.PubMed/NCBI View Article : Google Scholar
|