Introduction
Acute liver failure (ALF) is a dramatic but rare
clinical syndrome marked by the sudden loss of hepatic function in
a person with no prior history of liver disease (1). The course of ALF is variable and the
mortality rate is high. Orthotopic liver transplantation (OLT) is
the most effective treatment for severe liver injury; however, the
widespread clinical application of liver transplantation is
restricted by the shortage of available donor livers and multiple
post-operative complications (2,3).
Due to its potential to promote liver regeneration with fewer
complications than the surgical approach, the use of stem cells
seems to be a promising method for the treatment of liver diseases
(4–6). Sources of exogenous stem/progenitor
cells that are currently under investigation in the context of
repair of liver injury include embryonic stem cells, bone
marrow-derived mesenchymal stem cells (MSCs), fat-derived
mesenchymal stem cells, fetal annex stem cells and endothelial
progenitor cells (EPCs) (7–10).
MSCs represent an attractive option for successful
stem-cell-based therapy for liver diseases due to their ready
accessibility, minimal invasiveness and rapid proliferation
(11). Furthermore, isolated MSCs
are multipotent and can differentiate into multiple lineage cell
types, including mesodermal cell lineages, such as osteoblasts,
adipocytes, chondroblasts, myocytes and cardiomyocytes, as well as
non-mesodermal cells, such as hepatocytes and neurocytes (12).
For therapeutic applications, it is important to
understand the potency and possible repair mechanisms of MSCs.
Previous studies have demonstrated that MSCs can differentiate into
functional hepatic cells and can also produce a series of growth
factors and cytokines able to suppress inflammatory responses,
reduce hepatocyte apoptosis and enhance hepatocyte functionality
(13,14). To date, few comparative studies of
different methods for the transplantation of bone marrow MSCs are
available. Furthermore, the association between the transplant
route and the transplant effect remains unclear. In animal
experiments, MSC transplantation typically proceeds via portal vein
injection, hepatic artery injection, peripheral vein injection,
intraperitoneal injection or local injections into the liver or
spleen. In clinical applications, the principal transplantation
methods are portal vein injection, hepatic artery injection and
peripheral vein injection; however, the optimal method for
transplanting MSCs has not yet been identified. Kuo et al
(11) demonstrated that both
MSC-derived hepatocytes and MSCs transplanted through either the
intrasplenic or the intravenous route can be engrafted into the
recipient liver and differentiate into functional hepatocytes.
Intravenous transplantation was found to be more effective in
rescuing liver failure than intrasplenic transplantation. Wang
et al (15) investigated
the therapeutic effects of bone mesenchymal stem cells (BMSCs) on
liver cirrhosis in rats induced by CCl4 via partial liver BMSC
transplant, tail vein transplant, partial liver transplant, spleen
transplant and portal vein transplant. Their results indicated that
partial liver BMSC transplantation is more effective in liver
cirrhosis than other transplantation routes. MSC transplantation
via the spleen contributed little to the restoration of liver
function as the transplanted cells usually grow in nodules, while
MSC transplantation by hepatic multi-site injection involves the
risk of damaging important liver vessels and causing severe
complications, including hemorrhea and portal hypertension. Xiong
et al (16) demonstrated
that the transplantation of MSCs into rats with cirrhosis via the
portal vein, hepatic artery and vena caudalis had similar curative
effects. Zhao et al (17)
indicated that the intravenous injection of MSCs was effective in
treating liver fibrosis compared with intrahepatic injection and
intraperitoneal injection. Cao et al (18) showed that the use of human
placenta MSCs (hPMSCs) prolonged the survival time of pigs with ALF
and that the left branch of the portal vein inside the liver
offered a superior route compared with the jugular vein pathway.
Kim et al (19) observed
that the transplantation of adipose tissue-derived stem cells
(ADSCs) into mice with ALF via a peripheral vein (tail vein)
resulted in more prominent liver function than via the portal vein
and direct liver parenchymal injection. Other studies have
investigated transplantation methods in other diseases. For
example, Li et al (20)
investigated the transplantation of human umbilical cord MSCs for
the treatment of acute tubular necrosis and showed that the cells
can survive in the kidneys, while the benefits of intravenous
injection and arterial injection in repairing the kidney were
similar. Zonta et al (21)
investigated the most effective route of administration
(intra-arterial vs. intravenous) to achieve immunomodulating
effects in experimental rat kidney transplantation and demonstrated
that the intra-arterial infusion of MSCs was more effective in
controlling acute rejection.
In this study, we compared the therapeutic effects
among 4 different protocols for MSC transplantation (hepatic artery
injection, portal vein injection, vena caudalis injection and
intraperitoneal injection) in the treatment of D-galactosamine
(D-gal)/lipopolysaccharide (LPS)-induced ALF. In addition, we aimed
to elucidate the possible mechanisms responsible for the different
outcomes according to the cell transplant site.
Materials and methods
Animals
Male Sprague-Dawley (SD) rats aged 3–4 weeks
(weighing 80–120 g) were used as BMSC donors. Male SD rats aged 8
weeks (weighing 250–280 g) were used as BMSC recipients. All the
rats were purchased from the Animal Center for Disease Control in
Urumqi, China and kept in the animal facility of the First
Affiliated Hospital of Xinjiang Medical University, Urumqi, China.
All procedures were approved by the Ethics Committee of the First
Affiliated Hospital of Xinjiang Medical University (permit no.
A-20100723015) in compliance with institutional animal care
guidelines.
Induction of ALF
The rats were injected intraperitoneally to induce
ALF with D-gal [1.4 g/kg/per injection bis in die (b.i.d.;
twice daily), 12-h interval between injections, Sigma-Aldrich Inc.,
St. Louis, MO, USA] combined with LPS (0.005%, 20 μg/kg,
Sigma-Aldrich Inc.). The extent of hepatic damage was evaluated by
a biochemical analysis of blood samples and a histological
examination of liver tissue taken from the sacrificed rats. The
rats were sacrificed using a mixture of amiodarone 2 ml + diazepam
2 ml + atropine 1 ml + physiological saline 5 ml (7.5 ml/kg). Liver
tissues were immediately stored at −80°C for molecular detection or
fixed in 10% (v/v) formalin for histological and
immunohistochemical analyses.
Isolation and culture of rat BMSCs
BMSCs obtained from SD rats were isolated and
cultured according to an established protocol (22). The rats were anesthetized with 8%
ketamine (4.0 ml/kg), the femurs and tibiae of the rats were
excised and the soft connective tissue was removed. The 2 ends of
the femurs and tibiae were excised and the cells of the bone marrow
were harvested by flushing the bone marrow cavity with complete
culture medium. The extract was filtered using a 200-mesh filter,
centrifuged for 5 min at 1,000 × g, resuspended in medium and
inoculated into a 25-cm2 culture dish containing
Dulbecco’s modified Eagle’s medium with low glucose (DMEM-LG; Gibco
Corp, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum
(FBS; HyClone, Logan, UT, USA), 1% penicillin/streptomycin and 2
mmol/l L-glutamine at 37°C in 5% CO2. The medium in the
culture dish was replaced with the same volume of fresh culture
medium after 48 h, then replaced every 3–5 days when the adherent
cells reached 70–80% confluence. Cell collection was completed with
0.25% trypsin/ethylenediaminetetraacetic acid (EDTA; Solarbio Inc,
Beijing, China) treatment and subcultured using a 25-cm2
culture dish.
Labeling and tracing of rat BMSCs
The BMSCs (third passage) were collected using 0.25%
EDTA and cultured with DMEM medium containing 10% FBS (cell density
5×103/cm2). After 24 h,
5-ethynyl-2′-deoxyuridine (EdU; Cell-Light™ EdU Apollo™ DNA in
vivo Kit, Bo Rui Inc., Guangzhou, China) was added to the
medium at a concentration of 10 μM. After 72 h, the cells were
washed twice with phosphate-buffered saline (PBS). Approximately
2×107 EdU-labeled BMSCs were subsequently utilized for
injection. After transplantation, the tracing of the EdU-labeled
BMSCs in the liver tissues was carried out using immunofluorescence
staining according to the manufacturer’s instructions. The liver
tissues were fixed with methanol, dewaxed and then incubated in
0.5% Triton® X-100 in PBS at room temperature. The
tissues were then incubated with an Apollo reaction cocktail for 30
min at room temperature without light, counterstained with Hoechst
33324 reaction cocktail for 30 min at room temperature without
light, and imaged under a fluorescence microscope (OlympusBX5l;
Olumpus, Tokyo, Japan), as previously described (23).
General experimental protocols
A total of 80 SD rats with ALF were randomly divided
into 5 groups (n=16 in each group) and injected via the hepatic
artery (group 1), the portal vein (group 2), the vena caudalis
(group 3) and by intraperitoneal injection (group 4). Group 5, in
which the rats received the same volume of isotonic saline but no
BMSCs via the vena caudalis, served as the controls. At 24 h after
the administration of D-gal/LPS, the 0.8 ml EdU-labeled BMSC
suspensions (passages 3 to 6, 1.4×107/kg) were injected
through the different routes within 15 min. The procedure was
performed under general anesthesia. There were 5, 5 and 6 animals
per group sacrifice on days 1, 3 and 7 post-implantation,
respectively.
Flow cytometry
The phenotypic profile of the BMSCs was evaluated by
flow cytometric analysis (fluorescence-activated cell sorting, Epic
XL, Software Expo 32; Beckman Coulter, Fullerton, CA, USA), using
CD29, CD90, CD45 and CD11b/c antibodies (BioLegend, San Diego, CA,
USA), coupled to either phycoerythrin or fluorescein
isothiocyanate.
Alanine aminotransferase (ALT) and
aspartate aminotransferase (AST) levels
Blood samples were obtained from each rat in the 5
groups on days 1, 3 and 7 post-transplantion. The samples were
immediately centrifuged at 2,000 × g for 6 min before serum was
collected. The ALT and AST levels were measured using a serum
multiple automatic biochemical analyzer (HITACHI-7150;
Olympus).
Histological examination
Specimens from the rat livers in all groups were
fixed in 4% formaldehyde, embedded with paraffin, sectioned and
stained with hematoxylin and eosin (H&E). Pathological findings
were assessed according to the Scheuer score by one of the authors
blinded to the group allocations.
Immunohistochemistry for proliferating
cell nuclear antigen (PCNA) and cysteine-containing
aspartate-specific protease (caspase)-3
Regeneration and apoptotic hepatocytes were
identified by immunohistochemistry. According to the manufacturer’s
instructions, immunohistochemical staining was performed to
evaluate PCNA [fluorescein isothiocyanate-labeled monoclonal mouse
clone PC10; LifeSpan BioSciences (LSBio), Seattle, WA, USA] and
caspase-3 (fluorescein isothiocyanate-labeled monoclonal rabbit
clone CPP32-Ab-4, Thermo Fisher Scientific, Waltham, MA, USA).
Positive cells were counted in 10 random visual fields at ×200
magnification for each section, and the number was expressed as the
integrated optical density (IOD) value. The sections were examined
microscopically for specific staining, and photographs were
acquired using a digital image-capture system (Olympus CX40;
Olympus, Tokyo, Japan).
Enzyme-linked immunosorbent assay
Blood was collected from the rats in the 5 different
groups at 1, 3 and 7 days post-transplantation. Serum samples were
assayed for stromal cell-derived factor 1 (SDF-1) production with
an SDF-1 enzyme-linked immunosorbent assay (ELISA) quantification
kit (GBD, Santiago, CA, USA) according to the manufacturer’s
recommendations.
Quantitative reverse
transcription-polymerase chain reaction (RT-qPCR)
Total RNA was extracted from the liver tissue (50
mg) using TRIzol reagent (Invitrogen, Carlsbad, CA, USA). RNA (5
μg) was reverse-transcribed using the AMV First Strand cDNA
Synthesis Kit (Invitrogen) following the manufacturer’s
instructions, yielding the complementary DNA (cDNA) template. The
cDNA was then amplified by PCR using the primer sequences
(ShengGong, Shanghai, China) shown in Table I. After PCR, 10 μl of the reaction
mixture were subjected to electrophoresis on a 1% agarose gel. The
size of the PCR fragments was estimated using a 100-base-pair
ladder. The quantitative PCR amplification and data analysis were
performed using fluorescence quantitative PCR (StepOnePlus; Applied
Biosystems, Foster City, CA, USA). Primer sequences are listed in
Table I.
 | Table IGene primers used for detection. |
Table I
Gene primers used for detection.
| Gene | Sense | Antisense |
|---|
| β-actin |
ACGTTGACATCCGTAAAGACC |
GCCACCAATCCACACAGAGT |
| SDF1 |
CATCAGTGACGGTAAGCCAG |
CACAGTTTGGAGTGTTGAGGAT |
| HGF |
ATGACATCACTCCCGAGAACTT |
GAGAGCAGTAACCAACTCGGAT |
Statistical analysis
Data are presented as the means ± standard deviation
(SD). Differences in parameters were analyzed using a one-way
analysis of variance (ANOVA). All analyses were performed using
SPSS version 17.0 statistical software (SPSS Inc, Chicago, IL,
USA). Values of P<0.05 were considered to indicate statistically
significant differences.
Results
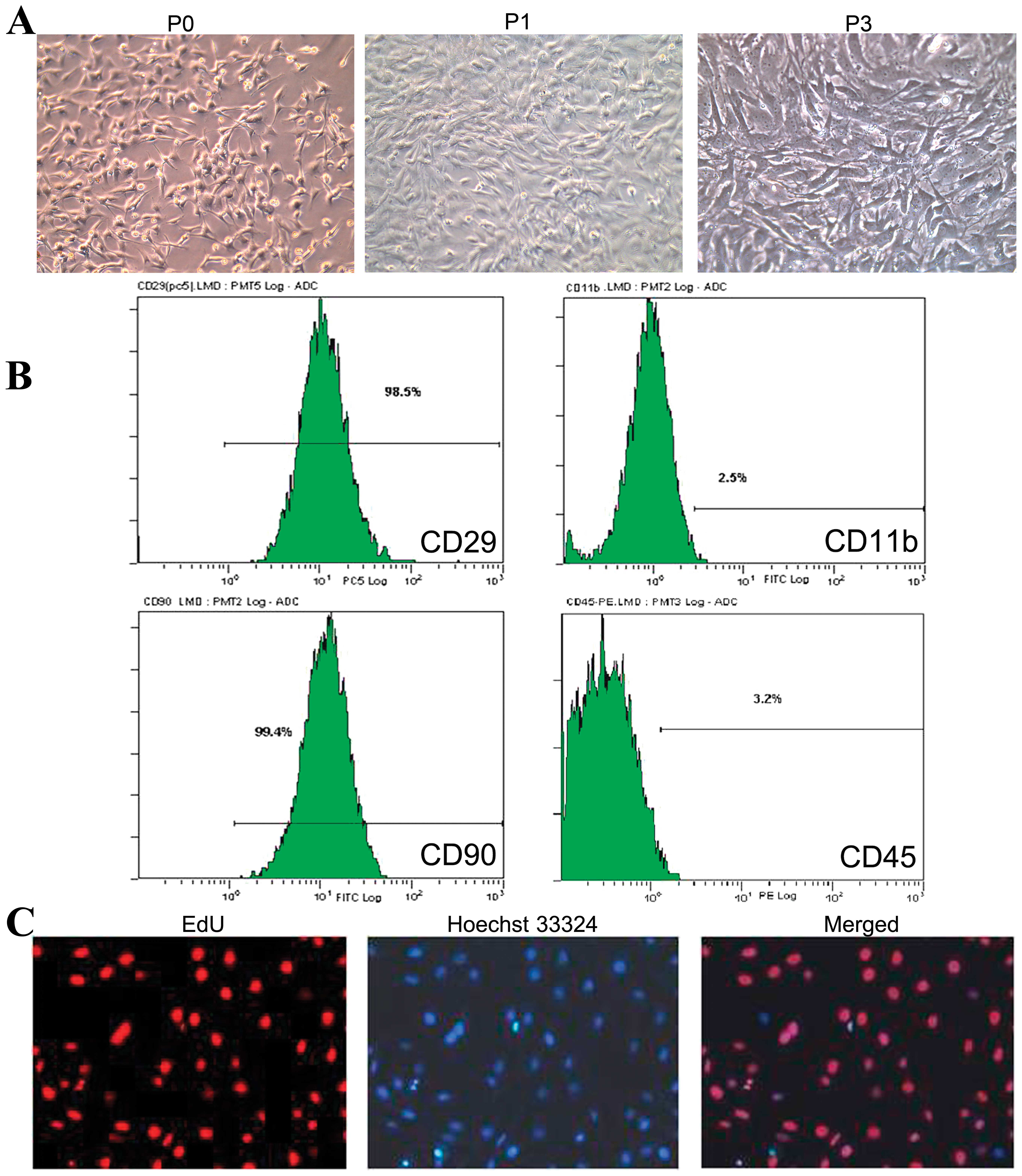
Morphology of cultured rat BMSCs
The adherent cells adopted a colony-like
distribution within 3 days after inoculation into the flask, as
shown under a phase-contrast microscope. Typically, approximately
70–90% confluence was reached by days 7–9. Cells of the third
passage had a typical spindle-shaped, fibroblastic morphology and
good refractivity. The profile of the cells could clearly be seen,
but the nuclei were not distinctly visible (Fig. 1A).
Surface markers of isolated rat BMSCs and
EdU-labeling efficiency
The immunophenotype of the culture-expanded cells
(passages 3 to 6) was analyzed by flow cytometry. The BMSCs
isolated from rat bone marrow were positive for CD29 (98.5%) and
CD90 (99.4%) and negative for CD11b (2.5%) and CD45 (3.2%)
(Fig. 1B). When the concentration
of EdU was 10 μmol/l, the labeling efficiency of the rat BMSCs was
93%. A fluorescence microscope revealed that the nucleus of the
EdU-positive cells was intensely red, with Hoechst 33324 staining
observed in the nucleus (blue fluorescence). EdU is a
nucleus-specific tag, located in the nucleus together with Hoechst
33324 (Fig. 1C).
Effect of BMSC transplantation on liver
function in rats with ALF
The levels of ALT and AST gradually decreased after
transplantation in all the groups. On day 7 post-implantation, the
levels of ALT and AST in the hepatic artery injection group, portal
vein injection group and vena caudalis injection group were lower
than those in the control group (P<0.05). Compared with the
control group, there was no statistically significant difference in
ALT and AST levels in the intraperitoneal injection group on day 7
post-operation (P>0.05) (Table
II).
 | Table IIComparison of liver function
post-transplantation (IU/l). |
Table II
Comparison of liver function
post-transplantation (IU/l).
| Day 1 | Day 3 | Day 7 |
|---|
|
|
|
|
|---|
| Injection
group | ALT | AST | ALT | AST | ALT | AST |
|---|
| Control group | 55.4±9.9 | 126.4±20.2 | 45.9±10.4 | 128.8±18.0 | 57.0±13.4 | 137.3±36.9 |
|
Intraperitoneal | 35.7±0.9a | 109.7±7.9a | 42.0±10.3a | 97.0±25.1a | 44.3±7.3a | 96.4±24.9a |
| Vena caudalis | 52.0±10.7a | 135.6±16.0a | 46.1±8.4a | 97.3±22.5a | 31.8±4.1b | 72.0±6.4b |
| Portal vein | 60.0±15.6a | 277.0±108.9a | 31.8±25.8a | 118.5±97.3a | 30.0±6.8b | 74.3±7.7b |
| Hepatic artery | 94.5±61.5a | 231.0±17.0a | 19.3±1.3a | 54.3±6.0a | 21.5±2.4b | 63.3±6.1b |
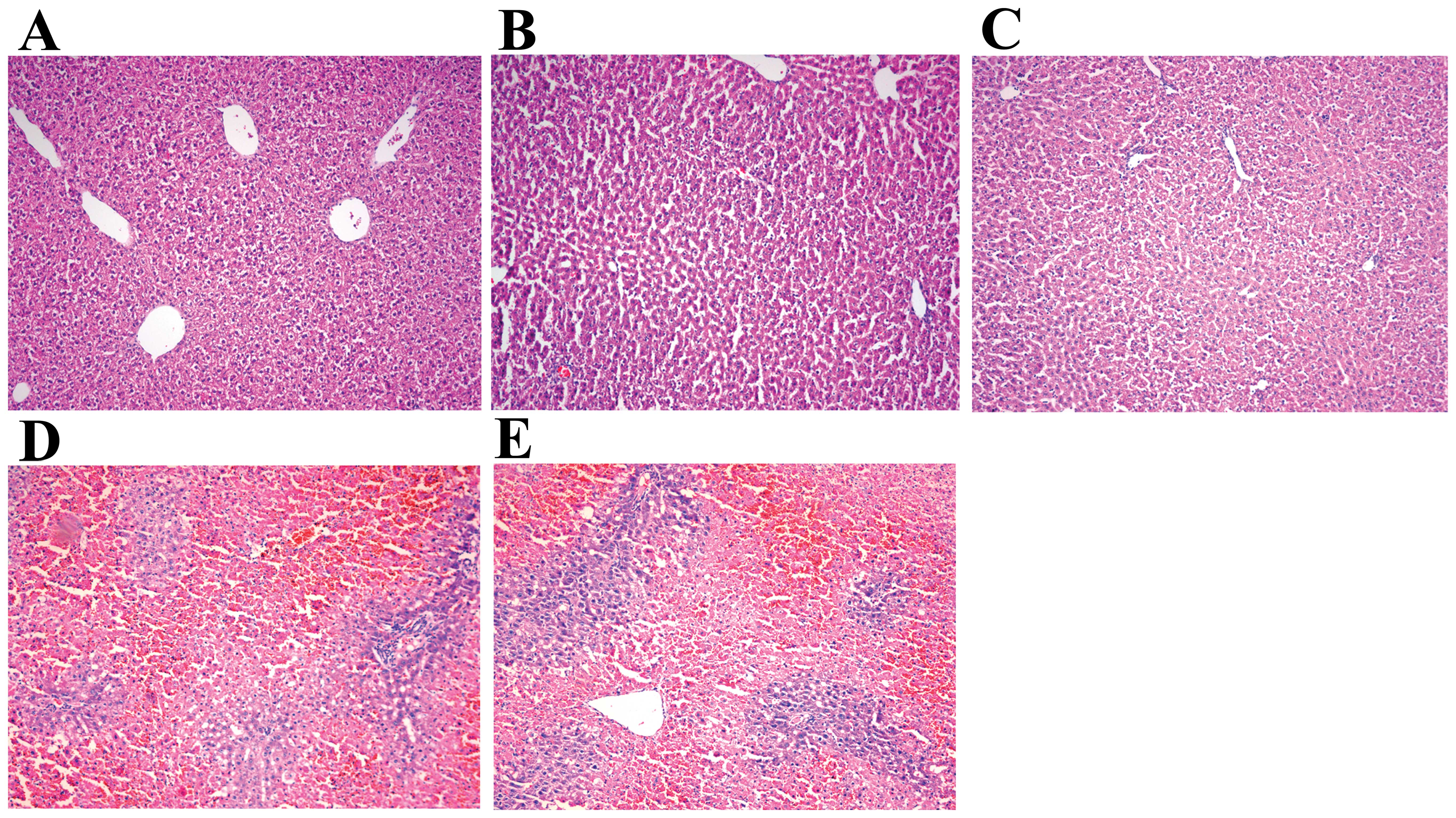
Three days after transplantation, histological
staining indicated that the sham (isotonic saline)-injected rats
with D-gal/LPS-induced ALF suffered serious inflammation.
Non-normal liver lobules had dispersed throughout the liver sinus,
hepatic sinusoid had dissociated, hepatocytes had diffuse necrosis,
and a large number of inflammatory cells had infiltrated into the
necrotic areas. In the hepatic artery, portal vein and vena
caudalis injection groups, histological staining indicated that
hepatocyte edema, degeneration and necrosis were improved, while
inflammatory cell infiltration was significantly reduced. The
intraperitoneal transplantation group displayed schistic necrosis,
eosinophilic changes and infiltration of inflammatory cells
(Fig. 2).
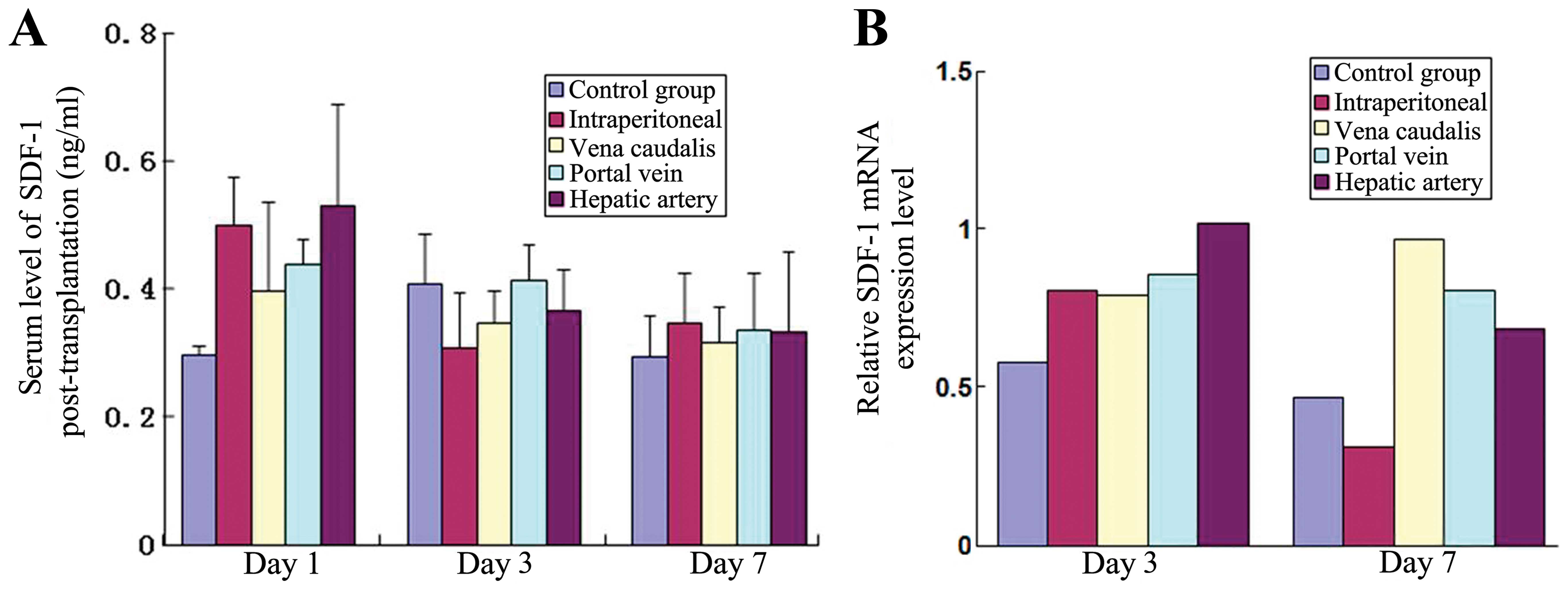
SDF-1 levels in serum and liver
tissue
The levels of SDF-1 in serum as assessed by ELISA
and the expression of SDF-1 mRNA in the liver tissue as measured by
RT-qPCR revealed no significant differences between the 5 groups
(P>0.05) (Fig. 3).
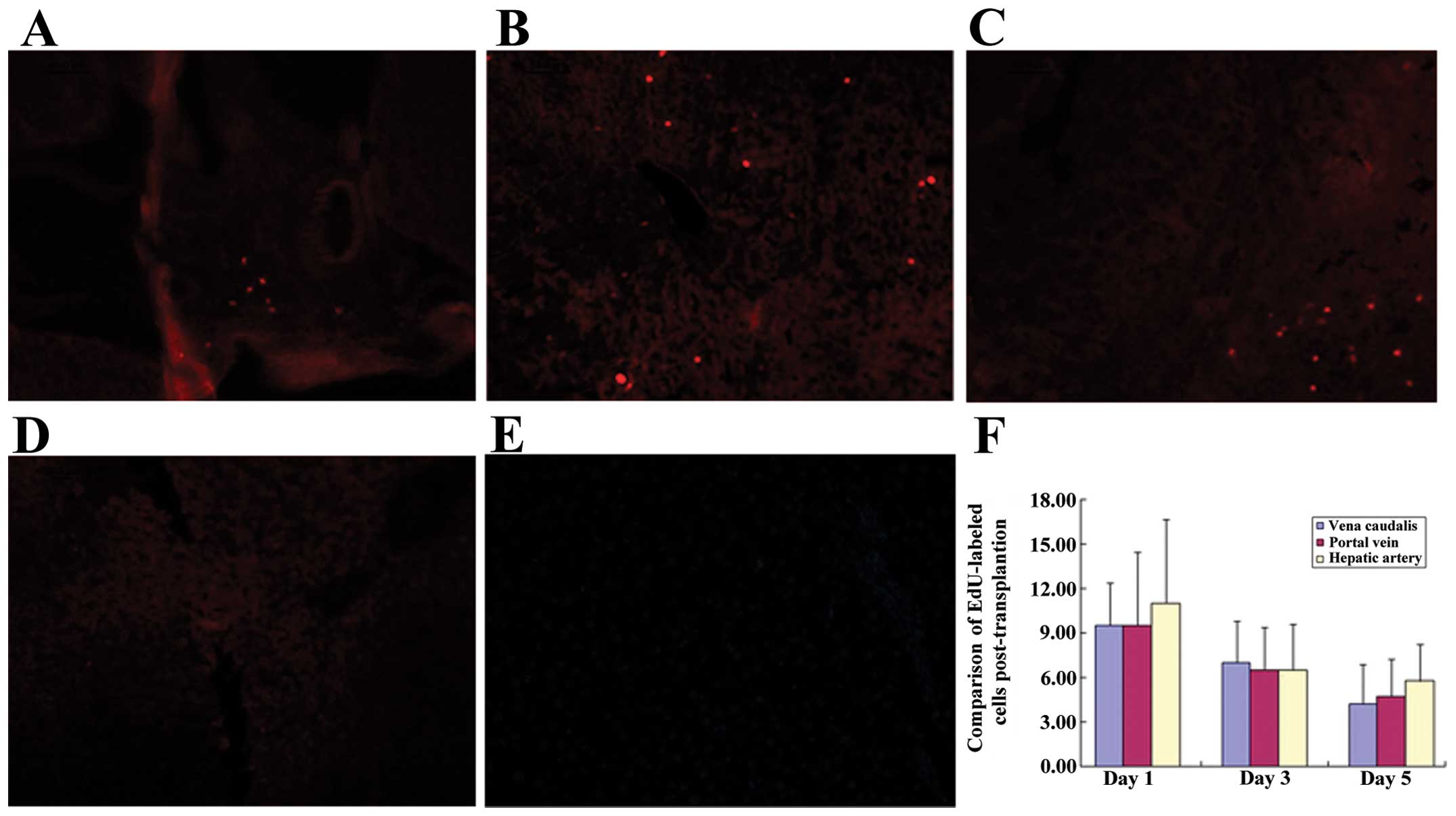
Homing of BMSCs post-implantation
The homing of BMSCs in the liver tissues was
examined using immunofluorescence on days 1, 3 and 7 following BMSC
transplantation. Transplanted BMSCs were not observed in the
intraperitoneal injection group or the control group. Labeled
transplanted cells were observed in the hepatic artery, the portal
vein and the vena caudalis injection groups on day 1. Labeled
transplanted cells were predominantly distributed in the hepatic
sinusoid. The numbers of EdU-labeled cells were 4.25±2.63/high
power lens (HP), 7.00±2.83/HP and 9.5±2.89/HP in the hepatic
artery, the portal vein and the vena caudalis injection groups,
respectively. On day 3 post-transplantation, the numbers of
positive cells in the hepatic artery, the portal vein and the vena
caudalis injection groups were 4.75±2.5/HP, 6.5±2.89/HP and
9.50±4.95/HP, respectively. The positive cells were predominantly
distributed around the damaged live tissue. On day 7, signs of the
transplanted cells were still present in the hepatic artery, portal
vein and vena caudalis injection groups (5.75±2.50/HP, 6.5±3.11/HP,
11.00±5.66/HP, respectively). There were no statistically
significant differences in the number of homing transplanted cells
between these 3 groups (P>0.05) (Fig. 4).
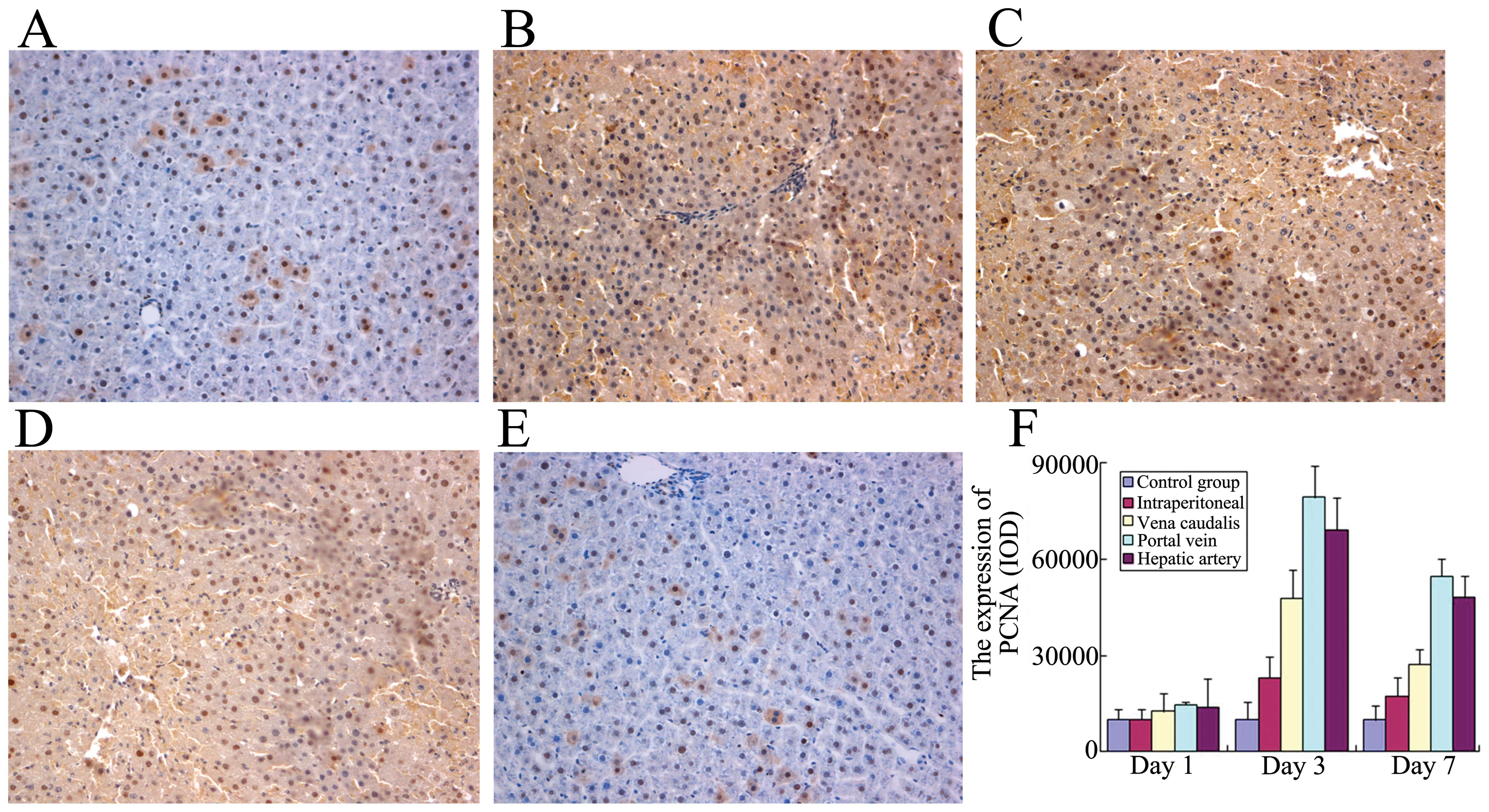
Expression of PCNA in liver tissue
The expression of PCNA in the liver tissue was
detected on days 1, 3 and 7 by immunohistochemical staining with a
monoclonal antibody to PCNA. PCNA-positive cell staining in the
nucleus was a brown-yellow color and had a fine granular
appearance. On day 3 after transplantation, there was a strong
expression of PCNA in the treatment groups. On day 7, PCNA staining
levels were weaker than the levels on day 3. At days 3 and 7 after
transplantation, PCNA was predominantly expressed in the
hepatocytes and bile duct cells. The PCNA staining levels in the
hepatic artery, the portal vein and the vena caudalis injection
groups were higher than the levels in the intraperitoneal injection
group and the control group (P<0.05). There were no significant
differences in PCNA staining levels between the intraperitoneal
injection group and the control group (P>0.05), or between the
hepatic artery, the portal vein and the vena caudalis injection
groups (Fig. 5).
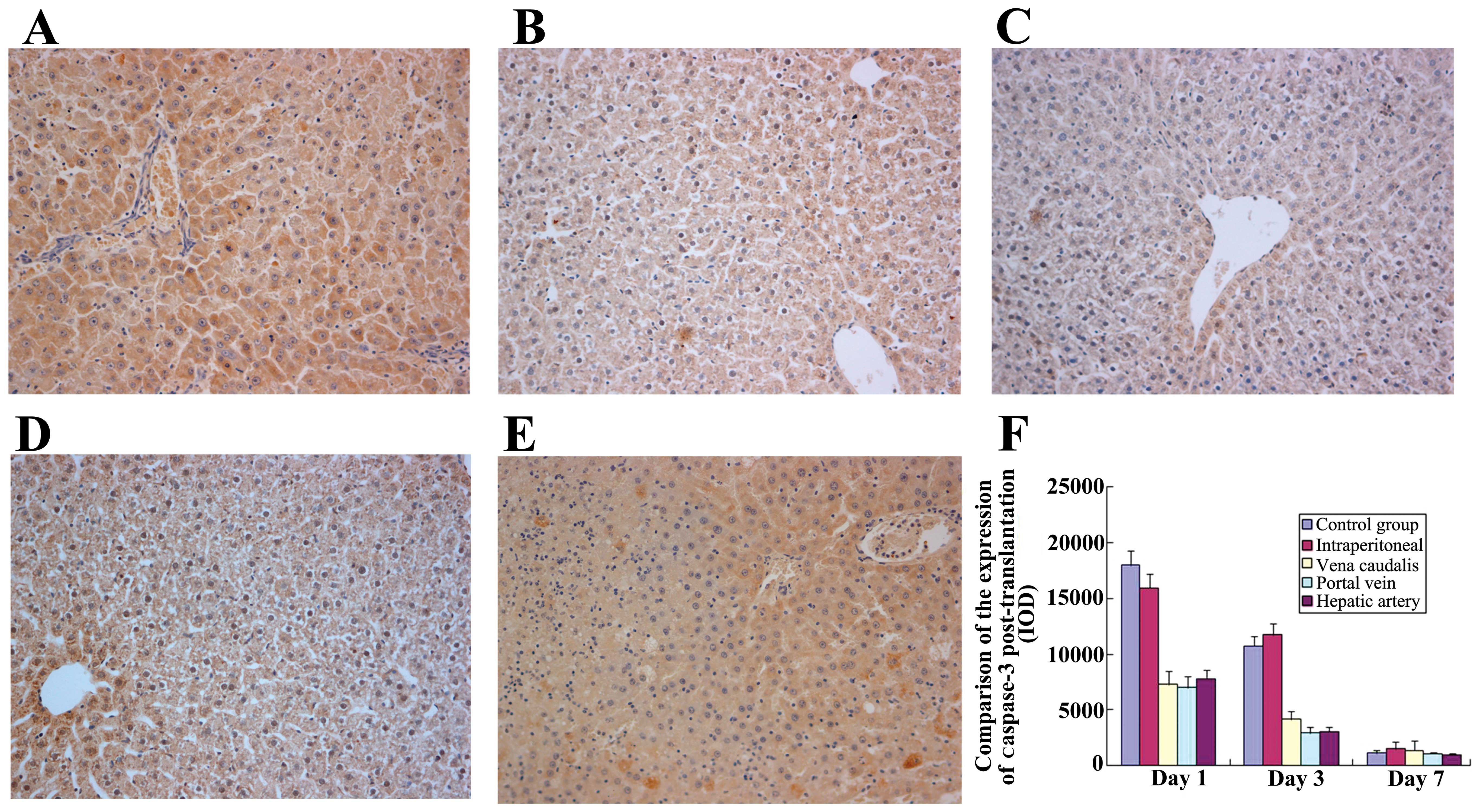
Expression of caspase-3 in liver
tissue
Caspase-3-positive cells were visible as brown
granules, predominantly expressed in the portal area around the
cytoplasm of the hepatocytes, with some expression in the nucleus.
In each group, caspase-3 expression was strong on day 1
post-transplantation, weaker on day 3, and almost entirely absent
on day 7. On days 1 and 3, caspase-3 expression in the hepatic
artery, the portal vein, and the vena caudalis injection groups was
lower than that in the intraperitoneal injection group and the
control group (P<0.05). Caspase-3 expression showed no
statistically significant differences between the intraperitoneal
injection group and the control group (P>0.05), or between the
hepatic artery, portal vein and vena caudalis injection groups
(P>0.05) (Fig. 6).
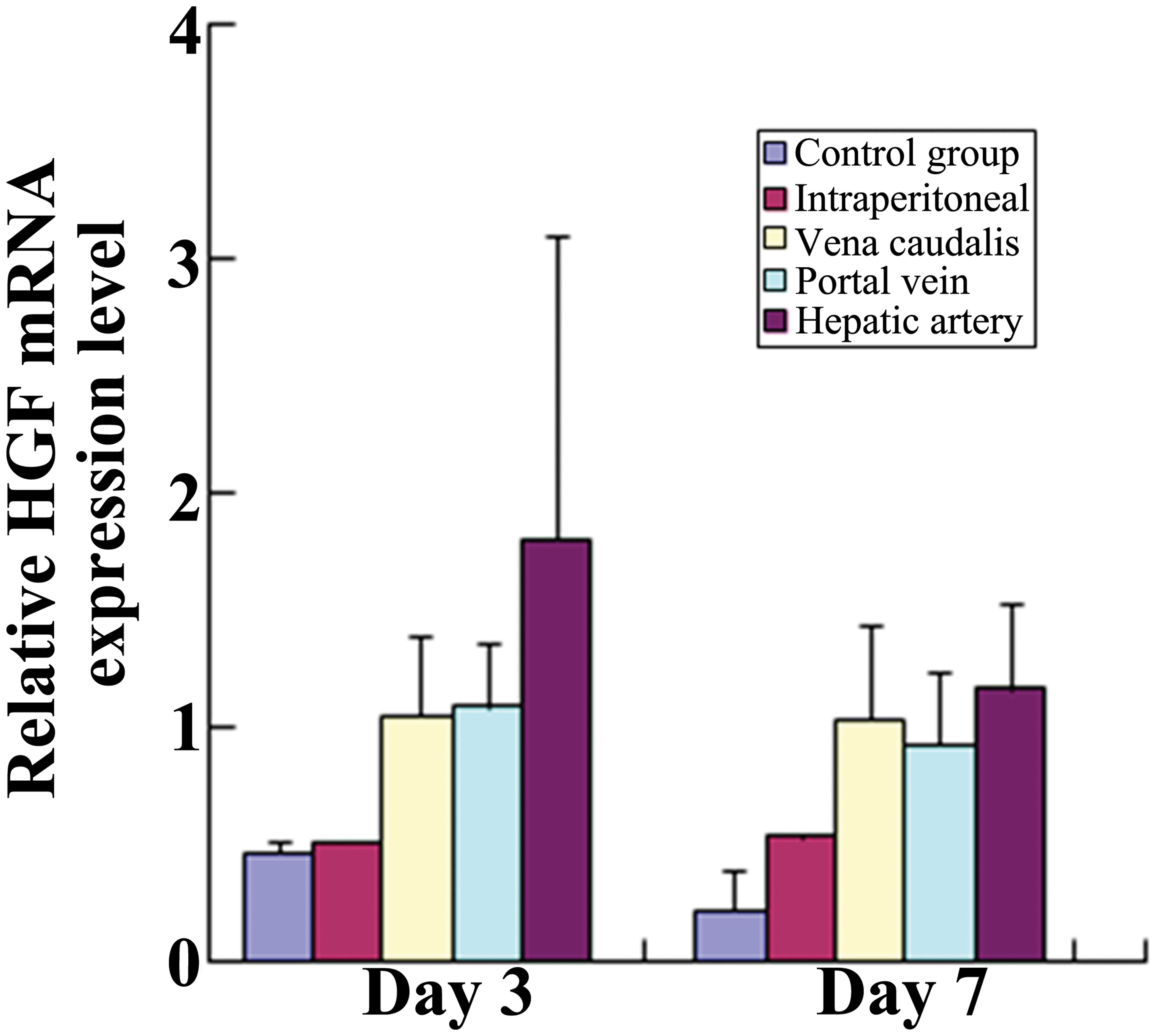
Hepatocyte growth factor (HGF) mRNA level
in liver tissue
On day 3 post-transplantation, the expression of HGF
in the 4 treatment groups was significantly higher than that in the
control group (P<0.05). However, the expression of HGF in the
intraperitoneal injection group was lower than that in the vena
caudalis injection group, the portal vein injection group, and the
hepatic artery injection group (P<0.05). There were no
statistically significant differences between the vena caudalis
injection group, the hepatic artery group, and the portal vein
groups (P>0.05). On day 7 post-transplantation, the expression
of HGF in the vena caudalis injection group, the portal vein group
and the hepatic artery group was higher than that in the
intraperitoneal injection group and the control group. The
difference between the intraperitoneal injection group and the
control group was not statistically significant (P>0.05). There
were no significant differences between the vena caudalis, the
hepatic artery and the portal vein injection groups (P>0.05)
(Fig. 7).
Discussion
ALF is the clinical manifestation of sudden and
severe hepatic injury and arises from many causes, such as viruses,
drugs and poisons. Due to the abrupt loss of hepatic metabolic and
immunological function, the condition leads to hepatic
encephalopathy, coagulopathy and in many cases, progressive
multi-organ failure (24).
Although uncommon, this critical illness occurs mostly in young
adults and is associated with high mortality and resource costs. In
many countries it is the most frequent indication for emergency
liver transplantation (25). The
current clinical treatment for liver failure includes medical
drugs, artificial liver support treatment, liver transplantation
and stem cell transplantation (5,26–28). Among these methods, OLT represents
the most suitable therapeutic option for patients with hepatic
failure; however, the speed of disease progression, as well as the
variable course of ALF and organ shortages limits its use (29). Cell-based therapy has been
proposed as a potential alternative to OLT. Allogeneic hepatocyte
transplantation has been reported for the treatment of ALF
(30,31). However, immune rejection and
hepatocyte disorder in in vitro cultures have provided
obstacles to the widespread use of this type of therapy (32,33).
Given this background, a growing enthusiasm has
greeted the development of stem-cell-based therapies for liver
diseases. The application of bone marrow MSC transplantation for
ALF has been a research hotspot over recent years (19).
MSCs are adherent, fibroblast-like, pluripotent and
non-hematopoietic progenitor cells. Numerous studies have
demonstrated that MSCs have a high degree of plasticity, as they
differentiate into cells of the mesenchymal lineage, but they can
also differentiate into neurons, splenocytes and various epithelial
cells, including liver, lung, intestinal and kidney cells (34,35). Recent experimental studies have
shown the successful application of MSC transplantation in the
treatment of fulminant hepatic failure (FHF), end-stage liver
disease (ESLD) and inherited metabolic disorders (IMDs) (36–38). According to the International
Society for Cellular Therapy (ISCT), MSCs are defined by their
expression of CD105, CD73 and CD90 and the lack of expression of
CD45, CD34, CD14 or CD11b, CD79a or CD19 and human leukocyte
antigen (HLA)-DR (39). In this
study, BMSCs were isolated and cultured from SD rats. The
immunophenotype of the BMSCs was evaluated by
fluorescence-activated cell sorting. More than 98% of the cells
stained positive for CD29 and CD90, which is in accordance with the
diagnostic characteristics of MSCs. The cells stained negative for
CD11b and CD45, which are indicative of neutrophilic granulocyte
and hematopoietic cell lines. These results demonstrate that the
cultured cells derived from the rat bone marrow consisted of more
than 98% MSCs, which is consistent with the results from previous
studies (40–42).
Selecting an appropriate MSC transplantation route
is vital for cell survival, the induction of cell differentiation
and the restoration of liver function. In this study, we injected
BMSCs via 4 different routes. Liver function was elevated in the
hepatic artery group, the portal vein group and the caudal vein
group compared with the control group 7 days post-implantation.
There was no significant difference between the intraperitoneal
injection group and the control group. Same changes were observed
in histological staining. This indicates that hepatocyte edema,
degeneration and necrosis were improved, while inflammatory cell
infiltration was significantly reduced in the hepatic artery group,
the portal vein group and the caudal vein group. Furthermore, these
differences had occurred by 3 days post-implantation. These results
confirm that BMSCs have a therapeutic effect in the treatment of
liver failure.
To further compare the functional restoration of
MSCs following hepatic artery, portal vein and caudal vein
injection, the levels of ALT and AST were measured, and revealed no
differences between these groups. Furthermore, no differences were
observed in the extent of histological improvement between these
groups. These results indicate that the implantation route may
impact on the curative effect of implantation; the endovascular
injection of BMSCs provides better treatment than extravascular
injection modalities.
SDF-1 is a micro-molecular protein, exhibiting a
variety of biologic activities. It has been shown that SDF-1 can
promote BMSC homing to the injured livers of mice (43). SDF-1 can also act as a
chemoattractant to promote the migration of stem cells (44) and to strengthen their locomotory
capacity (45). When stem cells
migrate to the target tissue, SDF-1 facilitates their adhesion to
fibrinogen, fibronectin, interstitium and endotheliocytes. In this
study, the level of SDF-1 in serum and the expression of SDF-1 mRNA
in the liver tissue were similar, indicating that the extent of
chemotaxis was the same in all the rats with ALF. However, labeled
transplanted cells were only observed in the hepatic artery
injection group, the portal vein injection group and the vena
caudalis injection group, and not in the intraperitoneal injection
group or the control group. These results confirm the effect of an
endovascular injection of BMSCs in promoting BMSC homing to the
injured livers. However, our study did not show superiority among
the hepatic artery injection group, the portal vein injection
group, or the vena caudalis injection group. In addition,
immunohistochemistry of the liver sections for PCNA expression
revealed that the PCNA staining levels in the hepatic artery, the
portal vein and the vena caudalis injection group were higher than
the levels in the intraperitoneal injection group or the control
group. The level of HGF mRNA in the liver, according to RT-qPCR,
also showed the same pattern (46). These results indicate that the
endovascular injection of BMSCs may promote hepatocyte
regeneration, as also previously demonstrated (47).
In the early stages of post-implantation, caspase-3
expression in the hepatic artery, the portal vein and the vena
caudalis injection group was lower than that in the intraperitoneal
injection group and the control group. However,
intraperitoneally-injected BMSCs were not a sufficiently effective
treatment when compared with the BMSCs in the endovascular
injection groups. These results indicate that an endovascular
injection of BMSCs has profound inhibitory effects on
hepatocellular death, and leads to reduced hepatocyte apoptosis,
enhanced liver regeneration and an increased number of
proliferating hepatocytes. However, this study did not show
superiority among the hepatic artery injection group, the portal
vein injection group, or the vena caudalis injection group.
Three factors affected the homing of stem cells in
the liver: i) the type and severity of liver damage; ii) the
expression of chemokines prompting the homing of stem cells to the
damaged liver; and iii) the number of bone marrow stem cells in the
circulation. It is well known that chemokines are released after
tissue damage and that the migratory direction of stem cells
follows the chemokine concentration gradient. The increase in the
inflammatory chemokine concentration at the site of inflammation is
a key mediator of MSC trafficking to the site of injury (46,48,49). MSCs have an inherent chemotaxis
ability to home in to sites of inflammation (50). MSCs express the SDF-1 chemokine
receptor [chemokine (C-X-C motif) receptor 4, CXCR4], while the
SDF-1/CXCR4 biological axis stimulates the recruitment of
progenitor cells to the site of tissue injury (51–54). BMSCs can migrate across
endothelial cell layers, attracted to injury tissue and be retained
in the ischemic tissue, but not in the remote or intact tissue.
Transplantation via an endovascular approach can ensure that stem
cells in the blood respond to the concentration gradient of
chemotaxis and migrate to the damaged liver tissue. Although the
hepatic artery, portal vein and caudal vein have different degrees
of influence on liver hemodynamics, and while each involve
different homing distances, the different endovascular approaches
did not affect the chemotaxis or the homing of stem cells in our
study. Due to a deficiency in stem cell homing, the BMSC
transplantation via intraperitoneal injection had no therapeutic
effect on ALF in rats.
In conlusion, following BMSC transplantation, liver
function in the rats with ALF was improved by hepatic artery
injection, portal vein injection and vena caudalis injection. The
extent of damage in the liver pathology was also reduced. At the
same level of the chemotactic factor, SDF-1, the 3 endovascular
graft methods (hepatic artery, portal vein and vena caudalis)
showed a benefit in terms of the BMSCs homing to the damaged liver
tissue, enhancing hepatocyte proliferation and inhibiting liver
cell apoptosis; all 3 methods were an effective route for the
transplantation of BMSCs for the treatment of ALF. However, the
selection of blood vessel as a migration path does not affect the
transplantation result. The intraperitoneal injection as a
transplantation route showed no therapeutic effect in our animal
experiments.
Acknowledgements
We would like to thank the staff of the Scientific
Research Center of The First Affiliated Hospital of Xinjiang
Medical University. We are grateful to Dr Mei Ma and Dr WenJun Chen
for the performance of the cell transplantation and biopsy
procedures.
References
|
1
|
Bernal W, Auzinger G, Dhawan A and Wendon
J: Acute liver failure. Lancet. 376:190–201. 2010. View Article : Google Scholar
|
|
2
|
Fiegel HC, Lange C, Kneser U, et al: Fetal
and adult liver stem cells for liver regeneration and tissue
engineering. J Cell Mol Med. 10:577–587. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wigg AJ, Gunson BK and Mutimer DJ:
Outcomes following liver transplantation for seronegative acute
liver failure: experience during a 12-year period with more than
100 patients. Liver Transpl. 11:27–34. 2005.PubMed/NCBI
|
|
4
|
Le Blanc K and Pittenger M: Mesenchymal
stem cells: progress toward promise. Cytotherapy. 7:36–45.
2005.PubMed/NCBI
|
|
5
|
Cantz T, Manns MP and Ott M: Stem cells in
liver regeneration and therapy. Cell Tissue Res. 331:271–282. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stutchfield BM, Forbes SJ and Wigmore SJ:
Prospects for stem cell transplantation in the treatment of hepatic
disease. Liver Transpl. 16:827–836. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Aurich I, Mueller LP, Aurich H, et al:
Functional integration of hepatocytes derived from human
mesenchymal stem cells into mouse livers. Gut. 56:405–415. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aurich H, Sgodda M, Kaltwasser P, et al:
Hepatocyte differentiation of mesenchymal stem cells from human
adipose tissue in vitro promotes hepatic integration in vivo. Gut.
58:570–581. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Banas A, Teratani T, Yamamoto Y, et al:
Adipose tissue-derived mesenchymal stem cells as a source of human
hepatocytes. Hepatology. 46:219–228. 2007.PubMed/NCBI
|
|
10
|
Beaudry P, Hida Y, Udagawa T, et al:
Endothelial progenitor cells contribute to accelerated liver
regeneration. J Pediatr Surg. 42:1190–1198. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kuo TK, Hung SP, Chuang CH, et al: Stem
cell therapy for liver disease: parameters governing the success of
using bone marrow mesenchymal stem cells. Gastroenterology.
134:2111–2121. 2121.e1–3. 2008.PubMed/NCBI
|
|
12
|
Bajek A, Olkowska J and Drewa T:
Mesenchymal stem cells as a therapeutic tool in tissue and organ
regeneration. Postepy Hig Med Dosw (Online). 65:124–132. 2011.(In
Polish).
|
|
13
|
Zhou P, Hohm S, Olusanya Y, Hess DA and
Nolta J: Human progenitor cells with high aldehyde dehydrogenase
activity efficiently engraft into damaged liver in a novel model.
Hepatology. 49:1992–2000. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cho KA, Ju SY, Cho SJ, et al: Mesenchymal
stem cells showed the highest potential for the regeneration of
injured liver tissue compared with other subpopulations of the bone
marrow. Cell Biol Int. 33:772–777. 2009. View Article : Google Scholar
|
|
15
|
Wang M, Shang Z, Zhang X and Jia C:
Therapeutic effect of different channels of BMSCs transplantation
on liver cirrhosis in rat. China Modern Doctor. 48:7–9. 2010.(In
Chinese).
|
|
16
|
Xiong Q, Feng J, Wang J, et al: Comparison
among curative effects of three different transplantation
approaches of mesenchymal stem cells on rat model of cirrhosis. J
Third Mil Med Univ. 33:804–808. 2011.(In Chinese).
|
|
17
|
Zhao W, Li JJ, Cao DY, et al: Intravenous
injection of mesenchymal stem cells is effective in treating liver
fibrosis. World J Gastroenterol. 18:1048–1058. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cao H, Yang J, Yu J, et al: Therapeutic
potential of transplanted placental mesenchymal stem cells in
treating Chinese miniature pigs with acute liver failure. BMC Med.
10:562012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim SJ, Park KC, Lee JU, Kim KJ and Kim
DG: Therapeutic potential of adipose tissue-derived stem cells for
liver failure according to the transplantation routes. J Korean
Surg Soc. 81:176–186. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li F, Hu X, Zhao HM, et al: Influence of
different infusion methods of human umbilical cord mesenchymal stem
cells on acute tubular necrosis. Zhongguo Zuzhi Gongcheng Yanjiu yu
Linchuang Kangfu. 14:7470–7473. 2010.(In Chinese).
|
|
21
|
Zonta S, De Martino M, Bedino G, et al:
Which is the most suitable and effective route of administration
for mesenchymal stem cell-based immunomodulation therapy in
experimental kidney transplantation: endovenous or arterial?
Transplant Proc. 42:1336–1340. 2010. View Article : Google Scholar
|
|
22
|
Zhang GQ, Fang CH and Chi DZ: Hepatocyte
growth factor induces differentiation of adult rat mesenchymal stem
cells into a hepatocyte lineage in vitro. Zhonghua Wai Ke Za Zhi.
43:716–720. 2005.(In Chinese).
|
|
23
|
Lin G, Huang YC, Shindel AW, et al:
Labeling and tracking of mesenchymal stromal cells with EdU.
Cytotherapy. 11:864–873. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ichai P and Samuel D: Etiology and
prognosis of fulminant hepatitis in adults. Liver Transpl. 14(Suppl
2): S67–S79. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pathikonda M and Munoz SJ: Acute liver
failure. Ann Hepatol. 9:7–14. 2010.
|
|
26
|
Podoll AS, DeGolovine A and Finkel KW:
Liver support systems - a review. ASAIO J. 58:443–449. 2012.
View Article : Google Scholar
|
|
27
|
Ostapowicz G, Fontana RJ, Schiodt FV, et
al: Results of a prospective study of acute liver failure at 17
tertiary care centers in the United States. Ann Intern Med.
137:947–954. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lysy PA, Campard D, Smets F, Najimi M and
Sokal EM: Stem cells for liver tissue repair: current knowledge and
perspectives. World J Gastroenterol. 14:864–875. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Campsen J, Blei AT, Emond JC, et al:
Outcomes of living donor liver transplantation for acute liver
failure: the adult-to-adult living donor liver transplantation
cohort study. Liver Transpl. 14:1273–1280. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fisher RA and Strom SC: Human hepatocyte
transplantation: worldwide results. Transplantation. 82:441–449.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bruzzone P and Strom SC: Historical
aspects of hepatocyte transplantation. Transplant Proc.
38:1179–1180. 2006. View Article : Google Scholar
|
|
32
|
Wu YM, Joseph B, Berishvili E, Kumaran V
and Gupta S: Hepatocyte transplantation and drug-induced
perturbations in liver cell compartments. Hepatology. 47:279–287.
2008.PubMed/NCBI
|
|
33
|
Kisseleva T, Gigante E and Brenner DA:
Recent advances in liver stem cell therapy. Curr Opin
Gastroenterol. 26:395–402. 2010. View Article : Google Scholar
|
|
34
|
Baksh D, Song L and Tuan RS: Adult
mesenchymal stem cells: characterization, differentiation, and
application in cell and gene therapy. J Cell Mol Med. 8:301–316.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Jiang Y, Jahagirdar BN, Reinhardt RL, et
al: Pluripotency of mesenchymal stem cells derived from adult
marrow. Nature. 418:41–49. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Flohr TR, Bonatti H Jr, Brayman KL and
Pruett TL: The use of stem cells in liver disease. Curr Opin Organ
Transplant. 14:64–71. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Mohamadnejad M, Alimoghaddam K,
Mohyeddin-Bonab M, et al: Phase I trial of autologous bone marrow
mesenchymal stem cell transplantation in patients with
decompensated liver cirrhosis. Arch Iran Med. 10:459–466.
2007.PubMed/NCBI
|
|
38
|
Banas A, Teratani T, Yamamoto Y, et al:
Rapid hepatic fate specification of adipose-derived stem cells and
their therapeutic potential for liver failure. J Gastroenterol
Hepatol. 24:70–77. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Dominici M, Le Blanc K, Mueller I, et al:
Minimal criteria for defining multipotent mesenchymal stromal
cells. The International Society for Cellular Therapy position
statement. Cytotherapy. 8:315–317. 2006. View Article : Google Scholar
|
|
40
|
Pittenger MF, Mackay AM, Beck SC, et al:
Multilineage potential of adult human mesenchymal stem cells.
Science. 284:143–147. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Majumdar MK, Thiede MA, Mosca JD, Moorman
M and Gerson SL: Phenotypic and functional comparison of cultures
of marrow-derived mesenchymal stem cells (MSCs) and stromal cells.
J Cell Physiol. 176:57–66. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hung SC, Chen NJ, Hsieh SL, Li H, Ma HL
and Lo WH: Isolation and characterization of size-sieved stem cells
from human bone marrow. Stem Cells. 20:249–258. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Jin SZ, Meng XW, Han MZ, Sun X, Sun LY and
Liu BR: Stromal cell derived factor-1 enhances bone marrow
mononuclear cell migration in mice with acute liver failure. World
J Gastroenterol. 15:2657–2664. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Peled A, Petit I, Kollet O, et al:
Dependence of human stem cell engraftment and repopulation of
NOD/SCID mice on CXCR4. Science. 283:845–848. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Reca R, Mastellos D, Majka M, et al:
Functional receptor for C3a anaphylatoxin is expressed by normal
hematopoietic stem/progenitor cells, and C3a enhances their
homing-related responses to SDF-1. Blood. 101:3784–3793. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Forte G, Minieri M, Cossa P, et al:
Hepatocyte growth factor effects on mesenchymal stem cells:
proliferation, migration, and differentiation. Stem Cells.
24:23–33. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Jia C: Advances in the regulation of liver
regeneration. Expert Rev Gastroenterol Hepatol. 5:105–121. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ji JF, He BP, Dheen ST and Tay SS:
Interactions of chemokines and chemokine receptors mediate the
migration of mesenchymal stem cells to the impaired site in the
brain after hypoglossal nerve injury. Stem Cells. 22:415–427. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ozaki Y, Nishimura M, Sekiya K, et al:
Comprehensive analysis of chemotactic factors for bone marrow
mesenchymal stem cells. Stem Cells Dev. 16:119–129. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Salem HK and Thiemermann C: Mesenchymal
stromal cells: current understanding and clinical status. Stem
Cells. 28:585–596. 2010.PubMed/NCBI
|
|
51
|
Honczarenko M, Le Y, Swierkowski M, Ghiran
I, Glodek AM and Silberstein LE: Human bone marrow stromal cells
express a distinct set of biologically functional chemokine
receptors. Stem Cells. 24:1030–1041. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lapidot T: Mechanism of human stem cell
migration and repopulation of NOD/SCID and B2mnull NOD/SCID mice.
The role of SDF-1/CXCR4 interactions. Ann NY Acad Sci. 938:83–95.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Son BR, Marquez-Curtis LA, Kucia M, et al:
Migration of bone marrow and cord blood mesenchymal stem cells in
vitro is regulated by stromal-derived factor-1-CXCR4 and hepatocyte
growth factor-c-met axes and involves matrix metalloproteinases.
Stem Cells. 24:1254–1264. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sordi V, Malosio ML, Marchesi F, et al:
Bone marrow mesenchymal stem cells express a restricted set of
functionally active chemokine receptors capable of promoting
migration to pancreatic islets. Blood. 106:419–427. 2005.
View Article : Google Scholar
|