1. Introduction
In a world where the growth of mobile phone use and
other wireless transmitting devices (WTDs) is without precedence,
the issue of brain cancer and radiation from mobile phones has
received considerable attention in the research community and by
the general public. Occupational studies and studies of atomic bomb
survivors indicate that the latency for brain cancer could be as
long as three decades or more. The first reports on case-control
studies published on this association in the 1990s lacked
sufficient power to find an effect, because they studied persons
who had used early technology (1 and 2G) phones for relatively
limited periods of time (1–4). The
definition of ‘regular use’ (at least once a week, for 6 months or
more) during a period of rapidly increasing mobile phone use
resulted in an average use time of ~6 years. Both the INTERPHONE
Study Group (5), and Coureau et
al (6) used this definition of
‘regular use.’
In the past few years a number of investigations
have included those who have used phones for a decade or longer. In
this report we identify and evaluate all case-control studies that
incorporate decade-long use of mobile phones to provide a more
complete picture of their potential impacts on public health.
ORs for the highest cumulative hours of exposure for
brain cancer, glioma and acoustic neuroma are doubled or greater
(range, 1.82–2.89) (Table I). Of
particular interest are studies from Sweden and Korea. In the
Korean study, significant increases for acoustic neuroma occurred
with >2,000 cumulative hours of use when compared to less
(7), and in the Swedish study for
>2,300 h of cumulative use (8).
In three studies, increased risks for meningioma were also found at
the highest cumulative hours of use (5,6,9).
 | Table IBrain tumor risks in studies of
decade-long mobile and cordless phone user metrics. |
Table I
Brain tumor risks in studies of
decade-long mobile and cordless phone user metrics.
| Studies (refs.) | Tumor | OR | 95% CI | Comments |
|---|
| Cumulative hours of
use | | | | | (DECT use not
included unless stated) |
| 1,640+ | INTERPHONE Study
Group (5) | Glioma | 1.82 | 1.15–2.89 | Ref. <5 cum.
hours |
| 1,640+ | Hardell and Carlberg
(21) | Glioma | 2.31 | 1.44–3.70 | Includes DECT
use |
| ≥896 | Coureau et al
(6) | Glioma | 2.89 | 1.41–5.93 | |
| >1,640 | INTERPHONE Study
Group (12) | Acoustic neuroma | 2.79 | 1.51–5.16 | Exp. 5 years before
ref. date |
| >1,486 | | | 2.6 | 1.5–4.4 | P-trend=0.052 |
| Per 100 h | Hardell et al
(8) | Acoustic neuroma | 10.3% | 2.4–18.7% | >tumor size
analogue phone |
| >2,000 | Moon et al
(7) | Acoustic neuroma | 8.8% | 2.3–15.7% | >tumor size, ref.
<2,000 h |
| ≥1,640 | INTERPHONE Study
Group (5) | Glioma | 3.77 | 1.25–11.4 | Use for 1–4 years; a
promotion effect? |
| INTERPHONE Study
Group (5) | Meningioma | 4.80 | 1.49–15.4 | Use for 1–4 years; a
promotion effect? |
| >2,376 | Carlberg et al
(9) | Meningioma | 1.4 | 0.9–2.0 | Includes DECT
use |
| ≥896 | Coureau et al
(6) | Meningioma | 2.57 | 1.02–6.44 | |
| Coureau et al
(6) | Glioma | 8.20 | 1.37–49.07 | Urban use only |
| Years of use |
| 10+ | INTERPHONE Study
Group (5) | Glioma | 2.18 | 1.43–3.31 | Ref. 1–1.9
years |
| 10+ | Hardell et
al (10) | Glioma | 2.26 | 1.60–3.19 | Includes DECT
use |
| >5–10 | Hardell et
al (8) | Brain cancer | 1.7 | 0.98–2.8 | For mobile phone,
total |
| >25 | Hardell et
al (8) | Brain cancer | 2.9 | 1.4–5.8 | |
| >5–10 | Hardell et
al (8) | Brain cancer | 2.3 | 1.6–2.3 | |
| >20 | Hardell et
al (8) | Brain cancer | 4.5 | 2.1–9.5 | |
| Per year | Hardell et
al (12) | Acoustic
neuroma | 7.4% | 1.0–14.2% | >tumor size
analogue phone |
| >10 | Moon et al
(7) | Acoustic
neuroma | 4.5% | −1.3–10.7% | >tumor size ref.
<10 years |
| Risk by age
used |
| <20 years | Hardell and
Carlberg (22) | Brain cancer | 7.8 | 2.2–28 | Mobile phone, >1
year, ipsilateral use |
| 20–29 years | Hardell and
Carlberg (22) | Brain cancer | 2.1 | 1.5–2.9 | Mobile phone, >1
year, ipsilateral use |
| 50–80 years | Hardell and
Carlberg (22) | Brain cancer | 1.8 | 1.3–2.7 | Mobile phone, >1
year, ipsilateral use |
At the highest years of use there were significant
risks for glioma (5,10), brain cancer (8) and acoustic neuroma (11,12).
For studies with greater years of use, acoustic neuroma tumor
volume increased compared to less years of use (7,12).
2. The CERENAT study
This French case-control study of cases ≥16 years of
age diagnosed between June 2004 and May 2006 included 253 glioma
and 194 meningioma cases with two age- and gender-matched controls
per case selected between 2005 and 2008 (6).
Potential confounders considered were the level of
education, smoking, alcohol consumption, and occupational exposures
to pesticides, extremely low frequency electromagnetic fields
(ELF-EMF), radiofrequency electromagnetic fields (RF-EMFs), and
ionizing radiation. In spite of listing RF-EMF as a potential
confounder, separate analyses of exposures to digitally enhanced
cordless telephones (DECTs) were not included, because questions
about DECT use were not asked in the questionnaire.
During the period when cases were selected, the
prevalence of French mobile phone use in 2004, 2005, and 2006 was
73, 78, and 84% respectively, while the use of cordless phones is
likely to have mirrored similar patterns of increasing use
(13).
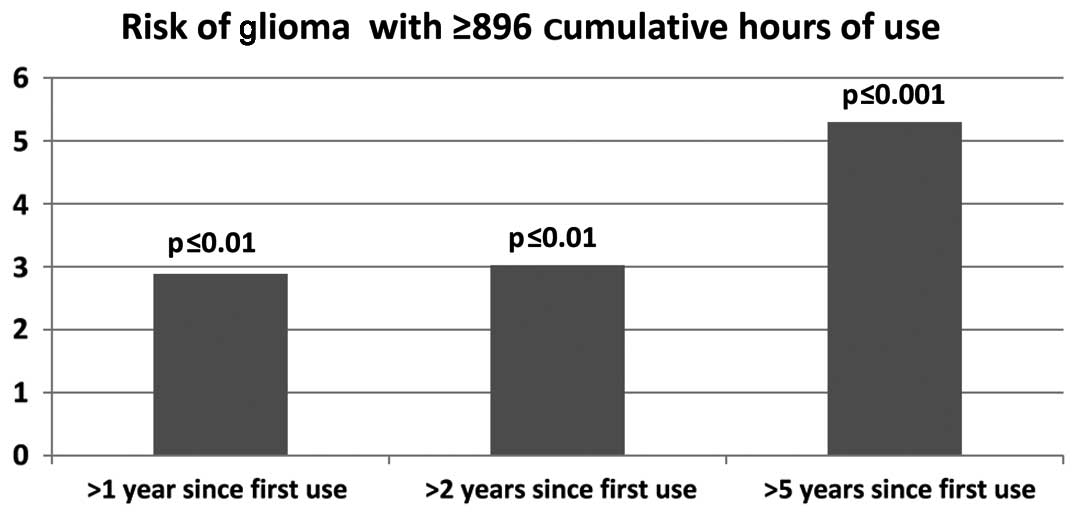
Risks of glioma were reported for ‘heavy mobile
phone use’ (≥896 cumulative hours of use) (Fig. 1). When ‘heavy mobile phone use’ was
examined by years since first use, glioma risk increased from >1
year since first use, to >2 years, and to >5 years, OR 2.89,
[95% confidence interval (CI) 1.41–5.93], OR 3.03, (95% CI
1.47–6.26), and OR 5.30, (95% CI 2.12–13.23), respectively
(6).
Risks were also reported by anatomical region. There
was a borderline significant risk for glioma in the temporal lobe,
OR 3.94 (95% CI 0.81–19.08), which when combined with at least 5
years of use increased to a significantly elevated 5.3-fold risk;
for frontal lobe tumors there was a non-significant increased risk,
OR 1.87 (95% CI 0.62–5.64), and for other regions a significant
increased risk, OR 3.61 (95% CI 1.00–12.96). Of the total mobile
phone radiation absorbed by the brain, the temporal lobe absorbs
50–60% and the frontal lobe absorbs 14–18% (14).
The highest risk reported was among heavy mobile
phone users from environments known to have multiple sources of
WTDs at work and home in urban areas, OR 8.20 (95% CI
1.37–49.07).
Higher risks were found from reported ipsilateral
use, OR 2.11 (95% CI 0.73–6.08) compared to contralateral use, OR
0.66 (95% CI 0.23–1.89).
The OR for analogue mobile phone use was 3.75 (95%
CI 0.97–14.43), that for digital mobile phone use was 2.71 (95% CI
1.03–7.10). This is consistent with mobile phone use constituting a
risk factor for glioma, because analogue mobile phones always
radiated maximum power while the digital mobile phone’s adaptive
power control circuitry reduces the radiated power consistent with
an acceptable signal to noise ratio.
For several exposure categories there was an
increased risk with increased number of hours or calls per day of
exposure: ‘average calling time per month (hours)’, p=0.02;
‘average number of calls per day’, p=0.04; ‘cumulative duration of
call (hours)’, p=0.02.
Consistent with what is expected if there is a
causal association between risks of glioma with different estimated
exposure intensities, overall for ≥896 cumulative hours of use
(‘heavy mobile phone use’), there was a significant 2.9-fold
increased risk.
3. Underestimation of risk of glioma in
CERENAT and INTERPHONE
There are two principal reasons why the CERENAT
findings as well as those of INTERPHONE are likely to have
underestimated the risks of glioma from mobile phone use. First,
exposures to RF-EMF radiation from conventional DECT can be
substantial (15). Neither in
INTERPHONE nor in CERENAT were these exposures evaluated. However
Hardell et al (8,12) reported risks of brain tumors from
these devices similar to those from mobile phones. While in the
CERENAT study RF-EMF exposures from other sources were listed as a
potential confounder, questions were not asked about DECT use.
Thus, the reference category ‘no regular use’ included subjects who
used a DECT. This misclassification of exposure biases the findings
towards the null.
Industry records reveal that the estimated
prevalence of DECT use in France (introduced into France in 1992)
was well above 50% between 2004 and 2006.
A second factor that could contribute to an
underestimation of risk is that the participation rate in CERENAT
was relatively low: 66% for cases and 45% for controls (6). The 13-country INTERPHONE study’s
average participation rate was 70% for glioma, 79% for meningioma,
56% for controls (5). The authors
of the INTERPHONE study acknowledged the possible selection bias
from low participation rates and calculated that these resulted in
a 10% underestimation of risk and the overall underestimation of
glioma and meningioma risk was per ‘the observed reductions below
the null in the ORs in ever regular mobile phone users for
meningioma (21%, 95% CI 32-9) and glioma (19%, 95% CI 30-6)’
(5).
Hardell and Carlberg (16) suggested that the CERENAT method for
analyzing laterality of risk was incorrect. In reply the CERENAT
authors provided corrected calculations, showing that ‘heavy’ users
incurred greater ipsilateral risks (≥896 cumulative hours of use)
(17) (Table II). By using the correction the OR
for the highest cumulative hours of use for glioma doubled.
 | Table IIResults for cumulative hours of use
[adapted from Coureau et al (6) Appendix 2; corrected results adapted
from Coureau et al (17)]. |
Table II
Results for cumulative hours of use
[adapted from Coureau et al (6) Appendix 2; corrected results adapted
from Coureau et al (17)].
| Glioma | Meningioma |
|---|
|
|
|
|---|
| Exposures | Ipsilaterala OR (95% CI) |
Contralateralb OR (95% CI) | Ipsilaterala OR (95% CI) |
Contralateralb OR (95% CI) |
|---|
| Cumulative hours of
use | | | | |
| Not regular
use | Referent | Referent | Referent | Referent |
| <43 | 0.43
(0.21–0.88) | 0.24
(0.10–0.57) | 0.39
(0.16–0.96) | 0.53
(0.23–1.19 |
| 43–112 | 0.39
(0.18–0.84) | 0.23
(0.08–0.63) | 0.34
(0.13–0.85) | 0.26
(0.10–0.68) |
| 113–338 | 0.87
(0.43–1.75) | 0.13
(0.04–0.44) | 0.03
(0.01–0.25) | 0.39
(0.17–0.92) |
| 339–895 | 0.86
(0.39–1.93) | 0.51
(0.21–1.28) | 0.30
(0.08–1.15) | No data |
| ≥896 | 2.11
(0.73–6.08) | 0.66
(0.23–1.89) | 2.29
(0.58–8.97) | 1.18
(0.34–4.12) |
| Cumulative hours of
use corrected | | | | |
| Not regular
use | Referent | Referent | Referent | Referent |
| <43 | 0.29
(0.11–.80) | 0.25
(0.07–0.95) | 0.64
(0.15–2.73) | 0.99
(0.34–2.90) |
| 43–112 | 0.44
(0.16–1.23) | 0.33
(0.10–1.08) | 0.37
(0.10–1.39) | 0.13
(0.02–1.07) |
| 113–338 | 0.78
(0.27–2.24) | 0.25
(0.06–1.02) | No data | 0.65
(0.23–1.80) |
| 339–895 | 1.69
(0.52–5.49) | 0.23
(0.05–1.11) | 0.14
(0.02–1.24) | No data |
| ≥896 | 4.21
(0.70–25.52) | 1.61
(0.36–7.14) | 2.27
(0.42–12.39) | 1.24
(0.21–7.48) |
For glioma, all ipsilateral ORs were greater than
contralateral ORs. With two exceptions, this was also true for
meningioma. Because ipsilateral use results in higher exposure than
contralateral, this is consistent what is expected if mobile phone
use is a risk for glioma and meningioma.
4. Meningioma elevated risk in CERENAT
‘Heavy mobile phone’ use was associated with
increased risks of meningioma (but somewhat weaker than the risks
for glioma): for >1 year, OR 2.57 (95% CI 1.02–6.44); for >2
years, OR 2.40 (95% CI 0.96–6.05), and for >5 years (5 cases),
OR 1.44 (95% CI 0.43–4.80).
Risks were non-significantly elevated for temporal
lobe (2 cases), OR 7.89 (95% CI 0.48–130.14) and for frontal lobe
(5 cases), OR 4.82 (95% CI 0.78–29.63).
There was one significant and one borderline
significant risk with increasing exposure: ‘average calling time
per month (hours)’, p=0.04; and ‘cumulative duration of calls
(hours)’, p=0.06 (6).
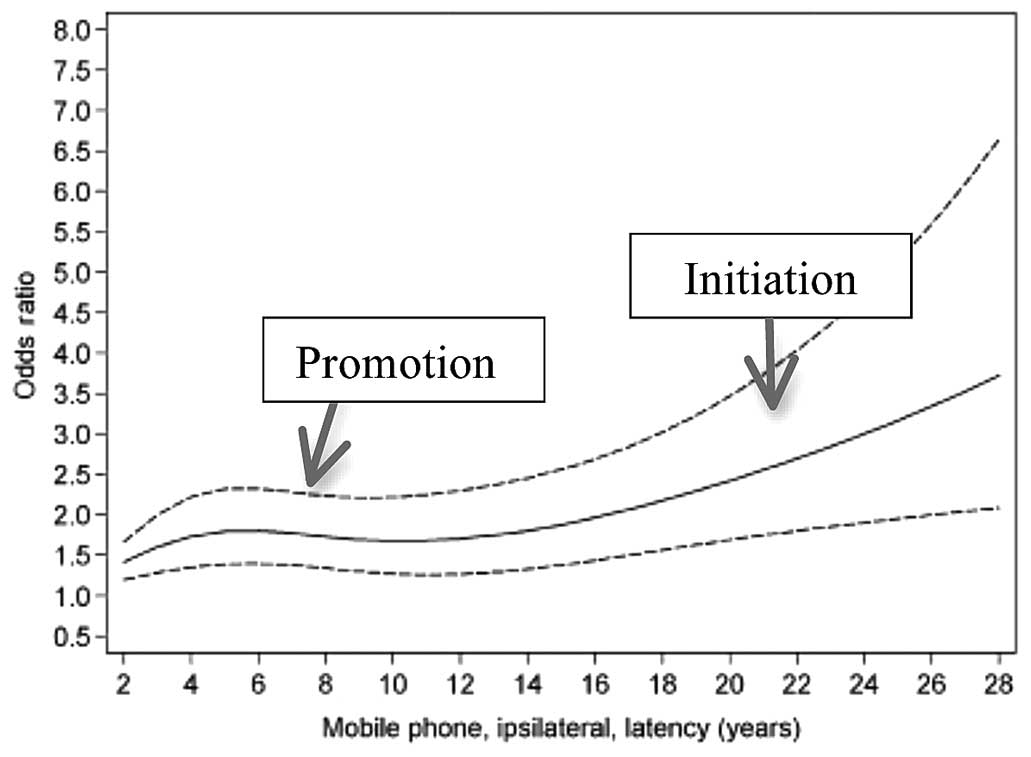
5. Evidence that electromagnetic radiation
can act both as an initiator and a promoter of tumors
For an agent that initiates a tumor, a long time to
detection is expected. Thus, brain tumors generally are believed to
have a latency of a decade or more, ranging up to five decades in
some studied populations. The average time (a statistical
distribution) to diagnosis (latency) falls within an expected range
of average times. In contrast, for an agent that acts at the later
stages of carcinogenesis, an earlier diagnosis of already initiated
tumors occurs (promotion).
With an average 2.9 years of mobile phone use Muscat
et al (4) reported a
borderline significant result for a rare brain cancer, OR 2.1 (95%
CI 0.9–4.7). Auvinen et al (1) reported a significant increased risk
of glioma with >2 years of mobile phone use, OR 2.0, (95% CI
1.0–4.1), with a dose-response increase in OR of 1.2/year (95% CI
1.1–1.5).
The INTERPHONE Study Group (5) also found indications of promoting
effects; the OR for glioma and meningioma with 1–4 years of use and
for >1,640 cumulative hours of use was 3.77 (95% CI 1.25–11.4)
and 4.80 (95% CI 1.49–15.4), respectively (Table I).
Hardell et al (18) also reported elevated risks with
short-term use. For example, the OR for meningioma and acoustic
neuroma with <1–5 years of digital mobile phone use for >64 h
was 1.8 (95% CI 1.1–3.0) and 1.9 (95% CI 0.7–4.7), respectively.
Hardell and Carlberg (15) wrote
‘...ipsilateral exposure indicated an early effect in glioma
development, which is an increased risk with long latency. However,
we also found an increased risk with short latency, indicating a
late effect in tumor development...these results could be
compatible with both tumor initiation and promotion’. This is
illustrated in Fig. 2.
6. Discussion
In reviewing the epidemiological evidence on mobile
phone use and brain tumors, The IARC Monograph Working Group
(19) noted the limited data
available from epidemiological studies at that time though noting
that Hardell et al have conducted the most detailed and
largest number of studies on the risks for glioma from wireless
phone (mobile and/or cordless phone).
Morgan et al (20) suggested that the magnitude of the
under-estimation of risk was 25% in the INTERPHONE study. This is
consistent with the INTERPHONE Study Group (5) conclusion that their under-estimation
was at least 19% based on ‘regular’ mobile phone use. Nevertheless,
when minimal use was defined as the reference level, risks in the
INTERPHONE study were significant: for 10+ years since first use
compared to 1–1.9 years since first use, OR 2.18 (95% CI
1.43–3.31), for >1,640 cumulative hours of use compared to <5
h of use, OR 1.82 (95% CI 1.15–2.80).
The IARC Monograph Working Group concluded that
radiofrequency fields were possible human carcinogens, Group 2B
(19). Since then, a number of
studies have been published of experimental results showing that
radiofrequency fields affect cellular repair and increase
biomarkers associated with cancer risk. In our view these results
and several epidemiology studies (8,21)
are consistent with what is expected if radiofrequency fields from
mobile phone use are a cause of brain cancer: the higher the
cumulative hours of use, the higher the risk; the longer the time
since first use, the higher the risk; the higher the radiated
power, the higher the risk; ipsilateral risk is higher than
contralateral risk.
Thus, evidence published since the IARC review
provides additional support, based on IARC criteria, for concluding
that radiofrequency fields are probable human carcinogens;
radiofrequency fields should now be classified Group 2A.
At the time of the IARC review it was known that
when mobile phone use began as a teenager, the risks were higher
than when use began as an adult (22,23).
Since then, additional evidence has accrued of an increased risk to
children. In the CEFALO study, using operator reported data, an OR
of 2.15 (95% CI 1.06–4.29) was reported for children of median age
13 with >2.8 years since time from first subscription, combined
with an increasing risk with increase in years since first use,
P-trend=0.001 (24). In addition,
the CEFALO authors reported an ipsilateral risk with >4 years of
cumulative duration of subscriptions, OR 3.74 (95% CI 1.19–11.77)
in combination of an increasing risk with increasing years of use,
P-trend=0.02.
As the young adult brain is not fully myelinated,
and wireless radiation has been shown to induce demyelination
experimentally, it is plausible that wireless radiation could have
a stronger impact on the developing brain than on older adults.
It has been suggested that if mobile phone use was
causing brain cancer, with so many people using mobile phones there
should be an increase in brain cancer, but there has been none
(25,26). This is not correct.
Recently a significant annual percent change (APC)
in age-adjusted rates of brain cancer between 1992 and 2006 was
reported from the United States using data from three cancer
registries: Los Angeles County (LAC), California Cancer Registry
(CCR), and the SEER 12 cancer registry (27). Table
III shows this increase in brain cancer for the three
anatomical regions that absorb the greatest proportion of the
absorbed mobile phone radiation in the brain (81% at 900 MHz and
86% at 1,800 MHz) (14).
 | Table IIIAPC of GBM by brain increased glioma
in three major cancer registries, 1992–2006 [adapted from Table III
of Deltour et al (25)]. |
Table III
APC of GBM by brain increased glioma
in three major cancer registries, 1992–2006 [adapted from Table III
of Deltour et al (25)].
| LAC | CCR | SEER 12 |
|---|
|
|
|
|
|---|
| Brain region | APC (%) | P-value | APC (%) | P-value | APC (%) | P-value |
|---|
| Frontal | +3.0 | 0.001 | +2.4 | <0.001 | +2.5 | <0.001 |
| Temporal | +2.0 | 0.010 | +1.9 | 0.026 | +1.3 | 0.027 |
| Cerebellum | N/A | N/A | +11.9 | <0.001 | +1.6 | NS |
Also showing incidence increases is an Australian
study of regional hospital-based data for the years 2000–2008.
Dobes et al (28) stated,
‘a significant increasing incidence in glioblastoma multiforme
(GBM) was observed in the study period (APC 2.5; 95% CI 0.4%–4.6,
n=2,275), particularly after 2006’.
An increasing incidence of brain tumors during
2003–2012, 41.2% among men and 46.1% in women has been noted in
Denmark, cases of GBM nearly doubled in the previous 10 years
(29).
The case-control design is generally considered the
preferred methodology for studying brain cancer risk tied with
mobile phone use, as with any relatively rare disease with
extensive exposure. The latency reported between known causes of
brain cancer and development of the disease appears to range from
10 to 50 years. Because brain cancer is a relatively rare disease
with a relatively long latency, and the reported relative risk
associated with mobile phone use thus far ranges from 1.5 to 8, in
order to have sufficient power to detect a real increase in risk
associated with mobile phone use, prospective cohort studies would
have to include >3 million persons followed for 20 years to have
80% power.
A retrospective cohort study of ~400,000 cell phone
users in Denmark has been reported evaluating brain cancer risk in
persons who began using cell phones in 1992–1994 compared to those
who began to use cell phones later (30). The authors excluded business users
from the exposed contending they were unable to know if a phone
registered to a business user was solely used by that person,
including these same business users in the unexposed category. This
misclassification of exposure impairs the ability of the study to
detect an increase in risk, while it lacks statistical power, as it
involves a small cohort for which exposure information has not been
updated for 20 years.
7. Conclusions
The CERENAT study corroborates the significant risks
of glioma associated with exposure to radiofrequency fields
reported by the Swedish team and by the 13-country INTERPHONE
study, and adds weight to the epidemiological evidence that
radiofrequency fields, classified by the International Agency for
Research on Cancer as a Group 2B (possible) carcinogen in 2011
should be reclassified as a Group 2A (probable) carcinogen.
In the CERENAT study, a significant increased risk
of brain cancer was found from mobile phone use overall with an
8-fold increased risk for higher urban exposures. Three out of
every four persons today live in mega-cities with populations of
>10 million, many in the rapidly developing world where
exposures to RF-EMF may be poorly controlled and access to medical
treatment problematic. CERENAT also corroborates those few studies
that have shown a risk of meningioma from mobile phone use.
The growth of mobile phone use worldwide has reached
the level that in many nations there are more phones than adults.
Exposures today can occur simultaneously from a number of WTDs such
as mobile phones, mobile phone base stations (as known as masts or
cell towers), and tablets, with the latter often being held quite
close to the bodies of users (ignoring that the exposure limit is
measured at 20 cm distance from tablets, laptop computer, and
similar WTDs).
Until further evidence is available, it is prudent
for policies about the use and development of WTDs rely on reducing
exposures to the ALARA standard used in pediatric radiology. The
ALARA approach would require hardware and software designers to
create proximity sensors and embed flash notices regarding simple
advisories about safer use within devices. In the meantime, we urge
that serious national programs of training and research be
established to train experts in evaluating this technology and
establish appropriate monitoring and surveillance systems such as
those in place for pharmaceuticals and other agents. This program
could be funded by a fee of 2 cents/month to be paid equally from
consumers, manufacturers, and providers into an independently
operated research and training program.
Acknowledgements
We wish to thank Barb Payne for her great
proofreading skills and the Environmental Health Trust, a
non-profit research and policy institution, for supporting this
effort.
References
|
1
|
Auvinen A, Hietanen M, Luukkonen R and
Koskela RS: Brain tumors and salivary gland cancers among cellular
telephone users. Epidemiology. 13:356–359. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Christensen HC, Schüz J, Kosteljanetz M,
Poulsen HS, Boice JD Jr, McLaughlin JK and Johansen C: Cellular
telephones and risk for brain tumors: A population-based, incident
case-control study. Neurology. 64:1189–1195. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Inskip PD, Tarone RE, Hatch EE, Wilcosky
TC, Shapiro WR, Selker RG, Fine HA, Black PM, Loeffler JS and Linet
MS: Cellular-telephone use and brain tumors. N Engl J Med.
344:79–86. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Muscat JE, Malkin MG, Thompson S, Shore
RE, Stellman SD, McRee D, Neugut AI and Wynder EL: Handheld
cellular telephone use and risk of brain cancer. JAMA.
284:3001–3007. 2000.Erratum in: JAMA 286: 1293, 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
INTERPHONE Study Group. Brain tumour risk
in relation to mobile telephone use: Results of the INTERPHONE
international case-control study. Int J Epidemiol. 39:675–694.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Coureau G, Bouvier G, Lebailly P, et al:
Mobile phone use and brain tumours in the CERENAT case-control
study. Occup Environ Med. 71:514–522. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Moon IS, Kim BG, Kim J, Lee JD and Lee WS:
Association between vestibular schwannomas and mobile phone use.
Tumour Biol. 35:581–587. 2014. View Article : Google Scholar :
|
|
8
|
Hardell L, Carlberg M, Söderqvist F and
Mild KH: Pooled analysis of case-control studies on acoustic
neuroma diagnosed 1997–2003 and 2007–2009 and use of mobile and
cordless phones. Int J Oncol. 43:1036–1044. 2013.PubMed/NCBI
|
|
9
|
Carlberg M, Söderqvist F, Hansson Mild K
and Hardell L: Meningioma patients diagnosed 2007–2009 and the
association with use of mobile and cordless phones: A case-control
study. Environ Health. 12:602013. View Article : Google Scholar
|
|
10
|
Hardell L, Carlberg M and Hansson Mild K:
Re-analysis of risk for glioma in relation to mobile telephone use:
Comparison with the results of the Interphone international
case-control study. Int J Epidemiol. 40:1126–1128. 2011. View Article : Google Scholar
|
|
11
|
INTERPHONE Study Group. Acoustic neuroma
risk in relation to mobile telephone use: Results of the INTERPHONE
international case-control study. Cancer Epidemiol. 35:453–464.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hardell L, Carlberg M, Söderqvist F and
Mild KH: Pooled analysis of case-control studies on acoustic
neuroma diagnosed 1997–2003 and 2007–2009 and use of mobile and
cordless phones. Int J Oncol. 43:1036–1044. 2013.PubMed/NCBI
|
|
13
|
The World Bank. Mobile cellular
subscriptions (per 100 people). http://data.worldbank.org/indicator/IT.CEL.SETS.P2?order=wbapi_data_value_2006wbapi_data_value&sort=asc&page=1.
Accessed September 19, 2014
|
|
14
|
Cardis E, Deltour I, Mann S, Moissonnier
M, Taki M, Varsier N, Wake K and Wiart J: Distribution of RF energy
emitted by mobile phones in anatomical structures of the brain.
Phys Med Biol. 53:2771–2783. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hardlell L and Carlberg M: Mobile phone
and cordless phone use and the risk for glioma - Analysis of pooled
case-control studies in Sweden, 1997–2003 and 2007–2009.
Pathophysiology. Oct 29–2014.(Epub ahead of print).
|
|
16
|
Hardell L and Carlberg M: Re: Mobile phone
use and brain tumours in the CERENAT case-control study. Occup
Environ Med. 72:792015. View Article : Google Scholar
|
|
17
|
Coureau G, Leffondre K, Gruber A, Bouvier
G and Baldi I: Author’s response: Re ‘Mobile phone use and brain
tumours in the CERENAT case-control study’. Occup Environ Med.
72:79–80. 2015. View Article : Google Scholar
|
|
18
|
Hardell L, Carlberg M and Hansson Mild K:
Case-control study on cellular and cordless telephones and the risk
for acoustic neuroma or meningioma in patients diagnosed 2000–2003.
Neuroepidemiology. 25:120–128. 2005. View Article : Google Scholar
|
|
19
|
International Agency for Research on
Cancer (IARC). Non- ionizing radiation, part 2: radiofrequency
electromagnetic fields. IARC Monographs on the Evaluation of
Carcinogenic Risks to Humans. 102. IARC; Lyon: 2013
|
|
20
|
Morgan LL, Kundi M and Carlberg M:
Re-evaluation of the Interphone Study: Application of a correction
factor. In: Proceedings of the Bioelectromagnetics Society Annual
Meeting; Seoul, Korea. pp. 1–7. 2010
|
|
21
|
Hardell L and Carlberg M: Using the Hill
viewpoints from 1965 for evaluating strengths of evidence of the
risk for brain tumors associated with use of mobile and cordless
phones. Rev Environ Health. 28:97–106. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hardell L and Carlberg M: Mobile phones,
cordless phones and the risk for brain tumours. Int J Oncol.
35:5–17. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hardell L, Carlberg M and Hansson Mild K:
Pooled analysis of two case-control studies on the use of cellular
and cordless telephones and the risk of benign brain tumours
diagnosed during 1997–2003. Int J Oncol. 28:509–518.
2006.PubMed/NCBI
|
|
24
|
Aydin D, Feychting M, Schüz J, et al:
Mobile phone use and brain tumors in children and adolescents: A
multicenter case-control study. J Natl Cancer Inst. 103:1264–1276.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Deltour I, Auvinen A, Feychting M,
Johansen C, Klaeboe L, Sankila R and Schüz J: Mobile phone use and
incidence of glioma in the Nordic countries 1979–2008: Consistency
check. Epidemiology. 23:301–307. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Little MP, Rajaraman P, Curtis RE, Devesa
SS, Inskip PD, Check DP and Linet MS: Mobile phone use and glioma
risk: Comparison of epidemiological study results with incidence
trends in the United States. BMJ. 344:e11472012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zada G, Bond AE, Wang YP, Giannotta SL and
Deapen D: Incidence trends in the anatomic location of primary
malignant brain tumors in the United States: 1992–2006. World
Neurosurg. 77:518–524. 2012. View Article : Google Scholar
|
|
28
|
Dobes M, Khurana VG, Shadbolt B, Jain S,
Smith SF, Smee R, Dexter M and Cook R: Increasing incidence of
glioblastoma multiforme and meningioma, and decreasing incidence of
Schwannoma (2000–2008): Findings of a multicenter Australian study.
Surg Neurol Int. 2:1762011. View Article : Google Scholar
|
|
29
|
The Danish Cancer Society. The increase in
new cases of aggressive brain cancer. http://www.cancer.dk/Nyheder/nyheds-artikler/2012kv4/Kraftigstigningihjernesvulster.html.
Accessed September 22, 2014
|
|
30
|
Schüz J, Jacobsen R, Olsen JH, Boice JD
Jr, McLaughlin JK and Johansen C: Cellular telephone use and cancer
risk: Update of a nationwide Danish cohort. J Natl Cancer Inst.
98:1707–1713. 2006. View Article : Google Scholar : PubMed/NCBI
|