Introduction
Ewing's sarcoma (ES) is an aggressive tumour with a
high incidence of local recurrence and distant metastasis, which is
more common in men compared with women, particularly in the first
2–3 decades of life (1). ES may
present with skeletal and extraskeletal forms. The skeletal form is
more common and typically occurs in the long bones of the
extremities. The extraskeletal form occurs in the soft tissues of
the lower extremities, paravertebral tissues, chest wall,
retroperitoneum and rarely in the head and neck region. ES of the
sinonasal tract is a rare occurrence and the number of clinical
studies published in the world literature, describing clinical
course and therapeutic approaches, is currently limited (2). Diagnosis is based on history,
immunostaining with at least two neural markers, ultrastructural
examination and evidence of an abnormal t(22;11) translocation,
which is the hallmark of ES (1). This
is the case report of a ES of the ethmoid sinus with intracranial
and orbital extension in a 33-year-old male patient who presented
with anosmia, epistaxis, reduction of visual acuity in the left eye
and headache.
Case report
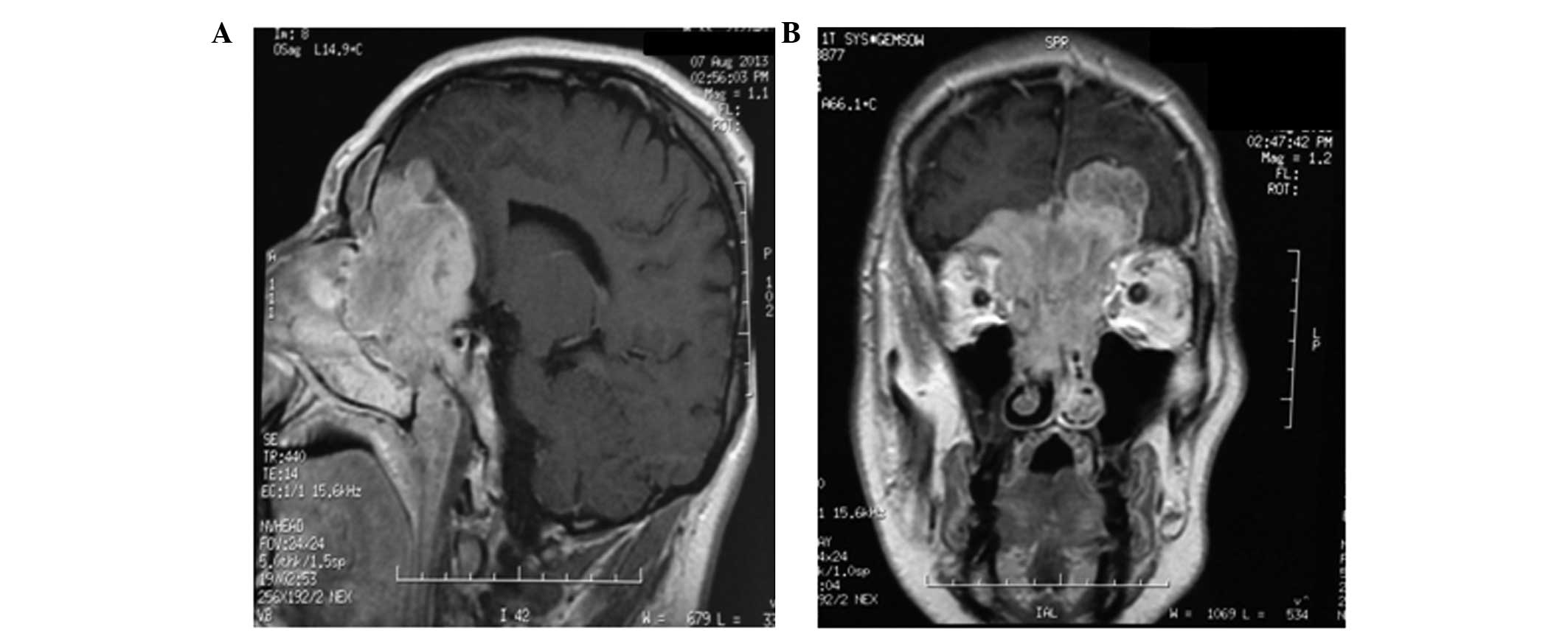
On August, 2013, a 33-year-old man underwent an
otorhinolaryngological clinical examination due to a history of
anosmia, epistaxis, reduction of visual acuity in the left eye and
headache. An otorhinolaryngological biopsy via flexible endoscope
was performed and an ethmoid sinus carcinoma was diagnosed. The
patient subsequently underwent a magnetic resonance imaging (MRI)
scan of the brain, which revealed a large mass (6×7 cm) eroding the
ethmoid and sphenoid sinuses, infiltrating the upper portion of the
nasal septum and extending to the upper posterior region of the
nasal cavities, affecting the inferior turbinates, particularly the
right turbinate. The lesion extended beyond the orbits, coming into
contact with the upper and medial rectus muscles on the right side
and with the medial rectus muscle on the left side. The lesion also
incorporated the intracranial portion of the optic nerves. The
pathological tissue occupied the anterior cranial fossa with a
maximum extension of ~5 cm, displacing and compressing the frontal
lobes, as well as the genu and horns of the corpus callosum
(Fig. 1). Subsequently, the patient
underwent surgical (combined neurosurgical and
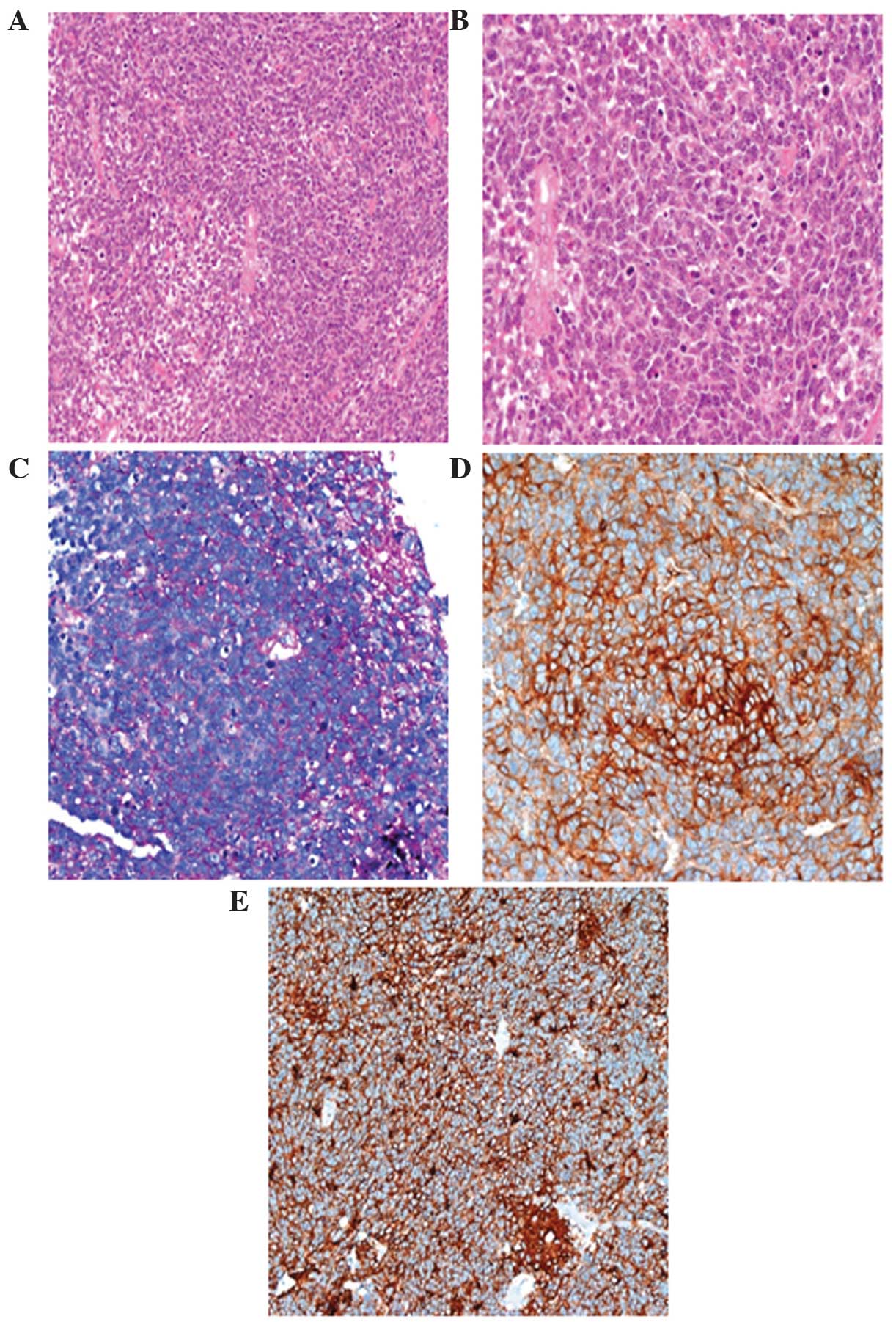
otorhinolaryngological) removal of the lesion. The microscopic
examination of the specimen revealed a population of epithelioid
cells with round nuclei and scant cytoplasm, with positive
resection margins (R2). A high number of mitotic figures and focal
necrosis were observed. The tumour cells were immunohistochemically
positive for CD99, neuron-specific enolase, CD56 and synaptophysin
and also for pancytokeratin, low-molecular weight cytokeratins and
vimentin. The periodic acid Schiff (PAS) stain exhibited strong
intracytoplasmic block positivity (Fig.
2). Furthermore, interphase fluorescence in situ
hybridization (FISH) revealed a t(22;11) translocation.
Subsequently, the diagnosis of ES was established based on the
histopathology, immunoprofile and FISH results. The diagnosis was
also confirmed following review of the slides by Professor J. Rosai
on September, 2013.
The first oncological clinical examination was
performed at the end of September, 2013.
A chemotherapy protocol that consisted of
doxorubicin (25 mg/m2 on days 1–3), ifosfamide (3,000
mg/m2 on days 1–3), 2-mercaptoethane sulfonate sodium
(mesna; 3,000 mg/m2 on days 1–3), vincristine (2 mg on
day 1) and granulocyte colony-stimulating factor (G-CSF) for
prophylaxis, was administered for a total of 3 cycles. On restaging
computed tomography, at the site of intervention, a hypervascular
inhomogeneous area sized 4,7×2,7 cm was identified, confirmed on
the subsequent MRI as local disease progression. Therefore, the
patient was ultimately treated with radiotherapy and second-line
chemotherapy. A total radiation dose of 54 Gy was delivered to the
naso-ethmoid sinus region. The second-line chemotherapy consisted
of cyclophosphamide (1,200 mg/m2 on day 1), etoposide
(150 mg/m2 on days 1–3), mesna (2,000 mg/m2
on day 1) and prophylactic G-CSF administered for 6 cycles. The
full treatment was administered every 21 days over the course of 9
months. The patient experience certain treatment-related
toxicities, including neutropenic fever (grade 4, according to the
Common Toxicity Criteria, v3.0; accessed at http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf)
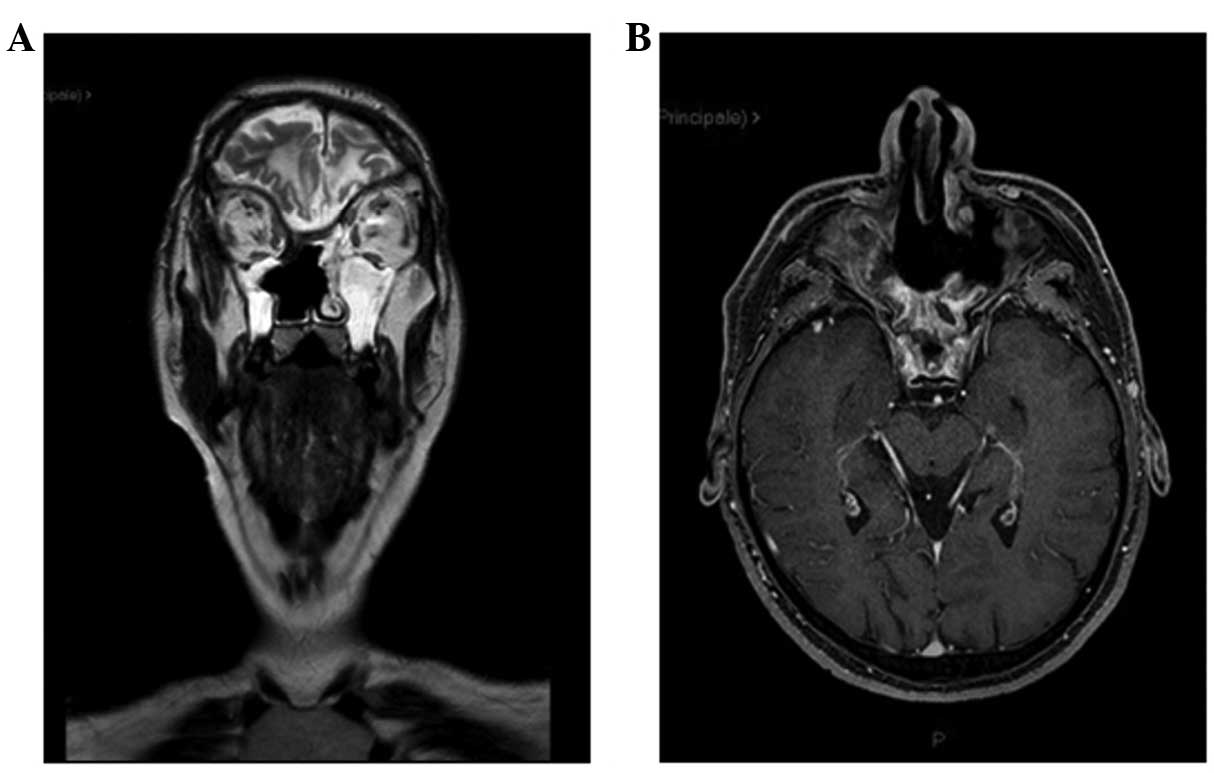
that required hospitalization. At 15 months after the diagnosis,
the patient remains recurrence-free (Fig.
3) and maintains a good functional status and quality of
life.
Discussion
We herein report a rare localization of ES in a
young male patient, who recovered well and currently remains
recurrence-free.
ES was first described by Ewing, an American
pathologist, in 1921 (3). ES is an
unusual disease, comprising ~4–6% of all primary bone tumours
(4). Involvement of the head and neck
in ES is unusual, accounting for ~1–4% of all cases, with primary
ES originating from the sinonasal tract being extremely rare. ES is
more often diagnosed during the second and third decades of life,
with a male gender predominance (4).
Microscopically, these tumours are composed of
uniform small round cells with round nuclei containing fine
chromatin, scanty clear or eosinophilic cytoplasm and PAS-positive
intracytoplasmic glycogen granules. In the sinonasal tract, the
differential diagnosis includes all tumours composed of small round
cells, such as olfactory neuroblastoma and undifferentiated
carcinoma (5). The diagnosis requires
a histopathological examination, immunohistochemistry and
cytogenetics. ES is characterized by translocation of the Ewing's
sarcoma gene (EWS) gene, which is located on 22q12.
EWS is fused with the friend leukemia virus integration site
1 gene (FLI-1), which is located on 11q24, resulting in a
t(22;11) translocation that is present in 85% of the cases of ES
and in >90% of all extraosseous ESs (6). A FISH test is used to detect the
EWS-FLI-1 fusion gene. The combination of the histological,
molecular and genetic characteristics establishes the diagnosis of
ES. This diagnosis is possible only following complete
histopathological examination of the surgical specimen; in fact,
during the first otorhinolaryngological clinical examination, the
lesion was misdiagnosed as ethmoid sinus carcinoma.
When treating ES, a multidisciplinary approach
consisting of surgical resection and radiotherapy plus chemotherapy
has increased the 5-year survival rate from 20 to 58% (7,8). The most
effective chemotherapy agents against ES are vincristine,
doxorubicin, cyclophosphamide, ifosfamide and etoposide. Using the
strategy of interval of chemotherapy cycles, the Children's
Oncology Group has demonstrated a 5-year event-free survival of 73%
in patients with localized tumours treated with these five drugs
(9). The majority of the patients
exhibit a rapid response of their primary tumour site following
chemotherapy initiation. However, recurrence of resistant tumours
either during or after completion of therapy occurs in up to
one-third of the patients, constituting a significant problem
(10). In the present case, the
patient had a recurrence after 3 cycles of first-line chemotherapy;
however, following radiotherapy and 6 cycles of second-line
chemotherapy, the patient recovered well without evidence of
recurrent disease. At 15 months after diagnosis the patient
maintains a good functional status and quality of life.
To the best of our knowledge, the availability of
scientific literature regarding ES of the ethmoid sinus is limited;
however, our results are in accordance with currently available
literature data (2,10).
Acknowledgements
The authors would like to thank Professor J. Rosai,
MD for kindly revising the immunohistochemical slides.
References
|
1
|
Tanboon J, Sitthinamsuwan B, Paruang T,
Marrano P and Thorner PS: Primary intracranial Ewing sarcoma with
an unusually aggressive course: A case report and review of the
literature. Neuropathology. 32:293–300. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li M, Hoschar AP, Budd GT, Chao ST and
Scharpf J: Primary Ewing's sarcoma of the ethmoid sinus with
intracranial and orbital extension: Case report and literature
review. Am J Otolaryngol. 34:563–568. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ewing J: Diffuse endothelioma of bone.
Pathol Soc. 21:17–24. 1921.
|
|
4
|
Balamuth NJ and Womer RB: Ewing's sarcoma.
Lancet Oncol. 11:184–192. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yeshvanth SK, Ninan K, Bhandary SK,
Lakshinarayana KP, Shetty JK and Makannavar JH: Rare case of
extraskeletal Ewings sarcoma of the sinonasal tract. J Cancer Res
Ther. 8:142–144. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Delattre O, Zucman J, Melot T, et al: The
Ewing family of tumors - a subgroup of small-round-cell tumors
defined by specific chimeric transcripts. N Engl J Med.
331:294–299. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de Bree R, van der Waal I, de Bree E and
Leemans CR: Management of adult soft tissue sarcomas of the head
and neck. Oral Oncol. 46:786–790. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Whaley JT, Indelicato DJ, Morris CG,
Hinerman RW, Amdur RJ, Mendenhall WM, Keole SR and Marcus RB Jr:
Ewing tumors of the head and neck. Am J Clin Oncol. 33:321–326.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Womer RB, West DC, Krailo MD, et al:
Randomized controlled trial of interval-compressed chemotherapy for
the treatment of localized Ewing sarcoma: A report from the
Children's Oncology Group. J Clin Oncol. 30:4148–4154. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ahmed AA, Zia H and Wagner L: Therapy
resistance mechanisms in Ewing's sarcoma family tumors. Cancer
Chemother Pharmacol. 73:657–663. 2014. View Article : Google Scholar : PubMed/NCBI
|