Introduction
The incidence of polycystic ovary syndrome (PCOS) in
females of childbearing age was 5–10% in 2004 (1). With improvements in the research of
PCOS, it has been identified that PCOS is one of the most common
types of endocrine disorder in females (2). The incidence of infertility induced
by ovulation disorders was 50–70% in 2010 (3). Therefore, drugs that promote
ovulation have become a major treatment for patients with PCOS
(4). A previous study reported
that a favorable effect has been achieved following treatment with
medicine, for example, letrozole that is used in clinics to promote
ovulation, however, the ovulation rates were high and the pregnancy
rates were low (5).
In order to investigate a method to improve the
reactivity of the ovaries to ovulation medicines, as well as the
egg quality and pregnancy outcomes, the present study was designed
to observe the blood flow around the follicles of patients with
PCOS following treatment with a low dose of aspirin in combination
with Tiao Jing Cu Yun pills, and thus investigate the clinical
value of this treatment.
Patients and methods
Patients
General information
A total of 78 patients with PCOS from the Department
of Reproductive Medicine at The Second Affiliated Hospital of
Harbin Medical University (Harbin, China) between March and
December 2012 were selected for inclusion in the present study. The
patients were of Chinese Han ethnicity from the Heilongjiang
Province. The patients were randomly divided into two groups; the
experimental group consisted of 38 patients with a mean age of
26.21±3.37 years, body mass index of 24.60±4.24 kg/m2 and duration
of infertility of 2.09±1.14 years. The control group consisted of
40 patients with a mean age of 26.30±3.38 years, body mass index of
24.52±3.86 kg/m2 and duration of infertility of 2.44±1.38 years. No
statistically significant differences between the two groups in
age, body mass index, or duration of infertility were identified.
The present study was approved by the ethics committee of The
Second Affiliated Hospital, Harbin Medical University (Harbin,
Heilongjiang, China). Written informed consent was obtained from
the patients. The trial was registered in Heilongjiang Province
Science and Technology Agency (No. LC08C19).
Diagnostic criteria
Due to the complicated heterogeneity and ethnic
differences in the clinical manifestations of PCOS, the diagnostic
criteria of PCOS has been continually disputed in individual
countries and internationally, and three sets of criteria have been
successively published (6–8). In July 2011, the Professional
Committee of the Ministry of Health Medical Service Standard set
the diagnostic criteria for PCOS in China, which is more suitable
for the diagnosis and treatment of patients of a Chinese ethnicity.
Suspected PCOS oligomenorrhea or irregular menstrual uterine
bleeding are the necessary conditions for the diagnosis of PCOS. In
addition, a patient may be diagnosed with suspected PCOS if they
exhibit one of the following two symptoms: i) High androgen
clinical manifestations or hyperandrogenism associated with high
androgen levels; or ii) an ultrasound scan revealing a polycystic
ovary, ≥12 ovarian follicles with a diameter of 0.2–0.9 cm uni- or
bilaterally, or an ovarian volume ≥10 cm3 [ovarian
volume calculated according to the formula: 0.5 × length (cm) ×
width (cm) × thickness (cm)]. To obtain a definitive diagnosis of
PCOS, the symptoms must meet the suspected diagnosed conditions as
well as the other potential causes of diseases associated with high
androgen levels. Furthermore, ovulation disorders should be ruled
out, including abnormal thyroid function, hyperprolactinemia, late
onset adrenal cortical hyperplasia, 21-hydroxylase deficiency,
adrenogenital syndrome, low ovarian reserve or premature aging of
primary ovarian function, androgen-secreting ovarian or adrenal
tumor and functional hypothalamic amenorrhea (8). All patients were aged between 22 and
30 years, sexually active and had experienced infertility for
between one and five years.
Exclusion criteria
The exclusion criteria were as follows: Patients
with a history of peptic ulcers or high blood pressure; patients
without at least one oviduct unobstructed, as confirmed by
iodolography; patients with acute genitourinary infections or
sexually transmitted diseases; patients with serious genetic,
physical or mental disorders; patients who used short-acting oral
birth control pills for ≥3 months to correct hormone levels;
patients who used metformin for ≥3 months due to insulin resistance
or abnormal glucose tolerance test results; routine inspection of
male semen of the partners of the patients during period of
ovulation promotion identified abnormalities.
Methods
Grouping
The treatment for the experimental groups was as
follows: Letrozole tablets (trade name, Winfrey; national medicine
number, H19991001; Jiangsu Hengrui Medicine Co., Ltd., Lianyungang,
China) were taken orally following five days of menstrual cramps or
withdrawal bleeding at a dose of 2.5 mg/day for five days. Also,
5-g Tiao Jing Cu Yun pills (national medicine number, Z20063997;
Shaanxi Jun Bisha Pharmaceutical Co., Ltd., Xianyang, China), which
regulate menstruation and promote pregnancy, were taken twice per
day, every day until ovulation, along with enteric-coated aspirin
tablets (national medicine number, J20080078; registered,
H20090978; Bayer S.p.A., Milan, Italy) at a dose of 100 mg/day
until the day of ovulation.
The control group were treated as follows: Winfrey
tablets were taken orally following five days of menstrual cramps
or withdrawal bleeding at a dose of 2.5 mg/day for five days.
Patients who did not become pregnant were included in the
experimental group in a subsequent cycle for ovulation
treatment.
Monitoring
Transvaginal color Doppler ultrasonography (ALOKA
ProSound Alpha 7; Hitachi Aloka Medical, Ltd. Tokyo, Japan) using a
vaginal probe (frequency, 5 mHz) and 1-ml sample volume, was
operated by the same person for each group and performed daily or
every other day to monitor follicular growth, beginning at 10–12
days of menstruation. When the diameter of a follicle was >14
mm, the urine luteinizing hormone (LH) levels were checked every
morning. When the diameter of at least one follicle was ≥18 mm and
the level of urinary LH was positive (+) or weakly positive (±),
10,000 IU human chorionic gonadotropin (hCG) hormone was
immediately injected intramuscularly to induce ovulation, with
guided copulation for 24–36 h. On the day of the hCG injection, the
number of follicles, vertical and horizontal diameters, endometrial
thickness and the hemodynamics surrounding the dominant follicle
were recorded. The sampling frame was placed around the follicular
artery with the most evident color flow, and the perifollicular
blood flow was measured following the appearance of at least three
stable waveforms. Ovulation was monitored daily by ultrasound.
Indications of mature follicle ovulation were as follows: The
dominant follicles grew from 1.0 cm to ≥2.2 cm in diameter,
followed by sudden disappearance, with surrounding echo
enhancement. There was effusion in the posterior fornix. Then the
echo-free zone in ovarian became fuzzy, with sparse dot- or
cluster-like echoes, indicating formation of corpus luteum
(9). The patients were
administered with luteal support following ovulation, and the blood
β-hCG was measured 14 days subsequently to determine whether the
patient was pregnant, this is termed a biochemical pregnancy. After
28 days of ovulation, a vaginal ultrasound was performed as
described above, to observe the gestational sac and fetal heart
beat, which determined a clinical pregnancy.
Statistical analysis
SPSS statistical software, version 16.0 (SPSS, Inc.,
Chicago, IL, USA) was used for the statistical analysis. All data
are presented as the mean ± standard deviation and comparisons
between groups were conducted using the independent samples t-test.
The paired t-test was used to compare data prior to and following
treatment; P<0.05 was considered to indicate a statistically
significant difference.
Results
Blood flow performance surrounding the
follicles of the two different groups using Doppler
ultrasonography
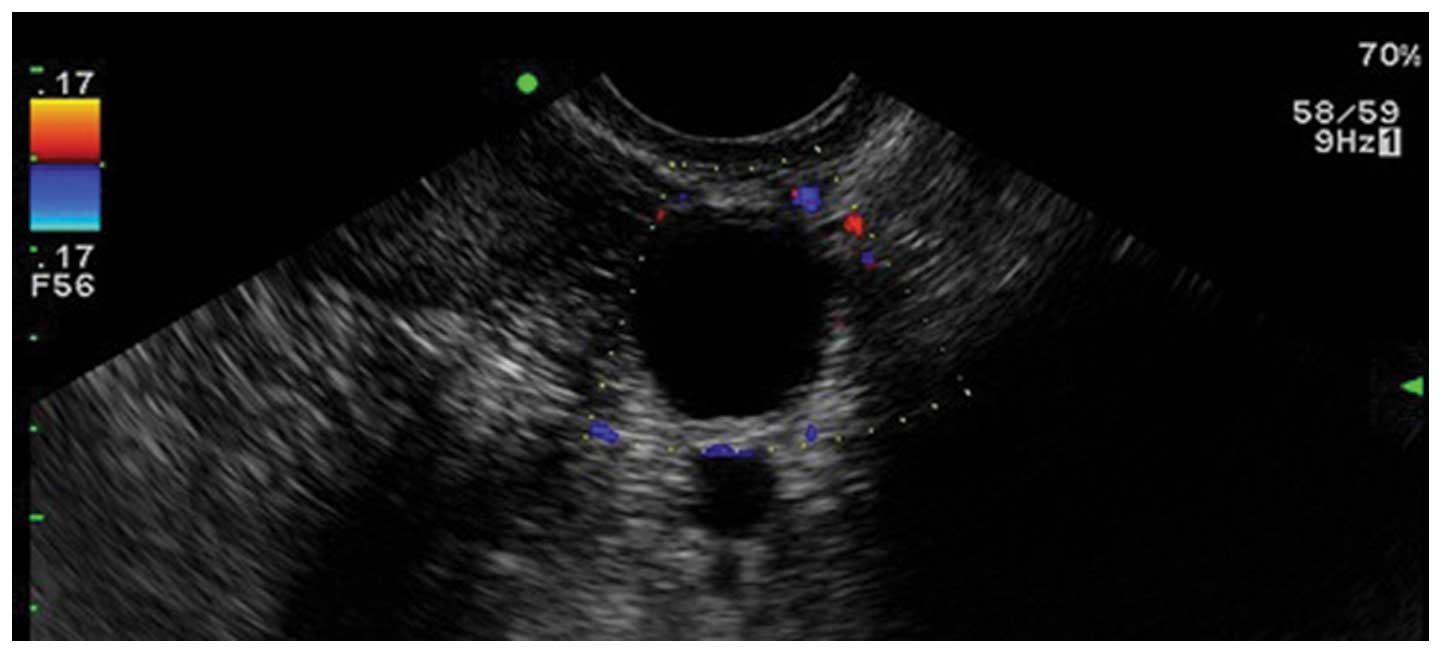
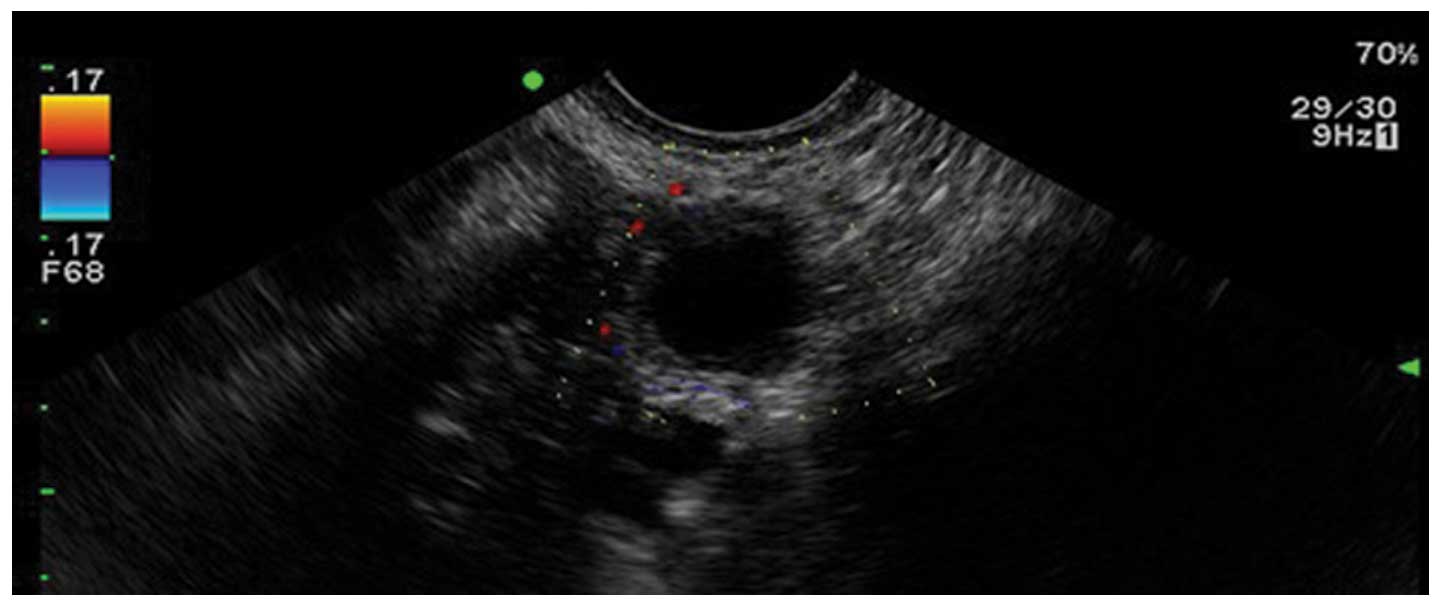
On the day of hCG injection, in the experimental
group, the dominant follicles had strong echo signal of peripheral
blood flow, with engorged perfusion and vigorous beating (Fig. 1). The patients in the control group
exhibited a sparsely punctuated multi-display color flow signal or
no color flow signals around the follicles (Fig. 2).
Endometrial thickness and clinical
pregnancy rate in the two different groups
On the day of the hCG injection, the endometrial
thickness was not identified to be significantly different between
the two groups (P>0.05). The clinical pregnancy rate of the
experimental group was significantly elevated compared with that of
the control group. The significant difference is shown in Table I.
 | Table IEndometrial thickness and clinical
effect in the experimental and control groups on the day of human
chorionic gonadotropin administration. |
Table I
Endometrial thickness and clinical
effect in the experimental and control groups on the day of human
chorionic gonadotropin administration.
| Group | Cases | Endometrial thickness
(mm) | Clinical pregnancy
rate (%) |
|---|
| Experimental | 38 | 9.376±1.187a | 42.11b |
| Control | 40 | 8.995±1.371 | 27.50 |
Perifollicular arterial blood flow
correlation coefficient test results
Of the surrounding follicular flow parameters, the
pulsatility index (PI), resistance index (RI) and end diastolic
velocity (EDV) values in the experimental group were significantly
different compared with those in the control group (P<0.01). No
significant difference in the peak systolic velocity (PSV) values
between the two groups was identified (P>0.05; Table II).
 | Table IIPerifollicular blood flow parameters
of the experimental and control groups on the day of human
chorionic gonadotropin administration. |
Table II
Perifollicular blood flow parameters
of the experimental and control groups on the day of human
chorionic gonadotropin administration.
| | Perifollicular blood
flow parameter |
|---|
| |
|
|---|
| Case | Cases | PI | RI | PSV | EDV |
|---|
| Experimental | 38 | 0.898±0.874a | 0.60±0.546a | 16.423±2.077 | 6.463±1.075a |
| Control | 40 | 1.027±0.944 | 0.659±0.560 | 16.825±2.858 | 5.628±0.982 |
The patients in the control group who did not become
pregnant were reintegrated into the experimental group (n=29),
receiving ovulation treatment. The follicles were monitored on the
day of HCG injection. Significant differences were identified in
the perifollicular blood flow parameters PI and RI of the dominant
follicles between prior to and following treatment with aspirin and
Tiao Jing Cu Yun pills (P<0.01), with a significant difference
in EDV values (P<0.05). However, no significant difference in
the PSV values between prior to and following the treatment was
observed (P>0.05; Table
III).
 | Table IIIComparison of perifollicular blood
flow parameters prior to and following treatment. |
Table III
Comparison of perifollicular blood
flow parameters prior to and following treatment.
| Perifollicular blood
flow parameter |
|---|
|
|
|---|
| Case | PI | RI | PSV | EDV |
|---|
| Prior to | 0.970±0.085 | 0.651±0.039 | 16.727±1.978 | 5.845±0.797 |
| Following | 0.907±0.081a | 0.605±0.043a | 15.851±2.437 | 6.228±0.813b |
Clinical outcome between the patients in
the control group and those reintegrated into the experimental
group
The control group pregnancy rate was only 27.50%,
while that of the experimental group of patients who were
reintegrated in the second cycle was 37.93%, which was
significantly higher (P<0.05; Table IV).
 | Table IVClinical outcome in the new
experimental and control groups. |
Table IV
Clinical outcome in the new
experimental and control groups.
| Group | Cases | Clinical pregnancy
rate (%) |
|---|
| New experimental | 29 | 37.93 |
| Control | 40 | 27.50 |
Discussion
Infertility is closely associated with intense
social competition and the increasing pressures of life (10). Numerous patients make the
uninformed decision to seek assisted reproductive technologies,
including IVF treatment. However, the majority of these patients
only require an agent for endocrine regulation or a treatment that
stimulates ovulation; fertility is achievable in certain patients
simply by monitoring ovulation. PCOS is currently the most common
cause of menstrual disorders in young females and it is the primary
cause of ovulatory infertility (11). A high-quality mature egg is the
most important factor for a successful pregnancy. At present, the
predominant method of judging whether a follicle is mature involves
measuring the size and morphological changes of the follicle by
ultrasound and testing the plasma estrogen levels; judgment of
follicle maturation by the morphology alone is not reliable.
Therefore, a reliable and effective method is required (12–14).
In 1991, Kurjak et al (15) proposed that blood flow parameters
surrounding the follicle could be used as an index to evaluate
follicular growth, maturation and ovulation. The function status of
a reproductive organ is closely associated with its angiogenesis
and hemodynamic performance. The blood circulation status, amount
of tissue blood perfusion and blood flow resistance are
prerequisite conditions for the growth and development of ovarian
follicles. In a previous study, it was demonstrated that following
the injection of hCG, the values of the ovarian artery blood flow
indexes, PI and RI, predict the development of follicles, and are
reliable indicators for evaluating the degree of maturity of
follicles and the quality of the ova (16). The present study indicated that the
color signal surrounding the follicles was stronger in the group of
patients taking letrozole alone compared with that of the group,
which were treated with a combination of aspirin and Tiao Jing Cu
Yun pills. This result indicated that the peripheral vascular
formation of the follicles was increased, the liquid oxygen content
of the follicles was rich and the conception rate was also high.
Additionally, the present study demonstrated that the arterial
blood flow index surrounding the follicle, presented as the values
of PI and RI, was significantly higher compared with that of the
experimental group. This result may be due to the fact that
letrozole leads to increased synthesis and activity of
follicle-stimulating hormone (FSH) through reducing estrogen
synthesis. Due to the secretion of FSH, the concentrations of
estradiol (E2) and progesterone in the serum rise, and the
increasing concentration of progesterone antagonizes the
vasodilation function of E2. The values of RI and PI of the
follicular peripheral artery increase, which reduces the follicular
blood perfusion rate and affects follicle maturation.
Aspirin has been used in the clinical setting for
hundreds of years (17). The
efficacy and safety of the application dose of aspirin used in
infertility treatment remains controversial. Aspirin inhibits the
activity of platelets, prevents the formation of microthrombi,
reduces intravascular resistance and improves the local blood
circulation (18). Low-dose
aspirin (50–150 mg/day) reduces the tension of blood vessels, and
improves tissue perfusion (19,20),
which increases the endometrial thickness, gland area, and
activation of various female and progestational hormone receptors.
Furthermore, aspirin improves the response to ovarian hormones,
which improves the clinical pregnancy rate. The present study
identified that, on the day hCG was injected, the perfusion of the
peripheral artery of the dominant follicle increased, and the blood
resistance of the PI, RI and PSV markedly decreased following
treatment of PCOS with letrozole combined with aspirin, when
compared with those of the control group. These changes are
beneficial to the development and maturation of dominant follicles.
In traditional Chinese medicine the kidneys are considered to be
the key organs for the control of reproduction, the egg is the core
of reproduction and fertility and is hidden in the kidney. Numerous
Chinese traditional medicines are used to activate the blood
circulation, nourish nerves, increase the blood flow around the
ovaries and other endocrine glands, and induce the mature follicle
to break away from the ovary. At the same time, the medicine is
conducive to the implantation of a fertilized egg by improving the
uterine blood supply and promoting the growth of the decidua.
The Tiao Jing Cu Yun pills contain numerous
ingredients, including Astragalus, dodder, pilose antler,
medlar, broiled Epimedium, Himalayan teasel root, parasitic
Loranthus and Chinese yam. The pills have the function of
tonifying the lddney and Yang, promoting blood circulation to
restore menstrual flow, tuning up Chong and Ren, and aid with
conception. Furthermore, the pills stimulate the ovaries and are
involved in endocrine regulation, and promoting and inducing
ovulation. Combined with suberect Spatholobus stem,
Salvia miltiorrhiza, raspberry, poria cocos, Radix Paeoniae
Rubra and Rhizoma Curculiginis, the pills are good for the kidney
and spleen, and also promote blood circulation to restore menstrual
flow and regulate menstrual function. The pill improves the
function of the hypothalamic-pituitary-ovarian axis and stimulates
the vitality of the ovaries (21).
Tiao Jing Cu Yun pills have synergy with aspirin in promoting
ovulation. It increases the ovulation rate and the probability of
pregnancy by promoting ovulation and increasing the thickness of
the endometrium, thus creating a favorable internal environment for
implantation (22). The present
study demonstrated that, on the day of the hCG injection, although
the endometrial thickness was not significantly different in the
group treated with lentrozole combined with aspirin and Tiao Jing
Cu Yun pills compared with that of the control group, it was a
suitable endometrial thickness (23). The results of the present study
showed that the clinical pregnancy rate was 42.11% in the
experimental group; however, in the control group it was only
27.50%. The patients in the control group that had not become
pregnant were integrated into the experimental group for the
subsequent cycle and the clinical pregnancy rate was 37.93%. This
result indicated that letrozole combined with a small dose of
aspirin and Tiao Jing Cu Yun pills results in an increased
pregnancy rate in females with PCOS.
In conclusion, the promotion of menstruation via the
combined use of low-dose aspirin, Tiao Jing Cu Yun pill and
letrozole induces ovulation, follicular development and leads to
pregnancy. A marked increase in clinical pregnancy rates was
observed as a result of ovulation induction, which was
significantly higher compared with using ovulation treatment. This
method can replace conventional ovulation-induction treatments,
which are associated with numerous side-effects, with the overall
effect presenting as an improvement of the internal environment of
the body. This treatment method is simple to use, affordable and
the effect is significant; furthermore, it is a relatively safe and
reliable infertility treatment option, worthy of promotion and
application.
References
|
1
|
Archer JS and Chang RJ: Hirsutism and acne
in polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol.
18:737–754. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Azziz R, Woods KS, Reyna R, Key TJ,
Knochenhauer ES and Yildiz BO: The prevalence and features of the
polycystic ovary syndrome in an unselected population. J Clin
Endocrinol Metab. 89:2745–2749. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hu WH, Qiao J, Wang LN and Tong J:
Clinical features of the metabolic syndrome in patients with
polycystic ovary syndrome. Beijing Da Xue Xue Bao. 42:159–163.
2010.(In Chinese).
|
|
4
|
Nahid L and Sirous K: Comparison of the
effects of letrozole and clomiphene citrate for ovulation induction
in infertile women with polycystic ovary syndrome. Minerva Ginecol.
64:253–258. 2012.PubMed/NCBI
|
|
5
|
Nahid L and Sirous K: Comparison of the
effects of letrozole and clomiphene citrate for ovulation induction
in infertile women with polycystic ovary syndrome. Minerva Ginecol.
64:253–258. 2012.PubMed/NCBI
|
|
6
|
Rotterdam ESHRE/ASRM-Sponsored PCOS
consensus workshop group. Revised 2003 consensus on diagnostic
criteria and long-term health risks related to polycystic ovary
syndrome (PCOS). Human reprod. 19:41–47. 2004. View Article : Google Scholar
|
|
7
|
Azziz R, Carmina E, Dewailly D, et al:
Androgen Excess Society: Positions statement: criteria for defining
polycystic ovary syndrome as a predominantly hyperandrogenic
syndrome: an Androgen Excess Society guideline. J Clin Endocrinol
Metab. 91:4237–4245. 2006. View Article : Google Scholar
|
|
8
|
Health industry standard of the People’s
Republic. Diagnosis of the polycystic ovary syndrome (WS 330–2011).
The Ministry of Health Medical Service Standard Professional
Committee of the People’s Republic of China; 2011
|
|
9
|
Zhang XN: Research on uterine and ovarian
arterial blood flow for kidney-tonification and blood
stasis-elimination treatment of polycystic ovarian syndrome. Chin J
Pract Med. 26:864–867. 2010.(In Chinese).
|
|
10
|
Thessaloniki ESHRE/ASRM-Sponsored PCOS
Consensus Workshop Group. Consensus on infertility treatment
related to polycystic ovary syndrome. Hum Reprod. 23:462–477. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goldenberg N and Glueck C: Medical therapy
in women with polycystic ovarian syndrome before and during
pregnancy and lactation. Minerva Ginecol. 60:63–75. 2008.PubMed/NCBI
|
|
12
|
Borini A, Maccolini A, Tallarini A, Bonu
MA, Sciajno R and Flamigni C: Perifollicular vascularity and its
relationship with oocyte maturity and IVF outcome. Ann NY Acad Sci.
943:64–67. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jokubkiene L, Sladkevicius P, Rovas L and
Valentin L: Assessment of changes in volume and vascularity of the
ovaries during the normal menstrual cycle using three-dimensional
power Doppler ultrasound. Hum Reprod. 21:2661–2668. 2006.
|
|
14
|
Otsuki J, Okada A, Morimoto K, Nagai Y and
Kubo H: The relationship between pregnancy outcome and smooth
endoplasmic reticulum clusters in MII human oocytes. Hum Reprod.
19:1591–1597. 2004. View Article : Google Scholar
|
|
15
|
Kurjak A, Kupesic-Urek S, Schulman H and
Zalud I: Transvaginal color flow Doppler in the assessment of
ovarian and uterine blood flow in infertile women. Fertil Steril.
56:870–873. 1991.PubMed/NCBI
|
|
16
|
Du B, Takahashi K, Ishida GM, Nakahara K,
Saito H and Kurachi H: Usefulness of intraovarian artery
pulsatility and resistance indices measurement on the day of
follicle aspiration for the assessment of oocyte quality. Fertil
Steril. 85:366–370. 2006. View Article : Google Scholar
|
|
17
|
Ozturk O, Greaves M and Templeton A:
Aspirin dilemma. Remodelling the hypothesis from a fertility
perspective. Hum Reprod. 17:1146–1148. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Saito H, Kaneko T, Kawachiya S, Du B,
Ishida GM and Kurachi H: Effects of aspirin on the oocyte quality.
Fertil Steril. 76:S1312001. View Article : Google Scholar
|
|
19
|
Patrono C, García Rodríguez LA, Landolfi R
and Baigent C: Low-dose aspirin for the prevention of
atherosclerosis. N Engl J Med. 353:2373–2383. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Daya S: Is there a benefit of low-dose
aspirin in assisted reproduction? Curr Opin Obstet Gynecol.
18:313–318. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lai Q: 96 cases of clinical observation on
Tiao Jing Cu Yun pills treatment for ovulation inhibition. Chin J
Cosmetic Med. 20:3532011.
|
|
22
|
Xu ZM, Zhou YH and Peng JY: Curative
effect observation on Tiao Jing Cu Yun pills for polycystic ovarian
syndrome. Chin J Shanxi Trad Chi Med. 27:18–19. 2004.(In
Chinese).
|
|
23
|
Isaacs JD Jr, Wells CS, Williams DB, Odem
RR, Gast MJ and Strickler RC: Endometrial thickness is a valid
monitoring parameter in cycles of ovulation induction with
menotropins alone. Fertil Steril. 65:262–266. 1996.PubMed/NCBI
|