Introduction
Epilepsy is one of the most prevalent and serious
central nervous system disorders that affects ~1% of the global
population (1). In previous
epilepsy studies, burst activities were often followed by a
depression of spike discharges, termed after burst depression (ABD)
or postictal depression (2–6).
This low-amplitude neuronal activity is believed to result from the
factors that lead to seizure auto-termination. This depression
period is very important, as it can extend the interval duration of
burst activity and also reduce the intensity of seizure onset. A
number of antiepileptic drugs can enhance this depression period in
patients with epilepsy (7).
Although a number of previous studies concentrated
on the dynamics of ion channels and other proteins in epileptic
seizure, little is known regarding the development of postictal
depression (8,9). One possibility is that there may be a
large influx of calcium ions during this burst activity, which may
activate calcium-activated potassium channels and thus mediate the
hyperpolarized current and lead to postictal depression (10,11).
Calcium-activated potassium channels are a group of potassium
channels that are different to voltage-gated potassium channels as
they are activated by elevated intracellular calcium concentration.
They can be divided into 2 types: Big conductance calcium-activated
potassium channels known as BK channels, and the small conductance
type known as SK channels (12).
BK channels contribute to the fast and medium after
hyperpolarization (AHP) activities that follow a single action
potential (AP). In contrast, SK channels have a small conductance
with a longer open duration, and they contribute to the slow AHP
activities of neurons following a series of APs (13–15).
In addition to this hypothesis involving
calcium-activated potassium channels, there are still a number of
other potential mechanisms. One such mechanism may involve membrane
shunting (16), which is
associated with a decrease in neuronal input resistance, a
consequence of seizure onset. Membrane shunting decreases the
synaptic current effect on the postsynaptic membrane and also
decreases the coupling effect of gap junctions. The energy failure
hypothesis has also been suggested as another potential mechanism.
Depletion of energy substances, such as ATP and glucose, may be an
important factor in ABD. However, it has been previously
established that hypoglycemia and hypoxia may lead to a seizure
onset rather than seizure control (17).
An increasing number of previous studies have
demonstrated that SK channels have an important role in
epileptogenesis (18,19). In the central nervous system, SK
channels couple directly with N-methyl-D-aspartate (NMDA) receptors
in dendritic spines. Calcium influx through NMDA receptors during
membrane depolarization can activate SK channels (20). In addition, activation of SK
channels may reduce epileptiform activity in an acute model of
epilepsy (21). By contrast,
suppression of SK channels may increase burst activity in the
hippocampal CA3 area of a brain slice (22,23).
Thus, SK channels may be critical in the formation of postictal
depression and spontaneous seizure control. In the present study,
cyclothiazide (CTZ) was used to establish the epilepsy model. CTZ
is a novel potent convulsant with the advantage of lower
excitotoxicity (24) and it is
capable of inducing a stable burst activity in vitro and
in vivo (24,25). CTZ induces convulsion via a number
of different physiological processes. The most important effect is
the allosteric modulation of AMPA and GABA receptors (26). In addition, there are also a number
of other mechanisms that contribute to the convulsant effect of
CTZ, including glutamate depletion (27), dynamic changes in ion
concentrations (28), persistent
activation of hyperpolarization activated cation conductance
(2,21,23)
and activation of acid-sensitive ion channels (3). On the basis of these previous
studies, it was hypothesized that SK channels may enhance the
amplitude and duration of ABD and control the strength of
seizures.
Materials and methods
Animals
The electroencephalographic experiments were
performed on 250–300 g male Sprague Dawley rats, 8 weeks old. These
rats were supplied by Shanghai SLAC Laboratory Animal Co., Ltd.
(Shanghai, China). In this study, 20 rats were used for the
experiments. All animals were maintained in air-conditioned rooms
with a controlled temperature at 23±2°C, 40–60% humidity, under a
12 h light/dark cycle with lights on from 7:00 a.m. to 7:00 p.m.
Animals were housed separately in plastic cages and were supplied
with water and food ad libitum. All experiments conformed to
the guidelines provided by the Institutional Committee of
Laboratory Animals, Fudan University and to Chinese government
regulations. The present study was approved by the Ethics Committee
of Fudan University (Shanghai, China).
Surgery and intracranial cortical
electroencephalogram (EEG) quantification
The protocols applied for surgery and
electroencephalography were performed as previously described
(25,29,30).
Briefly, as CTZ cannot pass through the blood-brain barrier, all
studies were performed using an intraventricular injection of CTZ.
Animals were mounted on stereotaxic apparatus, with a guide cannula
(22GA; Plastics One, Roanoke, VA, USA) planted into the lateral
ventricle (AP 0.3 mm, ML 1.3 mm, DP 4.0 mm). The intraventricular
CTZ injection was performed through a soft plastic catheter and
this guide cannula. To record the cortical EEG, two little screw
electrodes were embedded into the skull to reach the surface of the
brain. One screw was located in the left cortex above the
hippocampus (AP-3.8 mm, ML 2.0 mm), which served as the recording
electrode, while the other was located above the forehead, serving
as the reference electrode. Finally, two screws were attached to a
connector to create a link to the Neurolog system (Digitimer Ltd.,
Hertfordshire, UK). The signals were visualized by Spike2 software
version 6.04 (Cambridge Electronic Design Ltd., Cambridge, UK) and
recorded on a PC computer through an A-D converter, CED 1401 micro
(Cambridge Electronic Design Ltd.).
Primary hippocampal neuronal
culture
Primary hippocampal neurons were collected from
embryonic day 18 Sprague-Dawley rat fetuses, as described in our
previous studies (31–33). Briefly, the fetuses were first
dissected to collect the hippocampi. The tissues were rinsed in
cold Hanks' balanced salt solution, then digested with 0.05%
trypsin-EDTA solution for 15–20 min at 37°C. Following digestion,
single cells were subsequently isolated by trituration with 1 ml
plastic pipette tips in the plating medium (Dulbecco's modified
Eagle's medium with 10% fetal bovine serum, 10% F12 and 25 m/ml
penicillin/streptomycin, termed DF12; purchased from Invitrogen
(Thermo Fisher Scientific, Inc., Waltham, MA, USA), and then a
centrifugation step of 1,000 × g at 4°C, for 8 min. Then, following
rinsing twice by DF12, cells were seeded onto poly-D-lysine (0.1
mg/ml; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) pre-coated
coverslips at a density of 40,000–60,000 cells/cm2.
Following cell culture for 1 day, half of the media were changed to
neurobasal medium, containing 2% B27, 2 mM GlutaMAX™ and
25 ml/ml penicillin/streptomycin. AraC (1 µM; Sigma-Aldrich; Merck
KGaA) was added at 6 days following initial plating. Cell cultures
were fed once every 3 days by replacing half of the medium. All
cultures were maintained at 37°C and in 5% CO2
incubators. Following 14–21 days after plating, cultured neurons
were used for electrophysiology. All cell culture reagents were
obtained from Invitrogen; Thermo Fisher Scientific, Inc. (Waltham,
MA, USA).
Drug treatment
To induce robust burst activity in cultured neurons,
stock CTZ (Tocris Bioscience, Bristol, UK) solution (20 mM in DMSO)
was added into the culture medium to produce a final concentration
of either 5 or 20 µM CTZ. A similar volume of DMSO (1:1,000) was
added into the cultured medium as a control to form the DMSO group.
The two CTZ groups (5 or 20 µM CTZ) and the DMSO group, with 12–32
neurons in each group, were incubated for 2 h at 37°C prior to
patch clamp recordings. The SK channel antagonist, apamin (APM;
Tocris Bioscience, Bristol, UK), and the BK channel antagonist,
iberiotoxin (IBTX; Tocris Bioscience), were dissolved in water to
produce two stock solutions (500 µM), which were then added into
the bath solution to produce final concentrations of 500 nM,
forming +APM and +IBTX groups of neurons cultured with CTZ and
DMSO, respectively.
Electrophysiology
Whole-cell recordings were performed in current
clamps and held at −70 mV as described previously (24,32,34,35).
Patch pipettes were pulled from borosilicate glass with a pipette
puller (P-97; Sutter Instrument, Novato, CA, USA), and then fire
polished to a resistance of 3–6 MΩ. The pipette was filled with
following internal solution: 125 mM K-gluconate, 10 mM KCl, 10 mM
Hepes, 10 mM Tris-phosphocreatine, 4 mM MgATP, 0.5 mM
Na2GTP (pH 7.3 adjusted with KOH) and ~305 mM Osm. An
additional 30 mM ethylene glycol-bis(β-aminoethyl
ether)-N,N,N',N'-tetraacetic acid (EGTA) was added into the
internal solution for experiments involving high EGTA recordings,
with the same pH and osmolarity as normal; resulting in the EGTA
and Normal groups in CTZ and DMSO cultured neurons, respectively.
The recording chamber was continuously perfused with a bath
solution, containing the following components: 128 mM NaCl, 30 mM
Glucose, 25 mM Hepes, 5 mM KCl, 2 mM CaCl2, 1 mM
MgCl2 (pH 7.3 adjusted with NaOH) and ~315 mM Osm.
Electrical signals were digitized and sampled at a frequency of 5
kHz with Digidata 1440A and Multiclamp 700B amplifier (Axon
Instruments; Molecular Devices, LLC, Sunnyvale, CA, USA), using
pCLAMP version 10.2 (Axon Instruments; Molecular Devices, LLC).
Data were filtered at 2 kHz and analyzed with Clampfix version 10
(Axon Instruments; Molecular Devices, LLC). A large depolarization
shift was defined as a membrane potential ≥10 mV depolarizing
shift, with a ≥300 msec time period. An epileptiform burst was
defined by ≥5 consecutive APs overlaying on top of a large
depolarization shift (24). A
neuron with burst activities was defined by ≥2 repeated bursts
occurring within 6 min of recording (25,32).
Data within a group have ≥3 different groups of neurons. A bursting
neuron was not calculated in the analysis if the recording time was
<6 min, even if it had bursts ≥2. Only bursting neurons were
used for further analyses, including burst frequency, burst
duration, amplitude and duration of after burst hyperpolarization
(ABH) and the AP frequency in burst.
Statistical analysis
All of the ABH and burst results recorded in
cultured neurons were analyzed using Clampfit version 10 (Axon
Instruments; Molecular Devices, LLC). A 5-min baseline was recorded
for every neuron, and the baseline was calculated to confirm the
membrane potential value of the mean and noise using the software.
The value of the mean ± noise represents the baseline region. ABH
amplitude is calculated by baseline mean minus the negative peak
potential of ABH. ABH duration represents the lasting time of the
hyperpolarizing activity. There was potential of high level of
noise in the potential recording; therefore, the present study used
the baseline region rather than the single baseline value to reduce
the influence of noise as much as possible. Similarly, the baseline
definition in burst duration is also the same as that in ABH
duration. Finally, the AP frequency in burst was calculated by
dividing the AP number by the burst duration.
Pooled data are all presented as the mean ± standard
error mean and were analyzed using GraphPad Prism version 4
(GraphPad Software, Inc., La Jolla, CA, USA). An unpaired Student's
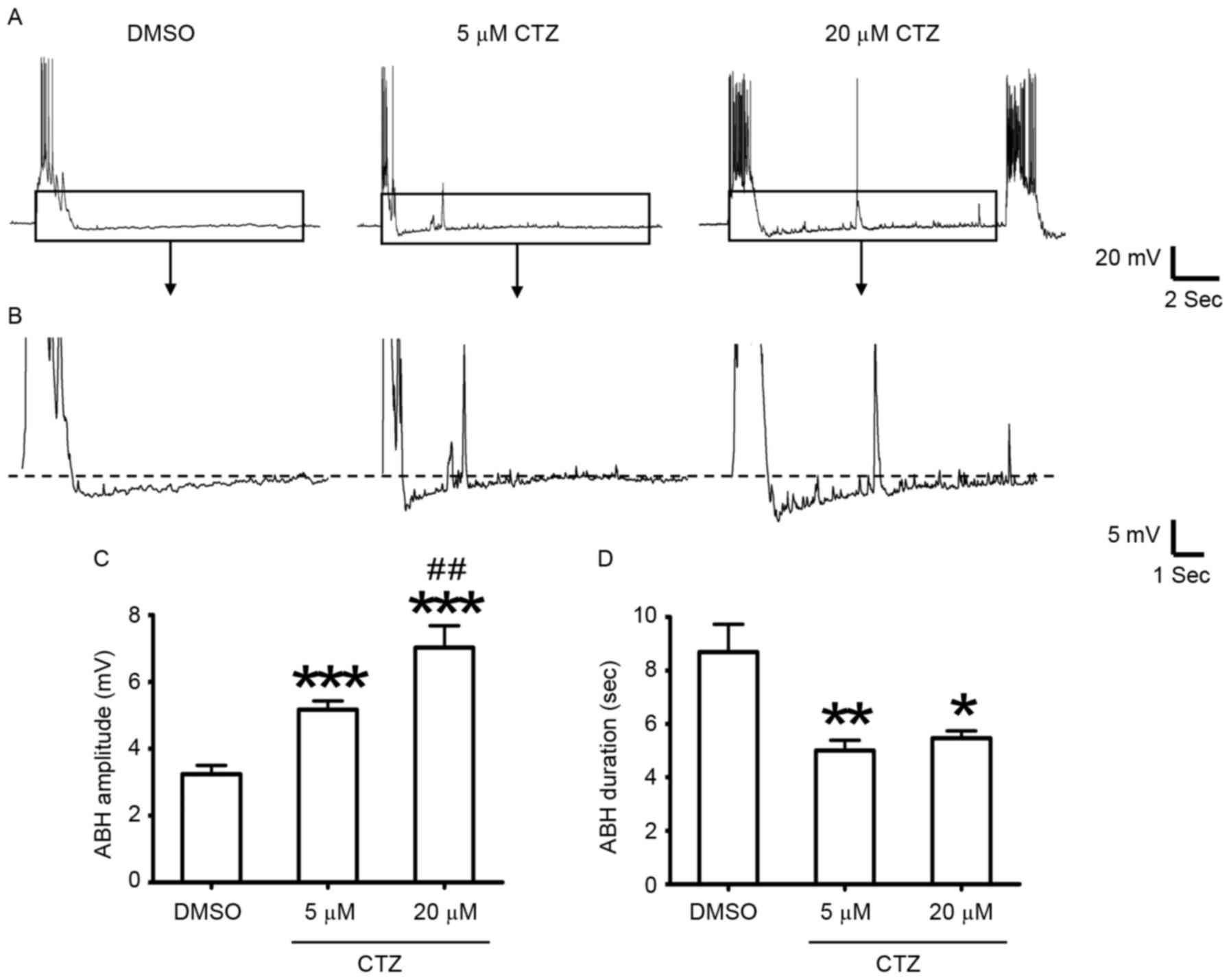
t-test was used for comparisons between 2 groups. In Figs. 1C and D, and 2C-E, an unpaired Student's t-test was
also performed for the comparisons group-by-group. A χ2
test was used for statistical analysis of percentage changes.
Linear regression was also tested using GraphPad software in linear
correlation analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
Epileptiform burst activities are
followed by a slow after hyperpolarization in cultured hippocampal
neurons
To investigate the underlying cellular mechanisms of
postictal depression, cultured hippocampal neurons were used as the
model. A relatively silent period was observed following burst
activity. Each period of burst activity, whether it was spontaneous
or CTZ-induced, was followed by a hyperpolarized potential
(Fig. 1A and B). ABH activity was
analyzed in the neurons that exhibited burst activity following
every period burst activity. The results revealed that the
amplitude of ABH significantly increased in the 5 µM CTZ treatment
group (5.17±0.26 mV; n=35 ABH activities from 10 neurons;
P<0.001; Fig. 1C) and in the 20
µM CTZ treatment group (7.03±0.65 mV; n=30 ABH activities from 10
neurons; P<0.001; Fig. 1C),
when compared with DMSO group (3.24±0.26 mV; n=47 ABH activities
from 11 neurons; Fig. 1C). The
high concentration group (20 µM CTZ) also had a significantly
greater amplitude when compared with the low concentration (5 µM)
CTZ group (P<0.01; Fig. 1C).
However, the ABH duration (length of the ABH period) significantly
decreased in the CTZ treatment groups (5 µM CTZ: 5.00±0.39 sec;
n=35 ABH activities; P<0.01; 20 µM CTZ: 5.47±0.27 sec; n=30 ABH
activities; P<0.05) when compared with the DMSO group (8.69±1.04
sec; n=47 ABH activities; Fig.
1D).
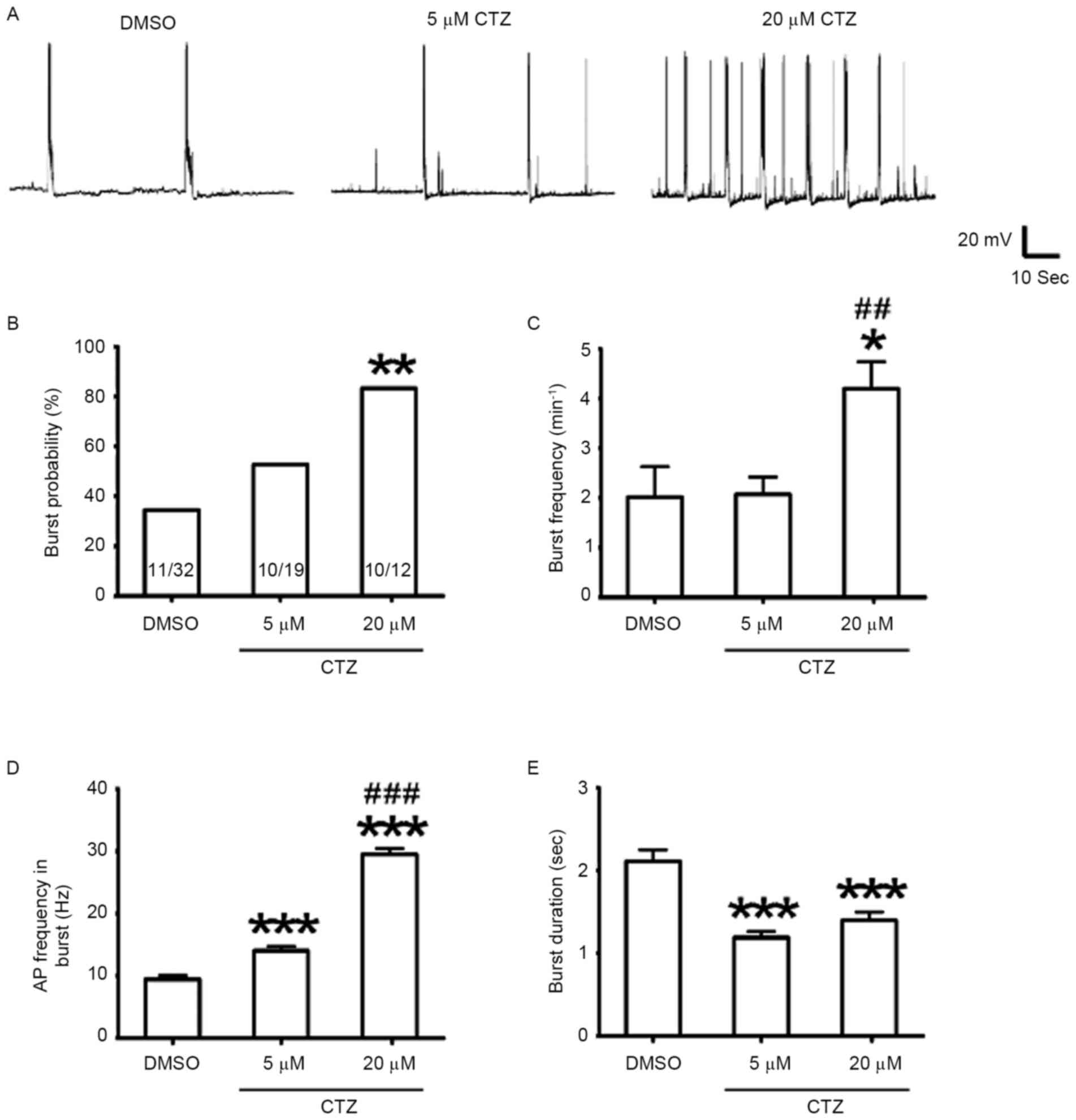
CTZ also induced stronger epileptiform burst
activities in cultured neurons. The percentage of neurons
exhibiting burst activities was compared with the burst frequency
(the average number of burst per minute), in neurons with and
without CTZ (Fig. 2A). Treatment
with a low concentration (5 µM) of CTZ did not significantly affect
the percentage of bursting neurons (5 µM CTZ: 52.6%, n=19 neurons;
DMSO: 34.4%, n=32 neurons; P>0.05; Fig. 2B), nor did it have an effect on the
bursting frequency (5 µM CTZ: 2.07±0.35/min, n=10 bursting neurons;
DMSO: 2.02±0.61/min, n=11 bursting neurons; Fig. 2C). However, a high concentration
(20 µM) of CTZ significantly increased the percentage of bursting
neurons to 83.3% (n=12 neurons; P<0.01; Fig. 2B) as well as the burst frequency
(4.20±0.54/min; n=10 bursting neurons; P<0.05; Fig. 2C). The burst frequency between the
two different CTZ concentrations was also significantly different
(P<0.01). These results indicated that CTZ induced burst
activity and increased the bursting frequency.
Subsequently, the changes in single burst activity
were observed. The average burst duration was compared with the
average AP frequency within each burst in all groups, to indicate
the dynamics of burst strength. When compared with the control
(DMSO: 9.45±0.63 Hz, n=47 bursting activities), the low and high
CTZ concentration treatments significantly increased the AP
frequency (5 µM CTZ: 14.04±0.68 Hz, n=35 bursting activities; 20 µM
CTZ: 29.49±0.96 Hz, n=30 bursting activities; both P<0.001;
Fig. 2D). The two CTZ groups were
also significantly different from one another (P<0.001; Fig. 2D). These results indicate that CTZ
may increase burst strength in a dose-dependent manner; however, as
only two different concentrations were evaluated in the present
study further investigation is required. In addition, the average
burst duration of the two CTZ groups were significantly reduced
when compared with the control (DMSO: 2.11±0.14 sec, n=47 bursting
activities; 5 µM CTZ: 1.19±0.07 sec, n=35 bursting activities; 20
µM CTZ: 1.40±0.10 sec, n=30 bursting activities; both P<0.001;
Fig. 2E).
APM-sensitive SK channels are involved
in the formation of ABH
The intracellular mechanism underlying the ABH was
also investigated. A large influx of calcium is known to occur in
neurons during burst activity (11); therefore, it was hypothesized that
calcium-activated potassium channels may be involved in the
regulation of ABH. Previous studies have demonstrated that SK
channels have a greater association with slow and long-lasting
hyperpolarization activities than BK channels (13,36).
Therefore, SK channels may have an important role in ABH. BK and SK
channels were pharmacologically investigated using their respective
antagonists.
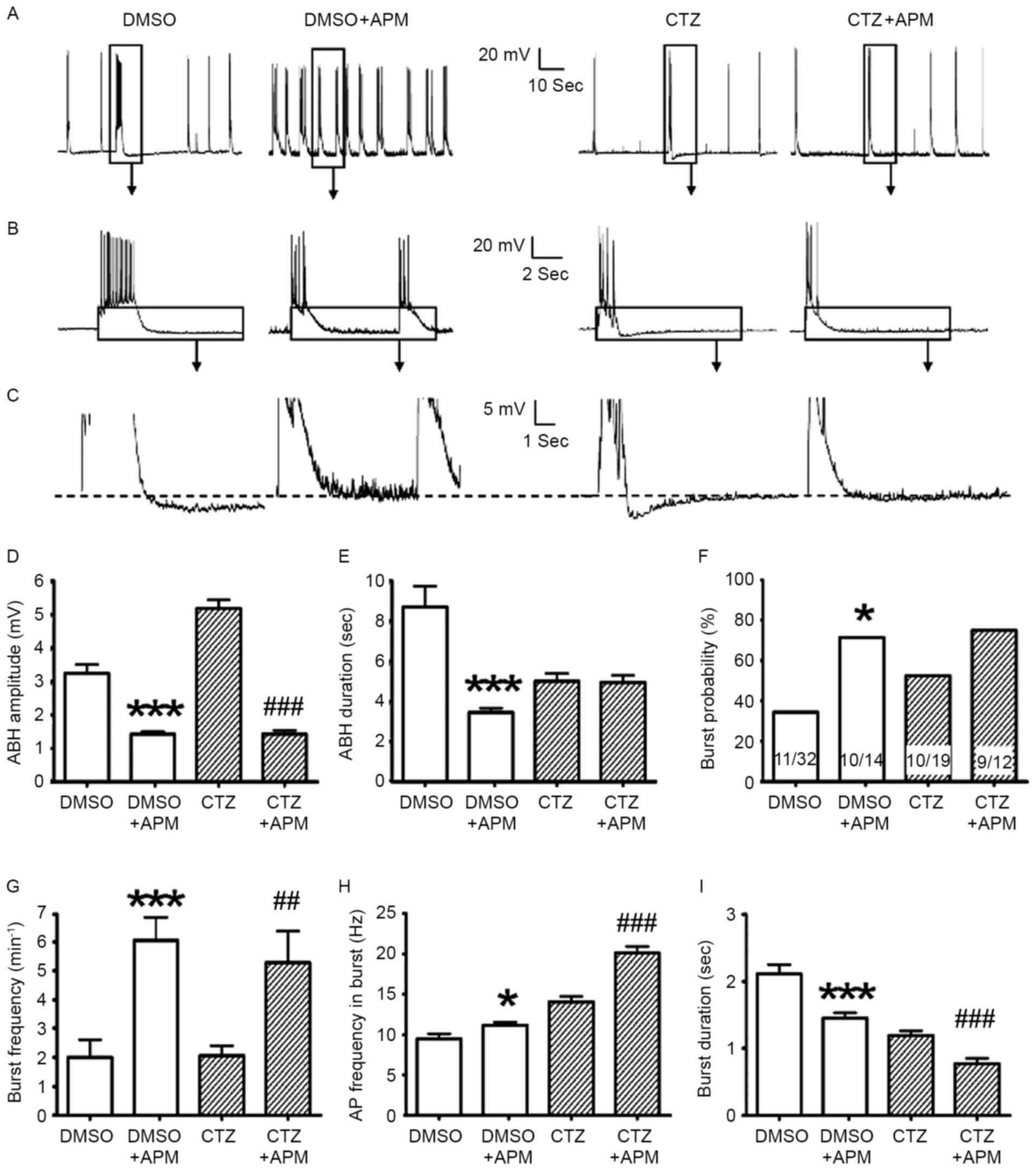
To determine whether SK channels regulate ABH and
burst activities, the SK channel-sensitive antagonist APM was used
to treat the cells cultured with and without 5 µM CTZ pretreatment.
SK channel inhibition with 500 nM APM induced a significant
reduction in the amplitude of ABH, in the CTZ pretreatment
(1.43±0.11 mV; n=61; P<0.001 vs. 5 µM CTZ; Fig. 3A-D) and the DMSO control (1.43±0.08
mV; n=64; P<0.001 vs. DMSO; Fig.
3A-D) groups. However, APM did not affect the duration of ABH
in the presence of CTZ (4.93±0.36 sec; n=61; P>0.05; Fig. 3E), although it did reduce the
duration in the DMSO control group (3.44±0.22 sec; n=64;
P<0.001; Fig. 3E). These
findings indicate that SK channels may mediate the majority of ABH
activities. The inhibition of SK channels reduced the amplitude of
ABH by ~50–70%. The APM insensitive potentials suggest there may be
additional receptors and ion channels involved.
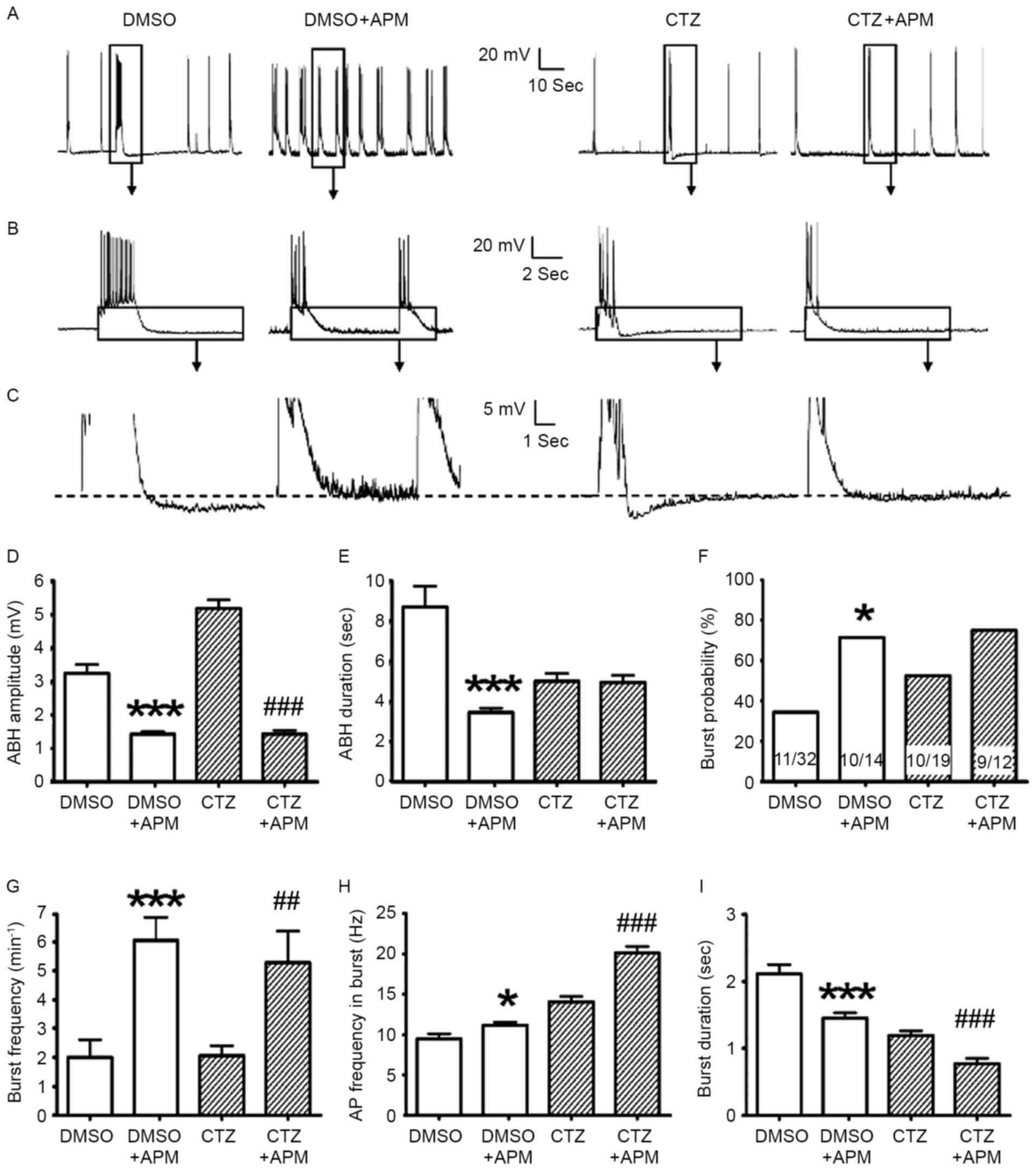 | Figure 3.APM impaired ABH; however, it also
enhanced burst activities. (A-C) Comparisons between the original
recording traces with and without 500 nM APM in the control and 5
µM CTZ group for 2 h. The boxes indicate the area that has been
enlarged in the subsequent images. (D) APM significantly suppressed
the amplitude of ABH in the control group (n=47 without APM; n=64
with APM) and the CTZ group (n=35 without APM; n=61 with APM). (E)
APM reduced the duration of ABH in the control group; however, this
was not observed in the CTZ group. (F) APM increased the percentage
of neurons exhibiting burst activities in the control group;
however, not in the CTZ group. The numbers written in the bars
represent the number of cells (number with burst activities/total
number). (G) APM significantly increased the burst number per
minute, in the control group (n=11 without APM; n=10 with APM) and
the CTZ group (n=10 without APM; n=9 with APM). (H) AP frequency in
burst increased with the application of APM, in the control and CTZ
groups. (I) Burst duration significantly decreased in the control
and CTZ groups when the bath solution contained APM. Data in D, E,
H and I represent the number of burst activities, whereas that in
(G) represent the number of neurons. Data are presented as the mean
± standard error mean. *P<0.05, ***P<0.001 DMSO vs. DMSO +
APM; ##P<0.01, ###P<0.001 CTZ vs. CTZ +
APM. APM, apamin; ABH, after burst hyperpolarization; CTZ,
cyclothiazide; AP, action potential. |
Given the inhibitory effect of APM on ABH, the
present study investigated the influence of this effect on burst
activity itself. Although it is thought that SK channels are able
to mediate the amplitude of ABH, the effect of SK channels on burst
activities remains to be elucidated. In this series of experiments,
a 5 µM dose of CTZ was selected to treat cultured neurons. The
effects of APM/IBTX were assessed through the comparison of
DMSO/DMSO + APM/DMSO + IBTX and the similar comparison of CTZ/CTZ +
APM/CTZ + IBTX. Following CTZ (5 µM) treatment, whole cell
recordings were performed in bath solution containing 500 nM APM to
block SK channels. Once the SK channels were blocked, the
percentage of neurons exhibiting burst activities increased in the
control and CTZ groups (from 34.4 to 71.4% in control and 52.6 to
75.0% in CTZ), however, only the control group presented
significant differences (P<0.05 in χ2 test; Fig. 3F). Burst frequency and burst
strength also significantly increased following blocking of the SK
channels with APM. Burst frequency increased from 2.02±0.61 to
6.08±0.81/min in the control groups (P<0.001) and from 2.07±0.35
to 5.31±1.10/min in the CTZ groups (P<0.01; Fig. 3G). The frequency of APs in burst
also increased from 9.45±0.63 to 11.14±0.40 Hz in control
(P<0.05) and from 14.04±0.68 to 20.12±0.79 Hz in CTZ group
(P<0.001; Fig. 3H). However,
the burst duration significantly decreased in the control and CTZ
groups (both P<0.001; Fig. 3I),
which was similar to the results observed following the initial
application of CTZ (Fig. 2E). The
results suggest that APM may enhance intrinsic excitability by
increasing the burst number per minute and also burst strength.
In contrast to APM, the BK channel antagonist IBTX
did not alter the majority of the parameters in ABH and burst
activities. In the DMSO control and 5 µM CTZ treated groups, the
ABH amplitude, ABH duration, burst probability and percentage,
burst frequency and burst inner AP frequency all had no
statistically significant differences, when comparing those with
and without IBTX, respectively (Fig.
4A-H). The burst duration was the only parameter that was
significantly different. In the presence of IBTX, the duration
increased from 2.11±0.14 sec (n=47) to 2.55±0.12 sec (n=22) in the
control group (P<0.05) and from 1.19±0.07 sec (n=35) to
2.02±0.20 sec (n=23) in the CTZ group (P<0.001; Fig. 4I). A previous study has reported
similar results (37). However,
the results of the present study revealed that blockage of the SK
channels is the principal induction of this excitatory effect.
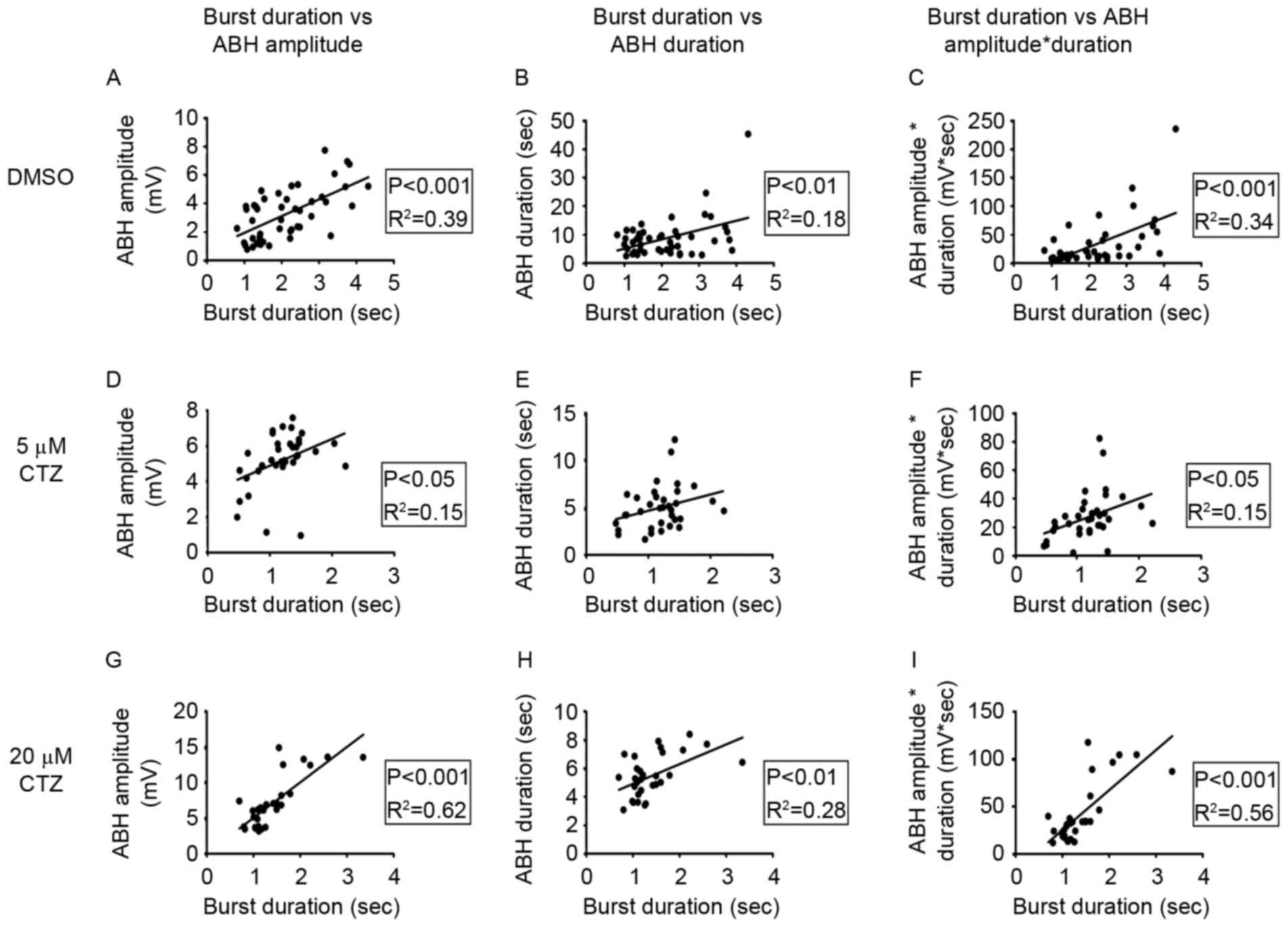
Correlations between epileptiform
bursts and ABH
Further analysis highlighted the associations
between burst and ABH. The present study compared the associations
between burst duration (the time a burst continued) and the
remaining three parameters: ABH amplitude, ABH duration and the
product of ABH amplitude and duration (Fig. 5). The last parameter was used to
represent the total hyperpolarizing charges in ABH activity,
although the unit is mV*s, not the unit of electric charge,
coulomb. The patch clamp recording mode used was ‘current clamp’,
which injects current to hold the membrane potential at −70 mV.
Therefore, the original data collected are the membrane potential
values. However, it is difficult to accurately calculate the
electrical charge value as the accurate calculation of neuronal
electrical charge requires a measurement of cellular membrane
conductance of each recorded neuron. As this membrane conductance
is highly dispersed and fluctuated in different neurons, so
actually the assessment parameter mV*s is only a carefully selected
approximation to the electrical charge value of neurons.
The results suggest that there may be a correlation
between ABH duration and burst duration. Despite the different
concentrations of CTZ treatment (Figs.
1D and 2E), or APM blockage
(Fig. 3E and I), ABH duration
exhibited similar changes to those of burst duration. Therefore, it
was hypothesized that there may be a positive correlation between
single cell activities. The experimental results revealed a
significant positive correlation between burst duration and ABH
amplitude (R2=0.39; P<0.001; Fig. 5A), ABH duration
(R2=0.18; P<0.01; Fig.
5B), and the product of ABH amplitude and duration
(R2=0.34; P<0.001; Fig.
5C) in the DMSO group. The 5 µM CTZ-treated group also
exhibited a significant positive correlation in the majority of the
parameters; however, the differences were not as significant as
those exhibited by the DMSO group. The correlation between burst
duration and ABH amplitude (R2=0.15; P<0.05; Fig. 5D), and burst duration and the
product (R2=0.15; P<0.05 Fig. 5F) were significant; however, there
was no significant association between burst duration and ABH
duration (R2=0.09; P=0.08; Fig. 5E). In the 20 µM CTZ group, all
three parameters were significant (burst duration vs. ABH
amplitude: R2=0.62; P<0.001; Fig. 5G; burst duration vs. ABH duration:
R2=0.28; P<0.01; Fig.
5H; burst duration vs. the product: R2=0.56;
P<0.001; Fig. 5I). These
results indicate that there is normal physiological feedback
between ABH activities and burst activities, as after a long burst
a large period of ABH follows in order to terminate the burst and
prevent any new burst activity.
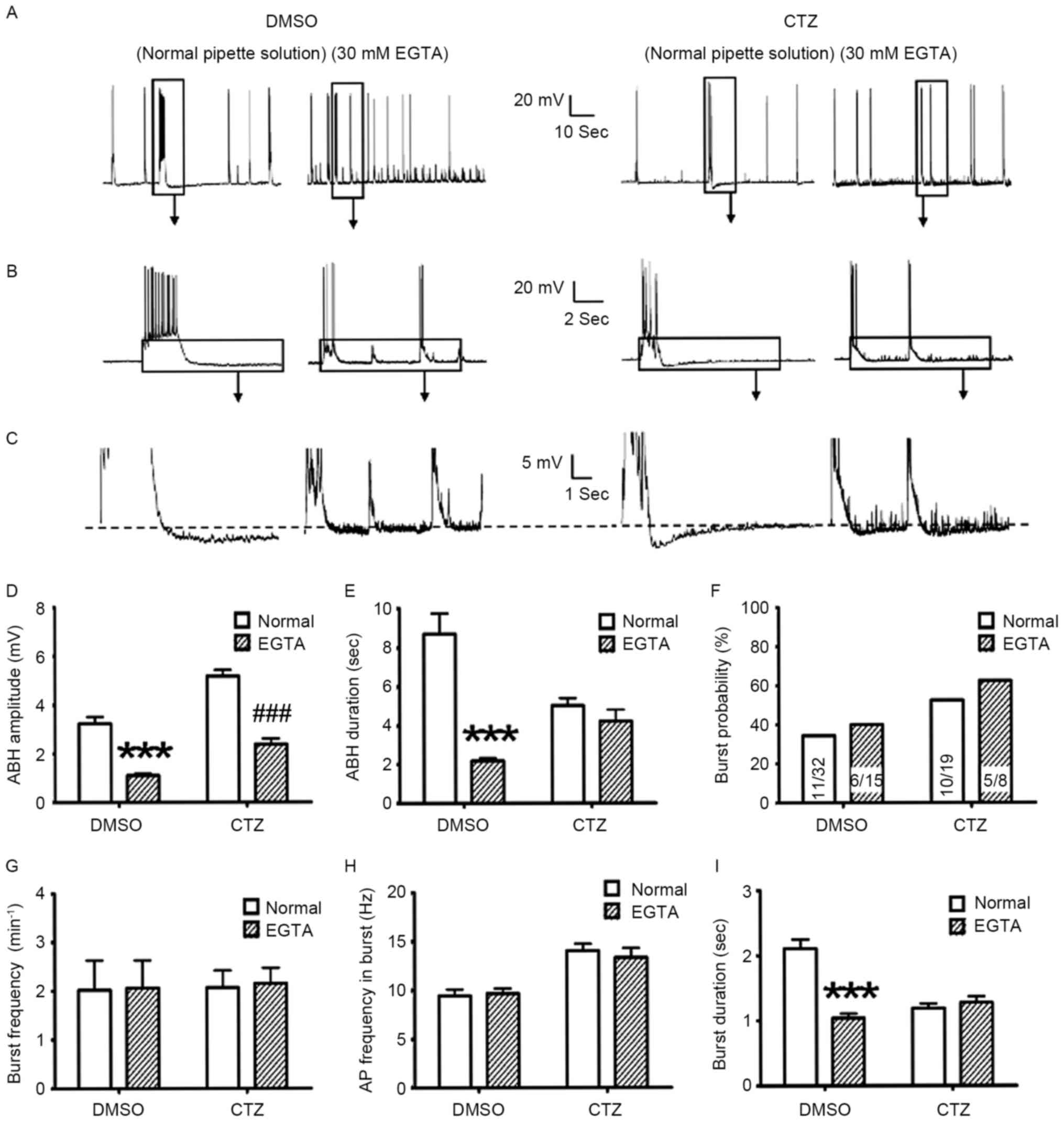
EGTA-induced reduction of
intracellular calcium concentration reduces ABH; however, it does
not affect burst activities
To determine the mechanisms underlying neuronal
regulation in ABH and burst, the present study investigated
intracellular calcium. Intracellular calcium is involved in the ABH
process and burst activities. The [Ca2+]i concentration
is associated with the strength of AP and burst and with the
activation of BK and SK channels (38–41).
EGTA, a calcium selective chelator, was added to the pipette
solution to reduce the intracellular calcium concentration. The ABH
and bursts with and without 30 mM EGTA, in the DMSO control and 5
µM CTZ pretreatment groups were subsequently compared. The results
demonstrated that there was a significant reduction in ABH
amplitude in the control (from 3.24±0.26 to 1.10±0.08 mV;
P<0.001) and CTZ treatment groups (from 5.17±0.26 to 2.39±0.22
mV; P<0.001; Fig. 6A-D).
However, burst duration was affected differently. The application
of 30 mM EGTA decreased the burst duration in the DMSO control
(Normal: 8.69±1.04 sec, n=47; 30 mM EGTA: 2.17±0.15 sec, n=35;
P<0.001); however, no decrease was observed in the CTZ group
(Normal: 5.00±0.39 sec, n=35; 30 mM EGTA: 4.19±0.60 sec, n=22;
Fig. 6E). In parallel to the
reduction of ABH, 30 mM EGTA did not alter the majority of the
burst activity parameters, including burst neuron percentage
(Fig. 6F), burst frequency
(Fig. 6G) and the burst inner AP
frequency (Fig. 6H). The only
significant difference identified was in the burst duration of the
control group (from 2.11±0.14 to 1.04±0.07 sec; P<0.001;
Fig. 6I).
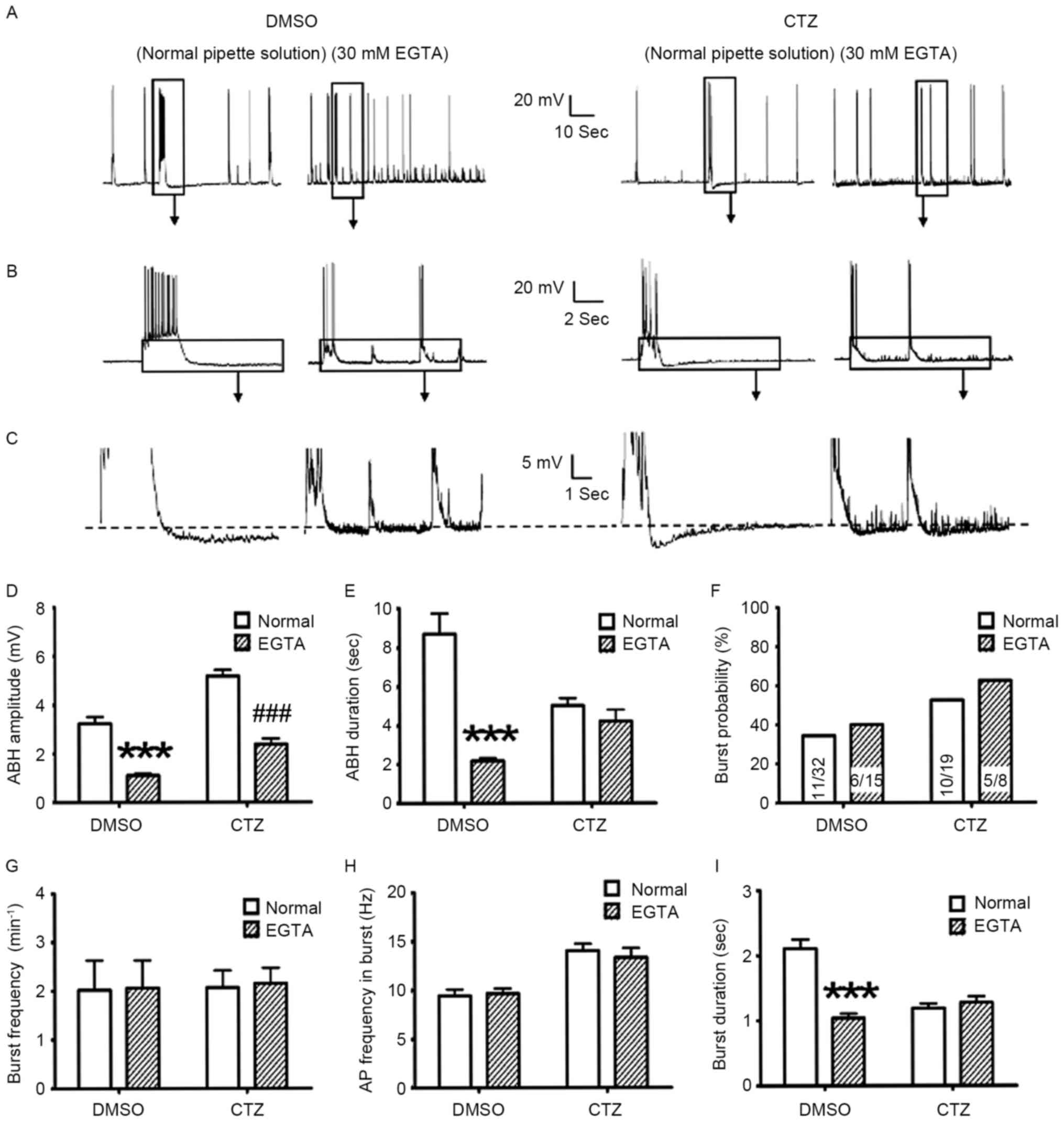 | Figure 6.High EGTA pipette solution reduced
the ABH; however, it did not alter the burst probability and
strength. (A-C) Representative original recording traces of neurons
treated with normal and 30 mM EGTA pipette solution in the DMSO
control and 5 µM CTZ groups. The boxes indicate the area that has
been enlarged in the subsequent images. (D) High EGTA significantly
reduced the amplitude of ABH in the control (normal: n=47 bursts in
11 neurons; 30 mM EGTA: n=35 bursts in 6 neurons) and CTZ groups
(normal: n=35 bursts in 10 neurons; 30 mM EGTA: n=22 bursts in 5
neurons). (E) High EGTA only reduced ABH duration in the control
group, not in the CTZ group. There were no significant differences
identified between two types of pipette solution, in control and
CTZ groups for (F) bursting neuron percentage [the numbers written
in the bars represent the number of cells (number with burst
activities/total number)], (G) bursting number per minute and (H)
AP frequency in burst. (I) High EGTA significantly decreased the
burst duration in the control group; however, not in the CTZ group.
Data are presented as the mean ± standard error mean. ***P<0.001
DMSO/normal vs. DMSO/EGTA; ###P<0.001 CTZ/normal vs.
CTZ/EGTA. EGTA, ethylene glycol-bis(b-aminoethyl
ether)-N,N,N',N'-tetraacetic acid; ABH, after burst
hyperpolarization; CTZ, cyclothiazide; AP, action potential. |
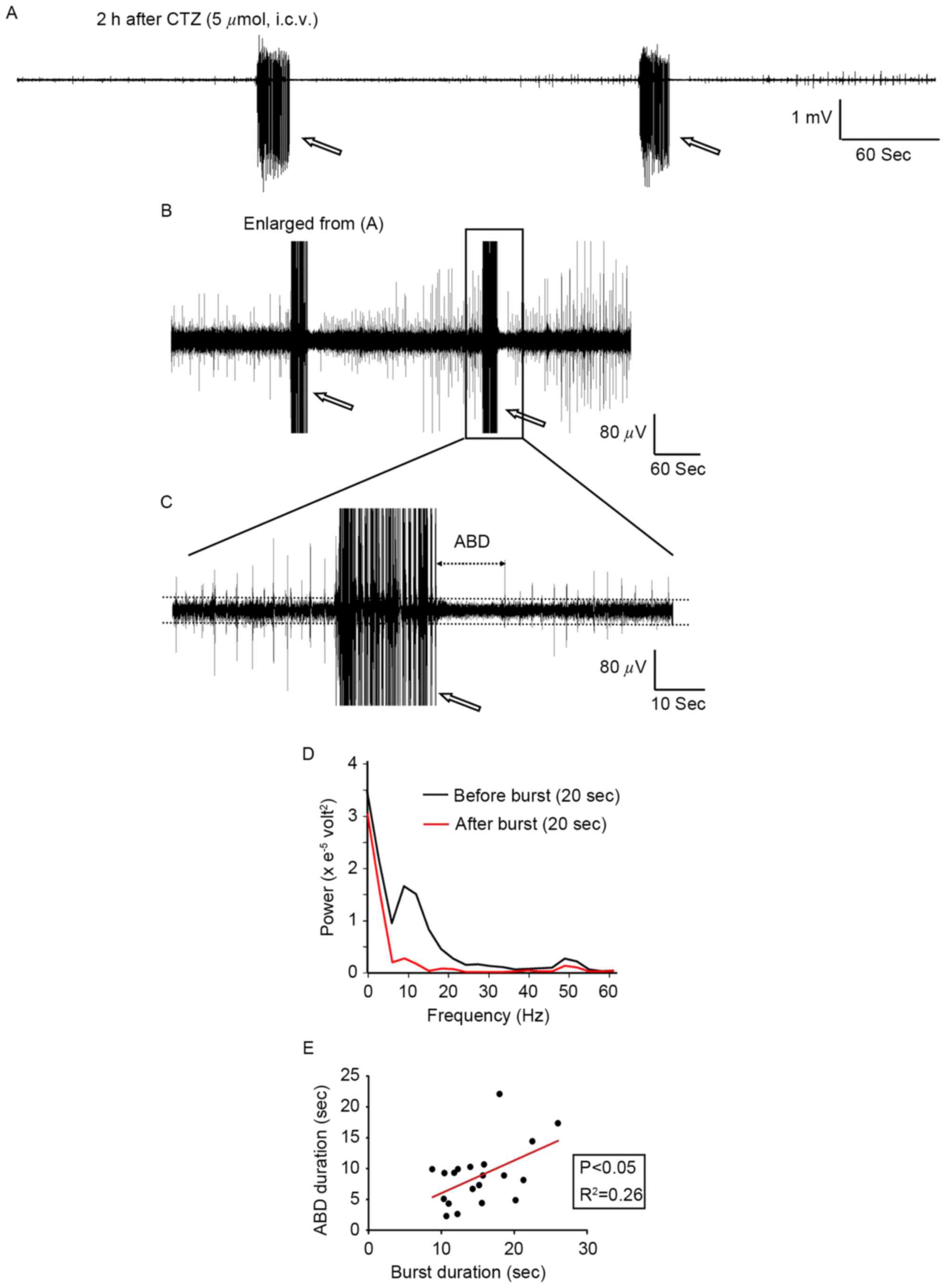
Epileptiform burst activities are
followed by a long-lasting ABD in the hippocampal neurons of
anaesthetized rats
CTZ has been previously reported to generate
epileptiform burst activities in hippocampal neurons in
vitro and in vivo (24,30)
and it also induced seizure behavior in rats (29). The present study investigated
whether the results from the cultured neurons also occurred in the
rat model. CTZ (5 µmol; 5 µl; intracerebroventricular injection)
induced epileptiform burst activities in all 6 rats tested, which
is in agreement with previous reports (24,30).
During the 3 h intracranial EEG recording, CTZ induced a total of
20 bursts in all 6 rats, with a mean burst duration of 15.26±1.04
sec (range, 10.37 to 26.04 sec; Fig.
7A). Immediately following burst activities, there was a long
period of depression, or ABD, which lasted for 8.80±1.08 sec on
average (range, 2.59 to 22.06 sec; n=20 bursts in 6 rats; Fig. 7B and C). A decrease in
electroencephalographic power occurred following burst activity.
Prior to burst activity, the power was recorded between 5–20 Hz in
20 sec, which was larger than that observed following burst
activities (Fig. 7D). Further
analysis revealed a significant positive correlation between burst
duration and ABD duration in all bursts tested (Fig. 7E), which is similar to the
correlation identified in cultured neurons. The goodness of fit in
the two groups has a R2 value of 0.26 and P=0.022. These
results indicate that the strength of the ABD may be directly
associated with the strength of the epileptiform burst activities
in seizure.
Discussion
The results of the present study are schematically
represented in Fig. 8. Burst
activities elevate the concentration of intracellular calcium,
which can conversely enhance the strength of burst. In addition,
the elevated calcium concentration activates the SK channels to
enhance the amplitude of ABH. This enhanced hyperpolarization
activity can inhibit or reduce burst activity. In the present
study, when CTZ was applied a number of excitatory processes were
activated, inducing burst activities. Bursts increased the calcium
influx, enhanced the intracellular calcium concentration and
produced a greater ABH. When APM was applied, the SK channels were
blocked and thus ABH was impaired. As a result, the neurons had
more excitatory activities and generated stronger bursts. However,
when IBTX was applied and the BK channels were blocked, no
significant differences were identified in the different
parameters. Therefore, the blockage of the SK channels was
identified as the principal induction of this excitatory effect.
EGTA (30 mM) reduced intracellular calcium concentration, and
impaired ABH and burst activities. However, the reduction in ABH
may have elevated burst activities. Thus, the effects of ABH and
intracellular calcium may offset each other. The majority of the
burst activity parameters were not altered (Fig. 8). In our experimental results, the
relationship between BK channel and bursting activities were not
identified. Thus, IBTX and BK channels were excluded from Fig. 8.
 | Figure 8.A schematic representation of the
associations identified among burst activities, ABH and
intracellular calcium concentration in the present study. The
schematic summarizes and analyzes the results from all of the
experiments performed in the present study. The three different
conditions, CTZ, APM and EGTA, are listed separately within the
schematic. ABH, after burst hyperpolarization; CTZ, cyclothiazide;
APM, apamin; EGTA, ethylene glycol-bis (β-aminoethyl
ether)-N,N,N',N'-tetraacetic acid; SK, small conductance
calcium-activated potassium channels. |
In the present study, cultured hippocampal neurons
treated with DMSO or without any treatment also exhibited
spontaneous burst activities (DMSO: 34.4%, n=32; Fig. 2B; No treatment: 38.6%, n=44; data
not shown). This is likely due to the environment changing from
culture media to the recording bath solution, which may have
stimulated the cultured neurons. However, the experimental protocol
included measures to counter this limitation to a certain degree,
such as heating the bath solution to ~37°C prior to recording.
The results of the present study appear to be
paradoxical as when the ABH duration and burst duration are
reduced, ABH amplitude and burst strength are increased; a
phenomenon that is difficult to account for. Cellular regulation
may exist in order to reduce the ion influx when the activity
strength is enhanced in ABH and burst. One possible explanation is
that enhanced ABH and burst may alter the membrane potential faster
than in the control, thereby shortening the duration. The currents
increase in burst and ABH, producing faster depolarization and
hyperpolarization, shortening the duration.
SK channels are Ca2+−activated
K+ channels with small conductance (10–20 pS) and are
widely expressed in vertebrate neurons and other tissues (42). SK channel-mediated hyperpolarized
K+ currents have an important role in regulating
neuronal excitability in physiological (43) and pathological conditions (18,23).
In the present study, the cultured neurons exhibited a depression
in ABH amplitude when treated with APM. This suggested that AHP may
be mediated by SK channels as APM can block the majority of SK
channel activation. This finding has also been observed in
different epilepsy models (22,23).
For example, Fernández de Sevilla et al (23) found that in 4-aminopyridine (4-AP)
epilepsy model and in Mg(2+)-free induced model, slow
AHP (sAHP) was also inhibited, particularly in hippocampal CA3
pyramidal neurons. 1-Ethyl-2-benzimidazolinone (1-EBIO), a
modulator of SK channels, can slow the deactivation of SK channels
and prolong their opening time (44). It has been previously demonstrated
that 1-EBIO may potentially inhibit burst activity in vitro
(21) and in vivo (45). The results of the present study
demonstrated this same effect in the opposite manner. The previous
study activated SK channels by agonist, and then assessed the
excitability, positively regulated the function of SK channels,
whereas the present study inhibited SK channels by antagonist
apamin, and then assessed the bursting activities through a
negative regulation.
Small conductance calcium-activated potassium
channels are the most important factor in the generation of ABH.
The elevation in ABH amplitude is dependent on the increase in
intracellular calcium concentration; stronger burst activity
requires more calcium ions, thereby inducing a larger ABH.
Although the association between burst strength and
ABH is relatively well-established, there are different hypotheses
to explain the underlying mechanisms. One such hypothesis is that
burst activities may activate some intracellular protein kinases
(25) such as protein kinase A
(PKA), which can regulate the kinetics of SK channels. A previous
study has demonstrated that SK channel activity is regulated by PKA
(46). Therefore, the future
studies will focus on intracellular protein kinases, in order to
elucidate which protein kinase regulates the dynamics of SK channel
function during the process of epileptic seizure.
In the present study, the correlation between the
strength of burst and ABH is, to the best of our knowledge, a
relatively new discovery in the field, but not a totally novel
finding. These positive correlations reveal that ABH may aid
neurons to reduce the damage of hyperexcitation during bursts. This
process is potentially mediated by SK channels. However, in the
control and CTZ groups, there was still a part of hyperpolarization
(~1.4 mV) that was insensitive to APM. These APM insensitive
potentials indicate that other receptors and ion channels may
participate, such as cyclic nucleotide-gated nonspecific cation
channels. Previous studies (15,36)
have suggested that SK channels may only contribute to those ABHs
with the duration of ~100 msec and not to those slow ABHs with the
duration of several sec. Based on these new experimental results,
it is possible that SK channels contribute, at least in part, to
second-level slow ABHs. Thus, mice with complete knockout of all SK
channels may still have second-level slow ABHs. In addition, SK
channels as intrinsic auto-balancers, may have an important role in
suppressing burst activity. Collectively, these findings suggest
that SK channels may be potential targets for designing novel
antiepileptic drugs.
The results in this animal model provide novel in
vivo evidence. However, the in vivo postictal ABD in EEG
and the in vitro ABH in a single neuron are clearly distinct
phenomena. One is neuronal activity and the other is the activity
of the brain region. Although they hold similar characteristics, a
straightforward association between them cannot be identified. The
EEG represents the population activities of neurons in a brain
region, whereas the neuronal population activities are based on the
activity of a single neuron. Thus, the recordings from the EEG and
patch clamp were compared to determine the similarities and
differences between them. This comparison may reveal the
characteristics of ABD and ABH; however, this may be insufficient
or incomplete. In addition, the present study, and those performed
previously, lack sufficient in vivo evidence to suggest that
blocking SK channels enhances burst activity. The in vivo
evidence represents the results from model animals and also those
from human patients (47,48). For example, Beck et al
(47) investigated 34 dentate
gyrus granule cells from 11 patients with temporal lobe epilepsy
and found that APM (50 nM) was only able to inhibit ~13%
Ca(2+)-dependent K+ currents. However, it
remains to be elucidated, with further patient-based studies that
investigate the dynamics of SK channels in epileptic seizures.
In conclusion, although there were a number of
limitations in the present study, one being that APM could only be
administered in in vitro experiments, it is evident that APM
may be able to suppress ABH to enhance the excitability of the
neuronal network in cultured neurons. However, the effect of APM on
ABD in anesthetic animal models remains to be elucidated. Future
studies will determine the effect of APM on the duration of ABD and
elucidate any changes in the CTZ epilepsy animal model.
Acknowledgements
The present study was supported by grants from the
Nature Science Foundation of China (grant nos. 81171224, 31471027
and 31771188) and the Science and Technology Commission of Shanghai
Municipality (grant nos. 13DJ1400302) to Professor Yun Wang. The
authors would like to acknowledge the technical support provided by
Dr Zheng Wu (Fudan University) for whole cell patch clamp
recording.
References
|
1
|
Browne TR and Holmes GL: Epilepsy. N Engl
J Med. 344:1145–1151. 2001. View Article : Google Scholar
|
|
2
|
Lado FA and Moshé SL: How do seizures
stop? Epilepsia. 49:1651–1664. 2008. View Article : Google Scholar :
|
|
3
|
Ziemann AE, Schnizler MK, Albert GW,
Severson MA, Howard MA III, Welsh MJ and Wemmie JA: Seizure
termination by acidosis depends on ASIC1a. Nat Neurosci.
11:816–822. 2008. View
Article : Google Scholar :
|
|
4
|
Van Gompel JJ, Bower MR, Worrell GA, Stead
M, Chang SY, Goerss SJ, Kim I, Bennet KE, Meyer FB, Marsh WR, et
al: Increased cortical extracellular adenosine correlates with
seizure termination. Epilepsia. 55:233–244. 2014. View Article : Google Scholar :
|
|
5
|
Afra P, Jouny CC and Bergey GK:
Termination patterns of complex partial seizures: An intracranial
EEG study. Seizure. 32:9–15. 2015. View Article : Google Scholar :
|
|
6
|
Ferastraoaru V, Schulze-Bonhage A, Lipton
RB, Dümpelmann M, Legatt AD, Blumberg J and Haut SR: Termination of
seizure clusters is related to the duration of focal seizures.
Epilepsia. 57:889–895. 2016. View Article : Google Scholar
|
|
7
|
Mula M and Sander JW: Negative effects of
antiepileptic drugs on mood in patients with epilepsy. Drug Saf.
30:555–567. 2007. View Article : Google Scholar
|
|
8
|
Spencer SS and Spencer DD: Implications of
seizure termination location in temporal lobe epilepsy. Epilepsia.
37:455–458. 1996. View Article : Google Scholar
|
|
9
|
Bragin A, Penttonen M and Buzsáki G:
Termination of epileptic afterdischarge in the hippocampus. J
Neurosci. 17:2567–2579. 1997.
|
|
10
|
Alger BE and Nicoll RA: Epileptiform burst
afterhyperpolarization: Calcium-dependent potassium potential in
hippocampal CA1 pyramidal cells. Science. 210:1122–1124. 1980.
View Article : Google Scholar
|
|
11
|
Albowitz B, König P and Kuhnt U:
Spatiotemporal distribution of intracellular calcium transients
during epileptiform activity in guinea pig hippocampal slices. J
Neurophysiol. 77:491–501. 1997.
|
|
12
|
Vergara C, Latorre R, Marrion NV and
Adelman JP: Calcium-activated potassium channels. Curr Opin
Neurobiol. 8:321–329. 1998. View Article : Google Scholar
|
|
13
|
Zhang L and McBain CJ: Potassium
conductances underlying repolarization and after-hyperpolarization
in rat CA1 hippocampal interneurones. J Physiol. 488:661–672. 1995.
View Article : Google Scholar :
|
|
14
|
Xia XM, Fakler B, Rivard A, Wayman G,
Johnson-Pais T, Keen JE, Ishii T, Hirschberg B, Bond CT, Lutsenko
S, et al: Mechanism of calcium gating in small-conductance
calcium-activated potassium channels. Nature. 395:503–507. 1998.
View Article : Google Scholar
|
|
15
|
Faber ES and Sah P: Physiological role of
calcium-activated potassium currents in the rat lateral amygdala. J
Neurosci. 22:1618–1628. 2002.
|
|
16
|
Llinas R, Baker R and Sotelo C:
Electrotonic coupling between neurons in cat inferior olive. J
Neurophysiol. 37:560–571. 1974.
|
|
17
|
Auer RN: Progress review: Hypoglycemic
brain damage. Stroke. 17:699–708. 1986. View Article : Google Scholar
|
|
18
|
Oliveira MS, Skinner F, Arshadmansab MF,
Garcia I, Mello CF, Knaus HG, Ermolinsky BS, Otalora LF and
Garrido-Sanabria ER: Altered expression and function of
small-conductance (SK) Ca(2+)-activated K+ channels in
pilocarpine-treated epileptic rats. Brain Res. 1348:187–199. 2010.
View Article : Google Scholar :
|
|
19
|
Schulz R, Kirschstein T, Brehme H, Porath
K, Mikkat U and Köhling R: Network excitability in a model of
chronic temporal lobe epilepsy critically depends on SK
channel-mediated AHP currents. Neurobiol Dis. 45:337–347. 2012.
View Article : Google Scholar
|
|
20
|
Luján R, Maylie J and Adelman JP: New
sites of action for GIRK and SK channels. Nat Rev Neurosci.
10:475–480. 2009. View
Article : Google Scholar
|
|
21
|
Lappin SC, Dale TJ, Brown JT, Trezise DJ
and Davies CH: Activation of SK channels inhibits epileptiform
bursting in hippocampal CA3 neurons. Brain Res. 1065:37–46. 2005.
View Article : Google Scholar
|
|
22
|
Empson RM and Jefferys JG: Ca(2+) entry
through L-type Ca(2+) channels helps terminate epileptiform
activity by activation of a Ca(2+) dependent afterhyperpolarisation
in hippocampal CA3. Neuroscience. 102:297–306. 2001. View Article : Google Scholar
|
|
23
|
de Sevilla Fernández D, Garduño J, Galván
E and Buño W: Calcium-activated afterhyperpolarizations regulate
synchronization and timing of epileptiform bursts in hippocampal
CA3 pyramidal neurons. J Neurophysiol. 96:3028–3041. 2006.
View Article : Google Scholar
|
|
24
|
Qi J, Wang Y, Jiang M, Warren P and Chen
G: Cyclothiazide induces robust epileptiform activity in rat
hippocampal neurons both in vitro and in vivo. J Physiol.
571:605–618. 2006. View Article : Google Scholar :
|
|
25
|
Wang Y, Qi JS, Kong S, Sun Y, Fan J, Jiang
M and Chen G: BDNF-TrkB signaling pathway mediates the induction of
epileptiform activity induced by a convulsant drug cyclothiazide.
Neuropharmacology. 57:49–59. 2009. View Article : Google Scholar :
|
|
26
|
Deng L and Chen G: Cyclothiazide potently
inhibits gamma-aminobutyric acid type A receptors in addition to
enhancing glutamate responses. Proc Natl Acad Sci USA.
100:13025–13029. 2003. View Article : Google Scholar :
|
|
27
|
Kullmann DM and Semyanov A: Glutamatergic
modulation of GABAergic signaling among hippocampal interneurons:
Novel mechanisms regulating hippocampal excitability. Epilepsia. 43
Suppl 5:S174–S178. 2002. View Article : Google Scholar
|
|
28
|
Krishnan GP and Bazhenov M: Ionic dynamics
mediate spontaneous termination of seizures and postictal
depression state. J Neurosci. 31:8870–8882. 2011. View Article : Google Scholar :
|
|
29
|
Kong S, Qian B, Liu J, Fan M, Chen G and
Wang Y: Cyclothiazide induces seizure behavior in freely moving
rats. Brain Res. 1355:207–213. 2010. View Article : Google Scholar :
|
|
30
|
Qian B, Sun Y, Wu Z, Wan L, Chen L, Kong
S, Zhang B, Zhang F, Wang ZY and Wang Y: Epileptiform response of
CA1 neurones to convulsant stimulation by cyclothiazide, kainic
acid and pentylenetetrazol in anaesthetized rats. Seizure.
20:312–319. 2011. View Article : Google Scholar
|
|
31
|
Chen B, Jiang M, Zhou M, Chen L, Liu X,
Wang X and Wang Y: Both NMDA and non-NMDA receptors mediate
glutamate stimulation induced cofilin rod formation in cultured
hippocampal neurons. Brain Res. 1486:1–13. 2012. View Article : Google Scholar
|
|
32
|
Liu X, Chen B, Chen L, Ren WT, Liu J, Wang
G, Fan W, Wang X and Wang Y: U-shape suppressive effect of phenol
red on the epileptiform burst activity via activation of estrogen
receptors in primary hippocampal culture. PLoS One. 8:e601892013.
View Article : Google Scholar :
|
|
33
|
Chen L, Wan L, Wu Z, Ren W, Huang Y, Qian
B and Wang Y: KCC2 downregulation facilitates epileptic seizures.
Sci Rep. 7:1562017. View Article : Google Scholar :
|
|
34
|
Zhang Y, Huang Y, Liu X, Wang G, Wang X
and Wang Y: Estrogen suppresses epileptiform activity by enhancing
Kv4.2-mediated transient outward potassium currents in primary
hippocampal neurons. Int J Mol Med. 36:865–872. 2015. View Article : Google Scholar
|
|
35
|
Zhang Y, Huang Y, Wang G, Wang X and Wang
Y: Inhibition of 17-beta-estradiol on neuronal excitability via
enhancing GIRK1-mediated inwardly rectifying potassium currents and
GIRK1 expression. J Neurol Sci. 375:335–341. 2017. View Article : Google Scholar
|
|
36
|
Faber ESL and Sah P: Functions of SK
channels in central neurons. Clin Exp Pharmacol Physiol.
34:1077–1083. 2007. View Article : Google Scholar
|
|
37
|
Kleiman-Weiner M, Beenhakker MP, Segal WA
and Huguenard JR: Synergistic roles of GABAA receptors and SK
channels in regulating thalamocortical oscillations. J
Neurophysiol. 102:203–213. 2009. View Article : Google Scholar :
|
|
38
|
Schwartzkroin PA and Stafstrom CE: Effects
of EGTA on the calcium-activated afterhyperpolarization in
hippocampal CA3 pyramidal cells. Science. 210:1125–1126. 1980.
View Article : Google Scholar
|
|
39
|
Lancaster B and Adams PR:
Calcium-dependent current generating the afterhyperpolarization of
hippocampal neurons. J Neurophysiol. 55:1268–1282. 1986.
|
|
40
|
Abel HJ, Lee JC, Callaway JC and Foehring
RC: Relationships between intracellular calcium and
afterhyperpolarizations in neocortical pyramidal neurons. J
Neurophysiol. 91:324–335. 2004. View Article : Google Scholar
|
|
41
|
Scutt G, Allen M, Kemenes G and Yeoman M:
A switch in the mode of the sodium/calcium exchanger underlies an
age-related increase in the slow afterhyperpolarization. Neurobiol
Aging. 36:2838–2849. 2015. View Article : Google Scholar
|
|
42
|
Köhler M, Hirschberg B, Bond CT, Kinzie
JM, Marrion NV, Maylie J and Adelman JP: Small-conductance,
calcium-activated potassium channels from mammalian brain. Science.
273:1709–1714. 1996. View Article : Google Scholar
|
|
43
|
Stackman RW, Hammond RS, Linardatos E,
Gerlach A, Maylie J, Adelman JP and Tzounopoulos T: Small
conductance Ca2+-activated K+ channels modulate synaptic plasticity
and memory encoding. J Neurosci. 22:10163–10171. 2002.
|
|
44
|
Pedarzani P, Mosbacher J, Rivard A,
Cingolani LA, Oliver D, Stocker M, Adelman JP and Fakler B: Control
of electrical activity in central neurons by modulating the gating
of small conductance Ca2+-activated K+ channels. J Biol Chem.
276:9762–9769. 2001. View Article : Google Scholar
|
|
45
|
Anderson NJ, Slough S and Watson WP: In
vivo characterisation of the small-conductance KCa (SK) channel
activator 1-ethyl-2-benzimidazolinone (1-EBIO) as a potential
anticonvulsant. Eur J Pharmacol. 546:48–53. 2006. View Article : Google Scholar
|
|
46
|
Kernig K, Kirschstein T, Würdemann T,
Rohde M and Köhling R: The afterhyperpolarizing potential following
a train of action potentials is suppressed in an acute epilepsy
model in the rat Cornu Ammonis 1 area. Neuroscience. 201:288–296.
2012. View Article : Google Scholar
|
|
47
|
Beck H, Clusmann H, Kral T, Schramm J,
Heinemann U and Elger CE: Potassium currents in acutely isolated
human hippocampal dentate granule cells. J Physiol. 498:73–85.
1997. View Article : Google Scholar :
|
|
48
|
Garduño J, Galván E, de Sevilla Fernández
D and Buño W: 1-Ethyl-2-benzimidazolinone (EBIO) suppresses
epileptiform activity in in vitro hippocampus. Neuropharmacology.
49:376–388. 2005. View Article : Google Scholar
|