Introduction
Acute basophilic leukemia (ABL) is a rare
hematologic malignancy that is currently poorly described. The
clinical progression of ABL is rapid and associated with a poor
prognosis. Although ABL is currently recognized as a distinct
clinical entity in the classification of myeloid malignancies
(1), its rarity complicates the
diagnosis of the disease and the establishment of a treatment
protocol. In the present report, the case of an elderly male who
presented with ABL, as well as a gastric antral ulcer and
maculopapular rashes is described. This study was approved by the
Ethics Committee of the First Affiliated Hospital of Chongqing
Medical University and was performed according to the Declaration
of Helsinki. Written informed consent was obtained from the
patient’s family.
Case report
In November 2012, a 65-year-old male was admitted to
the First Affiliated Hospital of Chongqing Medical University
(Chongqing, China) with dizziness that had persisted for one month
and described the occurrence of melena for two weeks. The physical
examination was notable for pallor and rashes, and the patient had
developed erythematous and maculopapular skin lesions on the legs
and hands (Fig. 1). The patient
refused to undergo a skin biopsy. Maculopapular rashes appeared
around the injection site minutes after intravenous injection.
Blood tests were performed and the results were as follows:
Hemoglobin level, 6.4 g/dl; hematocrit, 19.10%; platelet count,
58×109/l; and total leukocyte count,
4.55×109/l, with 8% blast cells and 6% mature basophils.
The fecal occult blood test was positive, the level of ferritin was
1,138 ng/ml and the levels of vitamin B12 and folic acid were
normal. Serum autoantibodies, including the anti-neutrophil
cytoplasmic antibodies (ANCA), myeloperoxidase (MPO)-ANCA and
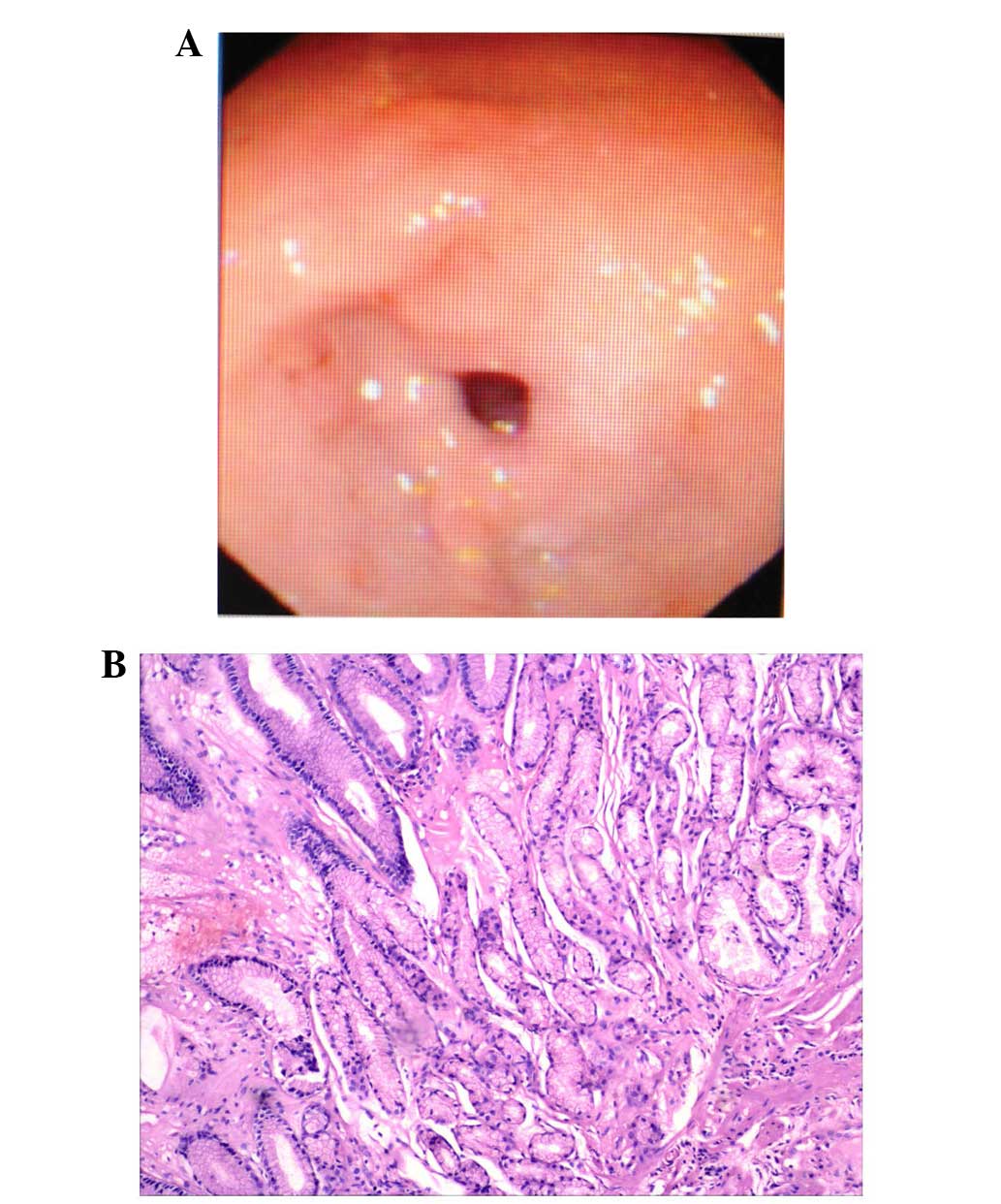
proteinase 3-ANCA, were negative. A gastroscopy demonstrated a
gastric antral ulcer (stage, A1), according to Sakita’s endoscopic
staging system (2) and the
endoscopy biopsy revealed mild mucosal inflammation and no specific
features. (Fig. 2A and B).
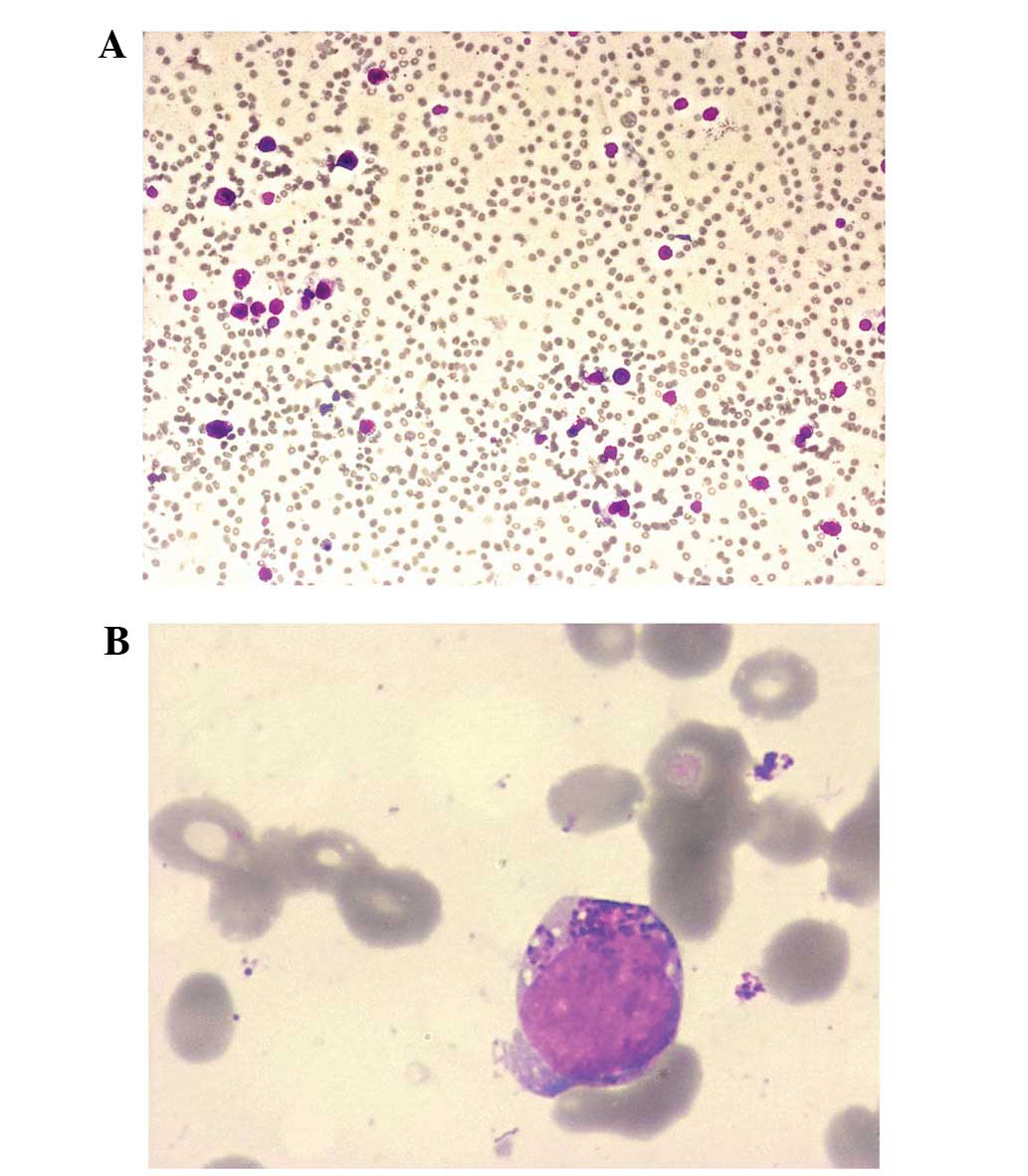
The results of a bone marrow aspirate (stain,
Wright-Giemsa) were as follows: Blast cells, 13%; atypical immature
basophils, 14%; mature basophils, 8%; normal mature neutrophils,
11%; and erythroid cells, 13%. The blast cells contained basophilic
granules, and the vacuoles in the cytoplasm and nuclei were oval
and bilobed and contained nucleoli (Fig. 3A and B). The blast cells were
positive for peroxidase and periodic acid-Schiff staining (PAS) and
negative for α-naphthyl acetate esterase. The blast cells exhibited
metachromasia as a result of staining with toluidine blue. Six days
later, the bone marrow aspirate with Wright-Giemsa stain was
conducted again, and showed 13% blast cells, 16% atypical immature
basophils and 8% mature basophils, with 9% normal mature
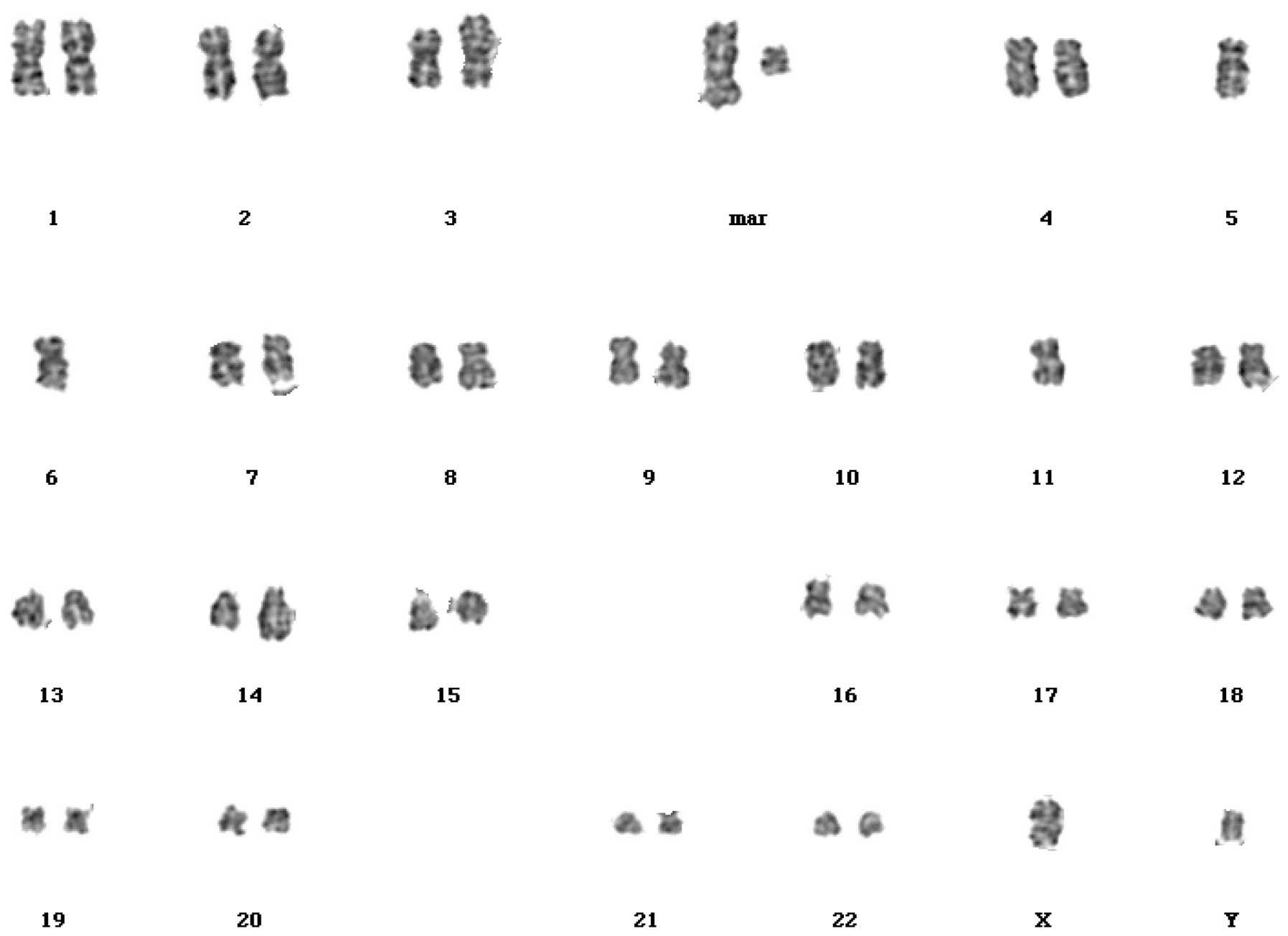
neutrophils. Cytogenetic studies using GTG banding revealed an
abnormal karyotype, 44 XY,add(3)(p26),-5,-11,add(14)(q32),+mar1, +mar2,inc[18]/46,XY[2]
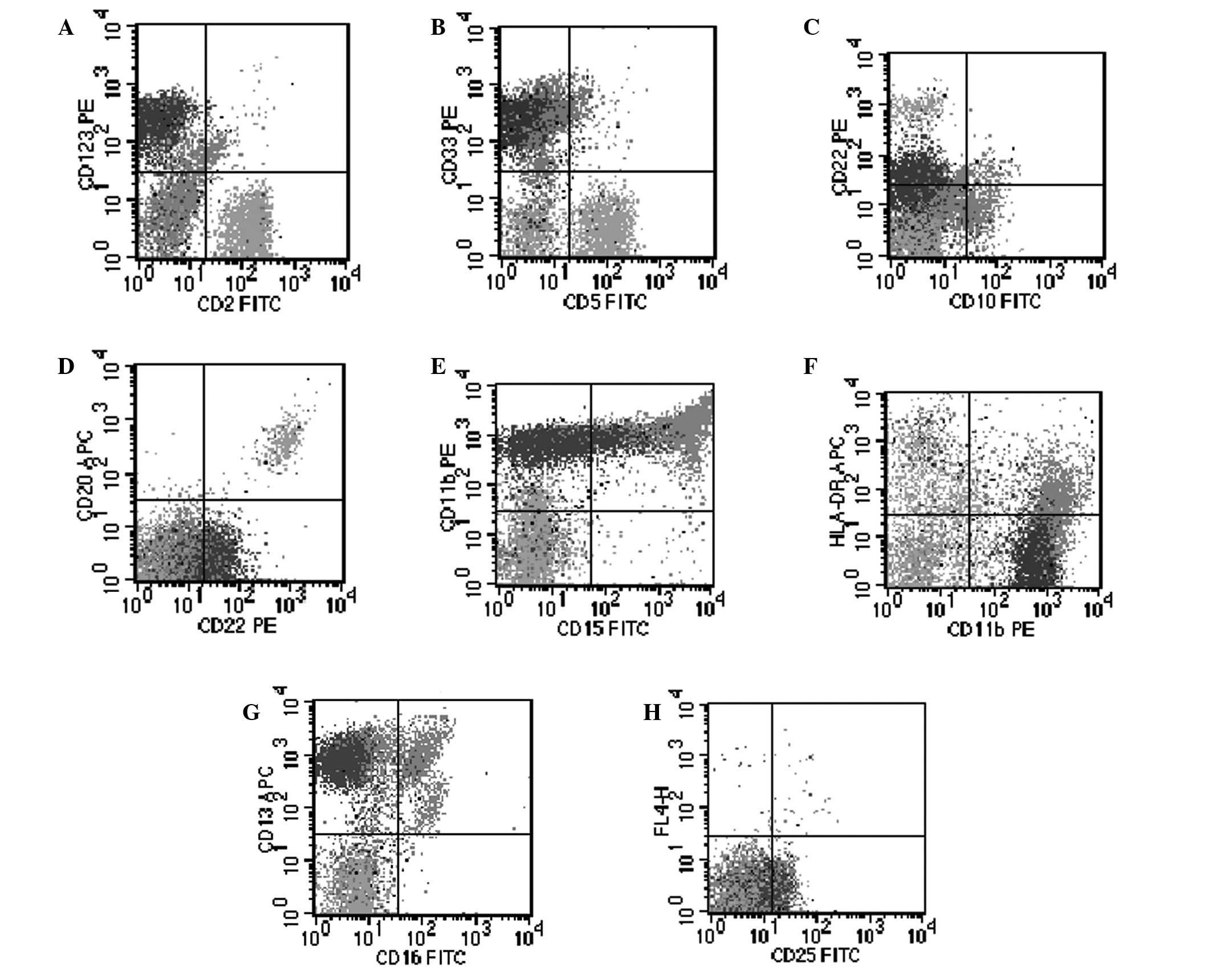
(Fig. 4). Flow cytometric analysis
of the blast cells was positive for cluster of differentiation
(CD)11b, CD13, CD22, CD25, CD33 and CD123 (Fig. 5). BCR-ABL fusion was identified to
be negative by reverse transcription-polymerase chain reaction
analysis and no c-kit D816V mutation was detected.
Following the above-mentioned assessments, the
diagnosis of ABL was determined. Induction therapy with
daunorubicin (45 mg/m2 daily) intravenously for three days and
cytarabine (100 mg/m2 daily) intravenously via
continuous infusion for seven days was initiated at the First
Affiliated Hospital of Chongqing Medical University (Chongqing,
China) on day 13. The hemoglobin level was 5.7 g/dl; the hematocrit
was 17.10%; the platelet count was 40×109/l; and the
total leukocyte count was 4.41×109/l, with 4% blast
cells and 4% basophils. Loratadine, cimetidine and steroids were
introduced into the treatment regimen due to concerns regarding the
patient’s increased histamine levels and the rashes and melena
subsequently disappeared. The patient’s bone marrow examination on
day 21 was hypocellular with 1% blast cells, 6% atypical immature
basophils and 19% mature basophils, with 24% normal mature
neutrophils. The hemoglobin level was 7.4 g/dl; the hematocrit was
22.80%; the platelet count was 31×109/l; and the total
leukocyte count was 2.95×109/l, with no blast cells and
12.2% mature basophils. The rashes reappeared, therefore,
reinduction therapy was initiated with idarubicin (8
mg/m2 daily) intravenously for three days and cytarabine
(100 mg/m2 daily) intravenously via continuous infusion
for seven days. Three weeks later, the bone marrow aspirate (stain,
Wright-Giemsa) showed 3% blast cells, 8% atypical immature
basophils and no mature basophils, with 58% normal mature
neutrophils. The hemoglobin level was 6.9 g/dl; the hematocrit was
21.00%; the platelet count was 34×109/l; and the total
leukocyte count was 3.71×109/l, with no blast cells and
0.8% mature basophils. The patient was discharged from hospital.
However, one month later, the patient contracted a severe pneumonia
infection and succumbed as a result of a multiorgan system failure
without evidence of relapse.
Discussion
Diagnosing de novo ABL can be challenging
(3). It was hypothesized that the
patient described in the present case was diagnosed with de
novo ABL due to the negative results that were obtained from
assessing the BCR-ABL transcripts and because there were no
previous events that were indicative of a blood count abnormality.
De novo ABL was first described by Wick et al
(3) and similar cases have
subsequently been reported by others (4,5). In
the WHO classification of myeloid malignancies (2008 revision)
(1), ABL has been integrated as a
distinct entity and defined as an acute myeloid leukemia (AML) in
which the primary differentiation is to basophils. A peripheral
blood smear should reveal basophilia and the bone marrow may
demonstrate blast cells, often in addition to immature basophilic
granules; mature basophils may or may not be observed. The blast
cells may stain positively for PAS, MPO and toluidine blue
(6). Furthermore, immunophenotyping
may identify a basophilic lineage (4). ABL blast cells exhibit a myeloid
phenotype and the following antigens may be expressed: CD9, CD45,
CD13, CD17, CD33, CD123, CD11b, and CD25. In addition, ABL is not
associated with any specific chromosomal abnormality; however,
cytogenetic studies and molecular analysis are required in all such
cases to rule out blast crisis of chronic myeloid leukemia (CML) as
most cases of ABL develop secondary to CML (7–9).
Differentiation of basophils from mast cells is not
complicated, however, may be problematic when evaluating leukemic
populations and, therefore, mast cell leukemia should be considered
in the differential diagnosis of ABL. While mature basophils are
positive for CD25 and negative for CD117, mast cells are positive
for CD117 and negative for CD25 (10). In complex cases, electron microscopy
may aid with discriminating basophils from mast cells (6). Although CD25 is characteristic, it is
not specific to basophil lineage of blast cells, as CD25 positivity
has been observed in blast cells of CML, and a small number of
cases of myeloblastic and BCR-ABL-positive lymphoblastic leukemia
(11). Furthermore, the c-kit D816V
mutation is detected in the majority of adult cases of systemic
mastocytosis (SM), including mast cell leukemia, which is one of
the minor criteria for a diagnosis of SM, according to the 2008 WHO
classification of myeloproliferative neoplasms (12). In the present case, the
characteristic cytomorphological features, the myeloid
immunophenotype of the blast cells with distinct maturation
patterns and positivity for CD25 and CD123, along with the absence
of the Philadelphia chromosome and the c-kit D816V mutation favored
a diagnosis of ABL and ruled out basophophilic blast crisis of CML,
acute lymphoblastic leukemia, non-basophil lineage AML, AML with
t(6;9)(p23;q34) (13) and mast cell
leukemia.
The maculopapular skin lesions on the patient’s legs
and hands may have been due to vasculitis, although no skin biopsy
was performed. The common hematologic malignancies that are
associated with secondary vasculitis include myelodysplastic
syndrome, lymphomas and hairy cell leukemia. In the majority of
cases they are ANCA negative (14).
In individuals presenting with ABL, the high blood levels of
histamine may elicit cutaneous signs, including pruritus, edema,
maculopapular rashes, areas of hyperpigmentation and/or digestive
signs, such as nausea, vomiting, diarrhea or ulcers. The patient’s
melena, gastric antral ulcer and cutaneous vasculitis may have
resulted from an anaphylactic reaction.
The treatment combination of daunorubicin/idarubicin
and cytarabine was selected with the addition of H1- and
H2-receptor antagonists and steroids introduced later in the
treatment regimen. In ABL, potential serious complications
associated with a massive release of histamines from the
degranulating basophilic cells must be addressed. These effects may
include shock or anaphylaxis, as well as gastric acid
hypersecretion, peptic ulcerations or gastrointestinal bleeding.
Although the prognosis was poor, the patient achieved a certain
level of clinical improvement on initiation of the treatment.
In conclusion, as a rare subtype of AML, ABL is
diagnosed with difficulty and associated with unique therapeutic
complications, including anaphylaxis, and gastroduodenal and
cutaneous involvement. Recognition of the occurrence of ABL enables
the appropriate prophylactic measures to be taken, including the
administration of H1- and H2-receptor blockers, proton pump
inhibitors and steroids, which may aid with minimizing the
treatment-associated complications.
Acknowledgements
The authors would like to thank Dr Zhao-Quan Li and
Dr Sheng Fang for their help with image acquisition.
References
|
1
|
Vardiman JW, Thiele J, Arber DA, et al:
The 2008 revision of the World Health Organization (WHO)
classification of myeloid neoplasms and acute leukemia: rationale
and important changes. Blood. 114:937–951. 2009.
|
|
2
|
Miyake T, Suzaki T and Oishi M:
Correlation of gastric ulcer healing features by endoscopy,
stereoscopic microscopy, and histology, and a reclassification of
the epithelial regenerative process. Dig Dis Sci. 25:8–14.
1980.
|
|
3
|
Wick MR, Li CY and Pierre RV: Acute
nonlymphocytic leukemia with basophilic differentiation. Blood.
60:38–45. 1982.
|
|
4
|
Yokohama A, Tsukamoto N, Hatsumi N, et al:
Acute basophilic leukemia lacking basophil-specific antigens: the
importance of cytokine receptor expression in differential
diagnosis. Int J Hematol. 75:309–313. 2002.
|
|
5
|
Giagounidis AA, Hildebrandt B, Heinsch M,
Germing U, Aivado M and Aul C: Acute basophilic leukemia. Eur J
Hematol. 67:72–76. 2001.
|
|
6
|
Duchayne E, Demur C, Rubie H, Robert A and
Dastugue N: Diagnosis of acute basophilic leukemia. Leuk Lymphoma.
32:269–278. 1999.
|
|
7
|
Peterson LC, Parkin JL, Arthur DC and
Brunning RD: Acute basophilic leukemia: A clinical, morphologic and
cytogenetic study of eight cases. Am J Clin Pathol. 96:160–170.
1991.
|
|
8
|
Seth T, Vora A, Bhutani M, et al: Acute
basophilic leukemia with t (8; 21). Leuk Lymphoma. 45:605–608.
2004.
|
|
9
|
Dastugue N, Duchayne E, Kuhlein E, et al:
Acute basophilic leukaemia and translocation t(X; 6) (p11; q23). Br
J Haematol. 98:170–176. 1997.
|
|
10
|
Agis H, Füreder W, Bankl HC, et al:
Comparative immunophenotypic analysis of human mast cells, blood
basophils and monocytes. Immunology. 87:535–543. 1996.
|
|
11
|
Nakase K, Kita K, Otsuji A, et al:
Diagnostic and clinical importance of interleukin-2 receptor alpha
chain expression on non-T-cell acute leukaemia cells. Br J
Haematol. 80:317–326. 1992.
|
|
12
|
Swerdllow SH, Campo E, Harris NL, et al:
WHO Classification of Tumours of Haematopoietic and Lymphoid
Tissues. 2. 4th edition. IARC Press; Lyon: 2008
|
|
13
|
Chi Y, Lindgren V, Quigley S and Gaitonde
S: Acute myelogenous leukemia with t(6;9)(p23;q34) and marrow
basophilia: an overview. Arch Pathol Lab Med. 132:1835–1837.
2008.
|
|
14
|
Fain O, Hamidou M, Cacoub P, et al:
Vasculitides associated with malignancies: Analysis of sixty
patients. Arthritis Rheum. 57:1473–1480. 2007.
|