Introduction
Medulloblastoma (MB) is the most common primary
brain tumor in children; however, the malignancy rarely occurs in
adults (1). In total, 7–10% of
patients diagnosed with MB develop extraneural metastases, which
most commonly involve the bone and lymph nodes, and recently, the
frequency of reported extraneural metastases has increased
(2–4).
The visceral organs are less common sites of extraneural spread in
medulloblastoma (5). It is generally
believed that the overwhelming majority of cases reported with
extraneural metastasis occur in patients who underwent a craniotomy
(6). At present, typical treatments
for high-risk childhood MB include maximal surgery, craniospinal
radiation therapy and adjuvant chemotherapy (7–9). The 2-
and 5-year overall survival rates following diagnosis of
extraneural metastasis have been reported to be 31 and 26%,
respectively (10). In general, the
survival rate is considered to be poor. In the current study, the
case of a 36-year-old male MB patient with recurrent disease
involving the soft tissues of the occipital bone is presented, as
well as the subsequent treatment course of the patient. In
addition, the extraneural metastasis of MB is discussed. Written
informed consent was obtained from the patient for the publication
of this case report and any accompanying images.
Case report
On November 15, 2009, a 36-year-old male presented
at the Binzhou Medical University Hospital (Binzhou, China) with
nausea and vomiting that had persisted for 5 days, but was not
accompanied by headache, visual impairment or ataxia. The patient
had no significant previous medical history. Cranial magnetic
resonance imaging (MRI) revealed the presence of a lesion in the
fourth ventricle. Total spinal MRI revealed no evidence of
additional central nervous system disease. Subsequently, three days
after presentation, the patient underwent a posterior fossa
craniotomy with gross total resection of the tumor, in which the
cerebrospinal fluid (CSF) circulation was restored, without the
insertion of a drainage strip. Following histopathological
analysis, the resected tumor was diagnosed as average risk MB
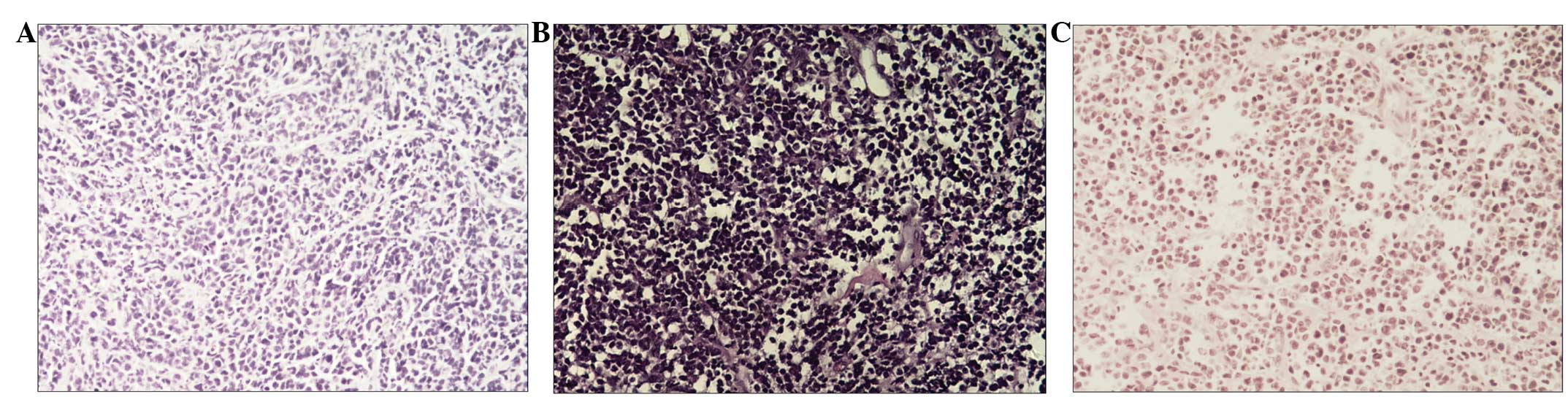
(Fig. 1A). The patient was
administered external beam radiation therapy to the craniospinal
axis at a dose of 36 Gy for 4 weeks, followed by a boost to the
posterior fossa at a dose of 54 Gy for 6 weeks, completing therapy
in early February 2010. Simultaneously, temozolomide (100 mg/day)
was administered orally 1 h before each radiotherapy treatment up
to the end of radiotherapy.
One month after the completion of radiotherapy, the
patient noticed an occipital mass without clinical symptoms, but
did not seek medical attention. The tumor grew to ~4×5×6
cm3 in size, until September 28, 2010, when a surgical
excision was performed. The histopathological diagnosis was also of
MB (Fig. 1B). The patient experienced
left-sided chest pain, and bone and chest computed tomography (CT)
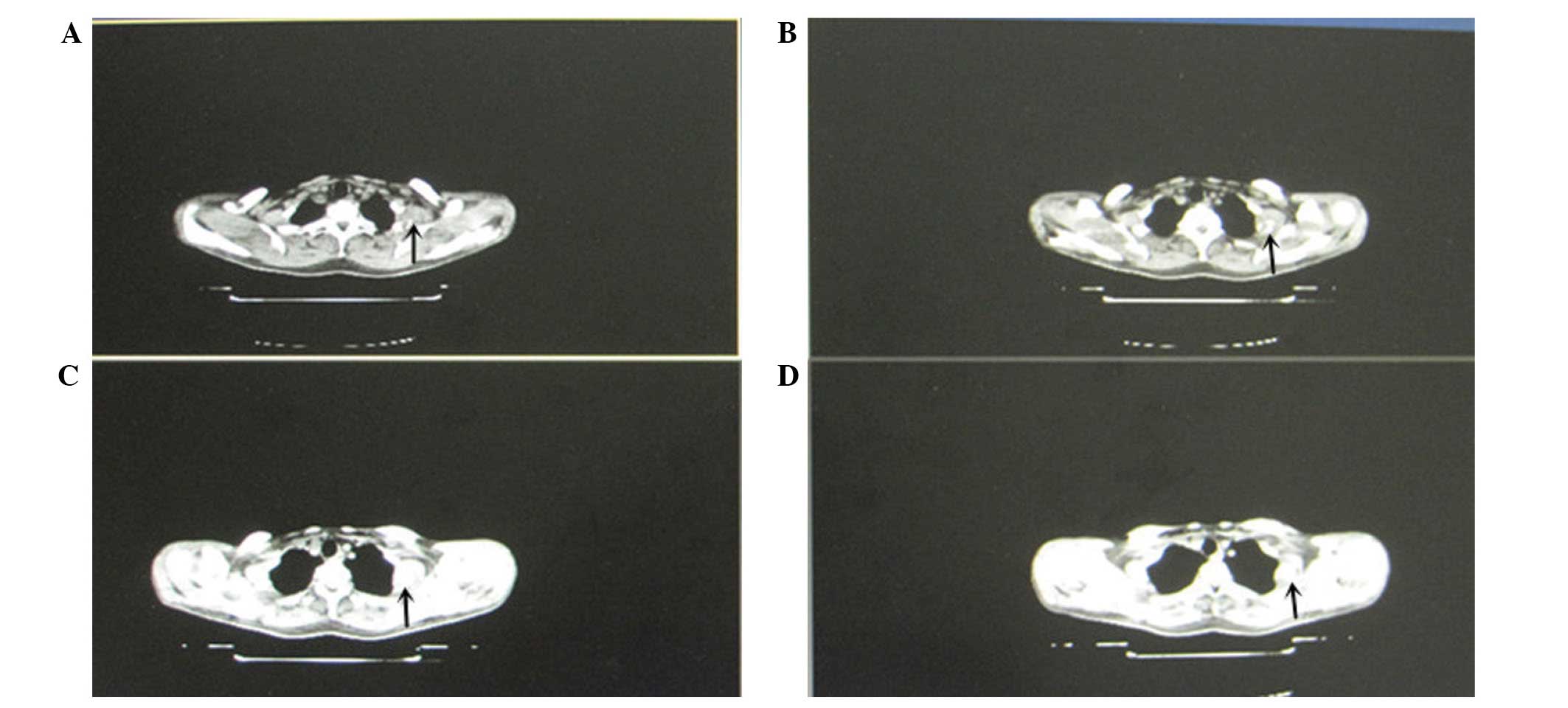
scans revealed fourth left rib metastasis (Fig. 2). On December 16, 2010, the fourth
left rib was resected. Histopathological analysis revealed
metastatic small cell cancer in the bone and soft tissue, which was
associated with the clinical response. Subsequently, according to
the histopathological analysis of the fourth left rib resection and
considering the previous biopsy, metastatic MB was diagnosed
(Fig. 1C). One month after surgery,
the patient experienced pain in multiple locations. Repeat bone and
CT scans revealed multiple bone metastases in several ribs, the
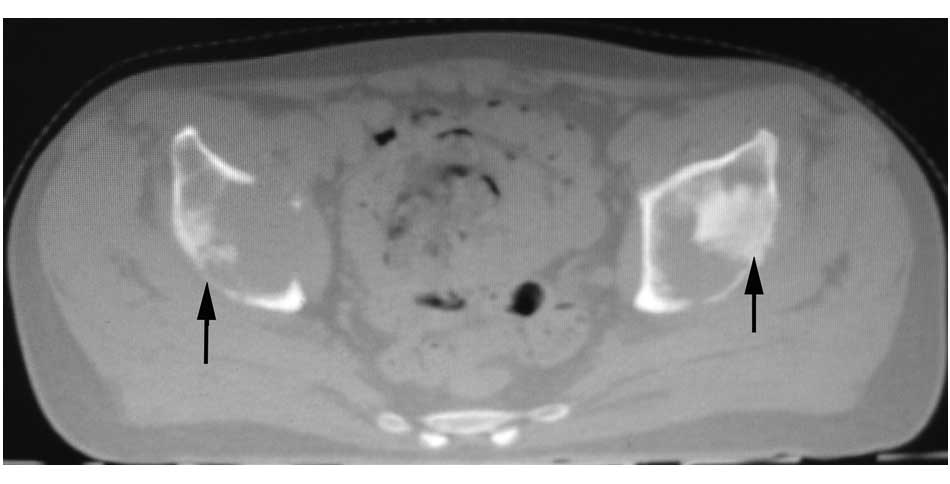
pelvis (Fig. 3), the humeri and the
femora. Consequently, the patient was administered palliative
radiotherapy and oxycodone hydrochloride prolonged-release tablets
(20 mg/12 h) to relieve the symptoms. The patient succumbed at 18
months post-diagnosis due to dissemination of the disease.
Discussion
MB is the most common primary brain tumor in
children, however, the occurrence of MB in adults is extremely
rare, with an incidence of 0.5 cases per 1,000,000 individuals. In
adults, 80% of MB cases occur prior to the end of the fourth decade
of life. Extraneural metastasis in MB is rare, occurring in 7–10%
of MB patients, and 1–2% of patients at the time of the initial
diagnosis (10). At present,
treatment for high-risk childhood MB includes maximal surgery,
craniospinal radiation therapy and adjuvant chemotherapy. Surgical
resection is the standard primary treatment for MB (10). Surgical techniques have three primary
goals: i) Restoring normal CSF flow; ii) maximal tumor resection;
and iii) obtaining tissue for histopathology. Radiotherapy to the
craniospinal axis at a dose of 36 Gy for 4 weeks followed by a
boost to the posterior fossa at a dose of 54 Gy for 6 weeks has
been adopted as standard practice. In a French multicenter study, a
radiotherapy dose of <50 Gy to the posterior fossa was found to
be a poor prognostic factor for MB patients (11). The extent of resection and the
interval between surgery and radiotherapy were also prognostic
factors of MB (12,13). Chemotherapy has been administered for
the treatment of MB for >20 years; initially, the regimens were
the same as those used to treat childhood MB, however, temozolomide
has begun to replace older chemotherapeutic combinations with a
reasonable efficacy and decreased adverse effects (7,14).
The clinical presentation and imaging features of
the disease are different in adults compared with children with MB,
and have the following characteristics: i) The craniosynostosis of
adults has closed and thus the compensatory ability of the cranial
space is poor. The cranial sutures of infants and small children
have not closed, and thus the effects of intracranial pressure
(ICP) differ. In infants, the fontanels bulge when the ICP is too
high. However, the course of the disease in adults is relatively
short. In the present case, the patient presented with nausea and
vomiting that had persisted for 5 days. ii) More than half of adult
MBs are located in the cerebellar hemispheres, whereas MBs in
children are usually located in the cerebellar vermis; cystic
necrosis and calcification within the tumor are more common in
adults with MB than in children (8).
iii) The brain and spinal cord of adults are mature and thus have
good tolerance for post-operative radiotherapy.
Infiltration of the subarachnoid space and
consequent metastatic spread via the CSF is common in MB (10), but extraneural metastasis is extremely
rare. The rarity of extraneural metastasis may be due to the
following factors: i) The lack of intraparenchymal lymphatic
vessels; ii) the collapse of tumor-adjacent intracerebral veins;
iii) the inability of the intracerebral environment for the
selection of metastatic malignant clones; iv) the presence of the
blood-brain barrier; and v) the short survival time of the affected
patients. Notably, the majority of patients with extraneural
metastasis have undergone craniotomy. In a previous study, Pasquier
et al (6) reported that
237/247 (96.0%) of patients with extraneural metastasis had
previously undergone craniotomy. Patients with unresectable tumors
exhibit a worse outcome, often succumbing to primary disease prior
to the development of extraneural metastasis. Extraneural
metastases may be induced iatrogenically, such as peritoneal
metastasis with ventriculoperitoneal shunts (15), hematogenous metastasis secondary to
disruption of blood vessels during surgery, seeding on the incision
and direct extensions from the central nervous system (16).
In the present case, we hypothesize that the dural
suture may not have been sufficiently tight intraoperatively and
thus, implantation metastasis occurred around the incision
following the procedure. Radiotherapy was administered to the
general target area; the surgical incision was not provided with
targeted attention, and additionally, as this was the head and neck
junction, coldspot (insufficient radiation dose deposition) was
prone to emerge in the succession of the radiation field, which
leads to the deficiency of the radiotherapy dose. The clinical
course of osseous metastasis of this patient was possibly initial
transfer of the tumor cells to the neck and then into the venous
system, followed by transfer to multiple bone tissues. For a
patient to be classified as intermediate risk according to the MB
classification (17), further study
is required to ascertain whether the application of preventive
chemotherapy is required and when to administer radiotherapy, or
whether it should be implemented concurrently (17). Thus, to prevent metastasis, during
surgery the surrounding tissue must be protected to reduce damage,
the surgical field must be kept clean, and the post-operative
suture must be closed or the dura repaired, ensuring enhancement of
the ‘tumor-free concept’. If signs of metastasis are identified,
prophylactic radiotherapy of the whole brain and spinal cord should
be administered promptly following surgery, close attention should
be paid to the surgical incision to avoid coldspot, the radiation
dose should be increased and chemotherapy should be
implemented.
When the current patient with MB developed an
extraneural metastasis, the disease progressed rapidly. After the
termination of active treatment, the patient succumbed to the
disease 18 months after diagnosis. The outcome is thus poor in
patients with MB with extraneural metastasis. In conclusion, we
suggest that for a prolonged survival time in adults with MB,
greater emphasis must be placed on the possibility of systemic
involvement. Increased understanding with regard to the
pathogenesis of systemic metastases may be useful for the
development of more aggressive multimodal therapies in the
future.
References
|
1
|
Smoll NR and Drummond KJ: The incidence of
medulloblastomas and primitive neurectodermal tumours in adults and
children. J Clin Neurosci. 19:1541–1544. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Paulino AC: Long-term survival in a child
with extraneural metastasis from medulloblastoma treated with
chemo-radiotherapy. Med Pediatr Oncol. 40:396–397. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Clement J, Varlotto J, Rybka W,
Frauenhoffer E and Drabick JJ: Unusual case of recurrent
extraneural metastatic medulloblastoma in a young adult: Durable
complete remission with Ewing sarcoma chemotherapy regimen and
consolidation with autologous bone marrow transplantation and local
radiation. J Clin Oncol. 31:e316–e319. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wendland MM, Shrieve DC, Watson GA, Chin
SS and Blumenthal DT: Extraneural metastatic medulloblastoma in an
adult. J Neurooncol. 78:191–196. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Koschny R, Ahnert P and Holland H:
Medulloblastoma: Therapy with bortezomib/tumor necrosis
factor-related apoptosis-inducing ligandTumors of the Central
Nervous System. 8. Hayat MA: Springer; New York, NY: pp. 77–84.
2012
|
|
6
|
Pasquier B, Pasquier D, N'Golet A, Panh MH
and Couderc P: Extraneural metastases of astrocytomas and
glioblastomas: Clinicopathological study of two cases and review of
literature. Cancer. 45:112–125. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
van den Bent MJ, Stupp R, Brandes AA and
Lacombe D: Current and future trials of the EORTC brain tumor
group. Onkologie. 27:246–250. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Koral K, Gargan L, Bowers DC, Gimi B,
Timmons CF, Weprin B and Rollins NK: Imaging characteristics of
atypical teratoid-rhabdoid tumor in children compared with
medulloblastoma. AJR Am J Roentgenol. 190:809–814. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang N, Ouyang T, Kang H, Long W, Thomas
B and Zhu S: Adult medulloblastoma: Clinical characters, prognostic
factors, outcomes and patterns of relapse. J Neurooncol. May
31–2015.(Epub ahead of print). View Article : Google Scholar
|
|
10
|
Caracciolo V and Giordano A:
Medulloblastoma: Classification (A Review)Tumors of the Central
Nervous System. Hayat MA: 8. Springer; New York, NY: pp. 23–86.
2012
|
|
11
|
Padovani L, Sunyach MP, Perol D, Mercier
C, Alapetite C, HaieMeder C, Hoffstetter S, Muracciole X, Kerr C,
Wagner JP, et al: Common strategy for adult and pediatric
medulloblastoma: A multicenter series of 253 adults. Int J Radiat
Oncol Biol Phys. 68:433–440. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Abacioglu U, Uzel O, Sengoz M, Turkan S
and Ober A: Medulloblastoma in adults: Treatment results and
prognostic factors. Int J Radiat Oncol Biol Phys. 54:855–860. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lai R: Survival of patients with adult
medulloblastoma: A population-based study. Cancer. 112:1568–1574.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hongeng S, Visudtibhan A, Dhanachai M,
Laothamatus J and Chiamchanya S: Treatment of leptomeningeal
relapse of medulloblastoma with temozolomide. J Pediatr Hematol
Oncol. 24:591–593. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Berry MP, Jenkin RD, Keen CW, Nair BD and
Simpson WJ: Radiation treatment for medulloblastoma. A 21-year
review. J Neurosurg. 55:43–51. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
McComb JG, Davis RL, Isaacs H Jr and
Landing BH: Medulloblastoma presenting as neck tumors in 2 infants.
Ann Neurol. 7:113–117. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rutkowski S, von Bueren A, von Hoff K,
Hartmann W, Shalaby T, Deinlein F, Warmuth-Metz M, Soerensen N,
Emser A, Bode U, et al: Prognostic relevance of clinical and
biological risk factors in childhood medulloblastoma: results of
patients treated in the prospective multicenter trial HIT'91. Clin
Cancer Res. 13:2651–2657. 2007. View Article : Google Scholar : PubMed/NCBI
|