Introduction
Sjögren's syndrome is an autoimmune disease
characterized by lymphocytic infiltration of the exocrine glands,
mainly the salivary and lacrimal glands (1). This leads to a loss of secretory
function, and patients with Sjögren's syndrome commonly present
with oral or ocular symptoms, such as xerostomia or xerophthalmia
(2). Sjögren's syndrome most commonly
affects females in their 50s and 60s (3). In a recent systematic review of 21
studies, the pooled incidence and prevalence of primary Sjogren's
syndrome (pSS) was estimated at 60.82/100,000 persons (4), and the mortality ratio reported in
another meta-analysis in patients with pSS was 682/7,888 persons
over a median average follow-up of 9 years, respectively (5). Whereas symptomatic and topical
treatments are essential in most patients with limited glandular
disease. For systemic complication of the disease, conventional
immunomodulatory treatements such as hydroxychloroquine and
azathioprine or the more specific target specific anti-B
lymphocytic therapeutic agents such as interferon inhibition,
interleukin-6 or interleukin-2 inhibition, and inhibition of B-cell
activating factor are now suggested possible treatments (6).
Mucosa-associated lymphoid tissue (MALT) lymphoma is
defined as an extranodal presentation of a low-grade B-cell
lymphoma. MALT lymphomas may also develop in the salivary glands,
lungs, stomach or lacrimal glands, and are commonly associated with
pre-existing autoimmune diseases or prolonged immune stimulation,
such as long-standing Sjögren's syndrome or chronic Helicobacter
pylori (H. pylori) infection, respectively (7). It is established that the development of
MALT lymphoma in the salivary gland can occur in long-term
autoimmune disease (7). The present
report is a rare case of a young female affected with Sjögren's
syndrome who presented with a single submandibular MALT
lymphoma.
Case report
A 24-year-old Chinese female with no history of drug
use, including tobacco, was admitted to China Medical University
Hospital (Taichung, Taiwan) on June 2014 presenting with a
non-tender left sub-mandibular mass, which started to grow 3 months
prior to the consultation, with rapid enlargement in the third
month. The patient was otherwise asymptomatic, with no clear signs
of xerostomia or xerophthalmia, and had no history of malignancy,
coagulation disorders, arthralgia or autoimmune disease.
Physical examination revealed a firm, movable mass
in the left submandibular area measuring 2.5×2.5 cm. There were no
other abnormalities in the nasopharynx, oral cavity, larynx or
ears, and no palpable cervical lymph nodes. The results of the
laboratory tests, including the differential white blood cell
count, were all within normal limits, and no leukocytosis or anemia
was noted.
Chronic sialolithiasis with sialadenitis was
suspected, and the patient was administered a course of antibiotics
for 2 weeks. However, the treatment did not improve her condition.
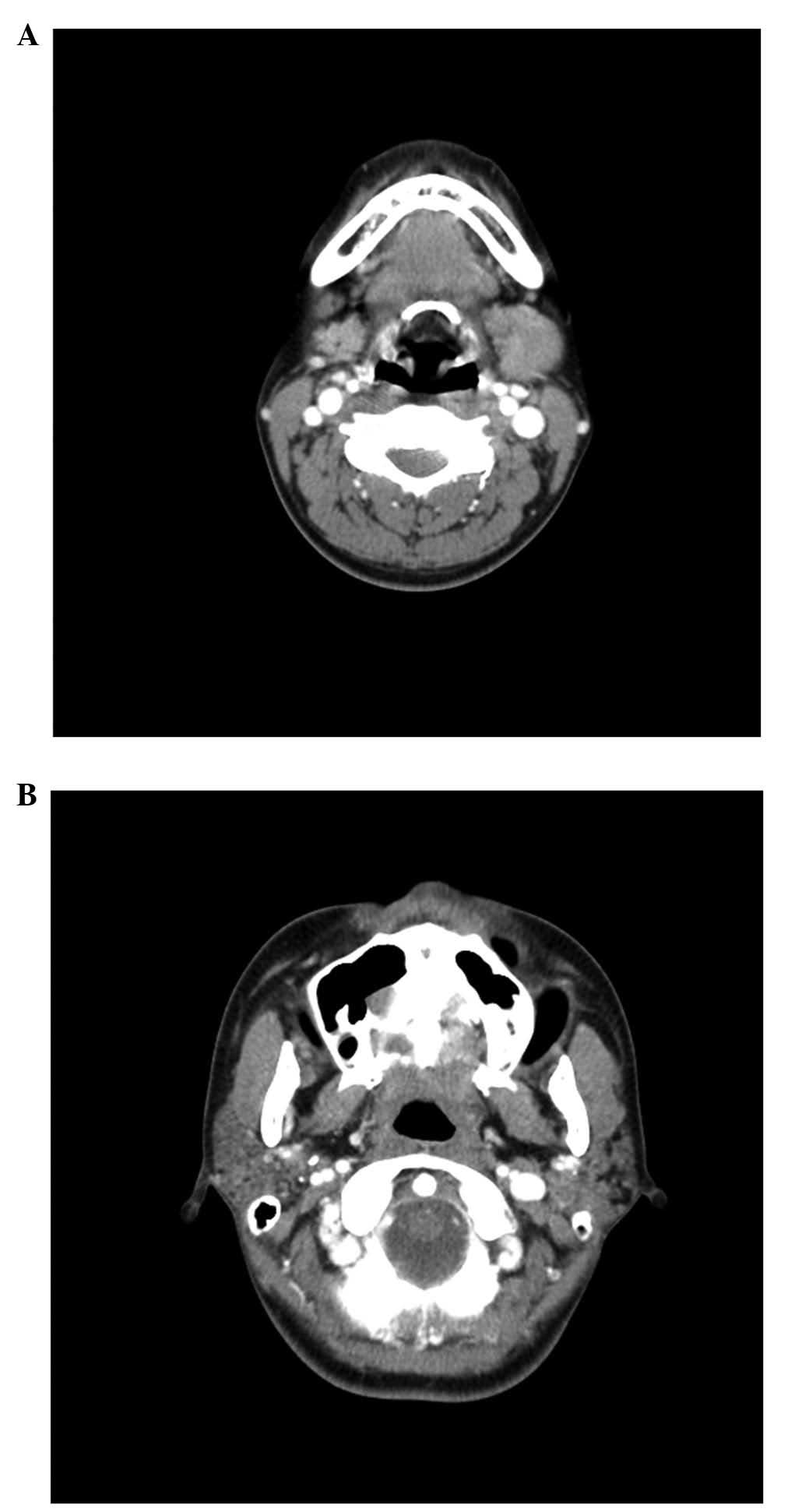
An helical computed tomography (CT) scan revealed an enlarged left
submandibular gland (Fig. 1A) without
any clearly enlarged lymph nodes. In addition, there were
heterogeneous enhancements with multiple microcysts in the
bilateral parotid glands (Fig. 1B).
Thus, the patient underwent ablation of the left submandibular
gland for cosmetic reasons and to rule out the presence of a
malignant growth. The size of the resected gland was 3.5×2.5
cm.
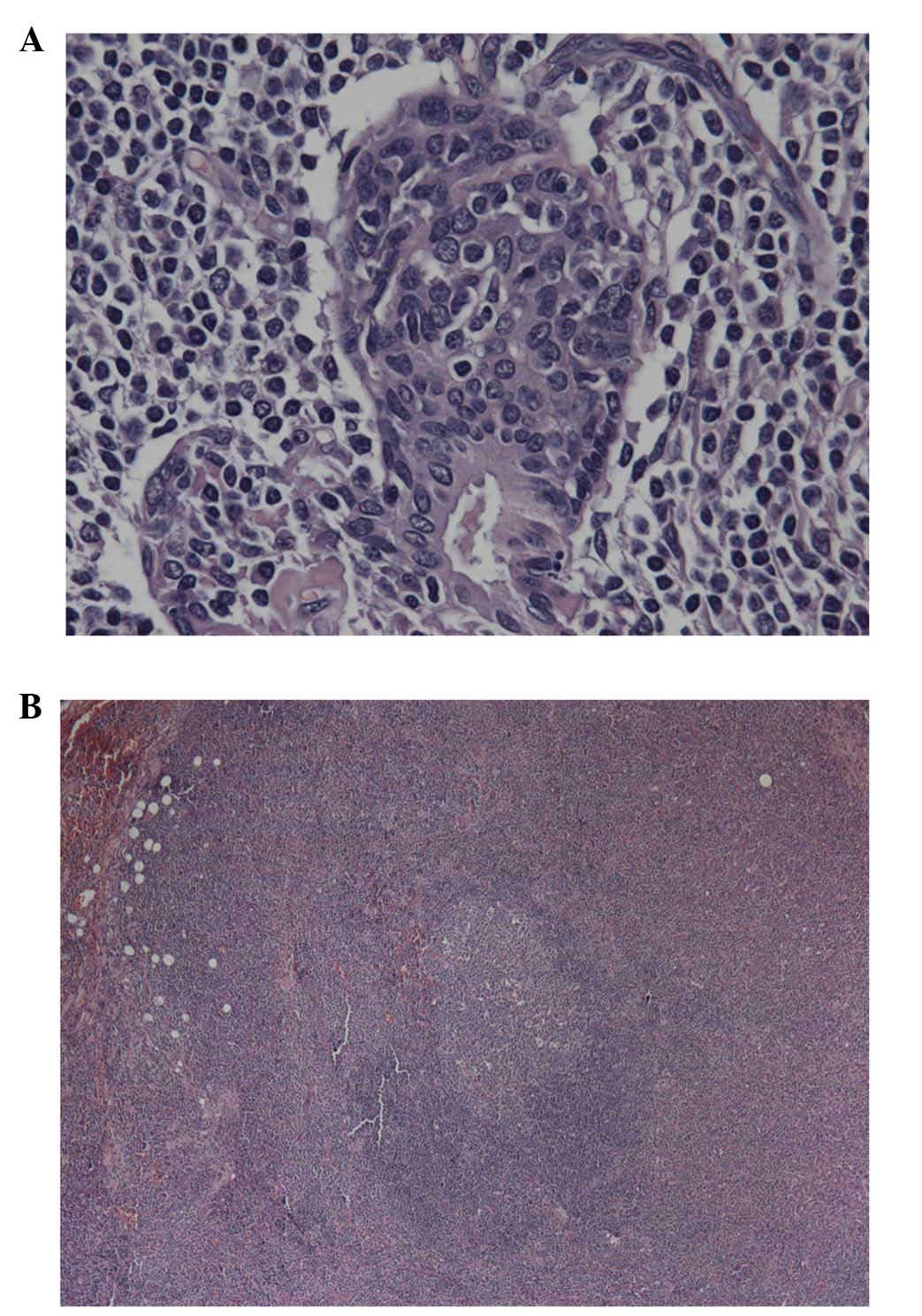
The pathology report was consistent with an
extranodal low-grade marginal zone B-cell lymphoma of MALT lymphoma
characterized by a lympho-epithelial lesion. Aggregates of
neoplastic marginal and monocytoid B-cells were identified in the
focally proliferative ducts of the salivary gland (Fig. 2A). Additionally, the majority of the
normal salivary parenchyma were replaced by neoplastic lymphoid
cells. There were many reactive follicular centers surrounded by an
infiltration of atypical small- to medium-sized lymphoid cells
(Fig. 2B; magnification, ×40). At
×400 magnification, these atypical lymphoid cells exhibited
irregular nuclei with hyperchromatia, chromatin clumping,
occasional prominent small nucleoli and abundant, partially pale
cytoplasm.
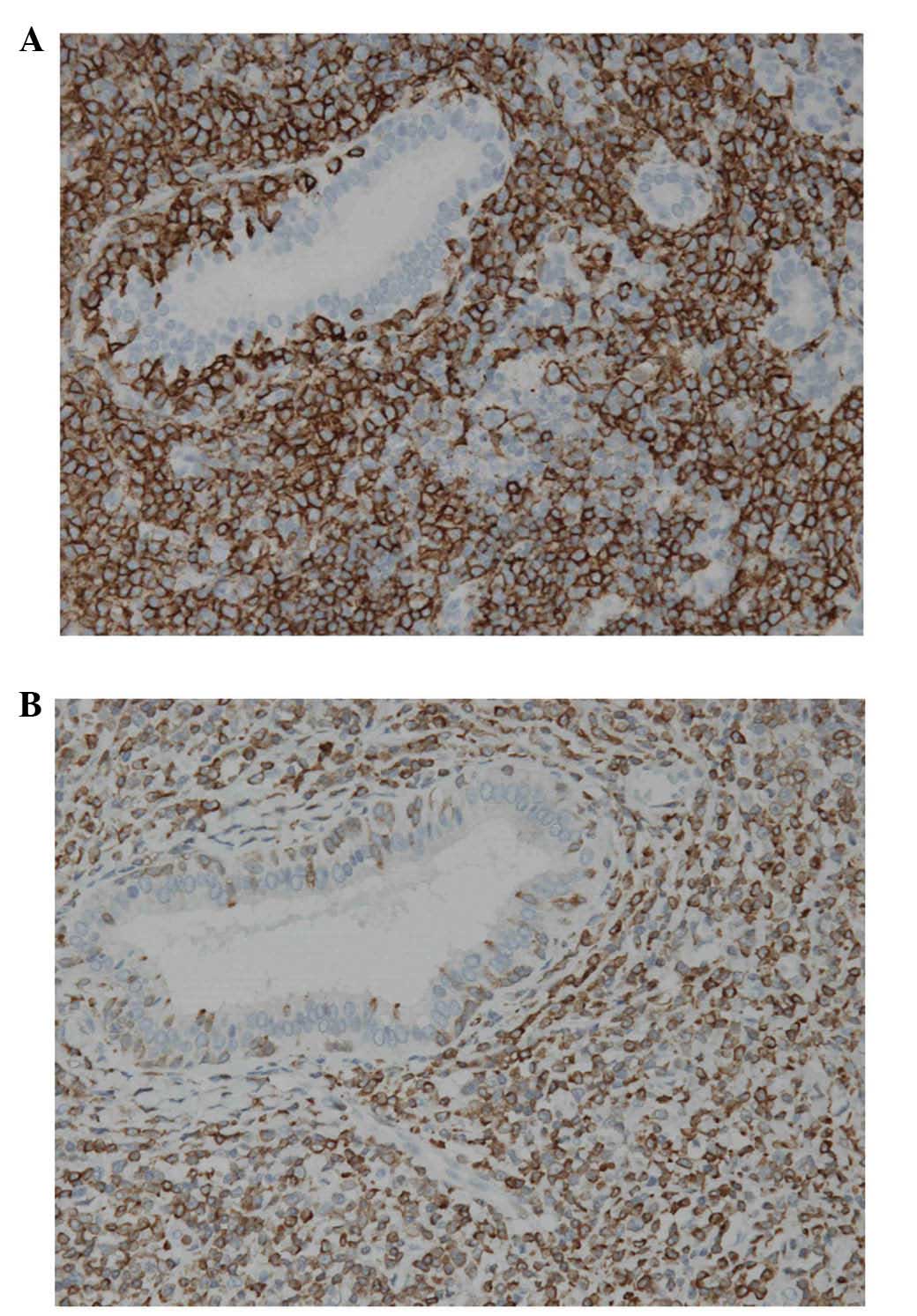
Immunohistochemical (IHC) analysis was performed
using an automated IHC stainer; Leica Bondmax (Leica Biosystems,
Milton Keynes, UK). IHC against cluster of differentiation (CD)3,
CD5, CD10, CD20, CD23, Cyclin-D1, B-cell lymphoma 2 (Bcl-2), IgG4,
κ and λ light chains and in situ hybridization of
Epstein-Barr virus were performed using the commercialized kits
provided by Leica. The results of the IHC analysis indicated that
these monocytoid cells were positive for B-lymphocyte antigen CD20
and Bcl-2 (Fig. 3A and B), but
negative for CD3, 5, 10 and 23, and for cyclin-D1 and B-cell
lymphoma 1. Immunohistochemical analysis for λ and κ light chains
demonstrated λ chain restriction, suggesting that the monocytoid
cells were monoclonal in origin. The results of Epstein-Barr virus
test using in situ hybridization, and the immunoglobulin
(Ig) G4 immunostaining test for the detection of IgG4-associated
sialadenitis, were negative.
The patient was then referred to the Department of
Hematology and Oncology (China Medical University Hospital) for
further assessment and management. Additional tests were conducted,
including a test for H. pylori infection, intestinal
metaplasia and lymphoma-associated alterations in the
gastrointestinal tract were examined by performing upper
gastroendoscopy and colonfiberscopy. However, the results of all
the tests performed were negative. Postoperative bone marrow biopsy
indicated no lymphoma infiltration, while positron emission
tomography/CT scan demonstrated no other malignancy.
Although the patient did not complain of any oral or
ocular symptoms, such as dryness or pain, she was referred to the
Department of Rheumatology (China Medical University Hospital) for
further evaluation. The results of the Schirmer's, Saxon and human
immunodeficiency virus (HIV) tests were negative; the result for
rheumatoid factor was also negative; and serum complement
components C3 (86.9 mg/dl; normal range, 79–152 mg/dl) and C4 (19.7
mg/dl, 16–38 mg/dl), and IgG level (1,010 mg/dl, normal range,
751–1560 mg/dl), were all within normal limits. However, the
antinuclear antibody test revealed a speckled appearance, while
serological markers for Sjögren's syndrome A (SS-A) were strongly
positive. Salivary gland scintigraphy demonstrated reduced trapping
function and excretion of radio-pertechnetate in the salivary
glands.
Despite the absence of clinical symptoms, Sjögren's
syndrome was then considered, based on the laboratory and
radiography findings. Using the Ann Arbor staging system (8), the patient was diagnosed with MALT
lymphoma, stage I with extralymphatic organ involvement, with
underlying SS-A. Although the patient was advised adjuvant therapy
for MALT lymphoma, she chose not to, but did attend regular
follow-ups for the management of her primary Sjögren's syndrome
(pSS). There was no evidence of tumor recurrence over the 6-month
follow-up period subsequent to surgery.
Discussion
Extranodal MALT lymphoma is an indolent B-cell
non-Hodgkin lymphoma that develops in organs that normally lack
lymphoid tissue, including the stomach, lungs, ocular adnexa and
salivary glands (7). A local,
chronic, antigen-driven stimulation triggers the development of
organized lymphoid tissue (7). B-cell
accumulation usually occurs in response to chronic inflammation
associated with chronic infection or autoimmune diseases, including
SS, systemic lupus erythematous (SLE), and Hashimoto thyroiditis
(7). These disorders are considered
to be associated with the development of MALT lymphoma (7), and the stomach is the most commonly
affected organ, often as a result of chronic H. pylori
infection.
MALT lymphoma of the salivary glands is rare: In a
recent study by Vazquez et al (9), salivary gland MALT lymphomas incidence
rate was reported as 0.086 cases/100,000 indivduals. The parotid
gland was involved in 80.87% of all the cases. MALT lymphoma of the
submandibular gland is less common, according to Vazquez et
al (9) only ~14.40% MALT
lymphomas arise from the submandibular gland, with an isolated
submandibular swelling associated with MALT lymphoma as the
singular symptom. Reports in the literature confirm that lymphoma
is rarely the initial presenting symptom in patients with SS;
usually, patients with this disorder experience other clinical
symptoms prior to the development of MALT lymphoma (10). Furthermore, pSS often manifests in the
parotid region, and submandibular involvement is uncommon (11,12).
Symptoms, such as xerostomia or xerophthalmia, are induced by
chronic inflammation of the secretory organs, and usually appear
prior to the development of MALT lymphoma (13).
A meta-analysis report concluded that patients with
SS present a higher risk of lymphoma compared with those with other
autoimmune diseases, such as SLE and rheumatoid arthritis (14). A previous study has also demonstrated
that the relative risk of the development of lymphoma in patients
with Sjögren's syndrome is 44 times higher than in other
individuals, and that clinically identifiable lymphomas develop in
~5% of these patients (15). A
single-center, retrospective study reported that patients with
early-onset SS present a high incidence of lymphoma, but not of
MALT lymphoma (3).
The CT imaging of the patient in the present case
report demonstrates an heterogeneous appearance, with evidence of
multiple microcystic changes in the major salivary glands. These
findings are typically observed in sarcoidosis, benign
lympho-epithelial lesions associated with HIV infection and chronic
inflammatory diseases, such as SS (16,17).
According to the American-European Consensus Group criteria for pSS
(18), ≥4 of the following 6 criteria
must be present for a diagnosis of pSS: i) Oral symptoms; ii)
ocular symptoms; iii) focal sialadenitis evidenced by biopsy of the
minor salivary glands; iv) evidence of kerato-conjunctivitis sicca;
v) presence of SS-A or -B antigen autoantibodies; and vi) changes
in the major salivary glands. Although the patient did not fulfill
the diagnostic criteria, her diagnosis of MALT lymphoma due to pSS
was based on expert opinion, serological and imaging analyses, and
the negative outcome of a series of tests aimed to investigate
other possible etiologies.
The prognosis of patients with MALT lymphoma is
excellent, and the 5-year survival rate is 90% (14). Nonetheless, extragastric MALT
lymphomas tend to be more aggressive than those of gastric origin,
and they may recur in regional or distant lymph nodes and in other
organs that are prone to MALT lymphomas (19). A previous study observed no
significant difference in the survival of patients with MALT
lymphomas treated with localized therapies, including surgery or
radiation therapy, or systemic therapies, such as chemotherapy
and/or immunotherapy with rituximab (14).
Currently, there is no standard treatment for MALT
lymphoma resulting from pSS (14). A
retrospective study reported that surgery is not a prognostic
factor for survival in patients with MALT lymphoma in ≥1 salivary
glands, and that radiotherapy for early-stage disease does not
confer long-term remission (11). A
systematic review also indicated that asymptomatic patients with
localized MALT lymphomas and without bone marrow involvement or
lymphadenopathy, and an international prognostic index score of
0–1, can be treated conservatively with regular follow-ups and no
therapeutic intervention (14). In
addition, the pSS disease activity may be a prognostic factor for
the progression of lymphoma and the requirement for intensive
management (20). The patient in the
current report, despite refusing post-operative adjuvant therapy,
presented no signs of tumor recurrence in the 6 months of follow-up
subsequent to surgery.
In conclusion, although MALT lymphoma of the
salivary glands is a well described condition, these lymphomas are
most often identified in the parotid gland, and a single
submandibular swelling and MALT lymphoma are rare symptoms of pSS.
A multidisciplinary team that includes rheumatologists and head and
neck oncologists is required for managing pSS and MALT lymphoma.
Although uncommon, lymphoid malignant changes should be part of the
differential diagnosis in patients who present with a single
submandibular gland swelling, and should be subjected to extensive
investigation aimed to identify possible underlying diseases.
References
|
1
|
Fox RI: Sjogren's syndrome. Lancet.
366:321–331. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kassan SS and Moutsopoulos HM: Clinical
manifestations and early diagnosis of Sjogren syndrome. Arch Intern
Med. 164:1275–1284. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ramos-Casals M, Cervera R, Font J,
García-Carrasco M, Espinosa G, Reino S, Pallarés L and Ingelmo M:
Young onset of primary Sjögren's syndrome, Clinical and
immunological characteristics. Lupus. 7:202–206. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Qin B, Wang J, Yang Z, Yang M, Ma N, Huang
F and Zhong R: Epidemiology of primary Sjögren's syndrome, A
systematic review and meta-analysis. Ann Rheum Dis. 74:1983–1989.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Singh AG, Singh S and Matteson EL: Rate,
risk factors and causes of mortality in patients with Sjögren's
syndrome A. systematic review and meta-analysis of cohort studies.
Rheumatology (Oxford). 2015.[Epub ahead of print] 2015. View Article : Google Scholar
|
|
6
|
Fazaa A, Bourcier T, Chatelus E, Sordet C,
Theulin A, Sibilia J and Gottenberg JE: Classification criteria and
treatment modalities in primary Sjögren's syndrome. Expert Rev Clin
Immunol. 10:543–551. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Thieblemont C, Bertoni F, Copie-Bergman C,
Ferreri AJ and Ponzoni M: Chronic inflammation and extra-nodal
marginal-zone lymphomas of MALT-type. Semin Cancer Biol. 24:33–42.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee SE, Paik JS, Cho WK, Choi BO, Lee SN,
Jung SE, Park KS, Kang CS, Kim SH, Yang SW and Cho SG: Feasibility
of the TNM-based staging system of ocular adnexal extranodal
marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT
lymphoma). Am J Hematol. 86:262–266. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vazquez A, Khan MN, Sanghvi S, et al:
Extranodal marginal zone lymphoma of mucosa-associated lymphoid
tissue of the salivary glands: a population-based study from 1994
to 2009. Head Neck. 37:18–22. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Voulgarelis M, Dafni UG, Isenberg DA and
Moutsopoulos HM: Malignant lymphoma in primary Sjögren's syndrome,
A multicenter, retrospective, clinical study by the European
Concerted Action on Sjögren's syndrome. Arthritis Rheum.
42:1765–1772. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Anacak Y, Miller RC, Constantinou N,
Mamusa AM, Epelbaum R, Li Y, Calduch AL, Kowalczyk A, Weber DC,
Kadish SP, et al: Primary mucosa- associated lymphoid tissue
lymphoma of the salivary glands: A multicenter Rare Cancer Network
study. Int J Radiat Oncol Biol Phys. 82:315–320. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Movahed R, Weiss A, Velez I and Dym H:
Submandibular gland MALT lymphoma associated with Sjögren's
syndrome, Case report. J Oral Maxillofac Surg. 69:2924–2929. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Maślińska M, Przygodzka M, Kwiatkowska B
and Sikorska-Siudek K: Sjögren's syndrome Still not fully
understood disease. Rheumatol Int. 35:233–241. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kassan SS, Thomas TL, Moutsopoulos HM,
Hoover R, Kimberly RP, Budman DR, Costa J, Decker JL and Chused TM:
Increased risk of lymphoma in sicca syndrome. Ann Intern Med.
89:888–892. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Routsias JG, Goules JD, Charalampakis G,
Tzima S, Papageorgiou A and Voulgarelis M: Malignant lymphoma in
primary Sjögren's syndrome, An update on the pathogenesis and
treatment. Semin Arthritis Rheum. 43:178–186. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cho CM, Tong SL, Bhatia KS, Wong KT, Yuen
HY, Lee YP and Ahuja AT: Unusual parotid gland lesions, A pictorial
review. J Clin Ultrasound. 41:501–508. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rastogi R, Bhargava S, Mallarajapatna GJ
and Singh SK: Pictorial essay, Salivary gland imaging. Indian J
Radiol Imaging. 22:325–333. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shiboski SC, Shiboski CH, Criswell L, Baer
A, Challacombe S, Lanfranchi H, Schiødt M, Umehara H, Vivino F,
Zhao Y, et al: Sjögren's International Collaborative Clinical
Alliance (SICCA) Research Groups: American College of Rheumatology
classification criteria for Sjögren's syndrome: A data-driven,
expert consensus approach in the Sjögren's International
Collaborative Clinical Alliance cohort. Arthritis Care Res
(Hoboken). 64:475–487. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wenzel C, Fiebiger W, Dieckmann K,
Formanek M, Chott A and Raderer M: Extranodal marginal zone B-cell
lymphoma of mucosa-associated lymphoid tissue of the head and neck
area, High rate of disease recurrence following local therapy.
Cancer. 97:2236–2241. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pollard RP, Pijpe J, Bootsma H, Spijkervet
FK, Kluin PM, Roodenburg JL, Kallenberg CG, Vissink A and van
Imhoff GW: Treatment of mucosa-associated lymphoid tissue lymphoma
in Sjogren's syndrome. A retrospective clinical study. J Rheumatol.
38:2198–2208. 2011. View Article : Google Scholar : PubMed/NCBI
|