Introduction
Liposarcoma is the most common type of soft-tissue
sarcoma, accounting for 15% of all sarcomas, with an incidence of
0.9 cases/100,000 person-year in adults (1). According to the 2002 World Health
Organization classification, liposarcomas are classified into 4
histological subtypes: atypical lipomatous
tumor/well-differentiated liposarcoma (ALT-WDLS), dedifferentiated
liposarcoma, myxoid round cell liposarcoma, and pleomorphic
liposarcoma (2). Liposarcoma may
occur anywhere in the body and usually arises from the extremities
(75%) and retroperitoneal cavity (20%) (3). However, primary tracheobronchial tumors
are rare, accounting for only 0.6% of all lung tumors (4). Most of them arise from the
tracheobronchial surface epithelium, and squamous cell carcinomas
are the most common histological types (5). Compared to tracheobronchial epithelial
tumors, mesenchymal neoplasms are quite rare and mostly benign.
Endobronchial liposarcoma is an extremely rare malignant tumor.
Herein, we present a case of primary endobronchial liposarcoma in
the left main bronchus causing cough, left-sided chest pain, and
polypnea after physical activity. The tumor was completely and
successfully removed using high-frequency electric snare and argon
plasma coagulation via flexible bronchoscopy.
Human homologue of the murine double-minute type 2
(MDM2) and cyclin-dependent kinase 4 (CDK4), located on chromosome
12q13-15, are believed to be the proto-oncogenes of liposarcoma and
are thus used for diagnostic and therapeutic considerations
(6–9).
Immunohistochemical (IHC) analysis was performed to detect the
levels of MDM2 and CDK4. Fluorescence in situ hybridization
(FISH) assay was also performed to detect MDM2 and CDK4 gene
amplification in liposarcoma tissue samples to further confirm the
diagnosis and for therapeutic considerations. To the best of our
knowledge, this is the first case of endobronchial ALT-WDLS that
was assessed and diagnosed using the protein and DNA levels of MDM2
and CDK4.
Materials and methods
Immunohistochemistry
Formalin-fixed, paraffin-embedded (FFPE) tissues
were cut into 4-µm sections and mounted on glass slides for IHC and
FISH analysis. The sections were routinely de-waxed, rehydrated in
graded ethanol, and subjected to high-pressure antigen retrieval in
10 mM sodium citrate (pH 6.0). The sections were then incubated
with 3% hydrogen peroxide to block endogenous peroxidase and 10%
normal goat serum to block nonspecific binding. Then, the slides
were incubated at 4°C overnight with a primary antibody (Table I). Primary mouse or rabbit monoclonal
antibodies were purchased from ZSGB-Bio (Beijing, China). Following
incubation with a biotin-labeled secondary antibody, horseradish
peroxidase-streptavidin was added. Finally, sections were treated
with DAB reagent and then counterstained with hematoxylin. Negative
control slides were incubated in phosphate buffer saline without
primary antibodies for each staining.
 | Table I.Antibodies used in immunohistochemical
staining. |
Table I.
Antibodies used in immunohistochemical
staining.
| Antibody | Clone | Dilution | Expression |
|---|
| MDM2 | SMP14 | 1:100 | +++ |
| CDK4 | EP180 | 1:100 | +++ |
| p16 | ABM51100-10 | 1:100 | +++ |
| S-100 | 15E2E2+4C4.9 | 1:100 | ++ |
| Ki-67 | EP5 | 1:100 | ++ |
| CD34 | QBEnd/10 | 1:100 | +++ |
| Rb | 13A10 | 1:50 | ++ |
The IHC evaluation of each protein was performed
independently by two professional pathologists in a double-blinded
manner. In case of ambiguity, a consensus score was obtained for
further evaluation. Five different fields at ×400 magnification
were randomly selected per slide. Staining intensity was classified
as: 0, no staining; 1, weak staining=light yellow; 2, moderate
staining=yellow brown; and 3, strong staining=brown. Percentages of
positively stained cells were categorized as follows: 0, ≤5%
positive cells; 1, 6–25% positive cells; 2, 26–50% positive cells;
3, 51–75% positive cells; and 4, >76% positive cells. The
overall score was calculated using the following formula: staining
intensity score × positive percentage score, which ranged from 0 to
12. The overall score was graded as follows: −, negative; +, 1-4;
++, 5–8; and +++, 9–12.
FISH assay
FISH was performed on 4-µm-thick FFPE tissue
sections with MDM2 (12q15)/chromosome 12 centromere (CEP12) or CDK4
(12q13-14)/CEP12 dual-color probes (ZytoVision, Bremerhaven,
Germany) following the manufacturer's instructions. At least 200
non-overlapping nuclei selected randomly were evaluated. A
MDM2/CEP12 or CDK4/CEP12 ratio ≥2 was defined as amplification of
MDM2 or CDK4.
Ethical statement
Written informed consent was obtained from the
patient for publication of this case report and associated images.
The study was approved by the Ethics Committee of Zhejiang
Provincial People's Hospital.
Case report
A 54-year-old man who smoked was referred to
Zhejiang Provincial People's Hospital (Hangzhou, China) on February
3, 2017 with a 1-year history of cough and polypnea after physical
activity, which worsened 3 days prior to consultation. The patient
developed left-sided chest pain and fever (maximum temperature in
the 3 days before admission: 38.3°C). He denied hypertension,
diabetes, cardiomyopathy, hepatopathy, nephropathy, and a family
history of malignancy. The electrocardiogram and serum tumor
markers were normal. Blood examination showed elevated inflammatory
markers (leukocyte count, 20.2×109/l; neutrophil
percentage, 85%; and C-reactive protein, 117 mg/l).
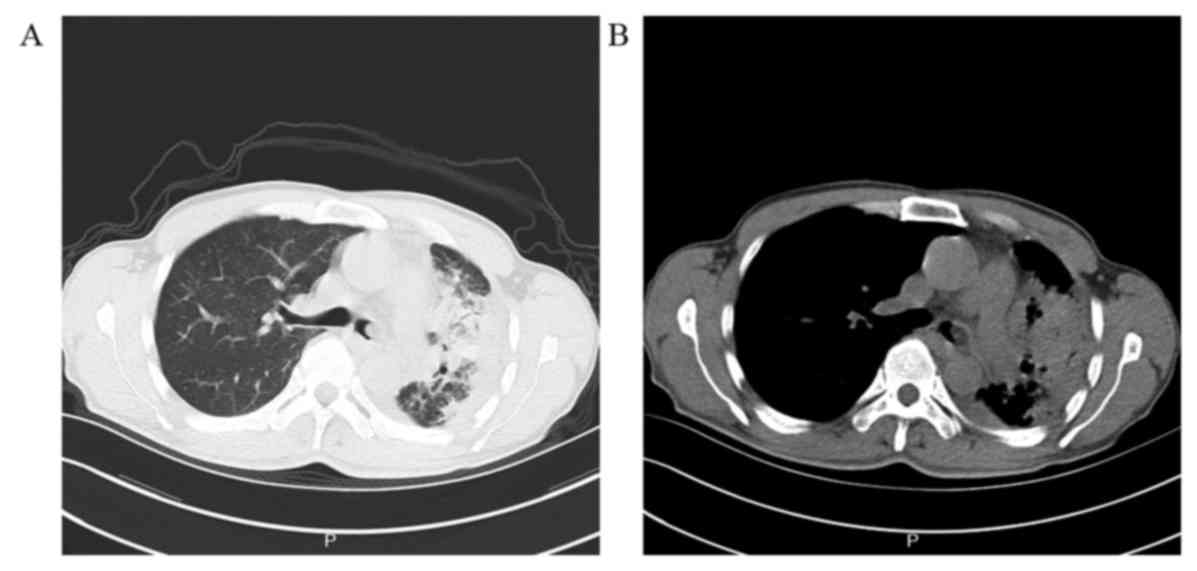
A chest X-ray revealed a large shadow in the left
middle and inferior lung and abnormal lesions along the left
pleura. Chest computed tomography (CT) scan (Siemens Healthcare,
Forchheim, Germany) revealed a neoplasm in the left main bronchus,
measuring 12.8×7.8 mm at its greatest dimension, obstructive
pneumonia, atelectasis of left lung, and a small amount of pleural
effusion in the left hemithorax (Fig.
1).
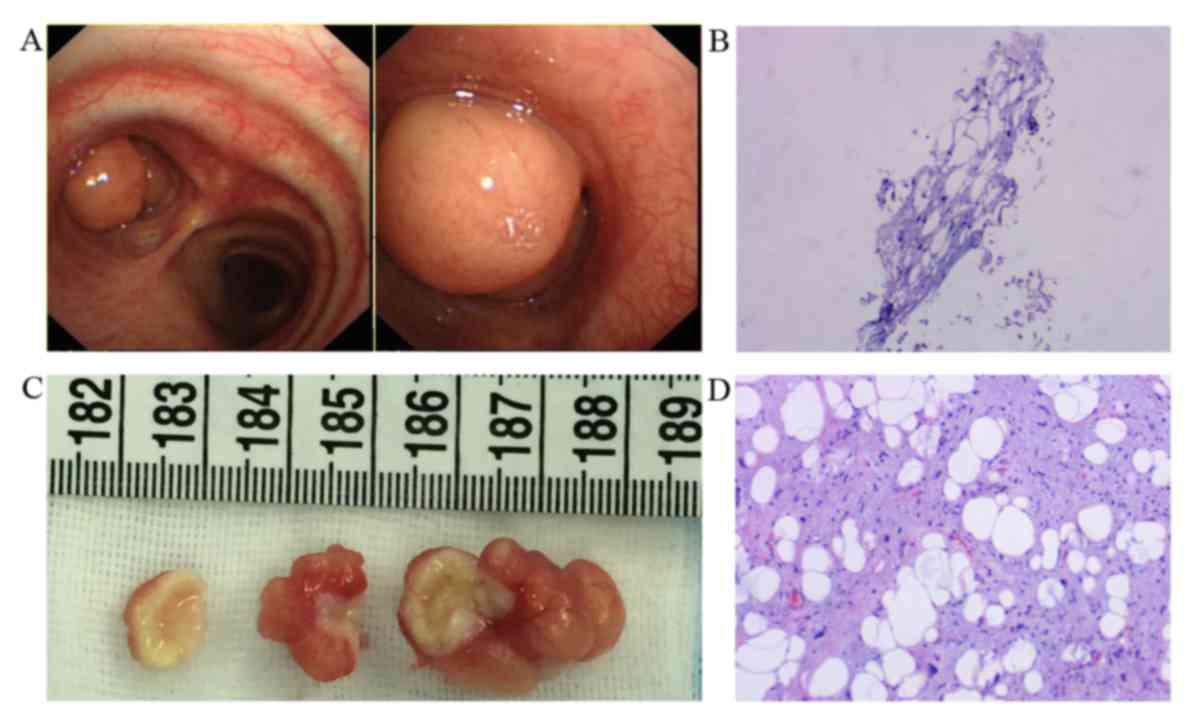
Flexible bronchoscopy under local anesthesia was
performed and demonstrated multiple roundish, pedunculated,
polypoid masses in the left main bronchus, which almost occluded
the bronchial lumen (Fig. 2A).
Bioptic specimens were obtained from the roundish masses and
pathological examination revealed an adipose tissue-derived tumor
(Fig. 2B). The masses were covered
with monolayer bronchial mucosal epithelium that was in good shape.
Submucosal fibrofatty tissue hyperplasia and myxoid degeneration
were seen.
No evidence of tumor metastasis was noted. The
masses were completely resected during the second bronchoscopy
under general anesthesia. The bronchoscope was introduced via an
oral trachea cannula to remove the large bulk of the biopsy
specimens. The mass was snared and resected at its base using a
high-frequency electric snare. Subsequently, the tip of the argon
plasma probe was placed in contact with the mass that was then
extracted simultaneously with the frozen specimens. Intriguingly, 3
tumors were observed and resected completely and successfully in 3
pieces (Fig. 2C). Gross examination
showed that the surgical specimens consisted of 3 solid masses with
moderate hardness and gray cut surfaces, measuring 2.8×1.5×1.5,
1.7×0.7×1, and 1.3×0.8×0.6 cm. Histopathological examination of the
radical resection specimen revealed that it was an ALT-WDLS.
Microscopically, the tumor was composed of mature lipocytes with
varying sizes and hyperplasia lipoblasts that had large, atypical,
and hyperchromatic nuclei (Fig.
2D).
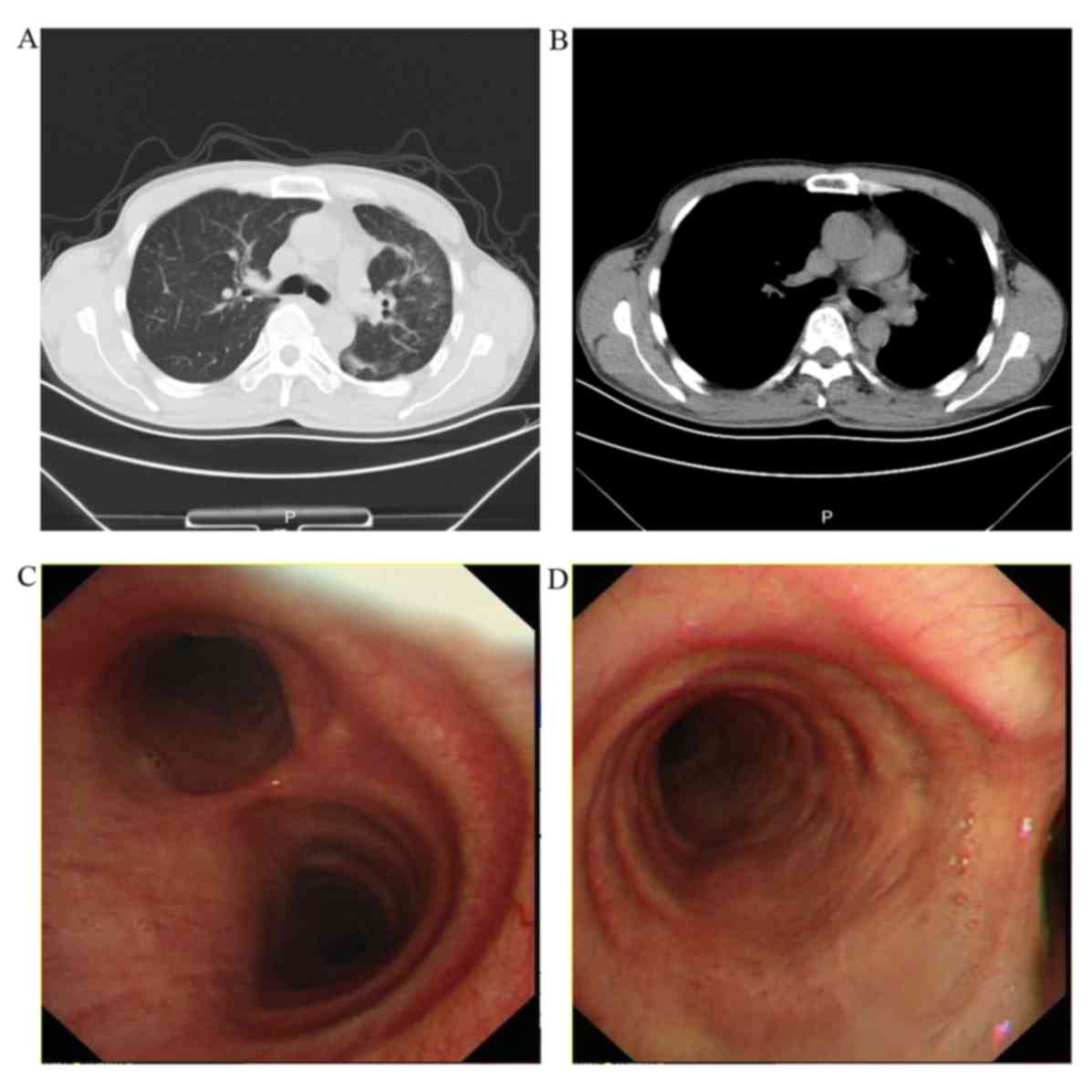
After appropriate antibiotic therapy and endoscopic
surgery, the patient recovered uneventfully. Chest CT performed 1
month postoperative did not show any endobronchial lesion (Fig. 3A and B). In the 6-month follow-up,
bronchoscopy revealed normal bronchial mucosa, and the patient has
good quality of life without evidence of recurrence (Fig. 3C and D).
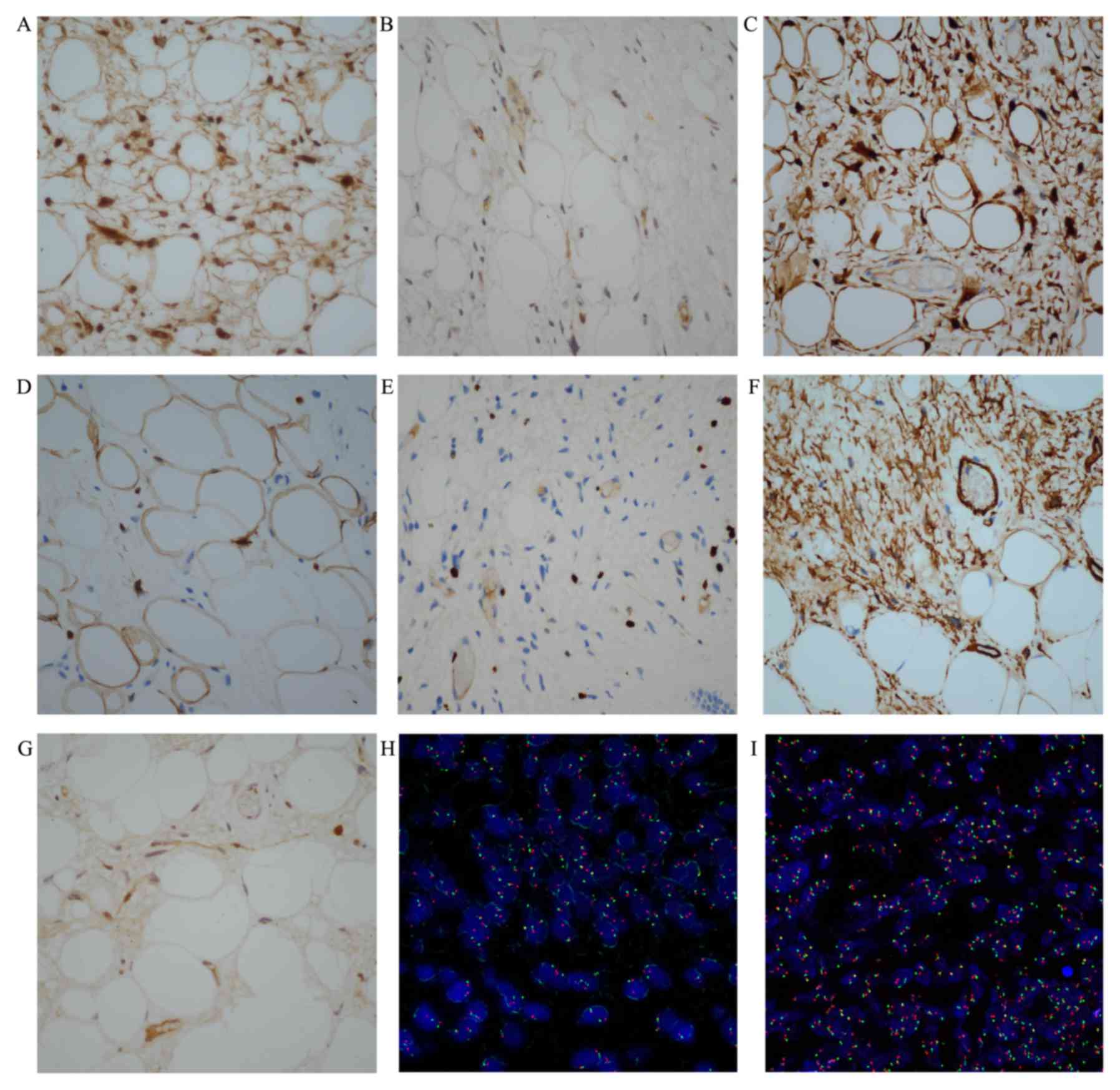
We analyzed FFPE tissues from surgically resected
endobronchial liposarcoma specimens to determine the protein levels
of MDM2 and CDK4 by IHC and DNA amplification of MDM2 and CDK4 via
FISH. The details on the antibodies used and IHC results are
presented in Table I. IHC was
completed on all 3 resected specimens with the human homologue of
MDM2 (+), CDK4 (+), p16 (+), S-100 (+), Ki-67 (+), CD34 (+), and Rb
(+), confirming ALT-WDLS (Fig. 4A-G).
FISH assay performed on all 3 resected specimens found no
amplification of MDM2 and CDK4 in the ALT-WDLS (Fig. 4H and I).
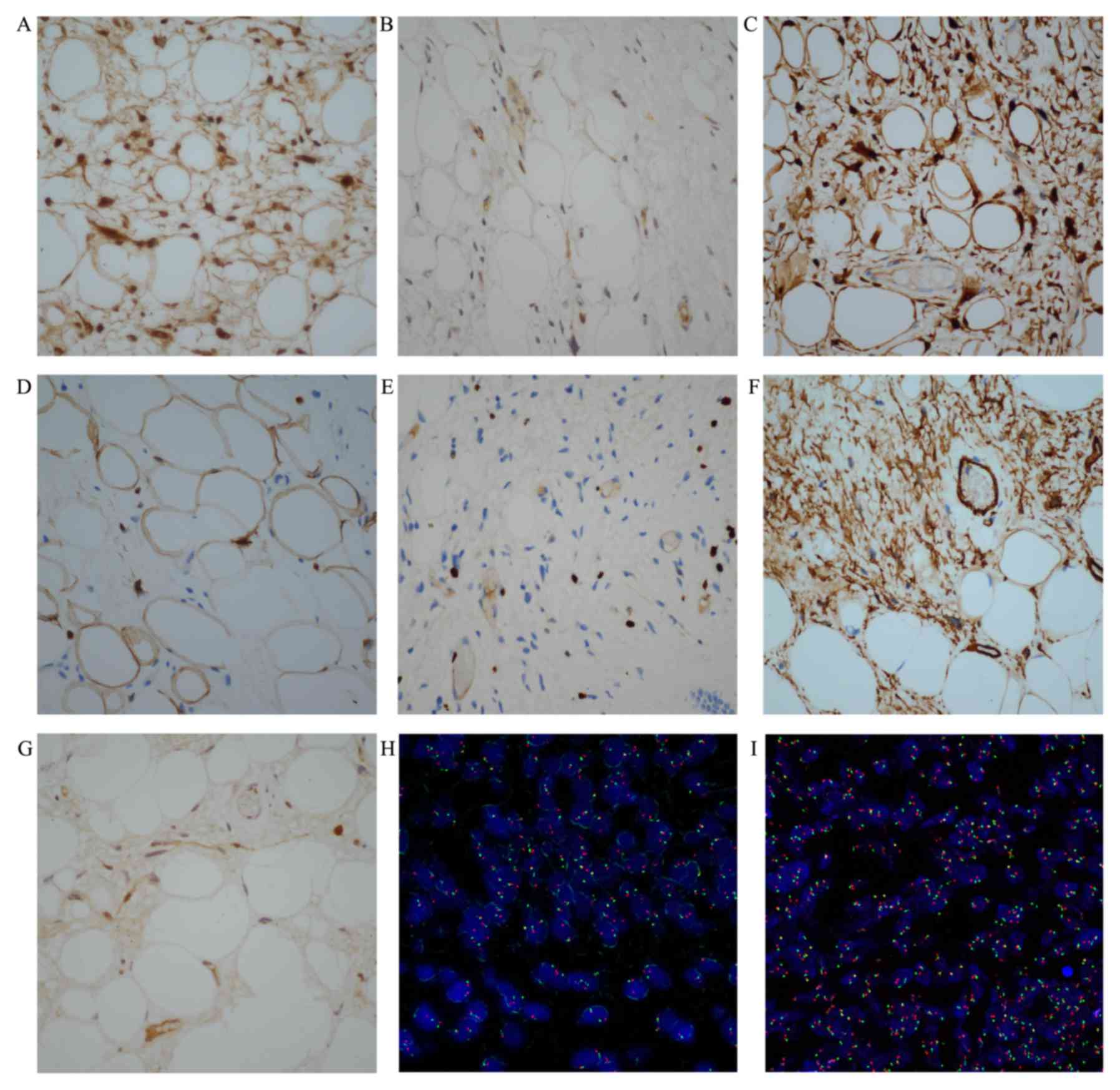 | Figure 4.Representative immunohistochemistry
images of the radical resection specimens (original magnification,
×400). (A) MDM2, (B) CDK4, (C) p16, (D) S-100, (E) Ki-67, (F) CD34
and (G) Rb. The FISH assay revealed non-amplification of MDM2 and
CDK4. (H) The ratio of MDM2 (red signal) to CEP12 (green signal)
was 1.03 (original magnification, ×1,000). (I) The ratio of CDK4
(red signal) to CEP12 (green signal) was 1.06 (original
magnification, ×1,000). MDM2, murine double-minute type 2; CDK4,
cyclin-dependent kinase 4; FISH, fluorescence in situ
hybridization; CD34, cluster of differentiation 34; Rb,
retinoblastoma protein; CEP12, chromosome 12 centromere. |
Discussion
Liposarcoma is the most common soft tissue
malignancy and represents approximately 20% of newly diagnosed
cases (10). It may occur anywhere in
the body and usually arises from the extremities (75%) and
retroperitoneal cavity (20%) (3). We
herein report a case of a man who presented with the disease at 54
years of age, which was consistent with the peak incidence of
liposarcoma at 50–65 years of age (9). To the best of our knowledge, the present
report is the first to describe the clinicopathologic features and
perform genetic analysis of endobronchial liposarcoma. Although
rare, this case is a reminder that clinicians should consider the
possibility of this rare endobronchial tumor in patients with
nonspecific symptoms such as chronic cough, chest pain, and
recurrent pneumonia. Our case was initially misdiagnosed as chronic
bronchitis in other hospitals. Conventional plain chest radiographs
have little diagnostic value for tracheobronchial tumors. Chest CT
and bronchoscopy should be performed early to determine any
tracheobronchial tumor. The tumor biopsy specimens obtained via
bronchoscopy may be insufficient for histological examination,
while endoscopic radical resection specimens can make a definitive
diagnosis (11). In our present
study, the pathologic result of bioptic specimens was adipose
tissue-derived tumor, whereas that of endoscopic radical resection
specimens was ALT-WDLS. The present case highlights the importance
of diagnosis standards for the pathologic diagnosis of
endobronchial liposarcoma. Liposarcoma is relatively resistant to
chemotherapy and radiotherapy (12).
The management of primary endobronchial ALT-WDLS, particularly the
choice between endoscopic treatment and radical surgery, is
controversial because of the disease rarity. As in this case,
endoscopic treatment provides an excellent clinical outcome in
patients with primary endobronchial ALT-WDLS. Our patient remains
under careful long-term follow-up to preclude the possibility of
local recurrence and distant metastasis.
ALT-WDLS is the predominant histopathologic subtype
and represents 40–45% of all liposarcomas (13). A diagnosis of liposarcoma based solely
on conventional histology may be difficult, and genetic and
molecular analyses are helpful for diagnosis and targeted therapies
(9,10,14). A
total of 90% of cases of ALT-WDLS show MDM2 and CDK4 amplification,
which are located on chromosome 12q13-15 (9). MDM2 overexpression promotes cell cycle
progression and tumor progression through ubiquitination and
degradation of p53 (15–17). CDK4 has a fundamental role in
oncogenesis by inactivating p53 and Rb phosphorylation (9,13,18,19). CDK
inhibitor 2A (p16), an important tumor-suppressor gene, suppresses
cell cycle progression through binding to CDK4/6 (20). He et al (21) previously suggested that p16 seemed to
be a sensitive diagnostic biomarker for ALT-WDLS. It may be a
valuable indication for distinguishing ALT-WDLS from deep-seated
lipomas. Thway et al (22)
stressed that p16 appeared to be useful in differentiating
ALT-WDLS/dedifferentiated liposarcoma from other adipocytic
neoplasms, which is consistent with the research of He et al
(21). IHC for MDM2 and CDK4 can be
used as a surrogate method in diagnosing WDLS and improving the
diagnostic accuracy (7,23–25).
Although cytogenetic analyses of MDM2 and CDK4 in liposarcomas of
the extremities and retroperitoneal cavity have been performed, no
research on MDM2 and CDK4 in endobronchial liposarcoma has been
reported by far. Thway et al (22) indicated that the combinations of p16,
MDM2, and CDK4 are useful tools for distinguishing
ALT-WDLS/dedifferentiated liposarcoma from other adipocytic tumors.
Kammerer-Jacquet et al (14)
suggested that the combinations of p16, MDM2, and CDK4 might
improve the diagnostic specificity of ALT-WDLS/dedifferentiated
liposarcoma, which is agreement with the study of Thway et
al (22). Immunostaining of p16,
MDM2 and CDK4 proteins were intensively positive in the present
case, confirming ALT-WDLS. However, FISH assay revealed
non-amplification of MDM2 and CDK4 in the patient. Therefore, high
levels of MDM2 and CDK4 proteins are not caused by gene
amplification. This result is probably caused by other molecular
regulation mechanisms such as transcriptional and
post-transcriptional control of MDM2 and CDK4 gene expression. The
array-based comparative genomic hybridization (array-CGH) technique
has been successfully applied to detect chromosome aberrations and
genomic imbalance in pleomorphic myxoid liposarcoma (26). Other assays such as array-CGH could be
performed in this study which may provide more information about
primary endobronchial liposarcoma. In addition, other genetic
events such as gene mutations in CTNNB1, CDH1, FBXW7, EPHA1 and the
fusion of FUS-DDIT3/EWSR1-DDIT3, known to be involved in
liposarcomas could be performed. We acknowledge it as the
limitation of our study. Therefore, reports of more such cases and
further research are needed to elucidate the specific pathogenesis
of primary endobronchial liposarcomas and whether it differs from
liposarcomas in the extremity and retroperitoneum.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from the
National Natural Science Foundation of China (grant nos. 81470241
and 81470109) and The Foundation of Science and Technology
Department of Zhejiang Province (grant no. 2014C37022).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contribution
YQL and YSL designed the study, and YSL and HJ
collected the data and drafted the manuscript. QRX and HBZ
performed the experiment and helped to revise the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Zhejiang Provincial People's Hospital. Written
informed consent was obtained from the patient to participate in
the study.
Consent for publication
Written informed consent was obtained from the
patient for the publication of this case report and associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ducimetière F, Lurkin A, Ranchère-Vince D,
Decouvelaere AV, Péoc'h M, Istier L, Chalabreysse P, Muller C,
Alberti L, Bringuier PP, et al: Incidence of sarcoma histotypes and
molecular subtypes in a prospective epidemiological study with
central pathology review and molecular testing. PLoS One.
6:e202942011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fletcher CDM, Bridge JA, Hogendoorn P and
Mertens F: WHO classification of tumours of soft tissue and bone.
4th edition. IARC Press; Lyon: 2013
|
|
3
|
Kashu Y, Yukumi S, Tsunooka N, Tanigawa K,
Arakane M, Nakagawa H and Kawachi K: Successful resection of a
massive mediastinal liposarcoma that rapidly extended into the
entire left thoracic cavity: Report of a case. Surg Today.
42:68–71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stevic R and Milenkovic B:
Tracheobronchial tumors. J Thorac Dis. 8:3401–3413. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Macchiarini P: Primary tracheal tumours.
Lancet Oncol. 7:83–91. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Weaver J, Downs-Kelly E, Goldblum JR,
Turner S, Kulkarni S, Tubbs RR, Rubin BP and Skacel M: Fluorescence
in situ hybridization for MDM2 gene amplification as a diagnostic
tool in lipomatous neoplasms. Mod Pathol. 21:943–949. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dei Tos AP, Doglioni C, Piccinin S, Sciot
R, Furlanetto A, Boiocchi M, Dal Cin P, Maestro R, Fletcher CD and
Tallini G: Coordinated expression and amplification of the MDM2,
CDK4, and HMGI-C genes in atypical lipomatous tumours. J Pathol.
190:531–536. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Singer S, Socci ND, Ambrosini G, Sambol E,
Decarolis P, Wu Y, O'Connor R, Maki R, Viale A, Sander C, et al:
Gene expression profiling of liposarcoma identifies distinct
biological types/subtypes and potential therapeutic targets in
well-differentiated and dedifferentiated liposarcoma. Cancer Res.
67:6626–6636. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kollar A and Benson C: Current management
options for liposarcoma and challenges for the future. Expert Rev
Anticancer Ther. 14:297–306. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nassif NA, Tseng W, Borges C, Chen P and
Eisenberg B: Recent advances in the management of liposarcoma.
F1000Res. 5:29072016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Spinelli P, Pizzetti P, Lo Gullo C, Rocca
F, Gobbi A and Ravasi G: Resection of obstructive bronchial
fibrolipoma through the flexible fiberoptic bronchoscope.
Endoscopy. 14:61–63. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Patel RB, Li T, Liao Z, Jaldeepbhai JA,
Perera HAPNV, Muthukuda SK, Dhirubhai DH, Singh V, Du X and Yang J:
Recent translational research into targeted therapy for
liposarcoma. Stem Cell Investig. 4:212017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Laurino L, Furlanetto A, Orvieto E and Dei
Tos AP: Well-differentiated liposarcoma (atypical lipomatous
tumors). Semin Diagn Pathol. 18:258–262. 2001.PubMed/NCBI
|
|
14
|
Kammerer-Jacquet SF, Thierry S, Cabillic
F, Lannes M, Burtin F, Henno S, Dugay F, Bouzillé G, Rioux-Leclercq
N, Belaud-Rotureau MA and Stock N: Differential diagnosis of
atypical lipomatous tumor/well-differentiated liposarcoma and
dedifferentiated liposarcoma: utility of p16 in combination with
MDM2 and CDK4 immunohistochemistry. Hum Pathol. 59:34–40. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vargas DA, Takahashi S and Ronai Z: Mdm2:
A regulator of cell growth and death. Adv Cancer Res. 89:1–34.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Oliner JD, Kinzler KW, Meltzer PS, George
DL and Vogelstein B: Amplification of a gene encoding a
p53-associated protein in human sarcomas. Nature. 358:80–83. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Oliner JD, Pietenpol JA, Thiagalingam S,
Gyuris J, Kinzler KW and Vogelstein B: Oncoprotein MDM2 conceals
the activation domain of tumour suppressor p53. Nature.
362:857–860. 1993. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kato J, Matsushime H, Hiebert SW, Ewen ME
and Sherr CJ: Direct binding of cyclin D to the retinoblastoma gene
product (pRb) and pRb phosphorylation by the cyclin D-dependent
kinase CDK4. Genes Dev. 7:331–342. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weinberg RA: The retinoblastoma protein
and cell cycle control. Cell. 81:323–330. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fåhraeus R, Paramio JM, Ball KL, Lain S
and Lane DP: Inhibition of pRb phosphorylation and cell-cycle
progression by a 20-residue peptide derived from p16CDKN2/INK4A.
Curr Biol. 6:84–91. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
He M, Aisner S, Benevenia J, Patterson F,
Aviv H and Hameed M: p16 immunohistochemistry as an alternative
marker to distinguish atypical lipomatous tumor from deep-seated
lipoma. Appl Immunohistochem Mol Morphol. 17:51–56. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thway K, Flora R, Shah C, Olmos D and
Fisher C: Diagnostic utility of p16, CDK4, and MDM2 as an
immunohistochemical panel in distinguishing well-differentiated and
dedifferentiated liposarcomas from other adipocytic tumors. Am J
Surg Pathol. 36:462–469. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pilotti S, Della Torre G, Mezzelani A,
Tamborini E, Azzarelli A, Sozzi G and Pierotti MA: The expression
of MDM2/CDK4 gene product in the differential diagnosis of well
differentiated liposarcoma and large deep-seated lipoma. Br J
Cancer. 82:1271–1275. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Binh MB, Sastre-Garau X, Guillou L, de
Pinieux G, Terrier P, Lagacé R, Aurias A, Hostein I and Coindre JM:
MDM2 and CDK4 immunostainings are useful adjuncts in diagnosing
well-differentiated and dedifferentiated liposarcoma subtypes: A
comparative analysis of 559 soft tissue neoplasms with genetic
data. Am J Surg Pathol. 29:1340–1347. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Coindre JM, Mariani O, Chibon F, Mairal A,
De Saint Aubain Somerhausen N, Favre-Guillevin E, Bui NB, Stoeckle
E, Hostein I and Aurias A: Most malignant fibrous histiocytomas
developed in the retroperitoneum are dedifferentiated liposarcomas:
A review of 25 cases initially diagnosed as malignant fibrous
histiocytoma. Mod Pathol. 16:256–262. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Creytens D, van Gorp J, Ferdinande L, Van
Roy N and Libbrecht L: Array-based comparative genomic
hybridization analysis of a pleomorphic myxoid liposarcoma. J Clin
Pathol. 67:834–835. 2014. View Article : Google Scholar : PubMed/NCBI
|