Introduction
Ovarian cancer is the leading cause of
cancer-associated mortality resulting from gynecological tumors in
the USA. The American Cancer Society estimated that 22,280 females
would develop ovarian cancer in 2016 and that 14,240 females may
succumb to the disease (1).
Epithelial ovarian cancer (EOC) accounts for >80% of all cases
of ovarian cancer. Among patients with EOC, ~3/4 cases are
diagnosed in patients with stage III or IV disease due to the lack
of sensitive detection methods or prominent symptoms; in addition,
patients in these later disease stages exhibit a 5-year survival
rate of <30%. Molecular targeted therapeutic drugs, including
bevacizumab and olaparib, have been confirmed to improve
progression-free survival (PFS) rates in women with EOC, but they
do not increase overall survival (OS) rates (2–8).
Furthermore, the cost of these drugs means that patients in
developing countries may not be able to afford them. Therefore,
complete resection with no residual disease is a critical factor
for the improvement of the prognosis of patients with advanced EOC.
However, it is difficult to completely resect the lesions of
advanced EOC on account of widespread intra-abdominal metastases
and peritoneal implantation. Consequently, molecular changes
associated with the metastasis of EOC may be identified to provide
novel targets for intervention.
A common feature of tumors is the dysregulation of
pH control (9). To sustain tumor
growth, cancer cells need to adapt to the tumor-associated acidic
microenvironment. Under these circumstances, the activation of
Na+/H+ exchanger isoform 1 (NHE1) is crucial
for the control of intracellular pH (pHi). NHE1 is a ubiquitous
membrane protein that is known to regulate pH homeostasis via the
electroneutral exchange of one intracellular H+ ion for
one extracellular Na+ ion (10,11).
Intracellular alkalinization and acidification of the
microenvironment caused by NHE1 serve an important role in cell
migration, invasion, proliferation, differentiation and apoptosis
in solid tumors and hematological malignancies, including breast
cancer (12,13), hepatocellular carcinoma (14,15),
pancreatic ductal adenocarcinoma (16), cervical cancer (17) and acute myeloid leukemia (18). Regarding triple-negative breast
cancer, NHE1 inhibition increases the efficacy of paclitaxel in
MDA-MB-231 cells and decreases their viability as well as their
migratory and invasive potential in vitro. Furthermore, the
knockout of NHE1 markedly decreases in vivo xenograft tumor
growth of MDA-MB-231 cells in athymic nude mice (12).
A previous study, which used reverse capture
antibody microarray technology to identify plasma autoantibodies
from patients with mucinous ovarian cancer, revealed significant
overexpression of NHE1 in plasma samples obtained from patients
with cancer compared with those obtained from healthy controls
(19). However, little research has
been performed on the role of NHE1 in the development and
progression of EOC. In the present study, the expression pattern of
NHE1 was detected in human EOC tissues and human ovarian cancer
cell lines. In addition, the prognostic value of NHE1 in EOC was
analyzed.
Materials and methods
Patients and samples
A total of 184 formalin-fixed paraffin-embedded
tissue samples consisting of 129 EOCs, 18 borderline tumors, 22
benign tumors and 15 normal ovarian tissues, were retrieved from
the archives of the Department of Pathology, Chongqing Medical
University (Chongqing, China), from February 2005 to December 2010.
Fresh surgical specimens, which were obtained from 52 patients with
epithelial ovarian tumors and 10 patients with normal ovaries, were
snap-frozen in liquid nitrogen immediately following surgery
performed between October 2011 and December 2012 and stored at
−80°C. The epithelial ovarian tumor samples comprised 28 EOCs, 10
borderline tumors and 14 benign tumors. Normal ovarian tissue
samples were collected from patients who underwent hysterectomy for
non-ovarian diseases. All patients had undergone cytoreductive
surgery as a primary treatment.
The specific clinicopathological features of
patients with EOC who provided samples for immunohistochemical
staining are summarized in Table I.
Surgical staging was based on the International Federation of
Gynecology and Obstetrics (FIGO) staging system. The carcinoma
grade was subdivided into low (G1) and high (G2/G3) grade. PFS and
OS rates were calculated from the date of initial diagnosis to the
date of progression/mortality or the date of the last follow-up.
Ethical approval for the present study was obtained from the local
ethics committee. Prior written informed consent was obtained from
the patients who participated in the present study in accordance
with The Declaration of Helsinki.
 | Table I.Clinicopathological features in 129
patients with EOC according to NHE1 expression. |
Table I.
Clinicopathological features in 129
patients with EOC according to NHE1 expression.
|
| n | NHE1
Expression |
|
|---|
|
|
|
|
|
|---|
| Clinicopathological
parameters | n=129 | Low (%) | High (%) | P-value |
|---|
| Age, years |
|
|
| 0.445 |
|
<50 | 61 | 11 (18.0) | 50 (82.0) |
|
|
>50 | 68 | 16 (23.5) | 52 (76.5) |
|
| Serum CA-125,
U/ml |
|
|
| 0.792 |
|
<35 | 17 | 4 (23.5) | 13 (76.5) |
|
|
>35 | 112 | 23 (20.5) | 89 (79.5) |
|
| FIGO stage |
|
|
|
<0.001a |
|
I/II | 37 | 17 (45.9) | 20 (54.1) |
|
|
III/IV | 92 | 10 (10.9) | 82 (89.1) |
|
| Grade |
|
|
|
<0.001a |
| G1 | 23 | 11 (47.8) | 12 (52.2) |
|
|
G2/G3 | 106 | 16 (15.1) | 90 (84.9) |
|
| Histological
type |
|
Serous | 74 | 13 (17.6) | 61 (82.4) |
|
|
Mucinous | 17 | 5 (29.4) | 12 (70.6) |
|
| Clear
cell | 9 | 2 (22.2) | 7 (77.8) |
|
|
Endometrioid | 29 | 7 (24.1) | 22 (75.9) |
|
| Serous
vs. non-serous |
|
|
| 0.278 |
| Ascites, ml |
|
|
| 0.129 |
|
<100 | 46 | 13 (28.3) | 33 (71.7) |
|
|
>100 | 83 | 14 (16.9) | 69 (83.1) |
|
| Residual disease,
cm |
|
|
|
0.438 |
|
<1 | 103 | 23 (22.3) | 80 (77.7) |
|
|
>1 | 26 | 4 (15.4) | 22 (84.6) |
|
Immunohistochemistry
Tumor tissues were fixed in 10% neutral-buffered
formalin for 24 h at room temperature, embedded in paraffin.
Immunohistochemical analysis of NHE1 was conducted on 4-µm-thick
formalin-fixed paraffin-embedded specimens. The slides were
deparaffinized in xylene and rehydrated in graded solutions of
alcohol. Antigen retrieval was performed by treating the sections
with citric acid (pH 6.0) for 20 min. Non-specific proteins were
blocked by incubating the slides with 5% bovine serum albumin
(Beyotime Institute of Biotechnology, Haimen, China) for 30 min at
room temperature. The sections were then incubated overnight at 4°C
with a primary rabbit polyclonal antibody against human NHE1 (1:100
dilution; cat. no. ab67314; Abcam, Cambridge, MA, USA). Next, the
slides were incubated with the appropriate biotinylated secondary
antibody for 30 min at 37°C. Following washing, the slides were
incubated with strepavidin-biotin complex reagent (SA1022, Boster
Biological Technology, Pleasanton, CA, USA) followed by development
with 3,3′-diaminobenzidine solution.
All tissue sections were randomly evaluated by two
independent blinded pathologists, Dr Rui Chen and Dr Jue Xiao, from
the Departments of Pathology, Chongqing University Cancer Hospital
and Institute and Cancer Center (Chongqing, China) . NHE1
expression in EOC was evaluated using an inverted microscope by
scanning the entire tissue specimen under low magnification
(magnification, ×40), and was confirmed under high magnification
(magnification, ×200). NHE1 staining was predominantly localized
within the membrane and cytoplasm. Immunostaining for NHE1 was
scored using a semiquantitative scale through the evaluation of the
staining intensity (0, absent; 1, weak; 2, moderate; 3, strong) and
the proportion of positive tumor cells (0, absent; 1, <33%; 2,
33–66%; 3, >66%). The staining intensity score was multiplied by
the percentage score to obtain the total score (0, 1, 2, 3, 4, 6
and 9). Scores between 0 and 4 were defined as low NHE1 expression,
whereas scores between 6 and 9 were defined as high NHE1
expression.
Cell culture
Distinct tumor-derived human ovarian cancer cell
lines (OVCAR-3, 3AO, SKOV3 and A2780) were used in the present
study. OVCAR-3 (serous) and 3AO (mucinous) were purchased from the
Chinese Academy of Sciences Type Culture Collection (Shanghai,
China). SKOV3 (papillary serous) and A2780 (adenocarcinoma) were
kindly provided by Dr Hua Linghu (Department of Obstetrics and
Gynecology, The First Affiliated Hospital of Chongqing Medical
University, Chongqing, China) and West China Second Hospital
(Sichuan University, Chengdu, China), respectively. All cell lines
were cultured as monolayers in RPMI-1640 medium (Thermo Fisher
Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal
bovine serum (GE Healthcare Life Sciences, Logan, UT, USA) and 1%
penicillin/streptomycin (Beyotime Institute of Biotechnology) at
37°C in a humidified incubator containing 5% CO2.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was isolated with TRIzol reagent (TaKaRa
Bio, Inc., Otsu, Japan), according to the manufacturer's protocol.
In total, 1 µg RNA was reverse-transcribed into cDNA using the
PrimeScript II First Strand cDNA Synthesis kit (Takara Bio, Inc.),
according to the manufacturer's protocols. qPCR was performed in a
CFX96™ Real-Time PCR Detection system (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) with a SYBR® PrimeScript®
RT-PCR kit (TaKaRa Bio, Inc.). The PCR thermocycling conditions
were 95°C for 30 sec followed by 40 cycles at 95°C for 5 sec and
60°C for 30 sec.
The following primers were used: Human NHE1 forward
5′-GCCTTCTCTCTGGGCTACCT-3′ and reverse 5′-CTTGTCCTTCCAGTGGTGGT-3′;
human GAPDH forward 5′-AATGTCCCAGAGTGTGCCGAG-3′ and reverse
5′-ATGCCTTGCCGACCGTGTA-3′. GAPDH was used as a reference gene. qPCR
results were quantified according to the 2−ΔΔCq method
(20).
Western blotting
Western blotting was performed as previously
described (21). Briefly, frozen
tissue samples and cell lines were homogenized on ice in
radioimmunoprecipitation assay lysis buffer (cat. no., P0013B,
Beyotime Institute of Biotechnology) consisting of 50 mM Tris/HCl
(pH 7.4), 150 mM NaCl, 1% Triton X-100, 1% sodium deoxycholate,
0.1% SDS, and protease inhibitor mixture, including sodium
orthovanadate, sodium fluoride, EDTA and leupeptin. The samples
were then centrifuged at 12,000 × g at 4°C for 10 min to remove
cellular debris. Following quantification of the protein extracts
using bicinchoninic acid protein assay, equivalent amounts of
protein (50 µg/lane) was loaded onto 10% acrylamide gels for
SDS-PAGE and then electrotransferred onto a polyvinylidene
difluoride membrane (Merck KGaA, Darmstadt, Germany). The membrane
was blocked with 5% non-fat dry milk in Tris-buffered saline
containing 0.1% Tween-20 for 1 h at 37°C, which was followed by
incubation with a primary rabbit polyclonal antibody against human
NHE1 (dilution, 1:1,000; cat. no., ab67314; Abcam) and a mouse
monoclonal antibody against human GAPDH (dilution, 1:1,000; cat.
no., AG019; Beyotime Institute of Biotechnology) at 4°C overnight.
Subsequent to washing, the membranes were incubated with secondary
antibodies, horseradish peroxidase (HRP)-labeled Goat Anti-Rabbit
IgG (dilution, 1:1,000; cat. no. A0208; Beyotime Institute of
Biotechnology) and HRP-labeled Goat Anti-Mouse (dilution, 1:1,000;
cat. no., A0216; Beyotime Institute of Biotechnology) for 1 h at
37°C. The immunoreactivity was detected using enhanced
chemiluminescence plus detection reagents (P0018; Beyotime
Institute of Biotechnology). GAPDH served as the loading
control.
Immunofluorescence
Cells were plated on sterilized coverslips in a
24-well plate (2×104 cells/ml) and allowed to adhere for
24 h. The cells were fixed in 4% paraformaldehyde at room
temperature for 20 min, followed by permeabilization with 1%
Triton-X-100 at 37°C for 10 min. The cells were blocked with 5%
normal goat serum at 37°C for 30 min and were then incubated with
the rabbit anti-NHE1 antibody (1:100) at 4°C overnight.
Subsequently, the cells were incubated with anti-rabbit FITC
conjugated secondary antibody (dilution, 1:500; cat. no., ab6717;
Abcam, Cambridge, MA, USA) at 37°C for 1 h, and propidium iodide
was used to label the nuclei. Finally, fluorescence images were
captured using a laser-scanning confocal microscope.
Statistical analysis
SPSS software was used for statistical analysis
(version 17.0; SPSS, Inc., Chicago, IL, USA). For continuous
variables, the data are presented as the mean ± standard deviation
and an independent Student's t-test was performed. The association
between NHE1 immunohistochemical staining and the
clinicopathological features was analyzed using the Mann-Whitney U
test. Survival rates were analyzed using the Kaplan-Meier estimator
method, and the difference in survival rates between patients whose
tumors demonstrated high and low NHE1 expression was determined
using a log-rank test. A multivariate analysis of survival rates
was performed using the Cox's hazard model. All tests were
two-tailed, and P<0.05 was considered to indicate a
statistically significant difference.
Results
NHE1 is overexpressed in patients with
EOC
To investigate the effect of NHE1 on the
determination of the clinical prognosis of patients with EOC, the
expression of NHE1 in 184 paraffin-embedded tissue samples was
detected. Immunohistochemical assays revealed that NHE1 was
primarily localized within the cytomembrane and the cytoplasm of
EOC tissue samples. High expression of NHE1 was revealed in 102/129
(79.7%) EOC tissues compared with only 5/18 (27.8%) borderline
tumor tissues (P<0.01), 7/22 (31.8%) benign tumor tissues
(P<0.01) and 4/15 (26.7%) normal ovarian tissues (P<0.01;
Fig. 1A). Furthermore,
immunohistochemical assays also revealed high expression of NHE1 in
samples that represented four different histological types
including serous, mucinous, clear cell and endometrioid tumors
(Fig. 1B). No difference was observed
among histological types with respect to NHE1 protein expression
(P>0.05; Table I).
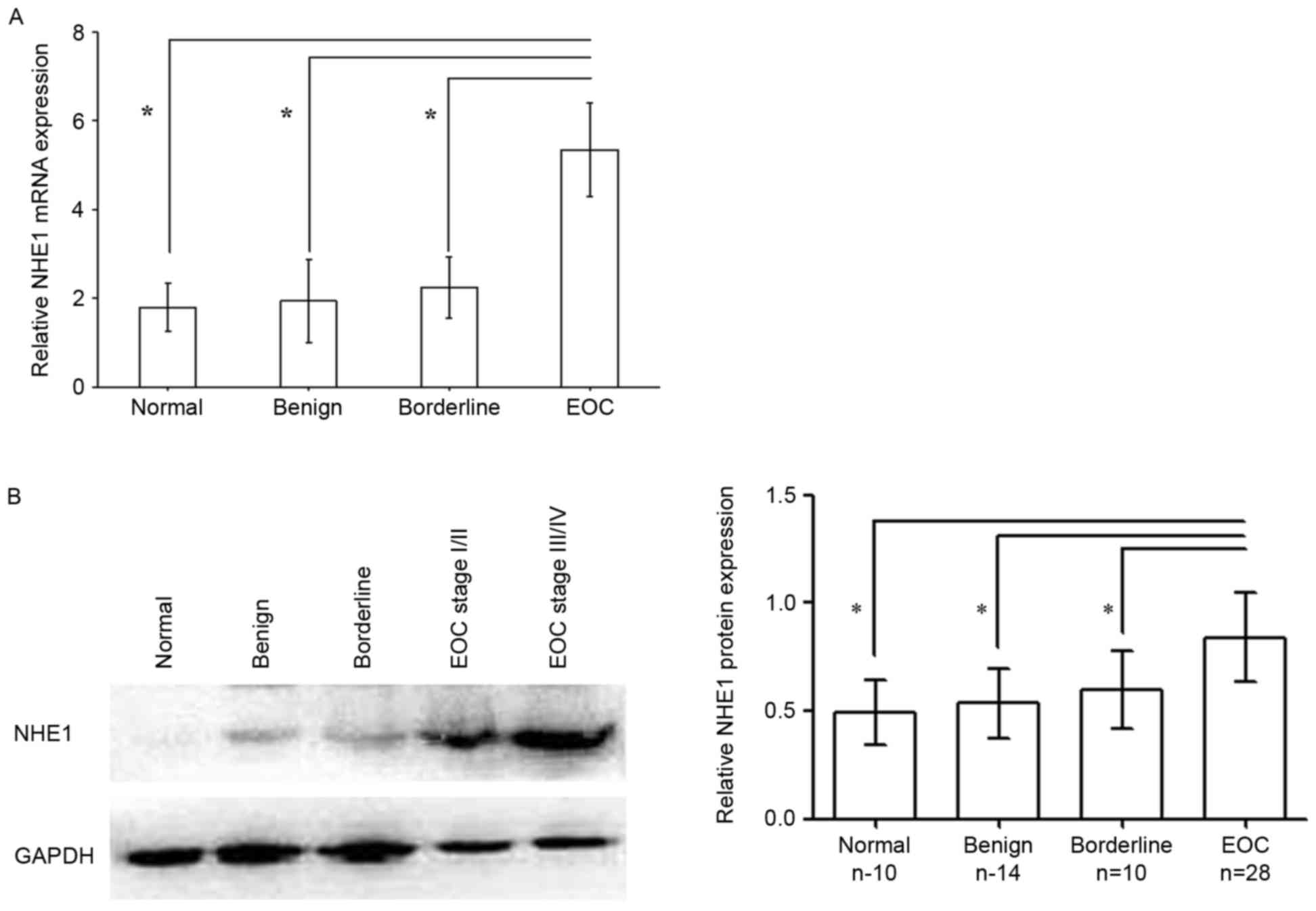
The increased expression of NHE1 was also confirmed
in an additional 28 frozen EOC tissues using RT-qPCR and western
blotting. The relative expression of NHE1 mRNA in EOC tissues
(5.348±1.054) was increased compared with that in the borderline
tumor tissues (2.242±0.683; P<0.01), benign tumor tissues
(1.936±0.932; P<0.01) and normal ovarian tissues (1.794±0.539;
P<0.01; Fig. 2A). The levels of
NHE1 protein were also significantly increased in EOC tissues
(0.841±0.208) compared with borderline tumors (0.598±0.182;
P=0.002), benign tumors (0.534±0.164; P<0.01) and normal ovarian
tissues (0.494±0.149; P<0.01; Fig.
2B).
Increased expression of NHE1 is
associated with tumor progression
To further explore the clinicopathological features
of NHE1-positive tumors, the relevance between the level of NHE1
protein and specific clinicopathological features [including age at
diagnosis, serum cancer antigen (CA)-125 level, FIGO stage, grade,
histological type, ascites and residual disease] in 129 EOC samples
was evaluated. As presented in Table
I, NHE1 immunoreactivity was significantly increased in samples
with FIGO stage III/IV (FIGO stage III/IV vs. I/II; P<0.001) and
high-grade carcinoma (grade 2–3 vs. grade 1; P<0.001). No
association between NHE1 protein expression and age at diagnosis,
serum CA-125 level, histological type, presence of ascites or
residual disease was identified.
NHE1 is expressed in the major
subtypes of human EOC-derived cell lines
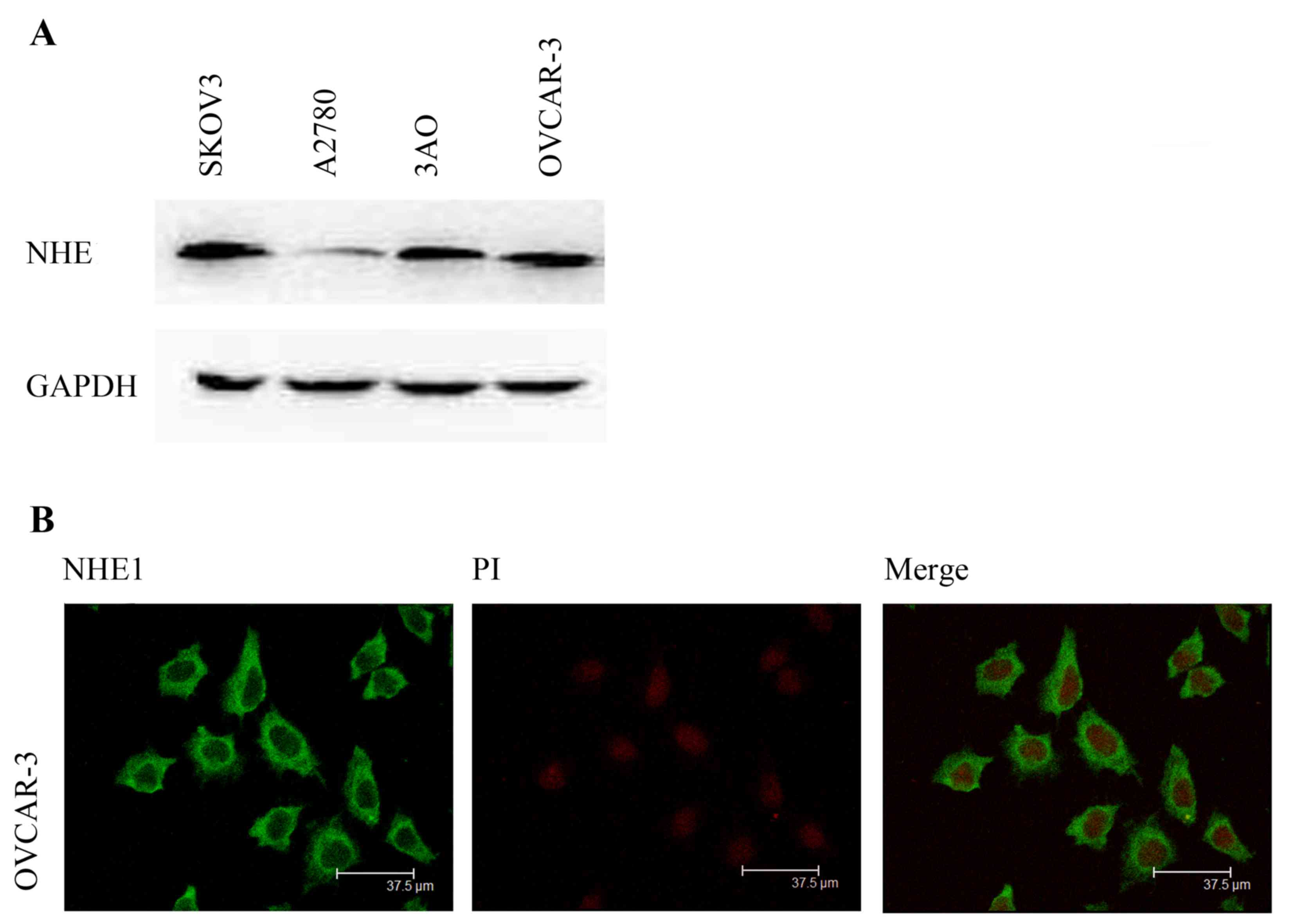
Considering that the immunohistochemistry results
demonstrated increased expression of NHE1 in human EOC tissues, the
level of NHE1 protein was analyzed in various EOC cell lines using
western blotting. The results revealed that NHE1 was highly
expressed at various levels in SKOV3, OVCAR-3, A2780 and 3AO cells
(Fig. 3A). Next, the localization of
NHE1 was also examined in OVCAR-3 cells using immunofluorescence,
and the results revealed that NHE1 was localized predominantly
within the cytomembrane and the cytoplasm (Fig. 3B).
Increased expression of NHE1 predicts
poor prognosis in EOC
The association of NHE1 overexpression with the
clinical prognosis of 129 patients with EOC was analyzed. Following
a 5-year follow-up, the survival rates of patients whose tumors
expressed low and high levels of NHE1 were 74.1 and 36.3%,
respectively. To assess whether NHE1 may serve as a predictor of
survival rate in EOC, a Kaplan-Meier estimator analysis was
performed to explore the association between the level of NHE1
expression and patient survival rate. The log-rank test revealed
that patients with high expression of NHE1 had a shorter PFS/OS
than those with low expression of NHE1 (Fig. 4A and B). According to a univariate
analysis, high expression of NHE1 was associated with a shorter OS
[hazard ratio (HR), 4.212; 95% confidence interval, 1.922–9.230;
P<0.001] in EOC (Table II).
According to a multivariate survival rate analysis, NHE1 remained a
significant factor when age, serum CA-125 level, FIGO stage, grade,
histological type, presence of ascites and residual disease were
used as covariates (HR, 0.402; 95% confidence interval,
0.173–0.993; P=0.034; Table II).
 | Table II.Univariate and multivariate analyses
of the factors that affect the overall survival rate of patients
with endothelial ovarian cancer. |
Table II.
Univariate and multivariate analyses
of the factors that affect the overall survival rate of patients
with endothelial ovarian cancer.
|
| n | Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|---|
| Clinicopathological
parameters | n=129 | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age, years |
|
<50 | 61 | Reference |
| Reference |
|
|
>0 | 68 | 1.023
(0.643–1.627) | 0.925 | 1.435
(0.848–2.428) | 0.178 |
| Serum CA-125,
U/ml |
|
<35 | 17 | Reference |
| Reference |
|
|
>35 | 112 | 0.794
(3.739–23.249) | 0.483 | 1.159
(0.499–2.693) | 0.731 |
| FIGO stage |
|
I/II | 37 | Reference |
| Reference |
|
|
III/IV | 92 | 9.324
(3.739–23.249) |
<0.001a | 0.117
(0.045–0.036) |
<0.001a |
| Grade |
| G1 | 23 | Reference |
| Reference |
|
|
G2/G3 | 106 | 14.339
(3.495–58.824) |
<0.001a | 0.082
(0.019–0.351) | 0.001a |
| Histological
type |
|
Serous | 74 | Reference |
| Reference |
|
| Serous
vs. non-serous | 55 | 1.033
(0.645–1.656) | 0.892 | 0.591
(0.321–1.087) | 0.091 |
| Ascites, ml |
|
<100 | 46 | Reference |
| Reference |
|
|
>100 | 83 | 1.058
(0.651–1.721) | 0.819 | 1.875
(0.965–3.645) | 0.064 |
| Residual tumor,
cm |
|
<1 | 103 | Reference |
| Reference |
|
|
>1 | 26 | 1.889
(1.100–3.276) |
0.021a | 0.594
(0.332–1.063) | 0.079 |
| NHE1
expression |
|
Low | 27 | Reference |
| Reference |
|
|
High | 102 | 4.212
(1.922–9.230) |
<0.001a | 0.402
(0.173–0.993) |
0.034a |
Discussion
The ability to alter the pH is a characteristic of
tumor cells. In vivo and in vitro experiments have
demonstrated that tumor cells exhibit an alkaline pHi (7.12–7.65 in
tumor cells vs. 6.99–7.20 in normal tissues) and an acidic
extracellular pH (pHe; 6.2–6.9 vs. 7.3–7.4) (9). The acidic tumor microenvironment is
hypothesized to accelerate extracellular matrix remodeling, which
results in metastasis (22). NHE1, as
an isoform of the Na+/H+ exchanger family
(comprising NHE1-NHE9), has been detected in the plasma membrane of
epithelial cells and has been demonstrated to be a crucial
regulator of pHi and pHe via ion exchange (23).
Previous studies indicate that the overexpression of
the NHE1 protein and the dysregulation of NHE1 activity are
associated with tumor malignancy (24,25). To
the best of our knowledge, the association between NHE1 and
metastasis has not previously been investigated in EOC. The present
study explored the expression pattern and prognostic effect of NHE1
in epithelial ovarian tumors of different pathological types and
normal ovarian tissues.
The results of the present study revealed that
abundant NHE1 protein expression was markedly detected in the
cytomembrane and cytoplasm of cancer cells. Furthermore, increased
levels of NHE1 mRNA and protein expression were detected in EOC
tissues, but not in borderline tumor tissues, benign tumor tissues
or normal ovarian tissues. Such results are similar to those of
previous studies of NHE1 in breast cancer (12,13),
hepatoma (14,15) and glioblastoma (26,27). The
possible association between the NHE1 expression pattern and the
specific clinicopathological features of patients with EOC was also
analyzed. The results revealed that an increased level of NHE1
expression was associated with advanced FIGO stage and high-grade
carcinoma. However, no association was identified between the NHE1
expression pattern and age at diagnosis, serum CA-125 level,
histological type, presence of ascites or residual disease. These
results suggest that NHE1 may serve an essential role in the
development of the transformed phenotype of cancer cells during
tumorigenesis. Various studies have investigated the role of NHE1
in the migration and invasiveness of malignant tumors in
vitro. NHE1 activation in the MDA-MB-435 breast cancer cell
line, which is a well-characterized human mammary epithelial cell
line that represents late-stage metastatic progression, led to
morphological and cytoskeletal changes with increased chemotaxis
and cell invasion (28). Furthermore,
in MDA-MB-435 breast cancer cells (29) and pancreatic ductal adenocarcinoma
cells (16), the inhibition of NHE1
decreased growth and invasive behavior, and during the
administration of chemotherapeutic drugs, the antineoplastic
effects of those drugs were synergistically strengthened. In
summary, it was concluded that the dysregulation of NHE1 may be
responsible for the invasive and metastatic behavior of EOC.
Consistent with the results that were obtained from
human EOC tissues, the four EOC cell lines examined in the present
study exhibited increased levels of NHE1 protein, and according to
immunofluorescence assays, the immunoreactivity of NHE1 protein was
also localized to the cytomembrane and cytoplasm of ovarian cancer
cells. A previous study revealed that NHE1 protein was colocalized
with ezrin within lamellipodia and that this protein is possibly
associated with the migration of glioma cells (26). It was speculated that the location of
NHE1 protein may be connected with the invasiveness and metastasis
of EOC cells.
Previous studies have identified a prognostic role
for NHE1 protein in malignant tumors (12,13,15,16,26,27,30).
The present study investigated the predictive value of NHE1 protein
expression in the clinical prognosis of patients with EOC. The
results revealed that patients with a high level of NHE1 expression
experienced a shorter PFS/OS compared with those with a low level
of NHE1 expression. Furthermore, high-grade carcinoma, advanced
FIGO stage and suboptimal cytoreductive surgery (residual disease
≥1 cm) were also significantly associated with an increased risk of
a poor outcome.
Additionally, a multivariate Cox's regression
analysis revealed that NHE1, FIGO stage and carcinoma grade were
independent prognostic factors for the prediction of outcomes of
patients with EOC. These results suggest that NHE1 may serve as a
potential biomarker for the development of EOC. Owing to the
relatively small sample size in the present study, further in-depth
studies are required to confirm the predictive value of NHE1
protein in EOC.
In summary, the results of the present study
revealed that increased expression of NHE1 was identified in EOC
tissues and that the overexpression of NHE1 was associated with
increased serum CA-125, advanced FIGO stage and high-grade
carcinoma. Furthermore, the results indicate that NHE1 may be an
independent predictor and risk factor for unfavorable outcome in
patients with EOC. These results suggest that a high expression of
NHE1 may be an unfavorable prognostic marker of EOC and that NHE1
may serve as a potential therapeutic target for the inhibition of
tumor aggressiveness.
Acknowledgements
The authors would like to thank Dr Ming Xiao
(Department of Pathology, The First Affiliated Hospital of
Chongqing Medical University, Chongqing, China) for assessing the
slides, Dr Hua Linghu (Department of Obstetrics and Gynecology, The
First Affiliated Hospital of Chongqing Medical University) for
providing the SKOV3 cells and the Chongqing Key Laboratory of
Oncology at Chongqing Cancer Institute (Chongqing, China) for the
experimental supplies. The present study was funded by Chongqing
Science & Technology Commission (grant no. cstc 2015jcyjBX0137)
and Chongqing Human Resources Social and Security Bureau (grant no.
Xm2015084).
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EOC
|
epithelial ovarian cancer
|
|
NHE1
|
Na+/H+ exchanger
isoform 1
|
|
FIGO
|
the International Federation of
Gynecology and Obstetrics
|
|
PFS
|
progression-free survival
|
|
OS
|
overall survival
|
References
|
1
|
American Cancer Society: Cancer Facts
& Figures, . American Cancer Society. http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdfMarch
21–2016
|
|
2
|
Oza AM, Cook AD, Pfisterer J, Embleton A,
Ledermann JA, Pujade-Lauraine E, Kristensen G, Carey MS, Beale P,
Cervantes A, et al: Standard chemotherapy with or without
bevacizumab for women with newly diagnosed ovarian cancer (ICON7):
overall survival results of a phase 3 randomised trial. Lancet
Oncol. 16:928–936. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aghajanian C, Goff B, Nycum LR, Wang YV,
Husain A and Blank SV: Final overall survival and safety analysis
of OCEANS, a phase 3 trial of chemotherapy with or without
bevacizumab in patients with platinum-sensitive recurrent ovarian
cancer. Gynecol Oncol. 139:10–16. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Perren TJ, Swart AM, Pfisterer J,
Ledermann JA, Pujade-Lauraine E, Kristensen G, Carey MS, Beale P,
Cervantes A, Kurzeder C, et al: A phase 3 trial of bevacizumab in
ovarian cancer. N Engl J Med. 365:2484–2496. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aghajanian C, Blank SV, Goff BA, Judson
PL, Teneriello MG, Husain A, Sovak MA, Yi J and Nycum LR: OCEANS: A
randomized, double-blind, placebo-controlled phase III trial of
chemotherapy with or without bevacizumab in patients with
platinum-sensitive recurrent epithelial ovarian, primary
peritoneal, or fallopian tube cancer. J Clin Oncol. 30:2039–2045.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stockler MR, Hilpert F, Friedlander M,
King MT, Wenzel L, Lee CK, Joly F, de Gregorio N, Arranz JA, Mirza
MR, et al: Patient-reported outcome results from the open-label
phase III AURELIA trial evaluating bevacizumab-containing therapy
for platinum-resistant ovarian cancer. J Clin Oncol. 32:1309–1316.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Oza AM, Cibula D, Benzaquen AO, Poole C,
Mathijssen RH, Sonke GS, Colombo N, Špaček J, Vuylsteke P, Hirte H,
et al: Olaparib combined with chemotherapy for recurrent
platinum-sensitive ovarian cancer: A randomised phase 2 trial.
Lancet Oncol. 16:87–97. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu JF, Barry WT, Birrer M, Lee JM,
Buckanovich RJ, Fleming GF, Rimel B, Buss MK, Nattam S, Hurteau J,
et al: Combination cediranib and olaparib versus olaparib alone for
women with recurrent platinum-sensitive ovarian cancer: A
randomised phase 2 study. Lancet Oncol. 15:1207–1214. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gillies RJ, Raghunand N, Karczmar GS and
Bhujwalla ZM: MRI of the tumor microenvironment. J Magn Reson
Imaging. 16:430–450. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Loo SY, Chang MK, Chua CS, Kumar AP,
Pervaiz S and Clement MV: NHE-1: A promising target for novel
anti-cancer therapeutics. Curr Pharm Des. 18:1372–1382. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Amith SR and Fliegel L: Regulation of the
Na+/H+ exchanger (NHE1) in breast cancer metastasis. Cancer Res.
73:1259–1264. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Amith SR, Wilkinson JM, Baksh S and
Fliegel L: The Na+/H+ exchanger (NHE1) as a
novel co-adjuvant target in paclitaxel therapy of triple-negative
breast cancer cells. Oncotarget. 6:1262–1275. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lin Y, Chang G, Wang J, Jin W, Wang L, Li
H, Ma L, Li Q and Pang T: NHE1 mediates MDA-MB-231 cells invasion
through the regulation of MT1-MMP. Exp Cell Res. 317:2031–2040.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yang X, Wang D, Dong W, Song Z and Dou K:
Suppression of Na+/H+ exchanger 1 by RNA interference or amiloride
inhibits human hepatoma cell line SMMC-7721 cell invasion. Med
Oncol. 28:385–390. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang X, Wang D, Dong W, Song Z and Dou K:
Expression and modulation of Na(+) /H(+) exchanger 1 gene in
hepatocellular carcinoma: A potential therapeutic target. J
Gastroenterol Hepato. 26:364–370. 2011. View Article : Google Scholar
|
|
16
|
Cardone RA, Greco MR, Zeeberg K,
Zaccagnino A, Saccomano M, Bellizzi A, Bruns P, Menga M, Pilarsky
C, Schwab A, et al: A novel NHE1-centered signaling cassette drives
epidermal growth factor receptor–dependent pancreatic tumor
metastasis and is a target for combination therapy. Neoplasia.
17:155–166. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lin Y, Wang J, Jin W, Wang L, Li H, Ma L,
Li Q and Pang T: NHE1 mediates migration and invasion of HeLa cells
via regulating the expression and localization of MT1-MMP. Cell
Biochem Funct. 30:41–46. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jin W, Li Q, Wang J, Chang G, Lin Y, Li H,
Wang L, Gao W and Pang T: Na+/H+ exchanger 1 inhibition contributes
to K562 leukaemic cell differentiation. Cell Biol Int. 36:739–745.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tang L, Yang J, Ng SK, Rodriguez N, Choi
PW, Vitonis A, Wang K, McLachlan GJ, Caiazzo RJ Jr, Liu BC, et al:
Autoantibody profiling to identify biomarkers of key pathogenic
pathways in mucinous ovarian cancer. Eur J Cancer. 46:170–179.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang H, Mu X, Zhou S, Zhang J, Dai J, Tang
L, Xiao L, Duan Z, Jia L and Chen S: NEDD9 overexpression is
associated with the progression of and an unfavorable prognosis in
epithelial ovarian cancer. Hum Pathol. 45:401–408. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Greco MR, Antelmi E, Busco G, Guerra L,
Rubino R, Casavola V, Reshkin SJ and Cardone RA: Protease activity
at invadopodial focal digestive areas is dependent on NHE1-driven
acidic pHe. Oncol Rep. 31:940–946. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Maly K, Strese K, Kampfer S, Ueberall F,
Baier G, Ghaffari-Tabrizi N, Grunicke HH and Leitges M: Critical
role of protein kinase C alpha and calcium in growth factor induced
activation of the Na+/H+ exchanger NHE1. FEBS Lett. 521:205–210.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cardone RA, Casavola V and Reshkin SJ: The
role of disturbed pH dynamics and the Na+/H+ exchanger in
metastasis. Nat Rev Cancer. 5:786–795. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Stock C, Ludwig FT and Schwab A: Is the
multifunctional Na(+)/H(+) exchanger isoform 1 a potential
therapeutic target in cancer? Curr Med Chem. 19:647–660. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cong D, Zhu W, Shi Y, Pointer KB, Clark
PA, Shen H, Kuo JS, Hu S and Sun D: Upregulation of NHE1 protein
expression enables glioblastoma cells to escape TMZ-mediated
toxicity via increased H+ extrusion, cell migration and
survival. Carcinogenesis. 35:2014–2024. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhu W, Carney KE, Pigott VM, Falgoust LM,
Clark PA, Kuo JS and Sun D: Glioma-mediated microglial activation
promotes glioma proliferation and migration: Roles of Na+/H+
exchanger isoform 1. Carcinogenesis. 37:839–851. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Paradiso A, Cardone RA, Bellizzi A,
Bagorda A, Guerra L, Tommasino M, Casavola V and Reshkin SJ: The
Na+-H+ exchanger-1 induces cytoskeletal
changes involving reciprocal RhoA and Rac1 signaling, resulting in
motility and invasion in MDA-MB-435 cells. Breast Cancer Res.
6:R616–R628. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
29
|
Reshkin SJ, Bellizzi A, Cardone RA,
Tommasino M, Casavola V and Paradiso A: Paclitaxel induces
apoptosis via protein kinase A- and p38 mitogen-activated
protein-dependent inhibition of the Na+/H+ exchanger (NHE) NHE
isoform 1 in human breast cancer cells. Clin Cancer Res.
9:2366–2373. 2003.PubMed/NCBI
|
|
30
|
Ariyoshi Y, Shiozaki A, Ichikawa D,
Shimizu H, Kosuga T, Konishi H, Komatsu S, Fujiwara H, Okamoto K,
Kishimoto M, et al: Na+/H+ exchanger 1 has tumor suppressive
activity and prognostic value in esophageal squamous cell
carcinoma. Oncotarget. 8:2209–2223. 2017. View Article : Google Scholar : PubMed/NCBI
|