Introduction
Mixed germ cell tumors consist of ≥2 types of germ
cells and usually occur in the gonads, with rare occurrences in the
mediastinum (1). The most common
combination observed is that of astrocytoma and yolk sac tumor
derived from primordial germ cells of the embryonic gonads. To the
best of our knowledge, only one case of spontaneous rupture and
bleeding in mediastinal mixed germ cell tumor has been reported.
Typically, these tumors consist of a combination of two cell types
(1,2), and a single case involving three cell
types has been reported, including yolk sac tumor, immature
teratoma and a small amount of embryonal carcinoma (3). However, there have been no reports of
mixed germ cell tumor with >4 cell types. To the best of our
knowledge, the present study is the first to report a mediastinal
mixed germ cell tumor presenting with these four pathological
types, including embryonal carcinoma, seminoma, yolk sac tumor and
immature teratoma. Mixed mediastinal germ cell tumors can
spontaneously rupture and bleed, leading to hemothorax (1). Emergency thoracotomy is commonly
considered for treatment, but the prognosis remains poor (3). Upon reviewing the literature, only one
related report where the patient had a fair prognosis following
surgical treatment was identified (1). However, the patient of the present
report experienced a poor prognosis post-surgery; their vital signs
and laboratory tests, including hemoglobin levels, showed no marked
abnormalities upon admission. Additionally, surgery might
accelerate tumor progression. It was hypothesized that conservative
treatment as an initial approach was a viable option under these
circumstances. The current report presents the approach adopted for
the treatment of a 20-year-old male patient with mixed germ cell
tumor aiming to provide references for the treatment of similar
diseases in the future.
Case report
In February, 2021, a 20-year-old male patient was
admitted to The Affiliated Hospital of Guizhou Medical University
(Guiyang, China) with complaints of cough and expectoration for
>20 days, chest tightness and shortness of breath for >1
week. The patient had started coughing and expectorating copious
amounts of yellow-white purulent sputum without any apparent cause
>20 days prior to admission. The patient underwent a thoracic
computed tomography (CT) scan at Fuquan City People's Hospital
(Fuquan, China) in January, 2021, which revealed an anterior
superior mediastinal mass, suggestive of thymoma with a likelihood
of malignancy, accompanied by a small amount of right-sided pleural
effusion. Subsequently, the patient was transferred to The Third
Affiliated Hospital of Guizhou Medical University (Guizhou, China)
for further diagnosis and treatment in January, 2021. At that
point, the patient presented with chest tightness, shortness of
breath and difficulty breathing, considered to be secondary to
tumor compression. A repeat of thoracic CT showed mediastinal
occupation and extensive right-sided pleural effusion. These CT
images were performed at Fuquan City People's Hospital and The
Third Affiliated Hospital of Guizhou Medical University, therefore
only the report results were provided by the patient. Thoracic
cavity puncture and tube drainage were performed, resulting in the
extraction of a moderate amount of bloody fluid which alleviated
the symptoms of dyspnea. Due to the severity of the patient's
condition, and at the request of the patient and their family, the
patient was urgently transferred to The Affiliated Hospital of
Guizhou Medical University with the initial diagnosis of
‘mediastinal occupation’. The patient reported no family history of
genetic or infectious diseases, or prior surgeries. Physical
examination revealed a slight leftward deviation of the trachea,
fullness in the right thorax and widened intercostal spaces. The
chest wall was non-tender, the left voice tremor was diminished and
there was no pleural friction. While the respiratory sound in the
left lung was clear, it was absent in the right lung. No bulging in
the precordial area, normal cardiac borders, strong heart sounds, a
heart rate of 95 beats/min and no pathological murmurs over the
valve auscultation areas were observed. After admission, laboratory
test results showed that the red blood cell count was
3.83×1012 cells/l [healthy adult range,
(3.5–5.5)x1012 cells/l], and the hemoglobin level was
116.00 g/l (healthy adult range, 130–175 g/l); however, the
platelet count was 523.00 cells/l [healthy adult range,
(125–300)x1012 cells/l], the fibrinogen level was 6.08
g/l (healthy adult range, 2–4 g/l), the D-Dimer level was 7.8 µg/ml
(healthy adult range, 0–1 µg/ml) and the bicarbonate radical level
was 27.00 mmol/l (healthy adult range, 1.3–24.8 mmol/l). The levels
of sodium, calcium, urea, creatinine, uric acid, total protein,
albumin, cholinesterase, prealbumin and creatine kinase were
slightly lower, but erythrocyte sedimentation rate, N-terminal
pro-brain natriuretic peptide, activated partial thromboplastin
time, fibrinogen, D-Dimer and fibrin (fibrinogen) degradation
product were slightly higher (Table
I). The red blood cell count and hemoglobin levels both
decreased immediately after surgery and gradually increased from
day 3 after surgery. It is noteworthy that postoperative myoglobin
levels increased to 2066.00 ng/ml (healthy adult range, 28.00–72.00
ng/ml). However, D-Dimer levels decreased gradually after
operation. The changes in laboratory tests and clinical parameters
during the hospital stay are shown in Table II. Upon arrival at The Affiliated
Hospital of Guizhou Medical University, a contrast-enhanced CT
revealed compression and thinning of the right pulmonary artery,
incomplete expansion of the right lung, moderate hemorrhaging in
the right thorax and slight enlargement of multiple mediastinal
lymph nodes (Fig. 1). Based on the
assessment of the patient, it appeared that the tumor was malignant
and had potentially infiltrated the pericardium, pleura or right
atrium. Emergency surgery was performed to address a hemothorax
caused by a ruptured tumor. Through surgery, it was observed that
the tumor was located in the right anterior superior mediastinum,
measuring ~17.0×15.0×6.0 cm, had a brittle and inactive texture,
easily bleeding upon touch, lacked an integrated envelope. In
addition, the tumor extended downwards along the mediastinum,
invading the right pericardium, middle and lower lobe of the right
lung, phrenic nerve and reaching the anterior border of the spine.
The entire lesion and invaded tissue were removed during surgery.
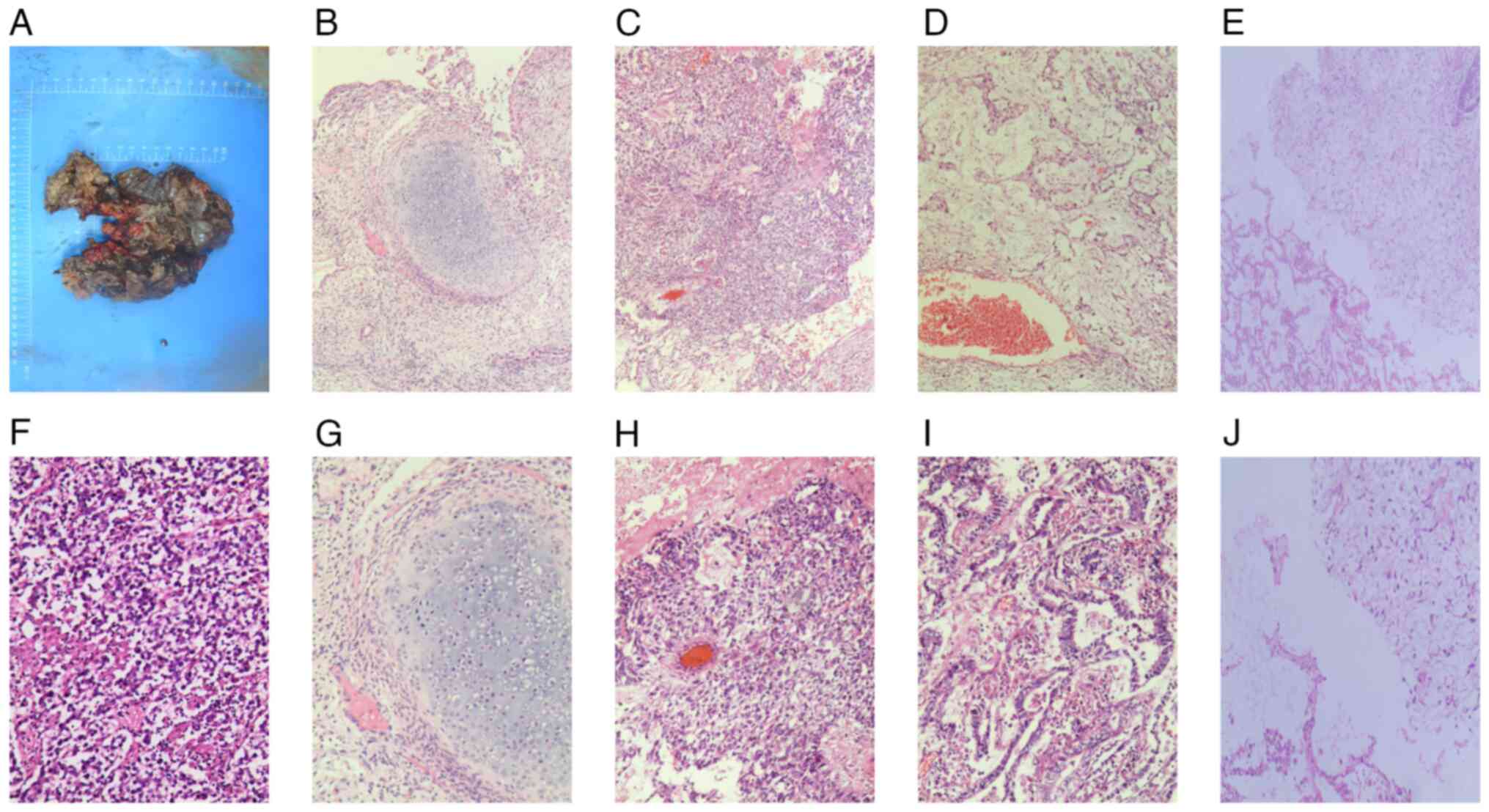
Tissues were stained with hematoxylin and eosin for 3 min at 65°C,
and images were captured under a LEICA DM3000 LED fluorescence
microscope (Leica Microsystems, Inc.). The results revealed that
the lesion was a mixed germ cell tumor consisting of four cell
types: embryonal carcinoma, seminoma, yolk sac tumor and immature
teratoma (Fig. 2). However, the
parents of the patient declined immunohistochemistry. Based on
these pathological features, the pathologist diagnosed the tumor as
mixed germ cell tumor, with ~85% yolk sac tumor, ~10% immature
teratoma, ~3% seminoma and ~2% embryonal carcinoma. No tumor
metastasis was observed in the fibrofatty tissue of the pleural
wall or in the group 11 lymph nodes. However, tumor involvement was
detected in the tissue of the middle and lower lung lobes of the
right lung, indicating metastasis of the tumor (Fig. 2I and J). The postoperative
α-fetoprotein (AFP) level was 1210.00 ng/ml (normal range, 0–7
ng/ml), and the β-human chorionic gonadotropin level was 3.54
mIU/ml (healthy male range, ≤2 mIU/ml). Although these tests were
not conducted before surgery, results are consistent with a
diagnosis of a germ cell tumor. The patient's respiratory distress
gradually improved after surgery, but both red blood cell count and
hemoglobin level markedly dropped on day 10 postoperatively, and a
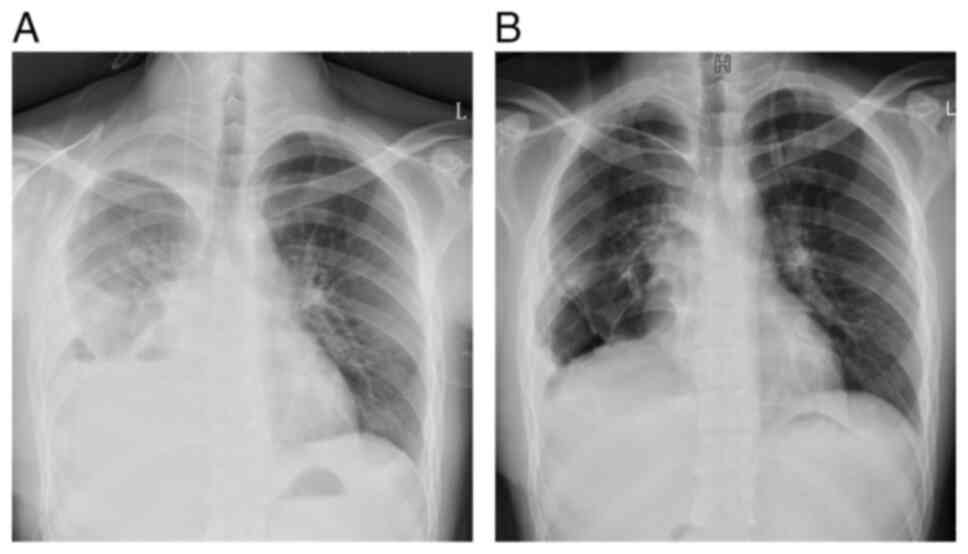
repeat chest radiograph indicated a notable recovery of the chest
cavity (Fig. 3). A positron
emission tomography (PET)/CT scan on day 12 postoperatively
revealed the presence of multiple skeletal metastases throughout
the body. The affected lung tissue had already been removed during
surgery, and therefore PET/CT did not reveal obvious signs of lung
metastasis (Fig. 4). Despite
recommendations for chemotherapy, the patient opted for discharge
on day 17 after surgery. As noted during the follow-up period, the
patient passed away 2 months after discharge in May 2021.
 | Table I.Laboratory examination after admission
hospital test results. |
Table I.
Laboratory examination after admission
hospital test results.
| Indices | Value | Variation | Normal range |
|---|
| RBCs per liter | 3.83 | Down |
(3.5–5.5)x1012 |
| Hemoglobin, g/l | 116 | Down | 130-175 |
| Platelets per
liter | 523 |
Up |
(125–300)x1012 |
| LYM% | 12.1 | Down | 20-50 |
| MON% | 17.1 |
Up | 3-10 |
| SBC, mmol/l | 27 |
Up | 21.3–24.8 |
| ABC, mmol/l | 3.8 |
Up | −3-3 |
| Sodium, mmol/l | 134.7 | Down | 137-147 |
| Calcium, mmol/l | 2.075 | Down | 2.11–2.52 |
| Urea, mmol/l | 2.33 | Down | 3.1–8.0 |
| Creatinine,
µmol/l | 49.62 | Down | 57-97 |
| Uric acid,
µmol/l | 90.5 | Down | 208-428 |
| Total protein,
g/l | 56.45 | Down | 65-85 |
| Albumin, g/l | 29.1 | Down | 40-55 |
| Cholinesterase,
U/l | 3793 | Down | 5,000-12,000 |
| Prealbumin, mg/l | 90 | Down | 200-400 |
| CK, U/l | 29.62 | Down | 50-310 |
| ESR, mm/h | 120 |
Up | 0-21 |
| NT-proBNP, pg/ml | 127.9 |
Up | 20.00–88.00 |
| APTT, sec | 49 |
Up | 28-44 |
| Fibrinogen, g/l | 6.08 |
Up | 2-4 |
| D-Dimer, µg/ml | 7.81 |
Up | 0-1 |
| FDP, µg/ml | 26.55 |
Up | 0-5 |
 | Table II.Changes of clinical indices of the
patient of the present case report. |
Table II.
Changes of clinical indices of the
patient of the present case report.
|
| Pre-surgery | Post-surgery |
|
|---|
|
|
|
|
|
|---|
| Clinical index | Admission to
hospital | Day 1 | Immediately after
operation | Day 1 | Day 3 | Day 7 | Day of
discharge | Normal range |
|---|
| Daily chest
drainage, ml | 50 | 50 | N/A | 10 | 250 | 150 | N/A | N/A |
| Blood pressure,
mmHg | 109/68 | 103/64 | N/A | 117/74 | 104/64 | 77/55 | N/A | 90-139/60-89 |
| Heart rate, beats
per min | 95 | 105 | N/A | 103 | 102 | 78 | N/A | 60-100 |
| White blood cells
per liter | 9.14 | 11.38 | 12.67 | 12.48 | 9.55 | 8.64 | 8.03 |
3.5–9.5×109 |
| Red blood cells per
liter | 3.83 | 3.92 | 3.21 | 2.37 | 2.88 | 2.86 | 3.32 |
3.8–5.1×1012 |
| Hemoglobin,
g/l | 116.00 | 119.20 | 98.00 | 71.00 | 85.00 | 89.00 | 95.00 | 130-175 |
| Platelets per
liter | 532.00 | 508.00 | 290.00 | 305.00 | 482.00 | 539.00 | 484.00 |
(100–300)x109 |
| Calcium,
mmol/l | 2.075 | N/A | 1.885 | 1.985 | 2.13 | N/A | N/A | 2.11–2.52 |
| Albumin, g/l | 29.10 | N/A | 21.80 | 30.10 | 37.50 | N/A | N/A | 40-55 |
| Myoglobin,
ng/ml | 21.00 | N/A | 2066.00 | N/A | N/A | N/A | N/A | 28.00–72.00 |
| hs-CTnT, ng/ml | 0.006 | N/A | 0.04 | N/A | N/A | N/A | N/A | 0.000–0.014 |
| AFP, ng/ml | N/A | N/A | N/A | N/A | N/A | 1210.00 | N/A | 0.00–7.00 |
| β-hCG, mIU/ml | N/A | N/A | N/A | N/A | N/A | 3.54 | N/A | healthy males,
≤2 |
| D-dimer, µg/ml | 7.81 | N/A | 6.52 | 2.23 | N/A | N/A | N/A | 0-1 |
Discussion
The patient of the current report had a tumor
comprising multiple types of germ cells. Spontaneous rupture of
mediastinal mixed germ cell tumors is a rare occurrence and may not
be well recognized by clinicians, and it can lead to hemorrhage and
potentially life-threatening complications. To the best of our
knowledge, there have been no reported cases of spontaneous rupture
and bleeding from a mixed germ cell tumor consisting of four cell
types. In the US, the overall incidence range of extragonadal germ
cell tumors between 1973 and 2007 was 1.8–3.4 cases per 1 million
individuals, with a lower incidence rate reported in females
(4). According to a study by the
Finnish National Cancer Registry, during the period 1969–2008, the
incidence rate of extragonadal mixed germ cell tumor was ~0.18 and
~0.10 per 1 million in men and women, respectively (5). While germ cell tumors are most
commonly seen in gonads, some can occur outside those. Mixed germ
cell tumors usually occur in the midline and can be found anywhere
from the head to the sacrum. The most common location for mixed
germ cell tumors is the anterior mediastinum (50–70% of cases)
(1–4). However, due to the rarity of ruptured
mixed germ cell tumors in the mediastinum, the rate of hemorrhage
associated with them remains unknown. Teratoma and pure seminoma
are the most common histological subtypes of mediastinal mixed germ
cell tumors (3). The exact cause of
mixed germ cell tumors has not yet been confirmed. Previous studies
suggested that the tumor originated from germ cell precursors that
were mistakenly stagnant during midline migration in embryogenesis
(3). Genetic studies have shown
that aneuploidy and chromosome 12 abnormalities are the most common
genetic aberrations observed in post-puberty germ cell tumors
(6–8). Mediastinal mixed germ cell tumors are
considered to arise from germ cells that remain in the anterior
mediastinum. This category encompasses various types of mature
teratomas, yolk sac tumors, immature teratomas, embryonal
carcinomas, choriocarcinomas and mixed germ cell tumors (1). The exact cause of spontaneous rupture
in mixed germ cell tumors is still debated, but it is hypothesized
to be associated with multiple factors such as autolysis,
infection, inflammation, crush necrosis and ischemia (9). Additionally, it has been suggested
that the rapid development of choriocarcinoma within a mixed
mediastinal germ cell tumor may be a contributing factor to tumor
rupture and hemorrhage (1).
Furthermore, chemotherapy might also play a role in precipitating
tumor rupture (10). However, in
the present case, the patient's tumor did not contain
choriocarcinoma components, and no chemotherapy was administered
prior to the rupture. Although the presence of an immature teratoma
in the patient of the current report does not exclude the
possibility of autolysis as an explanation for the ruptured
bleeding, it is noteworthy that Ruan et al suggested that
the presence of a large choriocarcinoma component in mediastinal
mixed germ cell tumors is the most likely cause of tumor rupture
(1). However, the patient of the
current report was not diagnosed with choriocarcinoma.
In terms of histology, mixed germ cell tumors share
the same subtypes as gonadal germ cell tumors, which include
seminoma and non-seminoma. Seminoma is limited to classic seminoma,
while non-seminoma includes embryonic carcinoma, teratoma (mature
or immature), yolk sac carcinoma, choriocarcinoma and mixed germ
cell tumor (8). Among these, mature
teratomas are benign tumors with a good prognosis, while the other
tumors are malignant and have a poor prognosis (8). The clinical manifestations of
mediastinal tumors can vary, ranging from no symptoms to severe
cardiorespiratory problems. These tumors can cause symptoms by
compressing the airways, causing superior vena cava syndrome,
invading the mediastinum directly, obstructing pulmonary blood
vessels, causing pericardial effusion, triggering paraneoplastic
syndrome and compressing the recurrent laryngeal nerve (5). Bokemeyer et al (11) showed that the most common symptoms
of mediastinal tumors are dyspnea (25%), chest pain (23%), cough
(17%) and fever (13%).
The diagnosis of mixed germ cell tumors is often
challenging and is typically diagnosed incidentally when the tumor
compresses adjacent organs, leading to corresponding symptoms. It
is commonly detected during routine diagnosis or treatment,
typically at a late stage. However, a correct and early diagnosis
can improve prognosis. Imaging plays a critical role in the
diagnosis and staging of thymoma, as well as in the follow-up
monitoring of patients with this tumor. Mediastinal lesions are
typically first diagnosed using chest X-ray, CT or echocardiography
(12). The CT imaging of the
patient presented in the current report revealed a tumor in the
right mediastinum with intratumoral hemorrhage, measuring
~17.0×15.0 cm in diameter. The right pulmonary artery was
compressed and attenuated, the right lung was not fully expanded,
there was moderate hemorrhaging in the right thoracic cavity and
multiple mediastinal lymph nodes were mildly enlarged. The actual
size of the tumor post-surgery is shown in Fig. 2A. Due to the emergent nature of the
intraoperative circumstances, cross-sectional images of the tumor
after excision were not captured. This limitation may impede a more
comprehensive understanding of the internal structure and nature of
the tumor. Most mediastinal cystic tumors are initially identified
in ultrasonographic examinations as either unilocular (57.7%) or
multilocular (15.4%) cysts. The cystic fluid displayed mixed
echogenicity (81.1%), with acoustic shadowing observed in 72.2% of
cases. Vascular formation was minimal or absent on color Doppler
imaging, as indicated by color scores of 52.9% and color scoring of
27.1%; additionally, these tumors may exhibit features such as
‘cotton wool tufts’, ‘mushroom cap sign’, ‘completely
hyperechogenic lesion’ and ‘starry sky sign’ (13). Ultrasound examination was not
performed upon admission. Magnetic resonance imaging (MRI) is
considered superior for examining soft tissue as it provides a
better characterization of lesions and their internal tissue
features. Additionally, MRI can identify the invasion of adjacent
structures, making it a useful tool for evaluating mediastinal
masses. MRI can help distinguish uncertain lesions that are not
clearly visible on CT and X-ray images (12–14).
Thymomas typically appear as low signal intensity on T1-weighted
images and high signal intensity on T2-weighted images (14). Mediastinal tumors exhibit increased
metabolic activity on PET-CT scans, which not only serve to
determine the nature of the tumor (benign or malignant), but can
also be used to assess the patient's response to treatment
(14,15). Mixed germ cell tumors exhibit
similar serological, histological and cytogenetic characteristics
as gonadal germ cell tumors (14).
Biochemical serum tumor markers, such as AFP, β-human chorionic
gonadotropin (β-hCG) and lactate dehydrogenase are often found to
be elevated in mixed germ cell tumors (13). AFP levels are typically increased in
non-myxomatous mixed germ cell tumors, but not in patients with
pure seminoma. Conversely, serum AFP levels are raised in patients
with pure yolk sac tumors or mixed germ cell tumors containing yolk
sac tumors. Serum β-hCG levels may also be increased in advanced
disease, regardless of whether it is a pure or non-serous germ cell
tumor. Additionally, the presence of multinucleated
trophoblast-like giant cells in seminiferous microcytomas is
associated with β-hCG production (8). Although AFP and β-hCG levels were not
available for the patient of the current report upon admission,
postoperative examination revealed elevated levels of both markers.
Zhou et al (16) discovered
that terminal deoxynucleotidyl transferase can serve as a novel
tumor marker for diagnosing seminoma, germ cell tumor in
situ, anaplastic cell tumor, embryonal carcinoma and mixed germ
cell tumor with a markedly high positive rate. Furthermore,
research has demonstrated that plasma levels of microRNA-371a-3p
can be used as an indicator for prognostic assessment of germ cell
tumors (17). However, the
histopathological examination remains crucial for the definitive
diagnosis of primary mediastinal mixed germ cell tumors.
Preoperative cytology through percutaneous fine needle biopsy has
emerged as a prevalent approach for diagnosing mediastinal masses.
However, there are instances where the sample obtained from the
core needle biopsy is insufficient for conducting
immunohistochemical experiments (15). Furthermore, Sakane et al
(18) reported a case of
mediastinal mixed germ cell tumor with diffuse lung metastasis
resulting from biopsy, indicating that there is a risk of tumor
metastasis associated with this procedure.
In the past, the standard treatment for extragonadal
germ cell tumors involved complete surgical tumor resection.
However, as surgical resection alone yielded poor prognosis,
chemotherapy based on cisplatin was introduced notably improving
patient's overall survival rates (19,20).
Nonetheless, in some patients with mixed germ cell tumor, a
residual mass may still be present after cisplatin chemotherapy and
conventional marginal chemotherapy (21). As a result, the current standard of
care for mixed malignant germ cell tumors involves a
multidimensional approach. This includes preoperative combination
chemotherapy followed by aggressive surgical excision of the
residual lesion (22). In patients
with mediastinal mixed germ cell tumor, the potential risk of
spontaneous rupture which can result in severe complications should
be considered. When patients with mediastinal mixed germ cell tumor
experience life-threatening bleeding, conservative therapies like
blood transfusion and volume resuscitation are ineffective, and
prompt surgical removal of the mass and hemostatic interventions
are required (1). The prognosis of
extragonadal germ cell tumors is closely related to the anatomic
location and histological type of the tumor (8). In adult patients with extragonadal
germ cell tumors, the primary location in the mediastinum and the
histological type are additional independent prognostic factors
that are associated with shorter survival (8). Mixed germ cell tumors that arise in
the mediastinum often have a poor prognosis due to the tumor
directly invading vital organs in that area. The tissue type is the
most important prognostic factor for adult extragonadal germ cell
tumors, with seminomas and non-seminomatous carcinomas having
long-term survival rates of ~90 and ~45%, respectively (8). Overall, germ cell tumors occurring in
the mediastinum have a poorer prognosis. Hu et al (3) reported an average survival time of
only 3 months in 10 patients with mixed mediastinal germ cell
tumors. Ruan et al (1)
documented a case involving a patient with a mediastinal mixed germ
cell tumor that spontaneously ruptured, leading to hemorrhage. This
rare clinical scenario manifested as bilateral massive hemothorax
and hypovolemic shock. To manage the severe bleeding, emergency
surgical excision of the tumor was completed. Pathological
examination revealed the tumor to be a combination of
choriocarcinoma and immature teratoma, with concurrent pulmonary
metastasis of choriocarcinoma cells. The patient exhibited a
favorable recovery postoperatively and received adjuvant salvage
chemotherapy. After a total of 2 years following the diagnosis, the
patient continued to show remission with no evidence of disease
recurrence.
It is noteworthy that surgery carries certain risks
and may potentially accelerate tumor metastasis. The PET/CT
examination results of the patient of the present case report 10
days after surgery indicated the possibility of bone metastasis.
However, it is unclear whether the metastasis occurred before the
surgery. Filho et al (23)
reported a case of a male patient with metastatic testicular cancer
presenting with spontaneous retroperitoneal hemorrhage, who, after
stabilization with conservative treatment, responded well to
chemotherapy. Given the stable vital signs, red blood cell count
and hemoglobin levels of the patient of the present case report
upon admission, and considering the uncertainties in tumor staging,
it was hypothesized that initial conservative treatment was more
appropriate. After stabilizing hemodynamics, chemotherapy could
have been administered, and the timing for surgery would be
reconsidered if the tumor shrunk post-chemotherapy, potentially
offering the best treatment outcome for the patient. Therefore, not
all mixed germ cell tumors are suitable for emergency surgery. For
patients with spontaneous rupture of mediastinal germ cell tumors,
careful evaluation of the patient's vital signs and approximate
tumor staging is needed before considering surgical treatment. We
aim to improve the prognosis of patients with this disease by
sharing the present case report.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JL and XSL guided the conception and design of the
study. XSL, SHX, YPT, KYW, YML and JM collected clinical data and
figures. XSL was responsible for writing the draft. XSL, JL and SHX
revised the manuscript. YBL conducted the second round of image
acquisition and modifications. JL, XSL, SHX, YPT, YKW, YML and JM
confirm the authenticity of all the raw data. All authors have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient's next of kin (father) provided signed
informed consent for the publication of the patient's data and
images after the patient succumbed to the disease.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ruan Z, Wang S, Wang Z and Jing Y: A rare
case of bilateral massive hemothorax from spontaneous rupture of a
primary mediastinal mixed germ cell tumor. Ann Thorac Surg.
93:664–666. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shaher A, Salameh M and Raslan A:
Mediastinal mixed germ cell tumor with purulent pericarditis and
empyema caused by Escherichia coli: A rare case report. J Cardiol
Cases. 26:239–241. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hu X, Li D, Xia J, Wang P and Cai J:
Mediastinal mixed germ cell tumor: A case report and literature
review. Open Med (Wars). 16:892–898. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stang A, Trabert B, Wentzensen N, Cook MB,
Rusner C, Oosterhuis JW and McGlynn KA: Gonadal and extragonadal
germ cell tumors in the United States, 1973–2007. Int J Androl.
35:616–625. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pauniaho SL, Salonen J, Helminen M,
Vettenranta K, Heikinheimo M and Heikinheimo O: The incidences of
malignant gonadal and extragonadal germ cell tumors in males and
females: A population-based study covering over 40 years in
Finland. Cancer Causes Control. 23:1921–1927. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cheng L, Zhang S, MacLennan GT, Poulos CK,
Sung MT, Beck SD and Foster RS: Interphase fluorescence in situ
hybridization analysis of chromosome 12p abnormalities is useful
for distinguishing epidermoid cysts of the testis from pure mature
teratoma. Clin Cancer Res. 12:5668–5672. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sung MT, Maclennan GT, Lopez-Beltran A,
Zhang S, Montironi R and Cheng L: Primary mediastinal seminoma: A
comprehensive assessment integrated with histology,
immunohistochemistry, and fluorescence in situ hybridization for
chromosome 12p abnormalities in 23 cases. Am J Surg Pathol.
32:146–155. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ronchi A, Cozzolino I, Montella M,
Panarese I, Zito Marino F, Rossetti S, Chieffi P, Accardo M,
Facchini G and Franco R: Extragonadal germ cell tumors: Not just a
matter of location. A review about clinical, molecular and
pathological features. Cancer Med. 8:6832–6840. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sasaka K, Kurihara Y, Nakajima Y, Seto Y,
Endo I, Ishikawa T and Takagi M: Spontaneous rupture: A
complication of benign mature teratomas of the mediastinum. AJR Am
J Roentgenol. 170:323–328. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lemańska A, Banach P, Stanisławska K,
Juszkat R, Spaczyński M and Nowak-Markwitz E: Urgent embolization
of hemorrhagic choriocarcinoma liver metastases-case report and
review of the literature. Ginekol Pol. 86:957–961. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bokemeyer C, Nichols CR, Droz JP, Schmoll
HJ, Horwich A, Gerl A, Fossa SD, Beyer J, Pont J, Kanz L, et al:
Extragonadal germ cell tumors of the mediastinum and
retroperitoneum: Results from an international analysis. J Clin
Oncol. 20:1864–1873. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chaturvedi A, Gange C, Sahin H and
Chaturvedi A: Incremental value of magnetic resonance imaging in
further characterizing hypodense mediastinal and paracardiac
lesions identified on computed tomography. J Clin Imaging Sci.
8:102018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Heremans R, Valentin L, Sladkevicius P,
Timmerman S, Moro F, Van Holsbeke C, Epstein E, Testa AC, Timmerman
D and Froyman W: Imaging in gynecological disease (24): Clinical
and ultrasound characteristics of ovarian mature cystic teratomas.
Ultrasound Obstet Gynecol. 60:549–558. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Park JW, Jeong WG, Lee JE, Lee HJ, Ki SY,
Lee BC, Kim HO, Kim SK, Heo SH, Lim HS, et al: Pictorial review of
mediastinal masses with an emphasis on magnetic resonance imaging.
Korean J Radiol. 22:139–154. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Marom EM: Advances in thymoma imaging. J
Thorac Imaging. 28:69–80. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhou J, Wang S, Zhu L, Zhou L, Zeng H, Gan
Y and Wang C: Terminal deoxynucleotidyl transferase commonly
expresses in germ cell tumors: Evaluation on a large series from
multiple centers. Int J Gen Med. 14:119–129. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mego M, van Agthoven T, Gronesova P,
Chovanec M, Miskovska V, Mardiak J and Looijenga LHJ: Clinical
utility of plasma miR-371a-3p in germ cell tumors. J Cell Mol Med.
23:1128–1136. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sakane T, Okuda K, Murase T, Watanabe T,
Oda R, Tatematsu T, Yokota K, Haneda H, Inagaki H and Nakanishi R:
Mixed-type primary germ cell tumor of the mediastinum in a young
adult male with a sudden life threatening condition: A case report.
Thorac Cancer. 11:166–169. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dulmet EM, Macchiarini P, Suc B and Verley
JM: Germ cell tumors of the mediastinum. A 30-year experience.
Cancer. 72:1894–1901. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nichols CR: Mediastinal germ cell tumors.
Clinical features and biologic correlates. Chest. 99:472–479. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Reuter VE: The pre and post chemotherapy
pathologic spectrum of germ cell tumors. Chest Surg Clin N Am.
12:673–694. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liu Y, Wang Z, Peng ZM and Yu Y:
Management of the primary malignant mediastinal germ cell tumors:
Experience with 54 patients. Diagn Pathol. 9:332014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Filho LHCP, Silva TA, Beal PR, Buonfiglio
VB and Sadi MV: Spontaneous rupture of a retroperitoneal lymph node
metastasis causing massive hemorrhage in a patient with advanced
mixed germ cell tumor. Urol Case Rep. 45:1021802022. View Article : Google Scholar : PubMed/NCBI
|