Introduction
Uterine leiomyoma (UL) is a benign monoclonal tumor
of the smooth muscle cells, which arises more specifically from the
underlying myometrial tissue in the uterus (1). These tumors contain high amounts of
extracellular matrix components, such as collagen, fibronectin and
proteoglycans (2). UL has been
diagnosed in 30–40% of females at a reproductive age and is the
leading indication for hysterectomy (1). Although this complication is often
asymptomatic, it may result in symptoms including abdominal
discomfort to uterine bleeding, menometrorrhagia, severe
dysmenorrhea, pelvic pain and infertility (3). Despite the high prevalence of UL, the
associated pathophysiology and proliferative pathway remains
unknown. Different risk factors have been suggested for UL,
including age, endogenous hormone levels (estrogen and
progesterone), certain enzymes, obesity, nulliparity and genetic
factors (2, 3). The genetic liability of UL is
supported by the fact that hysterectomy and hospitalization due to
UL is twice as high in monozygote female twins compared to
dizygotes (4, 5).
UL is an estrogen-dependent tumor and is more
prevalent during the reproductive age. The estrogen hormone
stimulates the progression of cell proliferation in the
G1 phase of the cell cycle in various target tissues,
including the uterus and breast (2,
6). Evidence has shown that
leiomyoma tissue is more sensitive to estrogen compared to
myometrium and the concentration of estrogen in leiomyoma tissue is
higher compared to the normal myometrium. Additionally, the
leiomyoma growth is regulated by serum estrogen and estrogen in the
tumor (7).
Estrogen exerts its biological effect through the
high affinity binding to estrogen receptors (ESR α and ESR β) and
muscle cells with leiomyoma express α and β ESRs (8, 9).
The P450 cytochrome system (CYP450) contains a group
of enzymes that are involved in steroid hormone biosynthesis and
metabolic activation of carcinogens (10, 11).
Five different enzymes have been identified in this system, which
are involved in estrogen synthesis and degradation. Cytochrome P450
17a (CYP17) and cytochrome P450 19 (CYP19 or aromatase) control the
early and terminal steps of the estrogen biosynthesis pathway
respectively (12).
Cytochrome P450 1A1 (CYP1A1) and cytochrome P450 1B1
(CYP1B1) are the main enzymes of the CYP450 system in estrogen
catabolism that catalyze the formation of 2-hydroxy and 4-hydroxy
estrogen metabolites. Catechol-O-methyl transferase catalyzes the
excretion of carcinogenic 4-hydroxy estrogen metabolites (12). Certain evidence has shown that human
endometrial epithelium produce cytochrome P450 (CYP P450) metabolic
enzymes that generate genotoxic intermediates and affect ESRs.
Therefore, these enzymes are associated with carcinogenesis in
extrahepatic tissues (13, 14). The study by Shastry (15) found high 4-hydroxylase activities in
human uterine myometrium and benign UL. This evidence strongly
proposes that estrogens and their metabolic products affect the
occurrence and development of UL. Therefore, CYP1A1 and
CYP1B1 variants are expected to affect estrogen synthesis or
degradation (16).
The association between polymorphisms of
estrogen-metabolizing enzyme genes and UL susceptibility have been
studied in different populations, however, their results were
inconsistent (14, 17). Therefore, in the present study the
association between Arg368His (rs79204362), Leu432Val (rs1056836),
Asp449Asp (rs1056837) and Asn453Ser (rs1800440) polymorphisms of
the CYP1B1 gene and UL susceptibility was examined in
southeast Iran.
Materials and methods
Subject characteristics
The present case control study was performed on 105
females in their pre-menopausal stage that had undergone myomectomy
or hysterectomy in Ali Ibn Abitaleb Hospital, Zahedan, southeast
Iran, and were enrolled between 2011 and 2013. All the participants
were selected using the convenient sampling method. In all the
participants, leiomyoma had been confirmed pathologically.
In total, 112 healthy females in their premenopausal
stage were selected as the control group among females referring
for a routine annual check-up and performing the Pap smear test.
The groups were matched with respect to demographic factors, such
as age and ethnicity (Fars or Balouch). Physical and
ultrasonographic evaluations were performed for females in the
control group to elimate UL. The Pap smear test was also
negative.
The exclusion criteria were existence of systemic
diseases and history of malignancy. All the participants were
Iranian and provided their informed consent prior to participating
in the study. The protocol of the study was approved by the Ethics
Committee of Zahedan University of Medical Sciences.
Genotype analysis
Genomic DNA was extracted from 2 ml peripheral blood
leukocytes using the salting out phenol chloroform method and
stored at −20 ˚ C until analysis. The analysis of the CYP1B1
polymorphisms was performed using the sequencing method.
The reference sequence was the human CYP1B1
gene (GeneBank accession number U56438). The fragment containing
all the polymorphisms was amplified using the forward and reverse
primers of 5′-TCACTTGCTTTTCTCTCTCC-3′ and
5′-AATTTCAGCTTGCCTCTTG-3′, respectively (18).
The total volume of the PCR mixture was 25 µ1 and
contained 300 ng genomic DNA, 25 pM of each primers, 0.1 mM dNTP,
1.5 mM MgCl2, 2.5 µ1 PCR buffer 10X and 1 unit of Taq
polymerase.
Amplification was performed in a Bio-Rad thermal
cycler (Bio-Rad, Hercules, CA, USA) using a thermal profile of
initial denaturation at 96˚C for 6 min, followed by 30 cycles at
96˚C for 30 sec, annealing at 61˚C for 40-base pair
insertion/deletion polymorphism and 60˚C for T309G polymorphism for
30 sec, primer extension at 72˚C for 60 sec, and a final extension
step at 72˚C for 6 min.
The PCR products were sequenced in a forward
direction with the same primers as used in the PCR, using ABI Big
Dye terminator chemistry and an ABI PRISM 3730/3730xl instrument
(Applied Biosystems, Foster City, CA, USA).
A schematic diagram of Arg368His (rs79204362),
Leu432Val (rs1056836), Asp449Asp (rs1056837) and Asn453Ser
(rs1800440) polymorphisms of the CYP1B1 gene is presented in
Fig. 1.
Statistical analysis
Statistical analyses were performed using SPSS
software, version 20 (IBM Corp, Armonk, NY, USA). The frequency of
the genotypes and alleles were compared between two groups using
the χ2 or Fisher's exact tests. Quantitative variables
were compared using the Student's t-test. Odds ratios (OR) and 95%
confidence intervals (CI) were accounted to the significant allelic
and genotypic associations. P<0.05 was considered to indicate a
statistically significant difference.
The frequency of haplotypes was calculated using
PHASE version 2.1 software (19,
20). Haplotypes with estimated
frequency <5% were excluded from the analysis. Logistic
regression analysis was used to assess the independent effect of
each risk polymorphism and haplotypes on UL. Bonferroni's
correction was applied to confirm the association of haplotypes
with the disease.
The computation of linkage disequilibrium (LD)
between single-nucleotide polymorphisms (SNPs) was estimated using
the normalized measure of allelic association D' and the
characterization of these patterns was determined using Haploview
4.2 software (http://www.borad.mit.edu/mpg/haploview).
Results
Subject characteristics
The demographic and clinical characteristics of the
UL patients and controls are shown in Table I. No significant differences in the
age, body mass index and marital status between the two groups were
observed. There were no significant differences in menstrual
histories, including duration of menstruations, age of menarche and
menstrual cycle between the two groups. Additionally, the frequency
of bleeding and pain were significantly higher in the UL females
(P<0.0001).
 | Table I.Demographic and clinical
characteristics of the UL females and control group. |
Table I.
Demographic and clinical
characteristics of the UL females and control group.
| UL females
(n=105) | Controls (n=112) | P-value |
|---|
| Age, years | 38.1±9.8 | 36.7±5.7 |
0.23 |
| Marriage status, n
(%) | 100 (95) | 109 (97) |
0.49 |
| BMI,
kg/m2 | 25.1±5.5 | 25.4±4.7 |
0.70 |
| Age of menarche,
years | 13.5±1.5 | 13.1±1.6 |
0.07 |
| Duration of menses,
days | 6.1±1.6 | 5.8±1.5 |
0.07 |
| Menstrual cycle,
days | 28.3±3.3 | 28.7±2.1 |
0.30 |
| Bleeding, n
(%) | 60 (57) | 4 (4) |
<0.0001 |
| Pain, n (%) | 30 (29) | 6 (5) |
<0.0001 |
Genotyping of CYP1B1 SNPs
Four SNPs of the CYP1B1 gene were
successfully genotyped in 105 UL females and 112 healthy controls.
The frequency of alleles and genotypes of CYP1B1
polymorphisms are shown in Table
II. All the loci conformed to the Hardy-Weinberg equilibrium in
UL females and control groups (P>0.05). The frequency of the
CYP1B1 432Val (G) allele in females with UL and controls
were 38 and 30%, respectively, and the difference was not
statistically significant. The genotype frequency of the
CYP1B1 Leu432Val polymorphism was not significantly
different between the two groups. Although the frequency of the
CYP1B1 449Asp (T) allele was higher in the UL group compared
to controls (38 vs. 31%), the difference was not significant. The
genotype frequency of the CYP1B1 Asp449Asp (T/C)
polymorphism was not significantly different between the two
groups.
 | Table II.Allelic and genotypic frequency of
the CYP1B1 gene polymorphisms in UL females and healthy
controls. |
Table II.
Allelic and genotypic frequency of
the CYP1B1 gene polymorphisms in UL females and healthy
controls.
| CYP1B1 | UL females
(n=105) | Controls
(n=112) | P-value | Non.adjusted OR
(95% CI) | P-value | Adjusted OR (95%
CI)a |
|---|
| Leu432Val (C/G)
rs1056836 |
|
CC, n (%) | 42 (40) | 56 (50) | | 1 | | 1 |
|
CG, n (%) | 47 (45) | 45 (40) |
0.30 | 1.4 (0.8-2.5) |
0.30 | 1.4 (0.8-2.4) |
|
GG, n (%) | 16 (15) | 11 (10) |
0.13 | 1.3 (0.8-2.0) |
0.20 | 1.4 (0.9-2.1) |
|
CG+GG, n (%) | 63 (60) | 56 (50) |
0.14 | 1.5 (0.9-2.6) |
0.20 | 1.5 (0.8-2.5) |
|
C, n (%) | 131 (62) | 157 (70) | | 1 | | − |
|
G, n (%) | 79 (38) | 67 (30) |
0.09 | 1.4 (1.0-2.1) | | − |
| Asp449Asp (T/C)
rs1056837 |
|
CC, n (%) | 42 (40) | 53 (47) | | 1 | | 1 |
|
CT, n (%) | 47 (45) | 48 (43) |
0.50 | 1.2 (0.7-2.2) |
0.50 | 1.2 (0.7-2.2) |
|
TT, n (%) | 16 (15) | 11 (10) |
0.20 | 1.4 (0.9-2.1) |
0.30 | 1.3 (0.8-2.0) |
|
CT+TT, n (%) | 63 (60) | 59 (53) |
0.30 | 1.4 (0.8-2.3) |
0.30 | 1.3 (0.8-2.3) |
|
C, n (%) | 131 (62) | 154 (69) | | 1 | | |
|
T, n (%) | 79 (38) | 70 (31) |
0.19 | 1.3 (0.9-2.0) | | |
| Asn453Ser (A/G)
rs1800440 |
|
AA | 71 (68) | 64 (57) | | 1 | | |
|
AG | 29 (27) | 42 (37) |
0.11 | 0.6 (0.4-1.1) |
0.12 | 0.6 (0.4-1.1) |
|
GG | 5 (5) | 6 (6) |
0.70 | 0.9 (0.5-1.6) |
0.70 | 0.9 (0.5-1.6) |
|
AG+GG | 34 (32) | 48 (43) |
0.11 | 0.6 (0.4-1.1) |
0.12 | 0.7 (0.4-1.1) |
| Allele |
|
A | 171 (82) | 170 (76) | | | | |
|
G | 39 (18) | 54 (24) |
0.16 | 0.7 (0.5-1.1) | | |
| Arg368His (G/A)
rs79204362 |
|
GG | 81 (77) | 98 (88) | | 1 | | |
|
GA | 21 (20) | 14 (13) |
0.11 | 1.8 (0.9-3.8) |
0.11 | 1.8 (0.9-3.8) |
|
AA | 3 (3) | 0 (0) | − | − | − | − |
|
GA+AA | 24 (23) | 14 (13) |
0.11 | 1.8 (0.9-3.8) |
0.11 | 1.8 (0.9-3.8) |
| Allele |
|
G | 183 (87) | 210 (94) | | | | |
|
A | 27 (13) | 14 (6) |
0.02 | 2.2 (1.1-4.4) | | |
Genotype frequencies of
polymorphisms
Although there was no significant difference in the
genotypes frequency of the Arg368His (G/A) polymorphism between UL
females and controls, a higher frequency of the A allele was
observed in UL females compared to healthy females (13 vs. 6%) and
the risk of UL was increased to 2.2-fold in the presence of the A
allele (OR, 2.2; 95% CI, 1.1-4.4; P=0.02). There was no association
between CYP1B1, Asn453Ser (A/G) polymorphism and UL. The
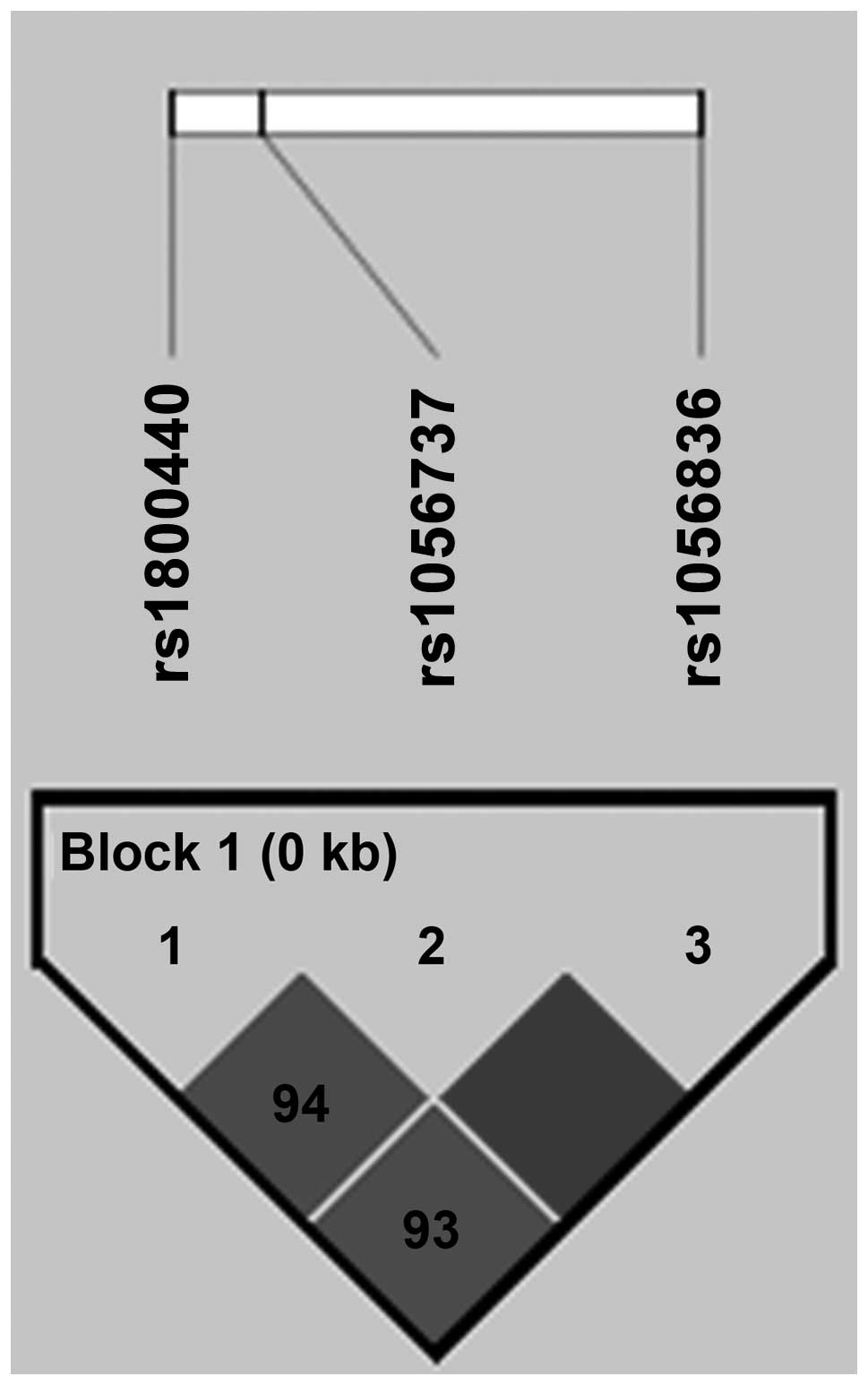
CYP1B1 Arg368His (rs79204362) polymorphism has not been
found in HapMap. Therefore, the LD patterns of the three
CYP1B1 SNPs were analyzed, as shown in Fig. 2. There was a strong LD between the
three common SNPs in CYP1B1 gene.
The frequency of five common haplotypes of four SNPs
in the CYP1B1 gene [Leu432Val (C/G), Asp449Asp (T/C),
Asn453Ser (A/G) and Arg368His (G/A)] are shown in Table III.
 | Table III.Haplotypes frequency of the
CYP1B1 gene polymorphisms in UL patients and controls. |
Table III.
Haplotypes frequency of the
CYP1B1 gene polymorphisms in UL patients and controls.
| CYP1B1
SNPs | |
|---|
| |
|---|
| rs1056836 | rs1056837 | rs1800440 | rs79204362 | Leiomyoma
(n=105) | Control
(n=112) | P-value | OR (95% CI) |
|---|
| C | C | A | G | 0.446518 | 0.445568 | | 1 |
| C | C | G | G | 0.240873 | 0.177685 | 0.30 | 1.3 (0.8-2.2) |
| C | T | A | G | 0.013393 | 0 | 0.10 | − |
| G | T | A | G | 0.236670 | 0.240574 | 0.95 | 1.0 (0.9-1.2) |
| G | T | A | A | 0.062302 | 0.127683 | 0.039a | 0.8 (0.7-1) |
Although the frequency of the CCGG haplotype was
higher in UL females compared to the controls (24 vs. 18%), the
difference was not statistically significant (P=0.3). The frequency
of the GTAA haplotype in controls was significantly higher than
that of the cases (12.7 vs. 6%, P=0.039) and the haplotype-based
association analysis revealed that the GTAA haplotype may have
potential to protect against UL in females (OR, 0.8; 95% CI, 0.7-1;
P=0.039). This association was also statistically significant
following Bonferroni's correction.
Discussion
In the present study, there was no association
between the Leu432Val, Asp449Asp and Asn453Ser polymorphisms of the
CYP1B1 gene and SLE. However, a higher frequency of the A
allele of Arg368His (G/A) polymorphism was observed in UL females
compared to healthy females and according to the current findings,
the presence of the A allele increased the SLE risk. In addition,
the frequency of the GTAA haplotype in the controls was
significantly higher compared to the patients; therefore, the GTAA
haplotype played a protective role in SLE susceptibility. A strong
LD between the three common SNPs in the CYP1B1 gene was
observed in the population of the present study.
UL is a common neoplasm associated with an
interaction between various genes, cytokines, growth factors,
hormones and environmental factors. Whether ovarian steroid
hormones play an essential role in the growth of leiomyoma is
unknown. The mitogenic effects of steroid hormones are induced
through their receptors or by regulation of growth factor
expression (7, 8). The UL development possibly occurs in
response to a certain type of injury to the myometrium, such as
hypoxia (21).
CYP1B1 is known as a key enzyme that metabolizes a
variety of putative human carcinogens and estrogens. Certain
evidence stated that this enzyme may play an essential role in
tumor development and progression (22). Therefore, polymorphisms in the
CYP1B1 gene may affect the metabolism of environmental
estrogens and hormone-like substances. The polymorphisms influenced
the inter-individual risk of developing a tumor (22). The CYP1B1 enzyme catalyzes the
conversion of estrogens to 4-hydroxy estrogen metabolites and
recent products can increase the quantity of estrogen within the
cells by activating the ESR. Certain evidence has shown that the
CYP1B1 variants are more efficient in the conversion and
accumulation of carcinogenic estrogens (23, 24).
Thus, inherited variations in the CYP1B1 activity
lead to differences in estrogen metabolism and explain
inter-individual differences in the UL risk in association with
estrogen-mediated tumorogenesis (25).
Several studies have addressed the association
between the genetic polymorphisms of enzymes involved in the
estrogen metabolism and the occurrence of UL (14, 17,
26, 27). In 2006, Herr et al (26) reported a significant correlation
between CYP2A13 and CYP1A1 SNPs and UL in a Caucasian
population. The genetic distribution of Ile462Val and T6235C
polymorphisms of the CYP1A1 gene and Arg48Gly, Ala119Ser,
Leu432Val and Asp449Asp polymorphisms of the CYP1B1 gene
were studied by Ye et al (17) in Chinese females. The studies
reported that only the CYP1A1 Ile462Val polymorphism was
associated with the increased risk of UL. However, similar to the
findings of the present study, there was no association between
polymorphisms of the CYP1B1 gene and UL susceptibility in
China. Despite the results of Ye et al (17) in Chinese females, El-Shennawy et
al (14) observed an elevated
risk of UL in females with the CC genotype of the CYP1B1
Leu432Val (C/G) polymorphism and according to their results this
genotype can predict the susceptibility to UL in Egyptian females.
Shen et al (27, 28) studied the association between the
Ala119Ser, Leu432Val and Asp449Asp polymorphisms of the
CYP1B1 gene and UL in Han Chinese females. Consistent with
the results of the present study, an association between the
Asp449Asp (T/C) polymorphism gene and UL was not observed, however,
the studies found that the Ala119Ser polymorphism was a risk factor
and the Leu432Val polymorphism was a protective factor for UL
development. The present study findings showed a strong LD between
the three common SNPs in the CYP1B1 gene in the population.
Similarly, Bethke et al (29) observed a strong LD between the five
common SNPs in the CYP1B1 gene in UK.
To the best of our knowledge, this is the first
study regarding the effect of CYP1B1 haplotypes (four SNPs)
on UL susceptibility, therefore, further studies in different
populations are required to evaluate the association between
CYP1B1 haplotypes and UL.
In conclusion, there was an association between the
A (His) allele of the CYP1B1 Arg368His (rs79204362)
polymorphism and UL. In addition, the GTAA haplotype may play a
protective role in SLE susceptibility. There was a strong LD
between the three common SNPs (rs1056836, rs1056837 and rs1800440)
of the CYP1B1 gene in the southeast Iranian population.
Acknowledgements
The present study was extracted from an MS thesis
(registered no. 2162; Comparison of CYP1A1 and Cyp1B1 genes
polymorphism in women with leiomyoma and controls, by Dr Saeedeh
Salimi, Maryam Khodamian and Dr Minoo Yaghmaei, 2013) at Zahedan
University of Medical Sciences. The authors would like to thank the
Deputy of Research Affairs at the University for funding the
study.
References
|
1
|
Falcone T and Walters MD: Hysterectomy for
benign disease. Obstet Gynecol. 111:753–767. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parker WH: Etiology, symptomatology, and
diagnosis of uterine myomas. Fertil Steril. 87:725–736. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sell SM, Tullis C, Stracner D, Song CY and
Gewin J: Minimal interval defined on 7q in uterine leiomyoma.
Cancer Genet Cytogenet. 157:67–69. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Luoto R, Kaprio J, Rutanen EM, Taipale P,
Perola M and Koskenvuo M: Heritability and risk factors of uterine
fibroids - the Finnish Twin Cohort study. Maturitas. 37:15–26.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Treloar SA, Martin NG, Dennerstein L,
Raphael B and Heath AC: Pathways to hysterectomy: insights from
longitudinal twin research. Am J Obstet Gynecol. 167:82–88. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sabbah M, Courilleau D, Mester J and
Redeuilh G: Estrogen induction of the cyclin D1 promoter:
involvement of a cAMP response-like element. Proc Natl Acad Sci
USA. 96:11217–11222. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Urabe M, Yamamoto T, Naito K, Kitawaki J,
Honjo H and Okada H: Study on the local estrogen biosynthesis in
human uterine leiomyoma. Nihon Sanka Fujinka Gakkai Zasshi.
42:1229–1236. 1990.(In Japanese). PubMed/NCBI
|
|
8
|
Roodi N, Bailey LR, Kao WY, et al:
Estrogen receptor gene analysis in estrogen receptor-positive and
receptor-negative primary breast cancer. J Natl Cancer Inst.
87:446–451. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jakimiuk AJ, Bogusiewicz M, Tarkowski R,
et al: Estrogen receptor alpha and beta expression in uterine
leiomyomas from premenopausal women. Fertil Steril. 82 (Suppl
3):1244–1249. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stiborová M, Martínek V, Rýdlová H, Koblas
T and Hodek P: Expression of cytochrome p 450 1A1 and its
contribution to oxidation of a potential human carcinogen
1-phenylazo-2-naphthol (Sudan I) in human livers. Cancer Lett.
220:145–154. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Somner J, McLellan S, Cheung J, et al:
Polymorphisms in the p 450 c17 (17-hydroxylase/17,20-Lyase) and p
450 c19 (aromatase) genes: association with serum sex steroid
concentrations and bone mineral density in postmenopausal women. J
Clin Endocrinol Metab. 89:344–351. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ashton KA, Proietto A, Otton G, et al:
Polymorphisms in genes of the steroid hormone biosynthesis and
metabolism pathways and endometrial cancer risk. Cancer Epidemiol.
34:328–337. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hukkanen J, Mäntylä M, Kangas L, et al:
Expression of cytochrome p 450 genes encoding enzymes active in the
metabolism of tamoxifen in human uterine endometrium. Pharmacol
Toxicol. 82:93–97. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
El-Shennawy GA, Elbialy AA, Isamil AE and
El Behery MM: Is genetic polymorphism of ER-α, CYP1A1, and CYP1B1 a
risk factor for uterine leiomyoma? Arch Gynecol Obstet.
283:1313–1318. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shastry BS: SNP alleles in human disease
and evolution. J Hum Genet. 47:561–566. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Maruo T, Ohara N, Wang J and Matsuo H: Sex
steroidal regulation of uterine leiomyoma growth and apoptosis. Hum
Reprod Update. 10:207–220. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ye Y, Cheng X, Luo HB, Liu L, Li YB and
Hou YP: CYP1A1 and CYP1B1 genetic polymorphisms and uterine
leiomyoma risk in Chinese women. J Assist Reprod Genet. 25:389–394.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zheng W, Xie DW, Jin F, et al: Genetic
polymorphism of cytochrome p 450–1B1 and risk of breast cancer.
Cancer Epidemiol Biomarkers Prev. 9:147–150. 2000.PubMed/NCBI
|
|
19
|
Stephens M and Donnelly P: A comparison of
bayesian methods for haplotype reconstruction from population
genotype data. Am J Hum Genet. 73:1162–1169. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Scheet P and Stephens M: A fast and
flexible statistical model for large-scale population genotype
data: applications to inferring missing genotypes and haplotypic
phase. Am J Hum Genet. 78:629–644. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mesquita FS, Dyer SN, Heinrich DA, Bulun
SE, Marsh EE and Nowak RA: Reactive oxygen species mediate
mitogenic growth factor signaling pathways in human leiomyoma
smooth muscle cells. Biol Reprod. 82:341–351. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Aklillu E, Oscarson M, Hidestrand M,
Leidvik B, Otter C and Ingelman-Sundberg M: Functional analysis of
six different polymorphic CYP1B1 enzyme variants found in an
Ethiopian population. Mol Pharmacol. 61:586–594. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hayes CL, Spink DC, Spink BC, Cao JQ,
Walker NJ and Sutter TR: 17 beta-estradiol hydroxylation catalyzed
by human cytochrome p 450 1B1. Proc Natl Acad Sci USA.
93:9776–9781. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhu BT and Conney AH: Functional role of
estrogen metabolism in target cells: review and perspectives.
Carcinogenesis. 19:1–27. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Houston KD, Hunter DS, Hodges LC and
Walker CL: Uterine leiomyomas: mechanisms of tumorigenesis. Toxicol
Pathol. 29:100–104. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Herr D, Bettendorf H, Denschlag D, Keck C
and Pietrowski D: Cytochrome p 2A13 and p 1A1 gene polymorphisms
are associated with the occurrence of uterine leiomyoma. Arch
Gynecol Obstet. 274:367–371. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shen Y, Ren ML, Xu J, et al: A multicenter
case-control study on screening of single nucleotide polymorphisms
in estrogen-metabolizing enzymes and susceptibility to uterine
leiomyoma in han chinese. Gynecol Obstet Invest. 77:224–230. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shen Y, Xu Q, Ren M, Cai Y and Xu J: Role
of single nucleotide polymorphisms in estrogen-metabolizing enzymes
and susceptibility to uterine leiomyoma in Han Chinese: a
case-control study. J Obstet Gynaecol Res. 40:1077–1084. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bethke L, Webb E, Sellick G, et al:
Polymorphisms in the cytochrome p 450 genes CYP1A2, CYP1B1, CYP3A4,
CYP3A5, CYP11A1, CYP17A1, CYP19A1 and colorectal cancer risk. BMC
Cancer. 7:1232007. View Article : Google Scholar : PubMed/NCBI
|