Introduction
With the rapid development of the catheter technique
and taking into account the pivotal function of renal sympathetic
nerves in hypertension, the study by Krum et al (1, 2) first
applied catheter-based radiofrequency renal sympathetic denervation
(RSD) for the treatment of patients with refractory hypertension
and obtained a positive antihypertensive efficacy. As a new
antihypertensive technique, radiofrequency RSD became a new
treatment of hypertension; however, its specific antihypertensive
effect and the underlying mechanism require further study (2, 3). In
addition, other than the significant inhibition of renal
sympathetic activity, the effects of radiofrequency RSD on the
renin-angiotensin system (RAS), oxidative stress and vascular
endothelial function remain unclear. In the present study, a
hypertensive dog model was established by administering a high-fat
diet and the antihypertensive effect and safety of radiofrequency
RSD were validated using these hypertensive dogs. The changes in
serum angiotensin II (AngII), nicotinamide adenine dinucleotide
phosphate oxidase (NADPH-ox), serum malondialdehyde (MDA), nitric
oxide (NO) and endothelial NO synthase (eNOS) were detected to
investigate the possible antihypertensive mechanisms of
radiofrequency RSD.
Materials and methods
Animals
A total of 12 same-strain qualified beagles, aged
10–12 months and including 6 for each gender, were purchased from
the Shanghai Experimental Animal Center (Shanghai, China). Animals
were purchased 2 weeks prior to the experiment and were housed in a
single cage in the Xiangya Animal Center of Central South
University (Changsa, China). After 1 week of habituation, the 12
beagles were randomly divided into the surgery (n=6) and
sham-surgery groups (n=6). Following the establishment of the
hypertension model, radiofrequency RSD was performed in the surgery
group; the sham-surgery group only received renal arteriography.
The study was approved by the Ethics Committee of the Third Xiangya
Hospital of Central South University.
Establishment of the hypertension
model
Animals were provided a high-fat diet for 3 months,
which consisted of 150 g basic feed/animal with the addition of
edible lard at 0.3-0.4 kg/animal. The basic feed was common dog
food (Xingtai Paide Pets Food Co., Ltd., Nanhe, Hebei, China) which
contained 23% crude protein, 4.9% crude fiber, 10% water, 9.2% ash,
1–3% calcium, 0.8% total phosphorus, 0.29% methionine, 11,000 IU/kg
vitamin A, 1,000 IU/kg vitamin D and 500 IU/kg vitamin E. Edible
lard (Sichuan Green Island Food Co., Ltd., Chengdu, Sichuan, China)
was purchased from the grain and oil market. Following successful
establishment of the model and the application of radiofrequency
RSD, animals in the surgery and sham-surgery groups were fed a diet
containing 0.1 kg/day fat to maintain their body weight (4).
Monitoring of pressure
The tail arterial pressure of the dogs in the awake
condition was measured using a BP-10E intelligent non-invasive
animal blood pressuremeter (Sofron Beijing Inc., China). The dogs
were placed on a fixator and when they were completely calm,
sleeves were placed on the root of their tails. Following
appropriate setup of the parameters associated with the blood
pressure meter, the instrument automatically read the systolic
arterial pressure (SAP), diastolic arterial pressure (DAP) and
heart rate (HR). Prior to the establishment of the model, blood
pressure levels were measured twice per week. After the measured
blood pressure and HR values were stable, which were used as the
baseline values, the establishment of the model began. The
measurement time points included before model establishment and 2,
4, 6 and 12 weeks after model establishment. The blood pressure
readings gradually stabilized after 12 weeks and radiofrequency RSD
was performed. Blood pressure was measured before the surgery and 3
days, 1 and 2 weeks, and 1, 2 and 3 months after the surgery.
Radiofrequency RSD intervention
The dogs were fasted prior to the surgery. The skin
areas at the back and bilateral femoral artery area of the dogs
were prepared accordingly, followed by an intramuscular injection
of Zoletil® (7 mg/kg; Virbac, Carros, France) and
Sumianxin (0.1 mg/kg; Jilin Shengda Animal Drug Co., Ltd., Yanbian,
Jilin, China) for anesthetization. Following successful anesthesia,
the dogs were immobilized on the surgery table in the supine
position. An ablation electrode was placed on the back and
connected to a radiofrequency ablation device (IBI, St. Jude
Medical, Inc., St. Paul, MN, USA). The temperature was controlled
at ~55˚C and the energy was set at 80 W. The right femoral artery
area was conventionally disinfected and a guiding catheter was
inserted through the femoral artery for renal arteriography and
renal artery positioning as the blood pressure was monitored. Three
to four ablation sites were selected from each site and a spiral
shape local ablation was performed (5F IBI radiofrequency ablation
catheter; St. Jude Medical). Each spot was ablated for 120 sec.
Blood pressure was monitored following completion of the surgery.
Sterile gauze was pressed on the puncture site to stop the bleeding
and penicillin was administered following the surgery to prevent
infection. Blood pressure and HR were measured in the morning
during the awake and non-feeding conditions at 3 days, 1 and 2
weeks, and 1 and 3 months after the surgery. Renal arteriography
was performed again at 3 months after the surgery. The sham-surgery
group only received renal arteriography (1, 4).
Measurement of neuroendocrine
factors
A total of 3 ml of blood was collected from the
great saphenous vein of all the dogs at baseline (before model
establishment), before the surgery (after model establishment) and
at 1 week, and 1 and 3 months after radiofrequency RSD. Blood
samples were stored in anticoagulant tubes at 4 ˚C. Subsequently,
the samples were centrifuged in a refrigerated centrifuge at 2,780
x g for 15 min to separate the serum (Xiangyi Centrifuge Instrument
Co., Ltd., Changsha, Hunan, China) and the obtained serum samples
were stored in a −80˚C freezer (Meiling Freezer Technology Co.,
Ltd., Hefei, Anhui, China) for subsequent tests. The concentration
of AngII was measured using a radioimmunoassay (the reagent kit was
provided by Beijing Chemclin Biotech Co., Ltd., Beijing, China).
The concentration of MDA was measured using the thiobarbituric acid
method (the reagent kit was provided by the Nanjing Jiancheng
Bioengineering Institute, Nanjing, Jiangsu, China). The serum NO
concentration was determined using the nitrate reductase method
(the reagent kit was provided by the Nanjing Jiancheng
Bioengineering Institute). The serum eNOS concentration was
determined using the chemical method (the reagent kit was provided
by the Nanjing Jiancheng Bioengineering Institute). The
concentration of serum NADPH-ox was measured using ELISA (the
reagent kit was provided by the Shanghai BlueGene Biotech Co.,
Ltd., Shanghai, China).
Statistical analysis
SPSS version 17.0 software (SPSS, Inc., Chicago, IL,
USA) was used for statistical analyses. Measurement data are
reported as the mean ± standard deviation. The major data were
subjected to the normality test and the test of homogeneity of
variance. The comparison of means between two groups was performed
using the t-test and the comparison among multiple groups was
performed using one-way analysis of variance. P<0.05 was
considered to indicate a statistically significant difference and
P<0.01 indicated a strongly significant difference.
Results
Baseline condition of animals in the
two groups
The comparison of body weight, HR, blood pressure
and creatinine level between animals in the two groups did not
reveal any significant differences (P>0.05) (Table I).
 | Table I.Comparison of the baseline condition
between the surgery and sham-surgery groups prior to establishment
of the model. |
Table I.
Comparison of the baseline condition
between the surgery and sham-surgery groups prior to establishment
of the model.
| Group | Weight, kg | HR, time/min | SAP, mmHg | DAP, mmHg | MAP, mmHg | Creatinine,
µmol/l |
|---|
| Sham-surgery | 13.12±1.41 | 129±10 | 129.22±6.95 | 76.44±5.09 | 94.00±4.91 | 81.9±10.4 |
| Surgery | 13.08±2.43 | 127±13 | 122.89±4.84 | 75.64±6.09 | 93.39±4.66 | 82.4±12.1 |
Comparison of SAP, DAP and mean
arterial pressure (MAP) between animals in the two groups prior to
establishing the model
Compared to those measured prior to model
establishment, the levels of SAP, DAP and MAP of animals in the two
groups increased significantly following model establishment
(P>0.05), indicating that the model was successfully established
and there was no difference between the two groups (Table II).
 | Table II.Comparison of SAP, DAP and MAP levels
prior to the surgery between the surgery and the sham-surgery
groups. |
Table II.
Comparison of SAP, DAP and MAP levels
prior to the surgery between the surgery and the sham-surgery
groups.
| SAP, mmHg | DAP, mmHg | MAP, mmHg |
|---|
|
|
|
|
|---|
| Group | Baseline | Post-model
establishment | Baseline | Post-model
establishment | Baseline | Post-model
establishment |
|---|
| Sham-surgery | 129.22±6.95 |
149.33±9.16a | 76.44±5.09 |
83.56±2.52a | 94.00±4.91 |
109.44±2.14a |
| Surgery | 122.89±4.84 |
152.28±8.60a | 75.64±6.09 |
82.56±3.58a | 93.39±4.66 |
114.22±4.25a |
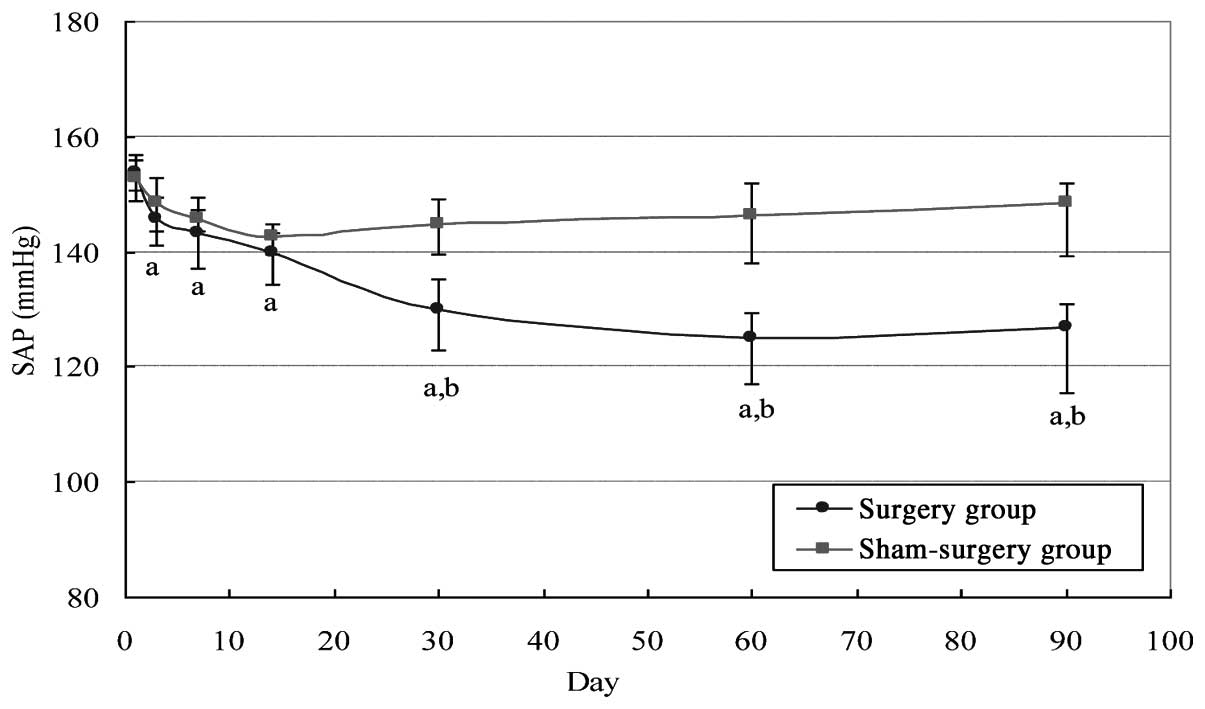
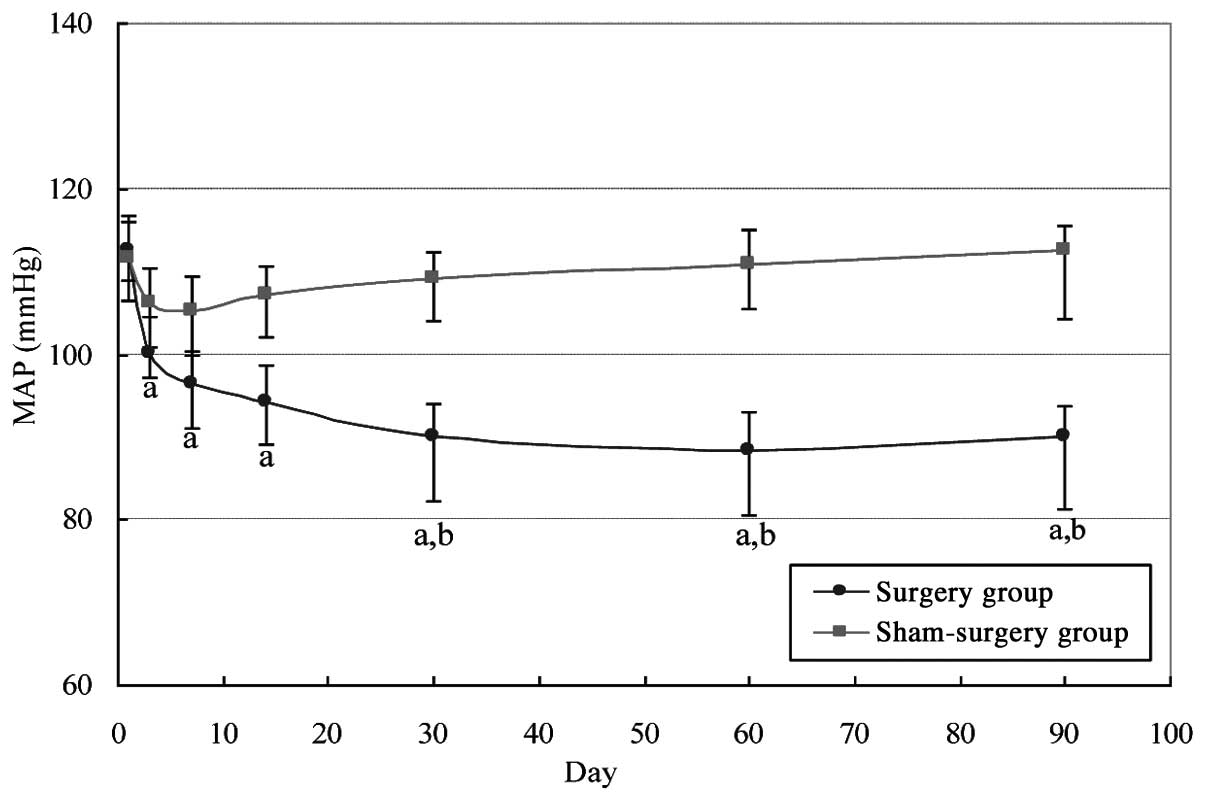
Changes in blood pressure following
radiofrequency RSD
The levels of SAP, DAP and MAP in the surgery group
at each time point following the surgery were significantly
decreased and showed significant differences from those obtained
prior to the surgery (P<0.05) (Figs.
1–3). In addition, the levels
of SAP, DAP and MAP in the sham-surgery group within 2 weeks after
the surgery also slightly decreased but did not show significant
differences from those in the surgery group (P>0.05). However,
at 1, 2 and 3 months after surgery, the comparison of SAP, DAP and
MAP between the surgery and the sham-surgery groups demonstrated
statistically significant differences (P<0.05).
Changes in the concentration of AngII
following radiofrequency RSD
The comparison of the baseline serum concentrations
of AngII between the sham-surgery and the surgery groups did not
reveal significant differences (P>0.05) (Table III). Following model
establishment, the serum AngII concentrations in the two groups
were significantly increased compared to the baseline levels
(P<0.05), with no difference between the two groups (P>0.05).
The serum concentrations of AngII at 1 week, and 1 and 3 months
after radiofrequency RSD in the sham-surgery group did not change,
whereas these levels were significantly decreased in the surgery
group, with a significant difference from the baseline level and
those observed prior to the surgery and in the sham-surgery group
(P<0.05).
 | Table III.Comparison of the serum concentrations
of angiotensinII (AngII) at each time point between the surgery
and sham-surgery groups. |
Table III.
Comparison of the serum concentrations
of angiotensinII (AngII) at each time point between the surgery
and sham-surgery groups.
| AngII concentration,
ng/ml |
|---|
|
|
|---|
| Group | Baseline | Post-model
establishment (prior to surgery) | 1 week
post-surgery | 1 month
post-surgery | 3 months
post-surgery |
|---|
| Sham-surgery | 51.76±10.77 |
120.77±17.30a |
123.61±11.78a |
124.60±13.20a |
126.30±12.92a |
| Surgery | 56.69±7.17 |
121.54±18.09a |
95.18±7.73a–c |
89.08±8.43a–c |
90.11±11.10a–c |
Changes in the serum concentrations of
NADPH-ox and MDA following radiofrequency RSD
Comparison of the baseline serum concentrations of
NADPH-ox and MDA between the surgery and sham-surgery groups did
not reveal significant differences (P>0.05) (Tables IV and V). Following model establishment, the
serum concentrations of NADPH-ox and MDA in these two groups
significantly increased from the baseline level (P<0.05);
however, there was no difference between these two groups
(P>0.05). In the sham-surgery group, the serum concentrations of
NADPH-ox and MDA at 1 week, and 1 and 3 months after the surgery
did not change. By contrast, these concentrations significantly
decreased in the surgery group, showing statistically significant
differences in comparison to the baseline levels and those observed
prior to the surgery and in the sham-surgery group (P<0.05).
 | Table IV.Comparison of the serum concentrations
of nicotinamide adenine dinucleotide phosphate oxidase (NADPH-ox)
at each time point between the surgery and sham-surgery groups. |
Table IV.
Comparison of the serum concentrations
of nicotinamide adenine dinucleotide phosphate oxidase (NADPH-ox)
at each time point between the surgery and sham-surgery groups.
| NADPH-ox
concentration, ng/ml |
|---|
|
|
|---|
| Group | Baseline | Post-model
establishment | 1 week
post-surgery | 1 month
post-surgery | 3 months
post-surgery |
|---|
| Surgery | 1.25±0.13 |
1.67±0.16a |
1.37±0.19a–c |
1.35±0.19a–c |
1.35±0.18a–c |
| Sham-surgery | 1.30±0.11 |
1.63±0.14a |
1.60±0.28a |
1.63±0.23a |
1.63±0.22a |
 | Table V.Comparison of the serum
malondialdehyde (MDA) concentrations at each time point between the
surgery and the sham-surgery groups. |
Table V.
Comparison of the serum
malondialdehyde (MDA) concentrations at each time point between the
surgery and the sham-surgery groups.
| MDA concentration,
nmol/ml |
|---|
|
|
|---|
| Group | Baseline | Post-model
establishment | 1 week
post-surgery | 1 month
post-surgery | 3 months
post-surgery |
|---|
| Surgery | 5.29±1.33 |
14.35±1.27a |
11.55±4.10a–c |
11.24±2.98a–c |
11.20±3.16a–c |
| Sham-surgery | 5.11±1.50 |
15.00±1.88a |
15.05±1.96a |
15.26±2.79a |
15.22±1.81a |
Changes in serum eNOS and NO
concentrations following radiofrequency RSD
Comparison of the baseline serum concentrations of
eNOS and NO in the surgery and the sham-surgery groups did not
demonstrate statistically significant differences (P>0.05)
(Tables VI and VII). Following model establishment, the
serum concentrations of eNOS and NO in these two groups were
significantly increased compared to the baseline level (P<0.05);
however, there was no difference between these two groups
(P>0.05). The serum concentrations of eNOS and NO in the
sham-surgery group at 1 week, and 1 and 3 months after surgery did
not change. By contrast, the concentrations in the surgery group
significantly decreased and showed significant differences in
comparison to the baseline levels and those observed prior to the
surgery and in the sham-surgery group (P<0.05).
 | Table VI.Comparison of the serum endothelial
nitric-oxide synthase (eNOS) concentrations at each time point
between the surgery and the sham-surgery groups. |
Table VI.
Comparison of the serum endothelial
nitric-oxide synthase (eNOS) concentrations at each time point
between the surgery and the sham-surgery groups.
| eNOS concentration,
U/ml |
|---|
|
|
|---|
| Group | Baseline | Post-model
establishment | 1 week
post-surgery | 1 month
post-surgery | 3 months
post-surgery |
|---|
| Surgery | 11.26±1.49 |
5.85±1.49a |
8.86±2.33a–c |
9.00±2.33a–c |
9.00±2.04a–c |
| Sham-surgery | 11.38±1.78 |
6.16±1.60a |
6.19±2.00a |
6.07±1.53a |
6.13±1.59a |
 | Table VII.Comparison of the serum
concentrations of nitric oxide (NO) at each time point between the
surgery and the sham-surgery groups. |
Table VII.
Comparison of the serum
concentrations of nitric oxide (NO) at each time point between the
surgery and the sham-surgery groups.
| NO concentration,
µmol/l |
|---|
|
|
|---|
| Group | Baseline | Post-model
establishment | 1 week
post-surgery | 1 month
post-surgery | 3 months
post-surgery |
|---|
| Surgery | 95.37±6.69 |
52.45±8.65a |
68.53±9.65a–c |
69.13±7.83a–c |
69.42±9.08a–c |
| Sham-surgery | 95.36±8.08 |
55.30±8.56a |
57.31±9.36a |
52.68±5.51a |
52.66±11.78a |
Safety of radiofrequency RSD
There were no deaths in the surgery or sham-surgery
groups. Three dogs developed hematomas at the puncture sites,
although following pressure depressing and bandaging, there were no
sequelae. During ablation, two dogs experienced renal artery spasms
and their symptoms were relieved 10 min after the injection of
nitroglycerin. Radiography was performed immediately following the
radiofrequency RSD surgery and there was no evidence of renal
artery dissection. The serum creatinine level was examined 3 days,
1 and 2 weeks, and 1 and 3 months after the surgery and the results
were all normal. Additionally, renal arteriography was performed
again at 3 months after the surgery and no stenosis was
observed.
Discussion
Hypertension is a common cardiovascular disease and
the leading risk factor for cardiovascular mortalities in China.
This disease not only severely endangers human health but also
creates a tremendous burden to the community. To thoroughly
investigate the pathogenesis and treatment methods for
hypertension, a number of hypertension experimental animal models
have been established. Lohmeier et al (4) provided dogs a high-fat diet for 4
weeks, which led to increases in body weight that were 1.5 times
greater than that of the control group and an increased MAP of 17±3
mmHg, indicating successful establishment of a hypertension model.
This model is not only stable and has a high success rate but also
possesses characteristics similar to human hypertension. In the
present study, beagle dogs were selected as study subjects.
Following feeding with a high-fat diet for 12 weeks, the blood
pressure levels in the two groups of animals significantly
increased (P<0.05), indicating that the hypertension model was
established successfully. The increase in sympathetic nerve
activity is the most important factor contributing to the elevation
of blood pressure. The sympathetic nervous system can activate the
RAS and AngII can activate the presynaptic angiotensin II type 1
receptor to promote the release of catecholamines, which can in
turn indirectly activate sympathetic nerve activity to cause
increased blood pressure and form a vicious cycle. As one of the
most important active biological molecule in RAS, AngII plays
significant roles in vasoconstriction and water-sodium retention
and its level can partially reflect sympathetic nerve activity. The
present study showed that the serum AngII levels in the two groups
of dogs following successful model establishment significantly
increased from the baseline level (P<0.05), although the serum
AngII level in the sham-surgery group always maintained a higher
level. These results suggested that activation of the RAS occurred
in the high-fat-diet-induced hypertension model and that the
increase in blood pressure in this dog model was significantly
associated with activation of the RAS. The results of the study
also showed that serum NADPH-ox and MDA levels increased, whereas
eNOS and NO production significantly decreased in this dog model.
The increase in NADPH-ox and MDA levels may reflect the activation
of oxidative stress and the decrease in eNOS and NO typically
reflects damage associated with vascular endothelial function.
Therefore, these results indicate that oxidative stress and
endothelial dysfunction may also play important roles in the
development of hypertension in this dog model.
Blood pressure was measured at each time point
following radiofrequency RSD and the results showed that within 2
weeks of the intervention the blood pressure of the surgery and
sham-surgery groups decreased. The decrease in blood pressure in
the surgery group was more evident, which may be associated with
the influence of surgical strike and anesthetic agents. The blood
pressure of the sham-surgery group gradually recovered to the
preoperative level, whereas that in the surgery group gradually
decreased, indicating that radiofrequency RSD had an
antihypertensive effect that emerged as soon as 3 days after the
surgery. The antihypertensive effect gradually increased with time
and reached a relatively stable level 1 month after the surgery and
this antihypertensive effect was maintained at 2 and 3 months after
the surgery. In addition, the experimental data showed that the
changing trends of SAP, DAP and MAP in the surgery group following
the surgery were consistent with each other, indicating that
radiofrequency RSD reduced SAP, DAP and MAP, consistent with
previous international studies (5,
6). However, the long-term
antihypertensive effect of this procedure requires further
observation. Radiofrequency RSD selectively transects renal
sympathetic nerves to inhibit sympathetic nerve activity, thus
affecting the release of catecholamines. In the study by Krum et
al (1), the release of
norepinephrine decreased by an average of 47% following
radiofrequency RSD. Allen (7) also
confirmed that renal denervation reduced renal sympathetic nerve
activity, enhanced the functions of urinary sodium excretion and
diuresis and decreased renin release. In addition, studies have
shown that the levels of catecholamine, renin and AngII in the
circulation can partially reflect sympathetic nerve activities. The
present study showed that the serum AngII levels at 1 week, and 1
and 3 months after radiofrequency RSD were significantly decreased
compared to those observed prior to the surgery (P<0.05);
additionally, these levels paralleled the decrease in blood
pressure, whereas these levels in the sham-surgery group
continuously increased. These results confirmed that the decrease
in blood pressure observed in hypertensive dogs was associated with
RAS inhibition caused by the reduction of sympathetic activity.
NADPH-ox is an important oxidase in the body that
consists of numerous subunits, including p22phox, gp91phox, p47phox
and Rac2 (8). NADPH-ox is the main
source of oxidative stress in the vascular system. A number of
studies have shown that primary hypertension patients and
spontaneously hypertensive rats have higher levels of NADPH-ox and
produced a greater amount of reactive oxygen species (ROS) compared
to the control group. As the detection of ROS is difficult, MDA was
detected, which is more representative of the level of oxidative
stress in the body (9). Oxidative
stress and the sympathetic nervous system are closely associated.
An increase in the ROS level can activate the RAS and sympathetic
nerve system (10) and sympathetic
nervous excitement can also increase the activity of NADPH-ox,
possibly through influencing α 1-adrenergic-receptor-mediated
activation of the phospholipase C and protein kinase C pathways
(11). If oxidative stress can be
effectively inhibited during the pathogenesis of hypertension,
hypertension may be effectively prevented and treated. Rafiq et
al (12) found that
radiofrequency RSD in rats with aortic regurgitation led to a
reduction in renal norepinephrine, angiotensinogen and AngII, as
well as an improvement in oxidative stress. The present study
showed that in the high-fat diet-induced hypertension model, the
AngII level decreased following radiofrequency RSD. In addition,
the serum NADPH-ox and MDA levels were significantly decreased at
each time point following the surgery compared to those measured
prior to the surgery (P<0.05). Compared to the levels in the
sham-surgery group, the levels of these factors at 1 and 3 months
after the surgery were significantly decreased (P<0.05),
indicating that blockade of the renal sympathetic nerves inhibited
oxidative stress.
Vascular endothelial cells secrete various
vasoactive substances, including NO, which is the most important
vasodilator in the body. Studies have shown that damage to
endothelial function is associated with a decrease in
endothelium-dependent NO activity and thus decreased NO release can
be used as a marker of endothelial injury. As a necessary enzyme
for NO synthesis, eNOS shares certain trends with NO. For example,
hemodynamic pressure changes caused by hypertension can reduce NOS
activity and damage NO synthesis, thus resulting in endothelial
dysfunction (13). Hypertension and
eNOS are also closely associated. Kayhan et al (14) found that the E298D polymorphism of
eNOS can increase the risk of hypertension and eNOS-knockout mice
were also shown to develop hypertension (15). The present study showed that the
serum levels of eNOS and NO in hypertensive dogs were significantly
lower than those in the control group, suggesting that hypertensive
dogs had damaged vascular endothelial function. One possible reason
for this result was that the increased synthesis and secretion of
AngII may have increased the NADH/NADPH-ox activity in the
endothelium and vascular smooth muscle membrane, thus increasing
vascular hydroxyl radicals to damage endothelium-dependent
vasorelaxation. Vascular endothelial dysfunction is an early
pathological change in numerous cardiovascular diseases. If the
damaged vascular endothelial function can be improved along with
the antihypertensive effect, the occurrence of complications of
hypertension can be effectively postponed or prevented. Currently,
it is generally believed that the mechanism underlying endothelial
cell damage induced by hypertension is mediated by AngII. For
example, AngII can cause endothelial dysfunction through the
activation of oxidative stress and oxidative stress-dependent
signaling pathways. The present study showed that the serum levels
of eNOS and NO in the surgery group were significantly higher than
those in the sham-surgery group at each time point following
radiofrequency RSD, suggesting that damaged vascular endothelial
function was improved by radiofrequency RSD. Additionally, the
steadily decreased level of AngII may not only improve endothelial
function through the reduction of blood pressure, but also through
the relief of oxidative stress and vasoconstriction.
In conclusion, in the high-fat-diet-induced
hypertension dog model, activation of the RAS, enhancement of
oxidative stress and endothelial dysfunction may serve as
mechanisms underlying the elevation of blood pressure.
Radiofrequency RSD not only persistently reduced the levels of SAP,
DAP and MAP in hypertensive dogs, but also reduced the serum
concentrations of AngII, NADPH-ox and MDA and increased the levels
of eNOS and NO. These results indicate that radiofrequency RSD may
significantly reduce blood pressure in hypertensive dogs through
the inhibition of the RAS and oxidative stress response and the
improvement of vascular endothelial function by suppressing
sympathetic activity. These results may provide an experimental and
theoretical basis for the antihypertensive mechanism and target
organ protection provided by catheter-based radiofrequency RSD.
The limitations of the study include the small
samples size and insufficient postoperative observation time due to
difficulties in the manipulation in large animals and the long-term
antihypertensive effect of radiofrequency RSD. In addition, the
mechanism underlying the antihypertensive effect of catheter-based
radiofrequency RSD is complex and multifactorial; therefore, this
topic requires further in-depth and long-term studies.
Acknowledgements
The present study was supported by Key Project
(grant no. 2012WK2002) and Science and Technology Plan (grant no.
2014FJ3097) of Science and Technology Bureau, Hunan, China.
References
|
1
|
Krum H, Schlaich M, Whitbourn R, et al:
Catheter-based renal sympathetic denervation for resistant
hypertension: a multicentre safety and proof-of-principle cohort
study. Lancet. 373:1275–1281. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Krum H, Schlaich MP, Sobotka PA, et al:
Percutaneous renal denervation in patients with treatment-resistant
hypertension: final 3-year report of the Symplicity HTN-1 study.
Lancet. 383:622–629. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Papademetriou V, Doumas M and Tsioufis K:
Renal sympathetic denervation for the treatment of
difficult-to-control or resistant hypertension. Int J Hypertens.
2011:1965182011.PubMed/NCBI
|
|
4
|
Lohmeier TE, Iliescu R, Liu B, et al:
Systemic and renal-specific sympathoinhibition in obesity
hypertension. Hypertension. 59:331–338. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Symplicity HTN-1 Investigators, .
Catheter-based renal sympathetic denervation for resistant
hypertension: durability of blood pressure reduction out to 24
months. Hypertension. 57:911–917. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Symplicity HTN-2 Investigators, . Esler
MD, Krum H, et al: Renal sympathetic denervation in patients with
treatment-resistant hypertension (The Symplicity HTN-2 Trial): a
randomised controlled trial. Lancet. 376:1903–1909. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Allen TR: Current status of lumbar
sympathectomy. Am Surg. 42:89–91. 1976.PubMed/NCBI
|
|
8
|
Babior BM: NADPH oxidase: an update.
Blood. 93:1464–1476. 1999.PubMed/NCBI
|
|
9
|
Maboudou P, Mathieu D, Bachelet H, et al:
Detection of oxidative stress. Interest of GC-MS for
malondialdehyde and formaldehyde monitoring. Biomed Chromatogr.
16:199–202. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Carlson SH and Wyss JM: Neurohormonal
regulation of the sympathetic nervous system: new insights into
central mechanisms of action. Curr Hypertens Rep. 10:233–240. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
DiBona GF and Kopp UC: Neural control of
renal function. Physiol Rev. 77:75–197. 1997.PubMed/NCBI
|
|
12
|
Rafiq K, Noma T, Fujisawa Y, et al: Renal
sympathetic denervation suppresses de novo podocyte injury and
albuminuria in rats with aortic regurgitation. Circulation.
125:1402–1413. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Beevers G, Lip GY and O'Brien E: ABC of
hypertension: the pathophysiology of hypertension. BMJ.
322:912–916. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kayhan FE, Koldemir M, Cagatay P, et al:
Prevalence of endothelial nitric oxide synthase E298D polymorphism
in Turkish patients with essential hypertension. Diabetes Metab
Syndr. 7:12–16. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rees DD, Palmer RM and Moncada S: Role of
endothelium-derived nitric oxide in the regulation of blood
pressure. Proc Natl Acad Sci USA. 86:3375–3378. 1989. View Article : Google Scholar : PubMed/NCBI
|