Introduction
A cytological examination using the vitreous fluid
based on the clinical ocular findings is important for differential
diagnoses between intraocular lymphoma (IOL) and uveitis (1,2). The
diagnostic probability by the cytological examinations, however,
varies in each IOL case (1,3). Due to the uncertain results in
cytological analysis with vitreous fluid, studies have reported
that measurements of interleukin (IL)-6 and -10 concentrations in
the vitreous can be used to identify IOL (1). A recent basic study demonstrated that not
only the IL-10/-6 ratio, but also a combination of other cytokine
analyses in intraocular fluid, may contribute to an accurate
diagnosis for uveitis/IOL (4).
Although undiluted vitreous fluid may be an appropriate material
for cytokine analysis, the undiluted fluid obtained by vitrectomy
or probing from the pars plana is critically limited in volume.
Therefore, cytokine analysis using vitreous fluid for clinical or
basic study has yet to be elucidated. Therefore, the present study
reports 2 patients diagnosed with panuveitis who underwent
vitrectomy. Additionally, to the best of our knowledge, this is the
first report showing IL-6 and -10 concentrations in the undiluted
vitreous fluid and vitreous infusion fluid, which were
simultaneously examined in the same patients.
Case reports
Patient 1
An 81-year-old female had complained of blurred
vision in both eyes for 3 months. The patient was referred to the
Teine Keijinkai Hospital (Sapporo, Hokkaido, Japan) for evaluation
and management on October 7, 2013. The patient provided written
informed consent. Visual acuity was 0.5 right eye [oculus dexter
OD)] and 0.01 left eye [oculus sinister (OS)]. Intraocular pressure
was normal. Slit-lamp examination revealed 1+ flare and 1+ cells in
the anterior chamber with keratic precipitates oculus uterque (OU).
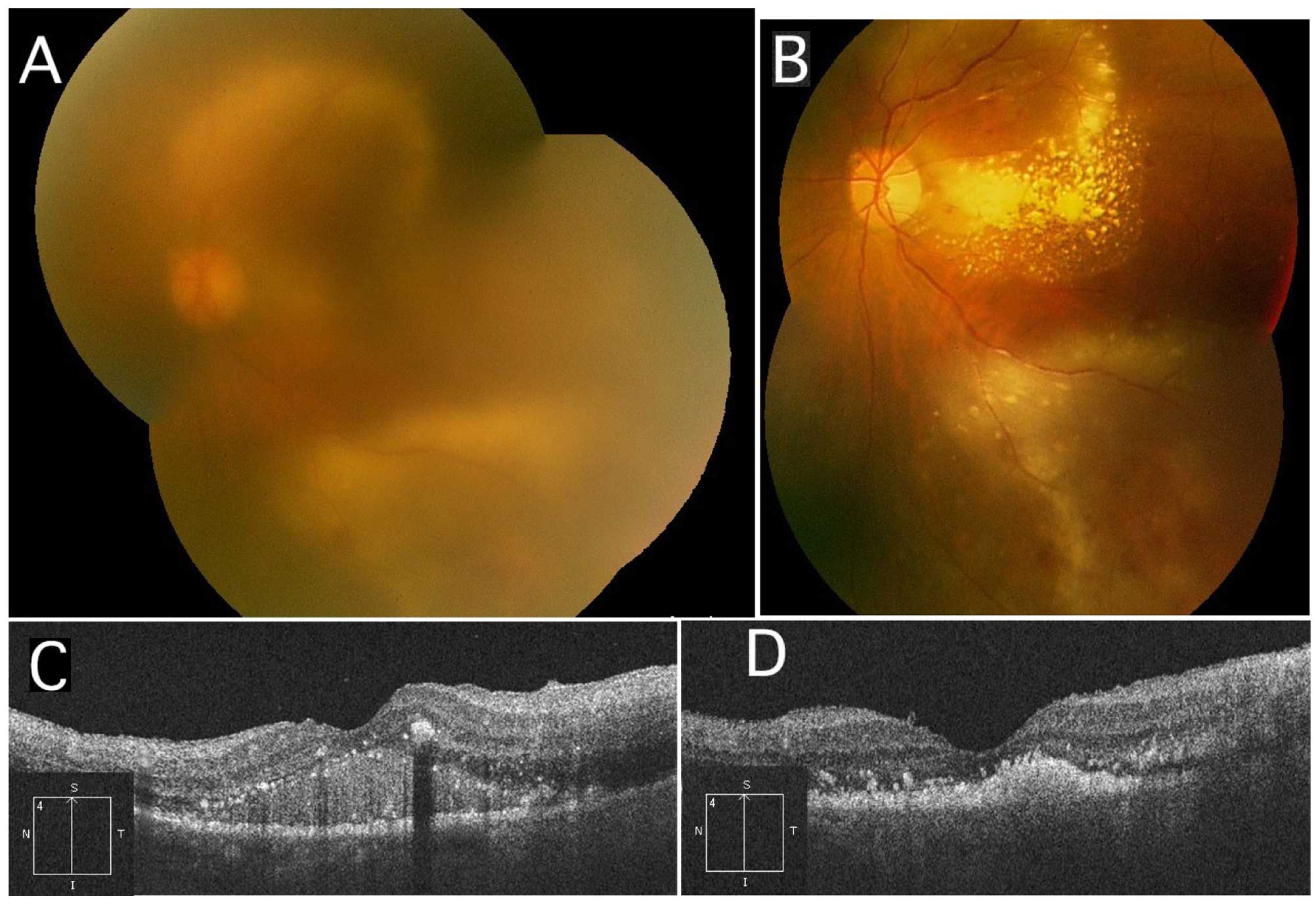
Fundus examination demonstrated marked diffuse vitreous opacity and
subretinal exudates with an unclear margin (Fig. 1A). Fluorescein angiography revealed
multiple leakages from subretinal exudates. Optical coherence
tomography (OCT) exhibited submacular fluids filled with high
reflective lesions (Fig. 1B). Results
in serological tests and systemic imaging modalities were not
noteworthy. Therefore, it was mandatory to make differential
diagnoses of panuveitis or IOL in this case. A 23-guage pars plana
vitrectomy was conducted in the left eye on October 15. Prior to
performing core vitrectomy, undiluted anterior vitreous fluid was
gained while an infusion system was stopped and the pressure was
carefully maintained by indentation of the sclera to prevent the
eyeball from collapsing. On that occasion, the indentation of the
sclera by a scleral depressor made it easier to gather vitreous gel
and fluid near the vitreous base. Subsequently, central vitreous
gel and fluid were removed with an active infusion system. IL-6 and
-10 concentrations were determined by a conventional enzyme linked
immunosorbent assay system. The patient was administered 80 mg
methyl-prednisolone intravenously for 2 days, which was thereafter
changed to oral administration of 40 mg prednisolone, which was
tapered gradually. Fundus showed marked hard exudates within the
arcade together with reduced subretinal lesions and vitreous
opacity (Fig. 1C). OCT exhibited
resolution of submacular lesions (Fig.
1D). Visual acuity improved to 0.05 OS in November 2013.
Patient 2
A 79-year-old female had complained of blurred
vision in both eyes following cataract surgery in 2012. The patient
provided written informed consent. Visual acuity was 0.4 OU.
Intraocular pressure was normal. Slit-lamp examination revealed 1+
flare and 1+ cells in the anterior chamber with keratic
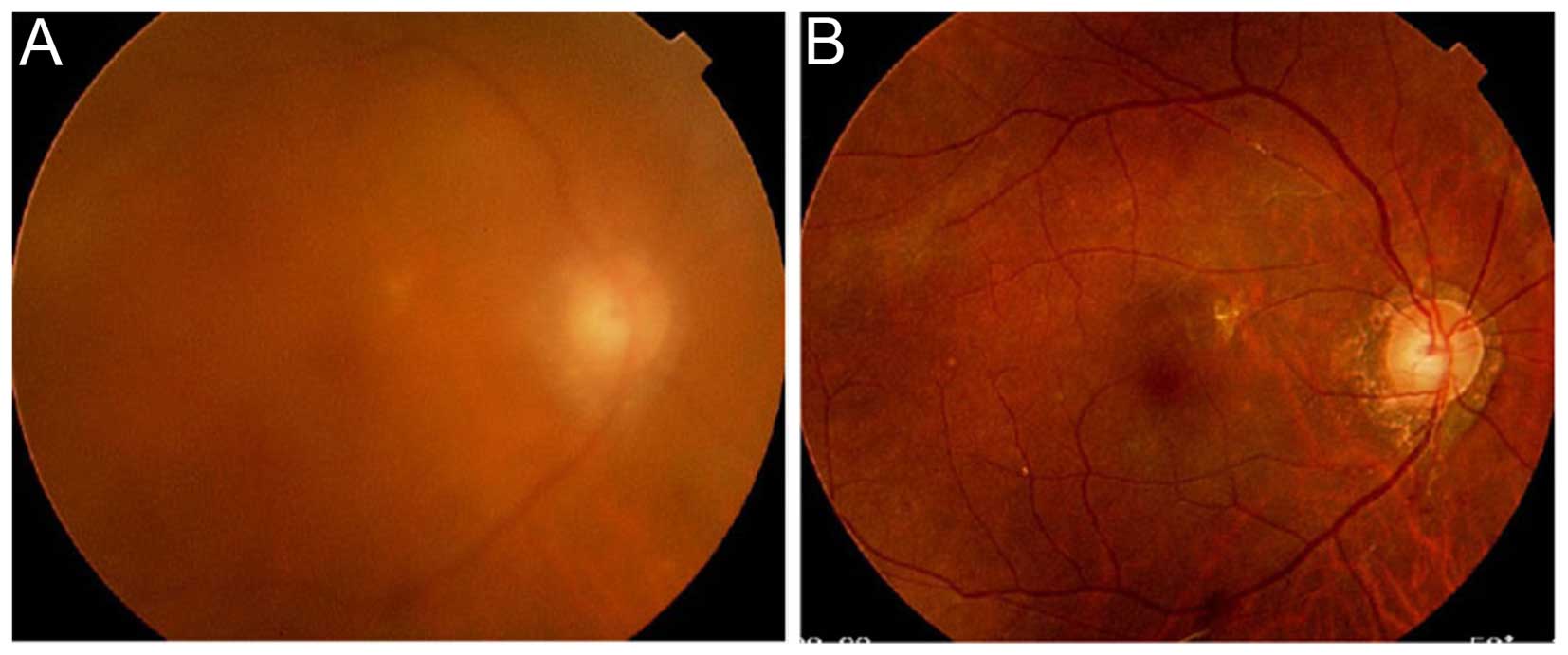
precipitates OU. Fundus examination demonstrated diffuse vitreous
opacity, and subretinal hemorrhage and exudates (Fig. 2A). Fluorescein angiography revealed
several leakages from the retinal vessels. OCT exhibited mild
macular edema OS. The patient was administered 30 mg oral
corticosteroid for 3 months; however, the vitreous opacity and
exudates were not resolved. A 23-guage pars plana vitrectomy was
conducted to make a diagnosis in the right eye in June 2014.
Undiluted anterior vitreous fluid was obtained by the same
vitrectomy way as in patient 1, however, not near the vitreous base
by indentation. Subsequently, diluted infusion fluid was gained.
The fluid was submitted for measurements of IL-6 and -10
concentrations, as described in patient 1. No additional treatments
were required and visual acuity remained 0.6 OD (Fig. 2B). Intraocular inflammation did not
recur during a follow-up period.
Interleukin concentrations
Approximately 800 µl of undiluted anterior vitreous
fluid was collected, whereas vitreous infusion fluid of 20 ml was
eventually collected following core vitrectomy in the two patients.
IL-6 concentrations were 513 and 106 pg/ml in the undiluted
vitreous and the infusion fluid in patient 1, and 263 and 29 pg/ml
in patient 2, respectively. By contrast, IL-10 was under the
detectable levels in all the fluids. Cytological examinations using
the infusion fluids showed numerous cluster of differentiation 68
(CD68)-positive macrophages infiltrating the vitreous, whereas
reactive CD3 and CD20-positive T and B-cells were not identified in
patient 1. A few small lymphoid cells were present in the fluid in
patient 2.
Discussion
In the present study, IL-6 and -10 in the undiluted
anterior vitreous fluid and infusion vitreous fluid were
simultaneously measured in 2 uveitis patients, showing that
concentrations of IL-6 in the former and latter fluid were 513 and
106 pg/ml in patient 1, and 263 and 29 pg/ml in patient 2,
respectively. By contrast, IL-10 concentrations were under the
detectable levels in the two cases. The IL-10/-6 ratio was <1 in
the two fluids in each patient. These findings strongly indicate
that severe inflammation was caused by uveitis rather than IOL
(1). The value of IL-6 concentration
was significantly high in the undiluted fluid, comparing with that
in the diluted infusion fluid in the two patients. Thus, the
present study potentially shows that the measurement of IL analysis
with vitreous fluid was useful for differential diagnosis between
uveitis and IOL. Furthermore, it is indicated that the dilution
rate of the concentrations in vitreous infusion fluid was different
among individuals, as this difference may be associated with the
infusion volume during vitrectomy or width of the vitreous fluid
removed. Therefore, in case of these analyses using the fluid
diluted with infusion water during vitrectomy, it is of note that
the values of cytokine concentration were too small in the diluted
vitreous infusion fluid as shown in the present study.
The values of IL-6 concentration in the undiluted
fluid were also different between the two cases. These results may
be based on the regional differences in IL-6 concentration within
the vitreous cavity, as peripheral vitreous gel and liquid were
clearly gathered to the vitreous base in patient 1 but not in
patient 2. By contrast, the severity in intraocular inflammation
was likely to be responsible for this difference.
In conclusion, measurements of IL concentrations in
vitreous infusion fluid provide with significant evidence on the
differential diagnosis between IOL and uveitis, when considering
how vitreous infusion fluid was diluted. Therefore, the present
study highlighted a novel application of cytokine analyses using
the vitreous infusion fluid, which may contribute to the
development of future translational research on uveitis/IOL
patients.
References
|
1
|
Kimura K, Usui Y and Goto H: Japanese
Intraocular Lymphoma Study Group: Clinical features and diagnostic
significance of the intraocular fluid of 217 patients with
intraocular lymphoma. Jpn J Ophthalmol. 56:383–389. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kase S, Namba K, Jin XH, Kubota KC and
Ishida S: Spontaneous regression of intraocular lymphoma.
Ophthalmology. 119:1083–1084. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sugita S, Takase H, Sugamoto Y, Arai A,
Miura O and Mochizuki M: Diagnosis of intraocular lymphoma by
polymerase chain reaction analysis and cytokine profiling of the
vitreous fluid. Jpn J Ophthalmol. 53:209–214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fisson S, Ouakrim H, Touitou V, Baudet S,
Ben Abdelwahed R, Donnou S, Miloudi A, Galand C, Bodaghi B, Lehoang
P, et al: Cytokine profile in human eyes: Contribution of a new
cytokine combination for differential diagnosis between intraocular
lymphoma or uveitis. PLoS One. 8:e523852013. View Article : Google Scholar : PubMed/NCBI
|