Introduction
The aim of bone defect reconstruction is to
regenerate bone loss and restore limb function (1). Several approaches can be adopted in the
clinic, including autologous bone graft, vascularized fibular
autograft and the Ilizarov bone transfer technique. Autologous bone
graft is not recommended for reconstruction of massive bone defects
due to its increased risk of resorption (2). Vascularized fibular autograft and the
Ilizarov bone transfer technique are the most frequently used
methods for reconstruction of extensive bone defects (3–5).
The Masquelet technique is another effective way to
repair extensive bone defects. This two-staged method for bone
reconstruction was first described by Masquelet et al in
1986 (6). The first-stage surgery
includes radical debridement of bone and soft tissues, followed by
implantation of a polymethylmethacrylate (PMMA) cement spacer at
the site of the bone defects. The cement spacer is expected to
obviate invasion of fibrous tissue at the recipient site
(mechanical role) and induce the surrounding membrane (biological
role) (7). After a duration of 6 to 8
weeks, a PMMA-induced pseudosynovial membrane formed. At the
second-stage surgery, the cement spacer is removed carefully in
order to maintain the already formed membrane and cause minimal
disturbance. Following this, the defect is filled with morcellised
cancellous autologous bone graft. Masquelet et al (6) reported that this method could repair a
bone defect of 25 cm in length.
Since the first study, the Masquelet technique has
been widely used to resolve massive bone defects caused by
different diseases and achieved clinical efficacy (8–12). However,
efficacy in the cases managed by the Masquelet technique does not
mean that this approach is optimal. The main disadvantage of this
technique is the PMMA cement spacer, which is not degradable and
requires a second surgery for removal. Additionally, the variable
antibiotic elution rates of PMMA may affect the antibacterial
effect. Furthermore, local implantation of PMMA may lead to a rise
in temperature, which limits its combination with heat-sensitive
antibiotics (13).
In recent years, calcium sulfate has been used
clinically as a delivery vehicle and bone substitute due to its
superiorities over PMMA. Firstly, calcium sulfate can be totally
degraded, entirely with its antibiotic load. Secondly, the rise in
temperature is minimal when using calcium sulfate combined with
antibiotics. Finally, no residual foreign body remains once the
antibiotics have been eluted, reducing the risk of biofilm
infections (13).
The present study assessed whether if PMMA is
replaced by calcium sulfate as a cement spacer in the Masquelet
technique, reconstruction of bone defects may be achieved through
one-stage surgery. We hypothesize that this one-stage surgery may
consist of three essential steps. The first step is radical
debridement of bone and surrounding soft tissues. The second step
is mixing calcium sulfate, with or without morcellised cancellous
autologous bone or other bone substitutes, and optional additives
at a correct ratio. Additives include, but are not limited to,
antibiotics, platelet-rich plasma (PRP) and mesenchymal stem cells
(MSCs). The last step is stabilization of the bone with appropriate
types of fixations.
Case report
Calcium sulfate can induce the
formation of membrane
A 24-year-old male had a main complaint of pain with
limited activity of the bilateral feet subsequent to falling down
from a height of ~12 m. Physical examinations and radiology tests
proved that the patient had multiple fractures all over the body.
The present report only focuses on the clinical management of the
right foot where an open fracture of the calcaneus was identified
(type II of the Gustilo-Anderson classification; with a wound in
the planta without loss of soft tissue), closed fractures of the
talus neck (type IV of the Hawkins classification), navicular and
cuboides, and dislocations of the calcaneocuboid and talonavicular
joints (Fig. 1). The patient initially
received debridement for the calcaneus with limited internal
fixations for the fractures of the talus, navicular and cuboides,
as well as dislocated joints (Fig. 2).
Postoperatively, aggravating exudation with suppuration occurred at
the calcaneal wound and diagnosis of calcaneal infection was
established accordingly. One month after the first surgery, the
patient underwent pin removal and once more radical debridement of
the right calcaneus. Subsequently, local calcium sulfate (Stimulan
Rapid Cure; Biocomposites, Ltd., Staffordshire, UK) with vancomycin
was implanted at the defect site of the calcaneus (Fig. 3). Approximately 8 weeks after the
second surgery, the patient returned for further treatment of the
bone defect. X-rays of the right foot clearly showed formation of
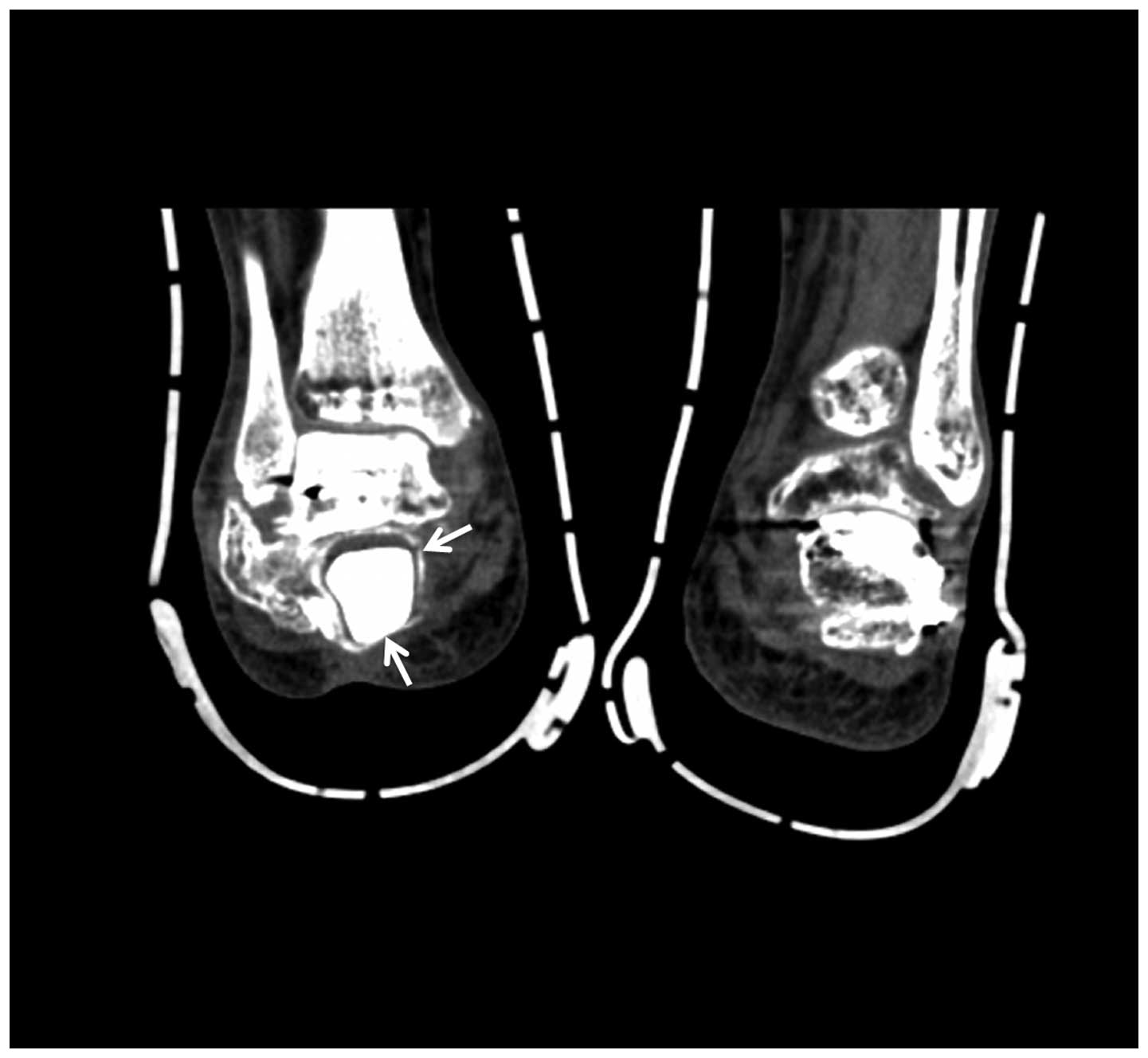
an induced membrane around the calcaneus (Fig. 4). A computed tomography scan (Fig. 5) also confirmed the existence of the
membrane. A one-stage strategy was not performed in this patient
due to the following considerations: i) A two-stage surgery was
originally planned, therefore, the defect was filled with only
calcium sulfate and antibiotics. Considering the large bone
defects, we believed that it would be more appropriate to
reconstruct the defect with bone graft. ii) The patient preferred
the reconstruction of the bone defect with autogenous bone graft.
Finally, the calcium sulfate was carefully removed and the defect
was filled with autogenous iliac crest. Postoperatively, there was
no recurrence of local infection. However, due to the severe
injury, although the wound recovered well, there remained
deformities, such as the loss of Bohler and Gissane angles and
decreased calcaneal height at one year follow-up time (Fig. 6).
Possibility of one-stage surgery
The evidence for the possibility of one-stage
surgery included the following aspects. i) Unique biological
superiority of calcium sulfate. The advantages of calcium
sulfate-based cement include biodegradability, biocompatibility,
osteoconductivity and non-exothermic setting reactions (14), of which total biodegradability is the
most important as it provides a vital foundation for one-stage
surgery. ii) Good clinical efficacy of calcium sulfate as a bone
substitute. In a previous study regarding the use of calcium
sulfate as a bone graft substitute to repair bone defects ranging
from 13–138 cm3, Kumar et al (15) concluded that calcium sulfate is a safe,
efficient and easily available bone graft substitute for the
treatment of osseous defects. Similarly, in a 3-year randomized
controlled trial, Di Alberti et al (16) also reported good outcomes of calcium
sulfate as a carrier for regeneration of human bone defects.
Whether autologous bone or other bone substitutes should be used or
not depends on the defect size. If a bone defect is limited, only
calcium sulfate may be enough for reconstruction. When a bone
defect is extensive, autologous bone or other bone substitutes
[such as recombinant human bone morphogenetic protein 2 (rhBMP-2)]
can be used in combination with calcium sulfate (17). Of note, radical debridement of the bone
and surrounding soft tissues is the premise of the following
surgical procedures. iii) With regards to the definitive outcomes
of the combination of calcium sulfate with additives in
reconstruction of bone defects, Howlin et al (18) identified that calcium sulfate with
antibiotics may have a potential ability to reduce or eliminate
biofilm formation on adjacent periprosthetic tissue and prosthesis
material, thus reducing the rates of periprosthetic infection.
Following the comparison of PMMA with calcium sulfate as antibiotic
carriers at the infected sites, McConoughey et al (13) indicated that calcium sulfate led to
similar or improved outcomes compared to PMMA in the inhibition of
bacterial growth. In a pilot study regarding the assessment of
clinical outcomes of grafted sockets using either calcium
sulfate-PRP or calcium sulfate alone in the socket preservation
procedure, Cheah et al (19)
reported that calcium sulfate-PRP-grafted sites had a higher
mineralized bone content compared to the calcium sulfate-grafted
sites. In a rat experiment, He et al (20) found that the combination of injectable
nano calcium sulfate/alginate paste and BMP2-gene-modified MSCs may
be a new and effective strategy for repair of bone defects.
Discussion
Although the Masquelet technique was initially
designed for the treatment of bone defects caused by infection, it
has now been widely used for the reconstruction of bone defects
caused by other disorders. Gouron et al (8) and Pannier et al (9) reported its use in the treatment of
congenital pseudarthrosis of the tibia, which resulted in
satisfactory bony union. Villemagne et al (10) adopted this method to reconstruct the
long bone defect following resection of the malignant bone tumor,
indicating that this simple and reliable technique may lead to
promising clinical outcomes.
Previous studies have reported its application
mainly for the defects in the long bones. Recently, this technique
was also used for repair defects in the foot and hand. Makridis
et al (21) used this technique
to repair an extensive defect of the first metatarsal bone in a
53-year-old man, who was able to conduct normal daily activities
with no pain 18 months postoperatively. Flamans et al
(22) used this approach for hand and
wrist bone defects in 11 cases, 9 of which achieved bone union with
no septic complications at the 1-year follow up.
Recently, investigations addressing the similarities
and differences between PMMA and calcium sulfate as two types of
cement spacer have drawn wide attention. In an in vitro
study, McConoughey et al (13)
found that calcium sulfate beads achieved similar or a more
improved efficacy compared to the PMMA beads in inhibiting
bacterial growth. Grimsrud et al (23) reported similar characteristics of in
vitro elution between voriconazole-loaded PMMA bone cement and
calcium sulfate bone substitute. A prospective, randomized clinical
trial (24), which compared the
clinical efficacy of antibiotic-impregnated calcium sulfate with
antibiotic-impregnated PMMA for the treatment of chronic
osteomyelitis and infected nonunion, revealed that calcium sulfate
was equivalent to PMMA in efficacy of eradicating infection, but
required fewer subsequent surgical procedures. In a biomechanical
pull-out strength test regarding the two cement spacers used for
augmentation of a failed pedicle screw, Güler et al
(25) found that calcium sulfate
augmentation may not be as strong as PMMA augmentation.
Taken together, the previous and present studies
have confirmed that calcium sulfate, as a novel delivery vehicle,
possesses similar effectiveness as PMMA, but a clear characteristic
of total biodegradability, which highlights its superiority over
PMMA. However, it should be noted that calcium sulfate is less
strong than PMMA.
Currently, the differences between the PMMA-induced
membrane and calcium sulfate-induced membrane remain to be
elucidated. However, it is clear that the PMMA-induced
psedosynovial membrane is characterized by maturing vascularized
fibrous tissue (26), which secretes
several growth factors, including the vascular endothelial growth
factor, BMP-2 and transforming growth factor-β1. Whether the
calcium sulfate-induced membrane has similar characteristics
requires further studies. In addition, detailed differences between
the PMMA- and calcium sulfate-induced membranes should be further
explored.
Although in the present study, calcium sulfate was
able to induce the formation of membrane, numerous aspects remain
to be elucidated, such as changes to the induced membrane and the
generated space during the degradation process and following
degradation. In addition, the fluid is produced around the spacer
during the resorption of calcium sulfate; however, compositions of
the fluid as well as its effects on the surrounding bones and soft
tissues remain to be elucidated. Therefore, more studies should be
performed to improve the understanding of calcium sulfate and the
induced membrane.
In the present study concerning the repair of bone
defects, calcium sulfate was demonstrated to induce the formation
of a membrane similar to PMMA and we hypothesized that one-stage
surgery may be achieved to reconstruct bone defects with calcium
sulfate as a cement spacer. Future studies may develop the use of
this one-stage hypothesis.
Acknowledgements
The authors are grateful for the support of the
National Natural Science Foundation of China (grant no.
81572165).
Glossary
Abbreviations
Abbreviations:
|
PMMA
|
polymethylmethacrylate
|
|
PRP
|
platelet-rich plasma
|
|
CT
|
computed tomography
|
|
MSCs
|
mesenchymal stem cells
|
|
BMP-2
|
bone morphogenetic protein 2
|
References
|
1
|
Giannoudis PV, Faour O, Goff T, Kanakaris
N and Dimitriou R: Masquelet technique for the treatment of bone
defects: Tips-tricks and future directions. Injury. 42:591–598.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weiland AJ, Phillips TW and Randolph MA:
Bone grafts: A radiologic, histologic, and biomechanical model
comparing autografts, allografts, and free vascularized bone
grafts. Plast Reconstr Surg. 74:368–379. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rigal S, Merloz P, Le Nen D, Mathevon H
and Masquelet AC: French Society of Orthopaedic Surgery and
Traumatology (SoFCOT): Bone transport techniques in posttraumatic
bone defects. Orthop Traumatol Surg Res. 98:103–108. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pederson WC and Person DW: Long bone
reconstruction with vascularized bone grafts. Orthop Clin North Am.
38:23–35. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tu Y, Ueng SW, Yeh W, Yen C and Wang K:
Reconstruction of post-traumatic long bone defect with vascularized
bone graft. J Orthop Trauma. 14:1382000. View Article : Google Scholar
|
|
6
|
Masquelet AC, Fitoussi F, Begue T and
Muller GP: Reconstruction of the long bones by the induced membrane
and spongy autograft. Ann Chir Plast Esthet. 45:346–353. 2000.(In
French). PubMed/NCBI
|
|
7
|
Pelissier P, Masquelet AC, Bareille R,
Pelissier SM and Amedee J: Induced membranes secrete growth factors
including vascular and osteoinductive factors and could stimulate
bone regeneration. J Orthop Res. 22:73–79. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gouron R, Deroussen F, Juvet M, Ursu C,
Plancq MC and Collet LM: Early resection of congenital
pseudarthrosis of the tibia and successful reconstruction using the
Masquelet technique. J Bone Joint Surg Br. 93:552–554. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pannier S, Pejin Z, Dana C, Masquelet AC
and Glorion C: Induced membrane technique for the treatment of
congenital pseudarthrosis of the tibia: Preliminary results of five
cases. J Child Orthop. 7:477–485. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Villemagne T, Bonnard C, Accadbled F,
L'kaissi M, de Billy B and de Gauzy Sales J: Intercalary segmental
reconstruction of long bones after malignant bone tumor resection
using primary methyl methacrylate cement spacer interposition and
secondary bone grafting: The induced membrane technique. J Pediatr
Orthop. 31:570–576. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wong TM, Lau TW, Li X, Fang C, Yeung K and
Leung F: Masquelet technique for treatment of posttraumatic bone
defects. ScientificWorldJournal. 2014:7103022014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Karger C, Kishi T, Schneider L, Fitoussi F
and Masquelet AC: French Society of Orthopaedic Surgery and
Traumatology (SoFCOT): Treatment of posttraumatic bone defects by
the induced membrane technique. Orthop Traumatol Surg Res.
98:97–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
McConoughey SJ, Howlin RP, Wiseman J,
Stoodley P and Calhoun JH: Comparing PMMA and calcium sulfate as
carriers for the local delivery of antibiotics to infected surgical
sites. J Biomed Mater Res B Appl Biomater. 103:870–877. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Koh I, López A, Helgason B and Ferguson
SJ: The compressive modulus and strength of saturated calcium
sulphate dihydrate cements: Implications for testing standards. J
Mech Behav Biomed Mater. 34:187–198. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kumar CY, Nalini KB, Menon J and Patro DK:
BH: Calcium sulfate as bone graft substitute in the treatment of
osseous bone defects, a prospective study. J Clin Diagn Res.
7:2926–2928. 2013.PubMed/NCBI
|
|
16
|
Di Alberti L, Tamborrino F, Lo Muzio L,
D'Agostino A, Trevisiol L, De Santis D, Nocini PF and Bertossi D:
Calcium sulfate barrier for regeneration of human bone defects. 3
years randomized controlled study. Minerva Stomatol. Jun
11–2013.(Epub ahead of print).
|
|
17
|
Chen H, Cui X, Yu X, Tian X, Zhang B, Tang
P and Wang Y: Effects of chitosan-coated pressed calcium sulfate
pellets combined with recombinant human bone morphogenetic protein
2 on bone formation in femoral condyle-contained bone defects. J
Craniofac Surg. 21:188–197. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Howlin RP, Brayford MJ, Webb JS, Cooper
JJ, Aiken SS and Stoodley P: Antibiotic-loaded synthetic calcium
sulfate beads for prevention of bacterial colonization and biofilm
formation in periprosthetic infections. Antimicrob Agents
Chemother. 59:111–120. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cheah CW, Vaithilingam RD, Siar CH,
Swaminathan D and Hornbuckle GC: Histologic, histomorphometric, and
cone-beam computerized tomography analyses of calcium sulfate and
platelet-rich plasma in socket preservation: A pilot study. Implant
Dent. 23:593–601. 2014.PubMed/NCBI
|
|
20
|
He X, Dziak R, Mao K, Genco R, Swihart M,
Li C and Yang S: Integration of a novel injectable nano calcium
sulfate/alginate scaffold and BMP2 gene-modified mesenchymal stem
cells for bone regeneration. Tissue Eng Part A. 19:508–518. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Makridis KG, Theocharakis S, Fragkakis EM
and Giannoudis PV: Reconstruction of an extensive soft tissue and
bone defect of the first metatarsal with the use of Masquelet
technique: A case report. Foot Ankle Surg. 20:e19–e22. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Flamans B, Pauchot J, Petite H, Blanchet
N, Rochet S, Garbuio P, Tropet Y and Obert L: Use of the induced
membrane technique for the treatment of bone defects in the hand or
wrist, in emergency. Chir Main. 29:307–314. 2010.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Grimsrud C, Raven R, Fothergill AW and Kim
HT: The in vitro elution characteristics of antifungal-loaded PMMA
bone cement and calcium sulfate bone substitute. Orthopedics.
34:e378–e381. 2011.PubMed/NCBI
|
|
24
|
McKee MD, Li-Bland EA, Wild LM and
Schemitsch EH: A prospective, randomized clinical trial comparing
an antibiotic-impregnated bioabsorbable bone substitute with
standard antibiotic-impregnated cement beads in the treatment of
chronic osteomyelitis and infected nonunion. J Orthop Trauma.
24:483–490. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Güler UO, Derincek A, Hersekli MA, Ozalay
M, Cinar BM and Acaroğlu E: Restoration of pull-out strength of the
failed pedicle screw: Biomechanical comparison of calcium sulfate
vs polymethylmethacrylate augmentation. Acta Orthop Traumatol Turc.
48:202–206. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Aho OM, Lehenkari P, Ristiniemi J,
Lehtonen S, Risteli J and Leskelä HV: The mechanism of action of
induced membranes in bone repair. J Bone Joint Surg Am. 95:597–604.
2013. View Article : Google Scholar : PubMed/NCBI
|