Introduction
Bone marrow-derived mesenchymal stem cells (BMSCs)
are multipotent stromal cells with the potential to differentiate
into a variety of cell types, including adipocytes, osteocytes,
cardiomyocytes and neurons (1).
Recently, BMSCs have been used to treat acute and chronic
myocardial infarction. Transplantation of BMSCs into the left
ventricle has been demonstrated to decrease the infarcted area,
inhibit left ventricular remodeling and improve cardiac function in
patients with myocardial infarction or animal models with heart
ischemia (2–5). Generally, BMSCs need to be induced
in vitro by special reagents for cardiomyogenic
differentiation. Transforming growth factor-β1 (TGF-β1) is one of
the most commonly used reagents for inducing the cardiomyogenic
differentiation of BMSCs (6–8). Previous studies have indicated that
TGF-β1 treatment in vitro promotes the transformation of
BMSCs into cardiomyocyte-like cells that express
cardiomyocyte-specific markers (6–8).
TGF-β1 is a growth factor with multiple functions.
It not only affects cell differentiation but also plays diverse
roles in regulating cell proliferation, migration, apoptosis and
autophagy (9–11). Previous studies have indicated that
TGF-β1 inhibits the proliferation of epithelial cells, cardiac
fibroblasts, hematopoietic cells and cancer cells but promotes the
proliferation of vascular smooth muscle cells, skin fibroblasts,
endothelial cells and other specialized cells (12–14).
TGF-β1 has also been demonstrated to induce the apoptosis of a wide
range of cells (15–17). Mitochondrial reactive oxygen species
(ROS) are a family of reactive molecules that can trigger cell
apoptosis by damaging mitochondrial DNA (18). It is known that TGF-β1 can induce
mitochondrial ROS production in numerous cell lineages (19). Our previous study showed that TGF-β1
induced BMSC senescence by promoting mitochondrial ROS generation
(20); however, whether TGF-β1
induces the apoptosis of BMSCs through the regulation of
mitochondrial ROS production has not been elucidated, and this
topic is a focus of the present study.
Materials and methods
Animals
A total of 6 male C57BL/6 mice (8 weeks old) were
obtained from the Experimental Animal Center of Xinxiang Medical
University (Xinxiang, China). The study protocol and animal use
were approved by the Ethics Committee of Xinxiang Medical
University. Animal treatment was strictly performed according to
the Guidelines of the Ministry of Science and Technology of the
People's Republic of China (approval no. 2006-398).
Isolation and culture of BMSCs
BMSCs were isolated and cultured according to a
recently published protocol (21).
The third-passage BMSCs were exposed to 0, 10 and 20 ng/ml
recombinant mouse TGF-β1 (Cell Signaling Technology, Inc., Danvers,
MA, USA) for 24 h, and cell proliferation, apoptosis and
mitochondrial ROS were subsequently measured.
MTT assay
BMSC viability was measured with an MTT assay kit
(American Type Culture Collection, Manassas, VA, USA) following
exposure to different concentrations of TGF-β1. The third-passage
BMSCs (3×103 cells/well) were placed in 96-well plates
and cultured with Dulbecco's modified Eagle's medium (DMEM) without
serum overnight. The next day, the medium was replaced with
complete DMEM (with 15% serum) supplemented with 0, 10 and 20 ng/ml
TGF-β1, and the cells were cultured for an additional 24 h. A total
of 10 µl MTT reagent was then added to each well and the plates
were incubated at 37°C for 2 h. Following incubation, MTT detergent
reagent (100 ml) was added to each well and the plates were
incubated at room temperature for 2 h in the dark. Finally,
absorbance at 570 nm was read using a plate reader (Bio-Rad
Laboratories, Inc., Hercules, CA, USA).
Apoptosis assay
Cell apoptosis was measured using DAPI (Beyotime
Institute of Biotechnology, Shanghai, China) staining. BMSCs
(1×105 cells/well) were seeded in 24-well plates with
round coverslips and exposed to 0, 10 and 20 ng/ml TGF-β1 for 24 h.
Following washing with phosphate-buffered saline (PBS), the cells
were fixed with buffered paraformaldehyde and incubated with 0.1%
Triton™ X-100 (Bao Biological Engineering Co., Ltd., Dalian, China)
for 10 min at room temperature. The cells were treated with
DNase-Free RNase (50 mg/ml) for 3 h at 37°C and then stained with 5
µM DAPI for 5 min at room temperature. Cell apoptosis was assessed
under a fluorescence microscope (Olympus Corp., Tokyo, Japan). The
cells with a condensed nucleus or a nucleus with irregular edges
were considered to be apoptotic.
Western blotting
Following treatment with different concentrations of
TGF-β1 for 24 h, proteins were extracted from the BMSCs using a
protein extraction kit containing 20 ml 5X lysis buffer, 0.5 ml
protease inhibitor, 0.5 ml phosphatase inhibitor and 0.5 ml
phenylmethylsulfonyl fluoride (Bao Biological Engineering Co.,
Ltd.). Protein concentrations were measured using a standard
Bradford protein assay method‥ Western blot analysis was performed
according to a recently published protocol (22). In brief, 20 µg proteins were mixed
with equal volume of 2X loading buffer (Bao Biological Engineering
Co., Ltd.) and heated at 95°C for 5 min. Proteins were separated
with 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis
(Bao Biological Engineering Co., Ltd), then transferred onto
polyvinylidene fluoride membranes (Bao Biological Engineering Co.,
Ltd). The membranes were blocked with 5% non-fat milk (Bao
Biological Engineering Co., Ltd) in Tris-buffered saline with
Tween-20 (TBS-T; Beijing Solarbio Science and Technology Co., Ltd.,
Beijing, China) and incubated with the following primary
antibodies: Rabbit polyclonal IgG anti-B-cell lymphoma 2 (Bcl-2;
1:1,000; sc-492; Santa Cruz Biotechnology, Inc., Santa Cruz, CA,
USA), rabbit polyclonal IgG anti-Bcl-2-associated X protein (Bax;
1:1,000; sc-493; Santa Cruz Biotechnology, Inc.), rabbit polyclonal
IgG anti-Annexin V (1:2,000; ab14196; Abcam, Cambridge, MA, USA) or
mouse monoclonal IgG anti-β actin (1:2,000; sc-47778; Santa Cruz
Biotechnology, Inc.) at 4°C overnight. Following washing with TBS-T
three times, the membranes were incubated with donkey anti-rabbit
IgG-horseradish peroxidase-conjugated secondary antibody (1:10,000;
sc-2313; Santa Cruz Biotechnology, Inc.) or donkey anti-mouse
IgG-horseradish peroxidase-conjugated secondary antibody (1:10,000;
sc-2314; Santa Cruz Biotechnology, Inc.) for 1 h at room
temperature. The immunoreactive bands were visualized with an
Enhanced Chemiluminescence Western Blotting Substrate Kit (Thermo
Fisher Scientific Inc., Waltham, MA, USA). The mean expression
levels of Annexin V, Bax and Bcl-2 in each group were calculated
using Image J software [National Institutes of Health (NIH),
Bethesda, MD, USA].
Mitochondrial ROS measurement
Mitochondrial ROS were measured by flow cytometry
following staining with MitoSOX™ Red mitochondrial superoxide
indicator (Invitrogen Life Technologies). The BMSCs were plated in
24-well plates, treated with different concentrations of TGF-β1 for
24 h and then detached using 2.5% trypsin digestion. Following
digestion, the cells were suspended in warm PBS and incubated with
5 µM MitoSOX reagent for 10 min at 37°C in the dark. The cells were
then washed thrice with PBS, and the mitochondrial ROS levels were
analyzed using flow cytometry (BD Biosciences, San Jose, CA,
USA).
Statistical analysis
Statistical analysis was performed with SPSS
software (version 16.0; SPSS Inc., Chicago, IL, USA). Data are
presented as the mean ± standard deviation. Univariate comparisons
of means were performed using one-way analysis of variance followed
by Tukey tests. P<0.05 was considered to indicate a
statistically significant difference.
Results
Effect of TGF-β1 on BMSC
viability
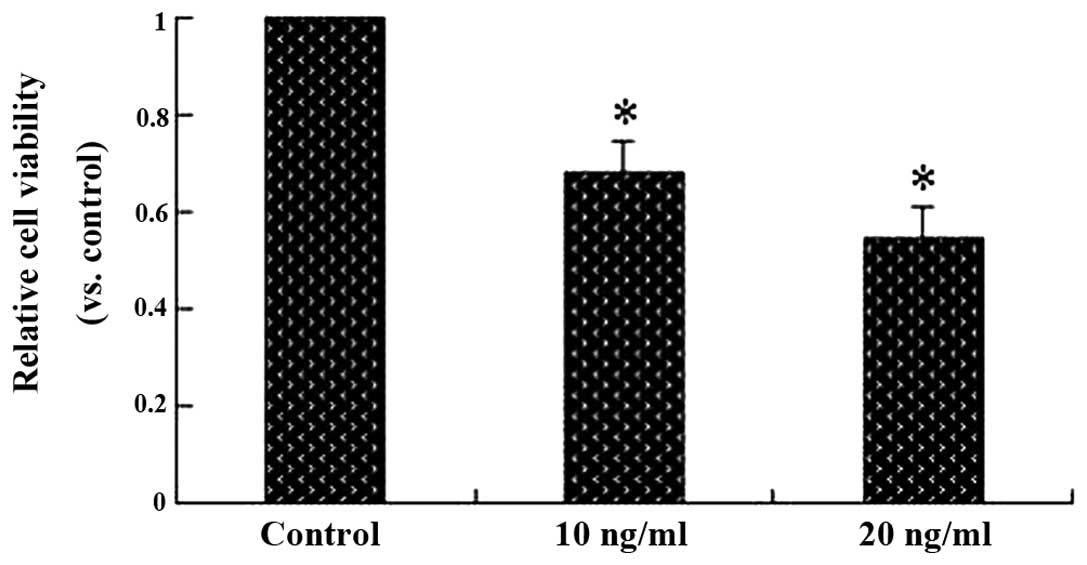
Compared with the control, treatment with 10 and 20
ng/ml TGF-β1 for 24 h significantly decreased BMSC viability
(Fig. 1).
Effect of TGF-β1 on apoptosis of
BMSCs
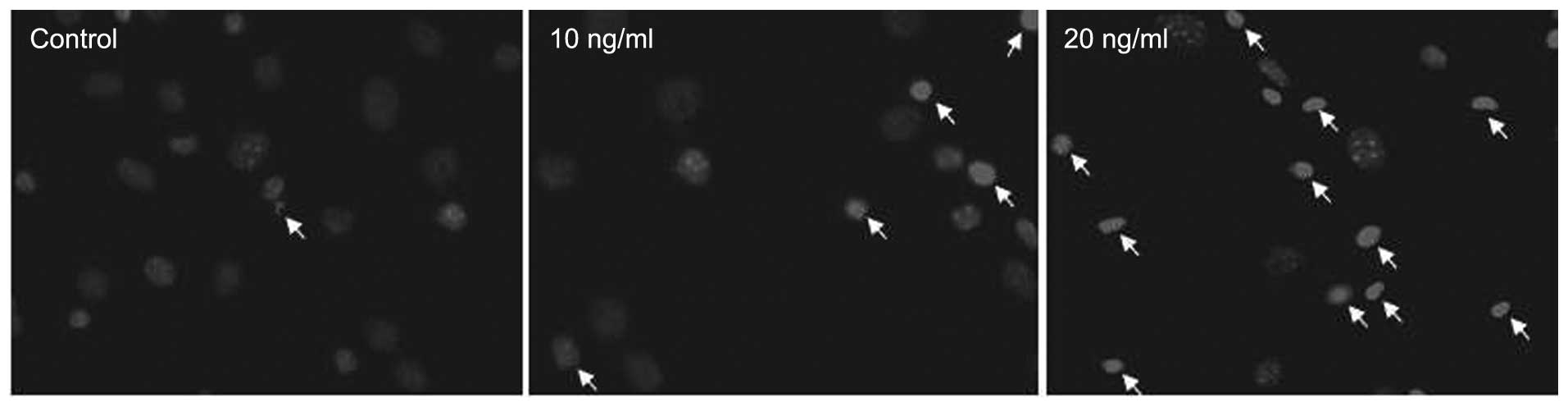
An increased number of cells with a condensed
nucleus or a nucleus with irregular edges (DAPI staining) was
observed in the TGF-β1 (10 and 20 ng/ml)-treated cells compared
with the control cells, which shows that TGF-β1 can stimulate BMSC
apoptosis (Fig. 2). The mean rate of
apoptosis in each group was calculated, and the results are shown
in Table I.
 | Table I.Rate of apoptosis in each group. |
Table I.
Rate of apoptosis in each group.
| Group | Rate of apoptosis
(%) |
|---|
| Control |
5.164±1.437 |
| 10 ng/ml TGF-β1 |
26.412±3.235a |
| 20 ng/ml TGF-β1 |
38.857±4.286a |
Effect of TGF-β1 on the expression of
apoptotic signals in BMSCs
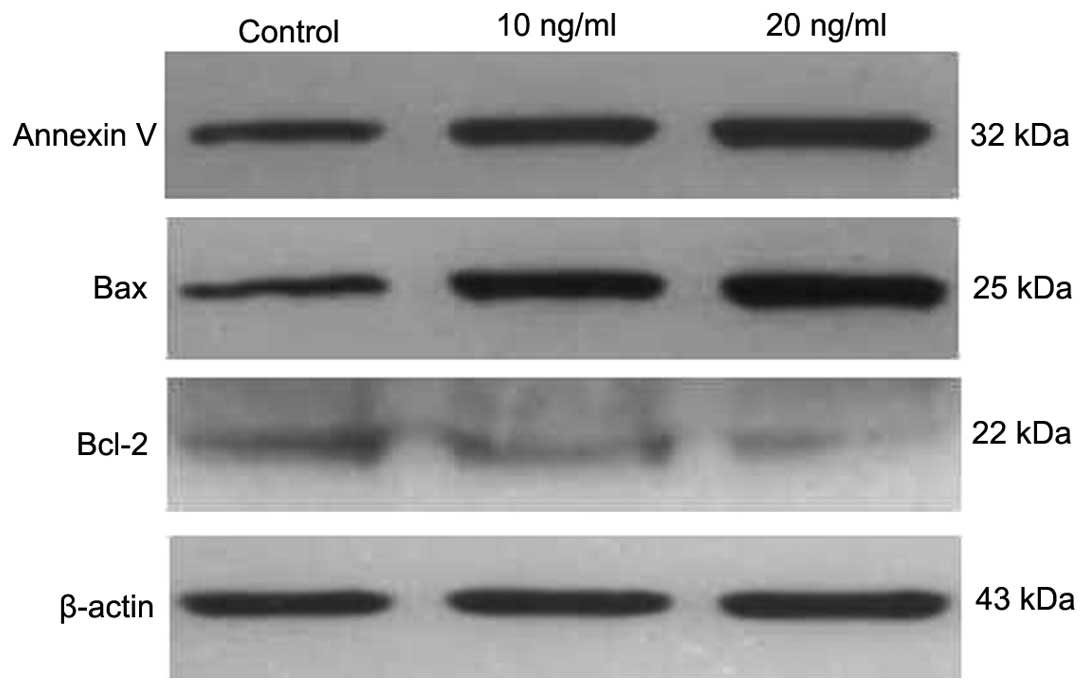
Annexin V is an anticoagulant protein that is
typically used as an indicator of cell apoptosis. Bcl-2 is an
important member of the Bcl-2 family of regulator proteins that
inhibits cell apoptosis (23). Bax
is an antagonist of Bcl-2 that promotes cell apoptosis (23). Western blotting showed that treatment
with 10 and 20 ng/ml TGF-β1 significantly increased the expression
of Annexin V and Bax but decreased the expression of Bcl-2
(Fig. 3). The average expression
levels of Annexin V, Bax and Bcl-2 in each group were calculated
using Image J software (NIH) and are listed in Table II.
 | Table II.Relative expression levels of Annexin
V, Bax and Bcl-2 in each group. |
Table II.
Relative expression levels of Annexin
V, Bax and Bcl-2 in each group.
| Protein | Control | 10 ng/ml TGF-β1 | 20 ng/ml TGF-β1 |
|---|
| Annexin V (%) | 58.262±4.372 |
74.972±6.301a |
89.331±6.996a |
| Bax (%) | 42.964±2.438 |
76.250±6.152a |
95.952±5.468a |
| Bcl-2 (%) | 41.194±3.875 |
26.412±3.235a |
10.513±3.781a |
Effect of TGF-β1 on mitochondrial ROS
generation in BMSCs
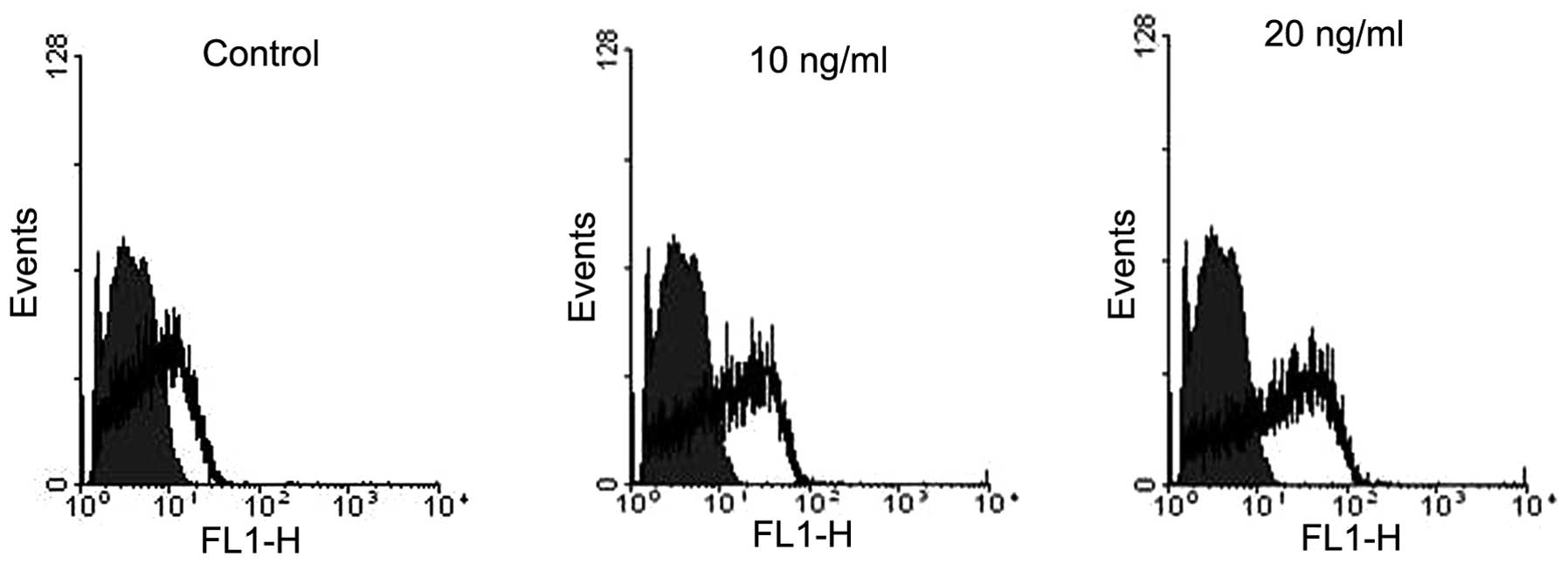
Mitochondrial ROS are strong inducers of cell
apoptosis (24). It has been
indicated that TGF-β1 can induce mitochondrial ROS production in
cell lineages other than BMSCs (19,25).
Flow cytometric data showed that treatment with TGF-β1 (10 and 20
ng/ml) also markedly increased mitochondrial ROS levels in BMSCs
(Fig. 4).
Discussion
BMSCs are the most promising seed cells in stem
cell-based transplantation and have been widely used in the
clinical treatment of certain diseases, such as neurodegeneration
and myocardial infarction (26,27).
Generally, BMSCs must be induced in vitro for directional
differentiation prior to transplantation. TGF-β1 is one of the most
commonly used reagents to induce the directional differentiation of
BMSCs into cardiomyocyte-like cells (6–8). In the
present study, it was found that the viability of the BMSCs was
markedly decreased and the apoptosis rates of the BMSCs were
increased following exposure to 10 and 20 ng/ml TGF-β1 for 24 h.
Furthermore, the mitochondrial ROS levels were notably increased in
the TGF-β1-treated BMSCs. These results suggest that TGF-β1 can
induce BMSC apoptosis, with a mechanism that may involve
mitochondrial ROS production.
The TGF-β proteins comprise a large family of cell
regulatory proteins that plays crucial roles in a series of
physiological processes, including cell proliferation,
differentiation, apoptosis and autophagy, in numerous cell types
(9–11). TGF-β has three main isoforms: TGF-β1,
TGF-β2 and TGF-β3 (28). TGF-β1 was
the first-identified isoform in the TGF-β family, and is the most
important isoform in the regulation of cell growth and
differentiation (29). A number of
studies have used TGF-β1 to induce the cardiomyogenic
differentiation of BMSCs and have successfully acquired
cardiomyocyte-like cells using this method (6–8);
however, several lines of evidence suggest that TGF-β1 acts to
trigger apoptosis of numerous cell types (15–17). In
the present study, it was found that TGF-β1 inhibited the
proliferation and promoted the apoptosis of BMSCs.
Bcl-2 and Bax are two important members of the Bcl-2
family, and their ratio (Bax:Bcl-2) determines the level of cell
apoptosis (23,24). In the present study it was found that
treatment with TGF-β1 (10 and 20 ng/ml) significantly upregulated
Bax but downregulated Bcl-2 protein expression in BMSCs. Annexin V
is another apoptotic promoter that preferentially binds
phosphatidylserine and promotes cell apoptosis (30). The present results demonstrated that
Annexin V was markedly upregulated in BMSCs following exposure to
10 and 20 ng/ml TGF-β1 for 24 h.
Mitochondrial ROS can induce apoptosis via
regulation of the balance between Bcl-2 and Bax (24). It has also been demonstrated that
mitochondrial ROS mediate the mitochondrial-dependent cell
apoptosis induced by TGF-β in certain non-BMSC lineages, such as
fetal hepatocytes (31). Our
previous study demonstrated that TGF-β1 induced mitochondrial ROS
generation in BMSCs (20).
Consistent with these previous data, the results in the present
study also demonstrated that TGF-β1, at doses of 10 and 20 ng/ml,
promoted mitochondrial ROS production in BMSCs. The TGF-β1-mediated
mitochondrial ROS production may be responsible for its actions on
BMSC apoptosis.
In conclusion, the present study has demonstrated
that TGF-β1 can promote the apoptosis of BMSCs. The effect of
TGF-β1 on BMSCs may involve mitochondrial ROS generation.
Acknowledgements
This study was supported by a grant (no. 31401246)
from the National Natural Science Foundation of China.
References
|
1
|
Zhang F, Wang C, Jing S, et al:
Lectin-like oxidized LDL receptor-1 expresses in mouse bone
marrow-derived mesenchymal stem cells and stimulates their
proliferation. Exp Cell Res. 319:1054–1059. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen Y, Teng X, Chen W, et al: Timing of
transplantation of autologous bone marrow derived mesenchymal stem
cells for treating myocardial infarction. Sci China Life Sci.
57:195–200. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Williams AR, Trachtenberg B, Velazquez DL,
et al: Intramyocardial stem cell injection in patients with
ischemic cardiomyopathy: Functional recovery and reverse
remodeling. Circ Res. 108:792–796. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fan CQ, Leu S, Sheu JJ, et al: Prompt bone
marrow-derived mesenchymal stem cell therapy enables early porcine
heart function recovery from myocardial infarction. Int Heart J.
55:362–371. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tong J, Ding J, Shen X, et al: Mesenchymal
stem cell transplantation enhancement in myocardial infarction rat
model under ultrasound combined with nitric oxide microbubbles.
PLoS One. 8:e801862013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bhang SH, Gwak SJ, Lee TJ, et al: Cyclic
mechanical strain promotes
transforming-growth-factor-beta-1-mediated cardiomyogenic marker
expression in bone-marrow-derived mesenchymal stem cells in vitro.
Biotechnol Appl Biochem. 55:191–197. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mohanty S, Bose S, Jain KG, et al: TGFβ 1
contributes to cardiomyogenic-like differentiation of human bone
marrow mesenchymal stem cells. Int J Cardiol. 163:93–99. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rouhi L, Kajbafzadeh AM, Modaresi M, et
al: Autologous serum enhances cardiomyocyte differentiation of rat
bone marrow mesenchymal stem cells in the presence of transforming
growth factor-β 1 (TGF-β 1). In Vitro Cell Dev Biol Anim.
49:287–294. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Al-Azayzih A, Gao F, Goc A and Somanath
PR: TGFβ 1 induces apoptosis in invasive prostate cancer and
bladder cancer cells via Akt-independent, p38 MAPK and
JNK/SAPK-mediated activation of caspases. Biochem Biophys Res
Commun. 427:165–170. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li YC, Ding XS, Li HM, et al: Role of G
protein-coupled estrogen receptor 1 in modulating transforming
growth factor-β stimulated mesangial cell extracellar matrix
synthesis and migration. Mol Cell Endocrinal. 391:50–59. 2014.
View Article : Google Scholar
|
|
11
|
Gajewska M, Gajkowska B and Motyl T:
Apoptosis and autophagy induced by TGF-β 1 in bovine mammary
epithelial BME-UV1 cells. J Physiol Pharmacol. 56:Suppl 3. 143–157.
2005.PubMed/NCBI
|
|
12
|
Huang SS and Huang JS: TGF-beta control of
cell proliferation. J Cell Biochem. 96:447–462. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Khan R, Agrotis A and Bobik A:
Understanding the role transforming growth factor-beta-1 in intimal
thickening after vascular injury. Cardiovasc Res. 74:223–234. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gonzalez CR, Calandra RS and
Gonzalez-Calvar SI: Testicular expression of the TGF-β 1 system and
the control of Leydig cell proliferation. Adv Biosci Biotech.
4:1–7. 2013. View Article : Google Scholar
|
|
15
|
Lafon C, Mathieu C, Guerrin M, et al:
Transforming growth factor beta 1-induced apoptosis in human
ovarian carcinoma cells: Protection by the antioxidant
N-acetylcysteine and bcl-2. Cell Growth Differ. 7:1095–1104.
1996.PubMed/NCBI
|
|
16
|
Cencetti F, Bernacchioni C, Tonelli F, et
al: TGFβ 1 evokes myoblast apoptotic response via a novel signaling
pathway involving S1P4 transactivation upstream of Rho-kinase-2
activation. FASEB J. 27:4532–4546. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li X, McFarland DC and Velleman SG:
Transforming growth factor-beta 1-induced satellite cell apoptosis
in chickens is associated with beta 1 integrin-mediated focal
adhesion kinase activation. Poult Sci. 88:1725–1734. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shimada K, Crother TR, Karlin J, et al:
Oxidized mitochondrial DNA activates the NLRP3 inflammasome during
apoptosis. Immunity. 36:401–414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yoon YS, Lee JH, Hwang SC, et al: TGF beta
1 induces prolonged mitochondrial ROS generation through decreased
complex IV activity with senescent arrest in MvLu cells. Oncogene.
24:1895–1903. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu J, Niu J, Li X, et al: TGF-β 1 induces
senescence of bone marrow mesenchymal stem cells via increase of
mitochondrial ROS production. BMC Dev Biol. 14:212014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang F, Wang C, Wang H, et al: Ox-LDL
promotes migration and adhesion of bone marrow-derived mesenchymal
stem cells via regulation of MCP-1 expression. Mediators Inflamm.
2013:6910232013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang F, Jing S, Ren T and Lin J:
MicroRNA-10b promotes the migration of mouse bone marrow-derived
mesenchymal stem cells and downregulates the expression of
E-cadherin. Mol Med Rep. 8:1084–1088. 2013.PubMed/NCBI
|
|
23
|
Misao J, Hayakawa Y, Ohno M, et al:
Expression of bcl-2 protein, an inhibitor of apoptosis and Bax, an
accelerator of apoptosis, in ventricular myocytes of human hearts
with myocardial infarction. Circulation. 94:1506–1512. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fleury C, Mignotte B and Vaysière JL:
Mitochondrial reactive oxygen species in cell death signaling.
Biochimie. 84:131–141. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Abe Y, Sakairi T, Beeson C and Kopp JB:
TGF-β 1 stimulates mitochondrial oxidative phosphorylation and
generation of reactive oxygen species in cultured mouse podocytes,
mediated in part by the mTOR pathway. Am J Physiol Renal Physiol.
305:F1477–F1490. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wen Z, Zheng S, Zhou C, et al: Repair
mechanisms of bone marrow mesenchymal stem cells in myocardial
infarction. J Cell Mol Med. 15:1032–1043. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen Y, Teng FY and Tang BL: Coaxing bone
marrow stromal mesenchymal stem cells towards neuronal
differentiation: Progress and uncertainties. Cell Mol Life Sci.
63:1649–1657. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ruiz-Ortega M, Rodriguez-Vita J,
Sanchez-Lopez E, et al: TGF-beta signaling in vascular fibrosis.
Cardiovasc Res. 74:196–206. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Xiangming C, Natsugoe S, Takao S, et al:
Preserved Smad4 expression in the transforming growth factor beta
signaling pathway is a favorable prognostic factor in patients with
advanced gastric cancer. Clin Cancer Res. 7:277–282.
2001.PubMed/NCBI
|
|
30
|
Liu T, Zhu W, Yang X, Chen L, Yang R, Hua
Z and Li G: Detection of apoptosis based on the interaction between
annexin V and phosphatidylserine. Anal Chem. 81:2410–2413. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Herrera B, Alvarez AM, Sánchez A, et al:
Reactive oxygen species (ROS) mediates the mitochondrial-dependent
apoptosis induced by transforming growth factor β in fetal
hepatocytes. FASEB J. 15:741–751. 2001. View Article : Google Scholar : PubMed/NCBI
|