Introduction
Non-invasive CT coronary angiography (CTCA) has
evolved into an important clinical tool for the assessment of
coronary artery disease (CAD) (1).
According to guidelines, its use is considered appropriate for
symptomatic patients with an intermediate risk of CAD (2). Specifically, the wide-spread use of
64-slice CT and dual-source CT (DSCT) in coronary angiography has
greatly improved the image quality and accuracy of diagnosis
(3), although the radiation dose
has also been increased (4). In a
recent multicenter, multivendor trial, Hausleiter et
al(5) demonstrated a median
effective radiation dose of 12 mSv for CTCA with retrospective
electrocardiography (ECG) gating, while certain sites used
protocols exceeding even 30 mSv.
Furthermore, adaptive ECG-pulsing algorithms for use
in spiral CT are designed to maintain diagnostic image quality in
arrhythmic patients since the continuous high X-ray tube output
allows flexible selection of the desired reconstruction phase
throughout the R-R interval. However, image quality is only
maintained at the cost of higher radiation exposure (6). Due to the inevitable problem of high
radiation doses in CT examination, various strategies to reduce the
radiation exposure of patients have been developed. The most
significant is prospectively ECG-gated CTCA, also called
step-and-shoot (SAS) mode. Low radiation doses ranging between 1.2
and 4.3 mSv have been reported using various 64-slice and
first-generation, dual-source 64-slice CT (7,8).
Most significantly, this low-dose SAS method provides high image
quality (8,9), although it remains necessary to
control the heart rate.
The purpose of the present study was to evaluate the
accuracy of using second generation DSCT to obtain high quality
images and diagnostic performance and to reduce the radiation dose
in adaptive prospective ECG-triggered sequence (CorAdSeq) CTCA
without heart rate control.
Materials and methods
Patient population
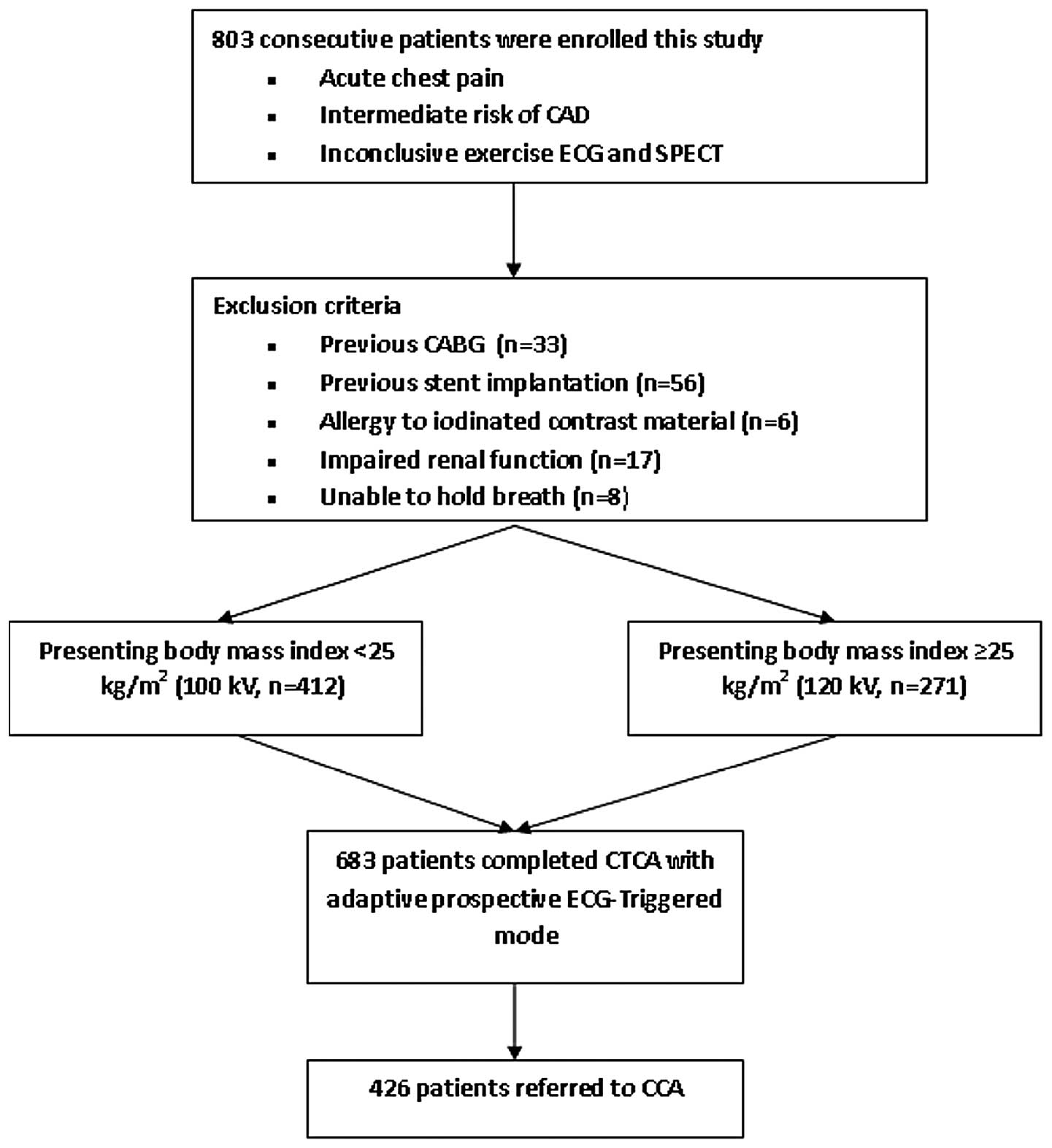
Between June 2010 and June 2011, 803 consecutive
symptomatic patients suspected of having or with known CAD were
eligible for inclusion in the present study (Fig. 1). Those patients with previous
coronary artery bypass grafts (n=33) and stent implantation (n=56)
were excluded. The exclusion criteria specific to CTCA were known
allergies to iodinated contrast material (n=6), impaired renal
function (serum creatinine levels >120 μmol/l; n=17) and
the inability to hold a breath (n=8). Thus, the study population
consisted of 683 patients (447 males, 236 females; mean age ±
standard deviation, 61.2±12.0 years). This study was conducted in
accordance with the declaration of Helsinki and with approval from
the Ethics Committee of Nanjing Medical University (Tianning,
Changzhou, Jiangsu, China). Written informed consent was obtained
from all participants.
Scan preparation
No β-blockers or other drugs were used to decrease
heart rate or/and change arrhythmia prior to scanning. An 18-G
needle was embedded in the middle vein of the right elbow. The skin
was cleaned and ECG lines were placed in standard positions. Prior
to scanning, the patients received one sublingual dose of
nitroglycerin aerosol spray (Jingwei Pharma Co., Ltd., Shandong,
China) to expand the coronary artery.
Scan protocol and image
post-processing
All patients were scanned on a second-generation
DSCT scanner (Somatom Definition Flash; Siemens Medical Solutions,
Munich, Germany) with the adaptive prospective CorAdSeq model. The
imaging parameters were as follows: detector collimation, 2×64×0.6
mm; slice acquisition, 2×128×0.6 mm by means of a z-flying focal
spot; gantry rotation time, 280 msec. The tube voltage was adjusted
to each patient’s body mass index (BMI); 100 kV was used for a BMI
<25.0 kg/m2 and 120 kV for a BMI of ≥25.0
kg/m2 for each technique. Automatic exposure control
system-based tube current modulation (Care-DOSE; Siemens Medical
Solutions) was used in all patients with the two data acquisition
techniques. The reference tube current was 390 mA, with the tube
current automatically adjusted to the size and density of the body
region (10) and a full tube
current applied between 30–80% of the R-R interval, so as to obtain
both systolic and diastolic images at full dose. A scout view of
the thorax was obtained to plan CT angiography data acquisition and
the scanning scope was performed from 2 cm below the level of the
tracheal bifurcation to the diaphragm in a cranio-caudal direction.
All examinations were performed following a verbal command,
instructing the patient to hold their breath after a deep
inspiration. The breath-hold maneuver was practiced once prior to
the actual examination. Patients intravenously received 70 ml (for
BMI <25.0 kg/m2) or 80 ml (for BMI ≥25.0
kg/m2) non-ionic contrast medium (Ultravist 370 mgI/ml;
Bayer Schering Pharma, Berlin, Germany) at a flow rate of 4.5
ml/sec (for BMI <25.0 kg/m2) or 5.0 ml/sec (for BMI
≥25.0 kg/m2), adjusted to each patient’s BMI
respectively, followed by a saline chaser of 40 ml at the same flow
rate, using a binocular high-pressure injector. Data acquisition
was started 4 sec after a region of interest in the ascending aorta
reached a threshold of 150 HU (bolus tracking technique). The data
were rebuilt and transferred automatically to the workstation
(Syngo MMWP VE36A, Siemens Medical Solutions).
Images for the two protocols were reconstructed with
a slice thickness of 0.75 mm, a reconstruction increment of 0.5 mm
and using a soft-tissue convolution kernel (B26f). For vessel wall
calcification, additional images were reconstructed using a
sharp-tissue convolution kernel (B46f) to compensate for blooming
artefacts. The post-processing included maximum intensity
projection (MIP), multiplanar reformation (MPR) and volume
rendering (VR).
Assessment of image quality
Image quality was evaluated in a double-blind manner
and scored by two experienced radiologists (T.W. and X.Q.T., each
with ≥3 years experience of interventional cardiology) who
identified all available coronary segments in invasive coronary
angiography using the 17-segment modified American Heart
Association classification (11).
Of the 683 patients, 426 (62.4%, 426/683) underwent conventional
coronary angiography (CCA). All conventional angiograms were
performed within one month before or after CTCA. All segments with
diameters ≥1 mm were included for comparison with CTCA. The
stenoses were classified as significant if the lumen diameter
reduction was ≥50%.
The image quality assessment criteria used a
semi-quantitative five-point grading scale (12), as follows: 5 points, images had
clear coronary edge and no motion artifacts; 4 points, images had
slightly blurred edges and only mild motion artifacts; 3 points,
images had moderately blurred edges and mild motion artifacts
without significant splitting, not impairing the diagnosis; 2
points, images with blurred edges and clear motion artifacts; and 1
point, images with the coronary lumen unidentifiable and thus
undiagnosable. Images of ≥3 points were regarded as diagnostic
image quality.
The mean heart rate (MHR) and minimal and maximal
heart rate per minute were recorded following CT acquisition for
each patient. Heart rate variability (HRV) was calculated as the
maximum bpm - minimum bpm.
Radiation dose assessment
The volume CT dose index (CTDIvol, in mGy) and dose
length product (DLP, in mGy x cm) were automatically generated by
the machine and recorded for each patient during examination.
Effective dose (ED, in units of mSv) was calculated using the
formula ED = DLP × C (13), where
C is the conversion factor (C=0.01 4 mSv × mGy−1 ×
cm−1) (14). CTDIvol
and ED were presented as mean values ± standard deviation.
Statistical analysis
The patients and scan characteristics were expressed
as numbers and percentages, while continuous variables were
expressed as mean values ± standard deviation. Statistical analyses
were performed using statistical software (SPSS, v.13.0 for
Windows; SPSS, Chicago, IL, USA). The diagnostic performance of
CTCA for the diagnosis of significant CAD compared with the
reference standard, quantitative coronary angiography, at CCA, was
determined using sensitivity, specificity, positive predictive
value (PPV) and negative predictive value (NPV) and their
corresponding 95% confidence intervals. The differences in patients
and scan characteristics were calculated using the Student’s
t-test. The image quality according to the MHR and HRV groups was
compared using Fisher’s exact test. An α level <0.05 was
considered to indicate a statistically significant difference. For
the dose estimates, the two-way analysis of variance test was
performed to evaluate the effect of MHR and HRV on the radiation
exposure (CTDIvol and ED), for each BMI group. An α level <0.05
was considered to indicate a statistically significant difference.
When there were differences between groups, the multi-comparison
correction was used to adjust the α level by the Bonferroni method.
The interobserver agreement on semi-quantitative grades of image
quality between the two readers was calculated prior to consensus
reading by using κ statistics. A κ value >0.81 corresponded to
excellent interobserver agreement, with values of 0.61–0.80
corresponding to good agreement (15).
Results
Patient demographics
The comparisons of demographic data for the patient
groups are listed in Table I. No
significant differences were observed in any of the demographic
parameters between the two groups. A total of 683 patients were
eligible for CTCA (group A, BMI <25 kg/m2, n=412 and
group B, BMI ≥25 kg/m2, n=271). Overall, 356 patients
had a heart rate >70 bpm during scanning (52.1% of 683
patients), with 195 in group A (47.3%, 195/412) and 161 in group B
(59.4%, 161/271). Of the 683 patients, 54 had a heart rate >100
bpm (7.9%, 54/683), with 24 in group A (5.8%, 24/412) and 30 in
group B (11.1%, 30/271). The MHR was 78.5±13.2 bpm in group A and
79.0±13.9 bpm in group B (P=0.711) and the HRV was 20.7±19.3 bpm in
group A and 23.7±26.8 bpm in group B (P= 0.201). No significant
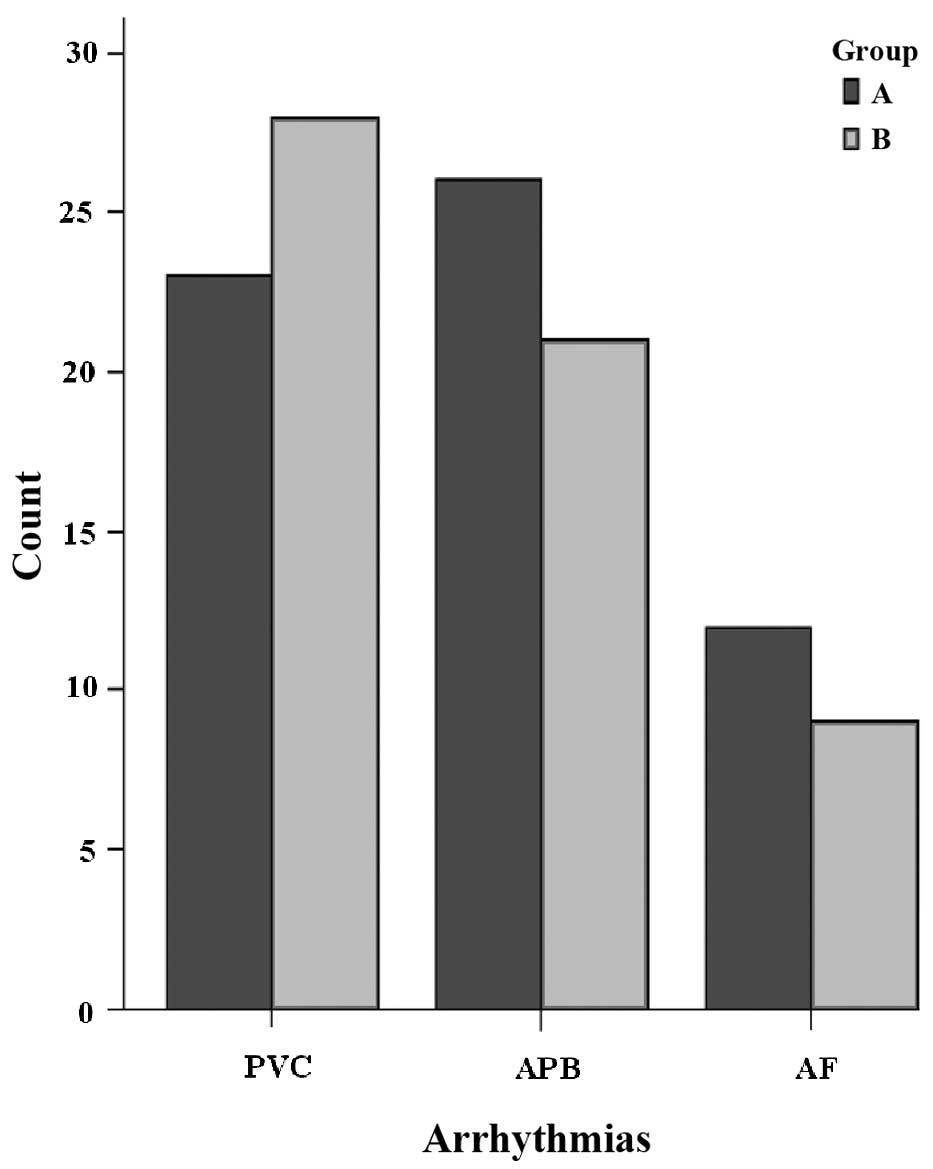
differences were observed between the two groups. Of the patients,
564 (82.6%, 564/683) remained in sinus rhythm during data
acquisition and 119 (17.4%, 119/683) exhibited irregular heart
beats, including premature ventricular contraction (n=51),
premature atrial beat (n=47) and atrial fibrillation (n=21). No
significant differences were identified between the two groups
(P=0.78; Fig. 2).
 | Table I.Patient demographics and scan
parameters. |
Table I.
Patient demographics and scan
parameters.
| Factors | Group A (n=412) | Group B (n=271) | P-value |
|---|
| Patient
characteristic | | | |
| Gender
(male/female) | 268/144 | 179/92 | 0.787 |
| Age (years)a | 61.8±12.3 | 60.6±11.7 | 0.327 |
| Body weight
(kg)a | 67.6±6.9 | 73.4±9.3 | 0122 |
| BMI
(kg/m2)a | 23.47±0.97 | 26.10±0.75 | 0.000 |
| Scan parameter | | | |
| MHR (bpm)a | 78.5±13.2 | 79.0±13.9 | 0.711 |
| HRVa | 20.7±19.3 | 23.7±26.8 | 0.201 |
| Scan range
(mm)a | 115±13 | 117±11 | 0.228 |
| Scan duration
(s)a | 5.8±0.8 | 6.2±0.6 | 0.212 |
| CTDIvol
(mGy)a | 16.05±3.84 | 38.64±11.63 | 0.000 |
| DLP (mGy ×
cm)a | 183.89±56.99 | 454.18±166.26 | 0.000 |
| ED (mSv)a | 2.57±1.01 | 6.36±1.88 | 0.000 |
| Score | 4.77±0.46 | 4.83±0.37 | 0.133 |
CT image quality
A five-point rating scale was used to assess the
image quality. A total of 683 coronary arteries were included in
the present study, of which 671/683 (98.2%) yielded high image
quality and 12/683 (1.8%) showed non-diagnostic image quality due
to severe respiratory motion. No coronary segment was considered
non-diagnostic due to elevated MHR or HRV. A total of 98.5%
(6493/6592) of the segments in group A and 98.8% (4286/4336) in
group B were evaluated. The interobserver agreement for image
quality ratings between the readers was excellent (κ=0.856). No
significant differences were observed between the number of
segments depicted with diagnostic image quality in the two groups
(P=0.158). Images with poor diagnostic quality were caused by
artifacts associated with respiratory motion (n=7; group A, 4;
group B, 3) and associated with severe coronary calcifications
(n=5; group A, 2; group B, 3). The mean image quality scores for
groups A and B were 4.77±0.46 and 4.83±0.37, respectively. No
significant differences were identified between the two groups
(P=0.133). No correlation was observed between the image quality
score and the MHR or HRV (P=0.492, P=0.564, respectively).
Radiation dose assessment
The CTDIvol, DLP and ED estimates were all
significantly lower for group A than for group B (P<0.001,
P<0.05, correction, Table I),
while the scan range was not significantly different between the
two groups (P=0.228; Table I). In
patients with a BMI <25.0 kg/m2, the estimated ED was
2.57±1.01 mSv and when the BMI was ≥25.0 kg/m2, the ED
was 6.36±1.88 mSv.
The MHR and HRV with ED and CTDIvol had a
significant (P<0.01, P<0.05, respectively) negative
correlations between the two groups, which may be attributed to the
increase in pitch values.
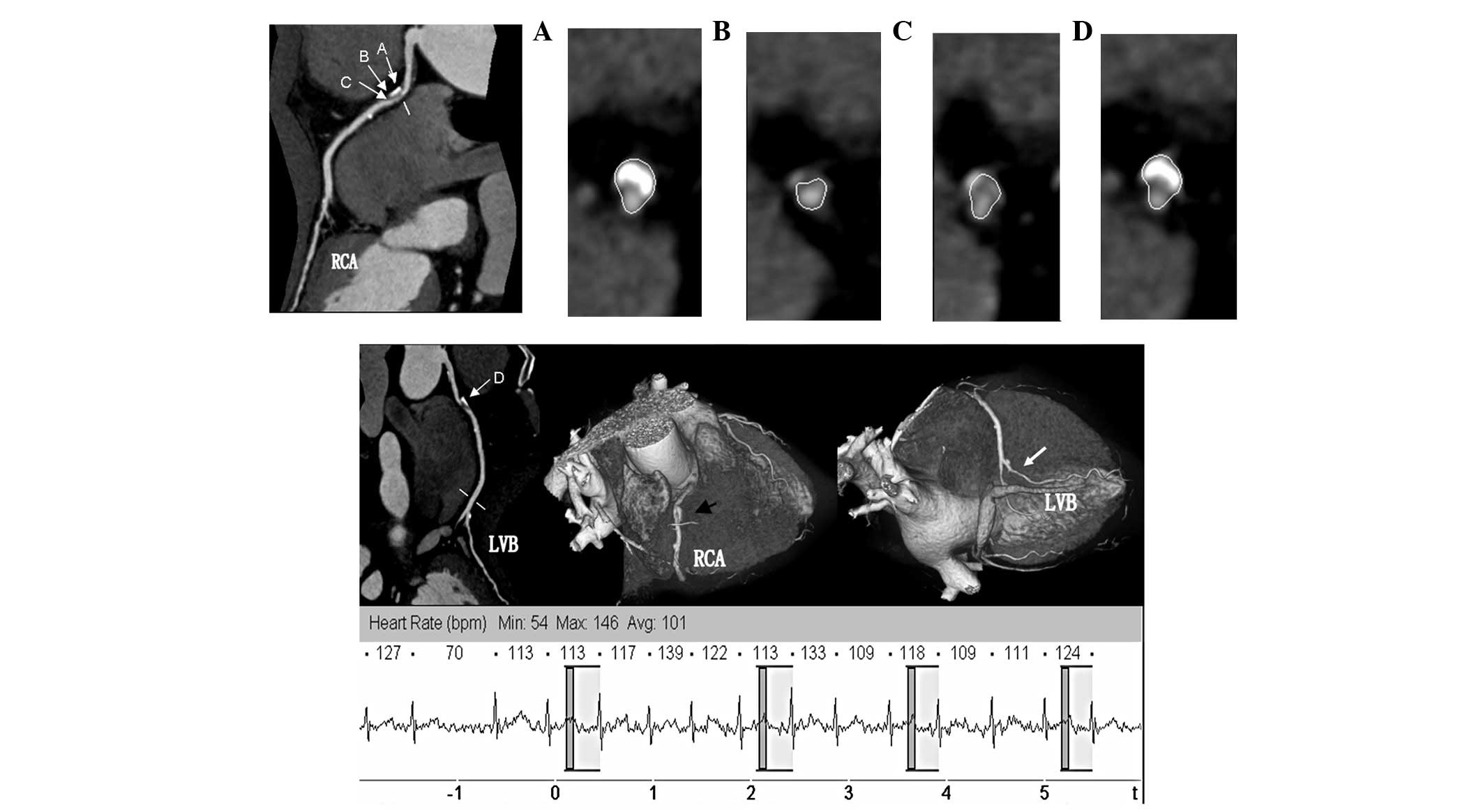
Diagnostic performance
CCA was used as the reference standard and
demonstrated the prevalence of CAD in 469 patients to be 68.7%. The
prevalence was 68.4% in group A (282/412) and 69.0% in group B
(187/271). In these 469 patients, 571 coronary stenoses of ≥50%
lumen diameter reduction were detected by CCA [15 in the left main,
285 in the left anterior descending (Fig. 3), 189 in the left circumflex and 82
in the right coronary artery]. Of the 562 coronary stenoses of ≥50%
lumen diameter reduction that were shown by DSCT, 9.1% (593/6493)
significant stenosis per segment was observed in group A and 9.7%
(415/4286) in group B. No significant differences were observed
between the proportion of segments depicted with significant
stenoses per segment between the two groups (P=0.344). Of the
coronary segments, 68 were classified as false-positives by DSCT:
44 were unevaluable and thus estimated as having significant
stenosis, but did not exhibit significant stenosis on CCA and 24
segments were evaluated as false-positives since the degree of
lumen reduction was overestimated. Thus, the κ value for coronary
artery stenosis detection with CTCA was 0.985, indicating high
intermethod agreement between readers. The A and B group data for
the segment-based, vessel-based and patient-based sensitivity,
specificity, PPV and NPV are presented in Table II.
 | Table II.Comparison of the two groups by CT
coronary angiography for the diagnosis of significant coronary
stenosis. |
Table II.
Comparison of the two groups by CT
coronary angiography for the diagnosis of significant coronary
stenosis.
| Group A (BMI<25
kg/m2)
| Group B (BMI≥25
kg/m2)
|
|---|
| Segment-based | Coronary-based | Patient-based | Segment-based | Coronary-based | Patient-based |
|---|
| TP | 587 | 369 | 272 | 410 | 198 | 189 |
| FP | 38 | 4 | 3 | 30 | 5 | 2 |
| FN | 6 | 2 | 1 | 5 | 1 | 1 |
| TN | 5862 | 1270 | 136 | 3841 | 876 | 79 |
| Sensitivity (%) | 99.0 (98.2–99.8) | 99.5 (98.8–100) | 99.6 (98.9–100) | 98.8 (97.8–99.8) | 99.5 (98.5–100) | 99.5 (98.5–100) |
| Specificity (%) | 99.4 (99.2–99.6) | 99.7 (99.4–99.9) | 97.8 (95.4–100) | 99.2 (98.9–99.5) | 99.4 (98.9–99.9) | 97.5 (94.1–100) |
| PPV (%) | 93.9 (92.0–95.8) | 98.9 (97.0–99.9) | 98.9 (97.7–100) | 93.2 (90.9–95.6) | 97.5 (95.4–99.6) | 98.9 (97.6–100) |
| NPV (%) | 99.9 (99.8–100) | 99.8 (99.6–100) | 99.3 (97.9–100) | 99.9 (99.8–100) | 98.9 (99.7–100) | 98.8 (96.4–100) |
Discussion
With the growing popularity of 64-Multidetector CT
(MDCT) and DSCT, CTCA has gained a wide spectrum of applications
due to its simplicity, non-invasiveness and high accuracy in
detecting significant stenoses in patients with regular and low
(<65 bpm) heart rates. β-blockers are commonly administered
prior to CTCA to lower the heart rate, thereby reducing the number
of image-degrading motion artifacts. DSCT scanners provide an
improved temporal resolution compared with single-source CT
equipment and may eliminate the need for prescan β-blockers
(16). However, in previous
studies, the number of patients with increased heart rate (>80
bpm) was small and patients with arrhythmias were excluded from the
majority of studies (3,16). Heart rate modulation by oral or
intravenous administration of β-blockers was not required prior to
the scanning procedure in the present study. The present technique
of the CorAdSeq demonstrated high image quality, even in a number
of patients with arrhythmias (Fig.
4). No correlation was identified between the image quality and
MHR or HRV.
A small number of studies have investigated the
effect of HRV on image quality and diagnostic performance. However,
in these studies the HRVs were defined as the standard deviation of
the MHR during CTCA. A sudden change in heart rate may cause
several problems in the acquisition of CTCA since artifacts are
created due to differences in the image reconstruction phases
between consecutive heart beats. Previous studies did not perform
CTCA in patients with arrhythmias. In the present study, 7.9%
(54/683) patients had a heart rate >100 bpm during scanning and
119 patients (17.4%) had arrhythmias. Diagnostic image quality was
obtained for all patients on the basis of adaptive prospective
CorAdSeq, even patients with severe HRV. This finding indicates
that CorAdSeq is a robust technique and may be used in all patients
undergoing CTCA.
DSCT uses two mutually perpendicular tubes, one
rotation of which significantly increases the covered area and scan
speed. Using a 0.33 sec gantry rotation time, the time resolution
is one quarter (1/4) of the rotation time, i.e. 83 msec (17). In the present study group, the
gantry rotation time was reduced to 0.28 sec and the time
resolution was increased to 75 msec. Such a time resolution was
enough for coronary CT scans without the need to control heart
rates. By contrast, conventional perspective CorAdSeq scanning
requires more strict control of heart rate and rhythm (heart rate
<70 bpm) and heart rate fluctuation <10 times/min (3,12).
Therefore, the conventional technique may only be applied to
patients with a regular rhythm and low heart rate. Furthermore, the
time phase cannot be changed when restructuring and split images
are likely to appear if the heart rate change is abrupt, thereby
affecting the image quality. CorAdSeq scanning selects appropriate
reconstruction phases to control the exposure to X-rays using the
heart rate monitoring by ECG. This has the advantage of increasing
the scanning speed and lowering radiation dose as the X-ray
exposure only occurs in selected phases rather than in the whole
cardiac cycle. If arrhythmia occurs, the patient table stops in the
original position without scanning and data collection. Only when
the next R-R wave becomes rhythmic is the patient table moved to
the appropriate position and scanning and data acquisition
restarted. Since the examination bed does not move, there is no
data gap in the cardiac cycle before and after arrhythmia. A high
overall diagnostic performance was observed for DS CTCA in the
detection of significant coronary artery stenosis with a
sensitivity of 99% and an NPV of 99% on a per-patient basis. These
results were obtained without excluding any segments or patients on
the basis of non-diagnostic image quality. No significant
differences were observed in image quality between the two groups
regardless of MHR and HRV. Despite high heart rates (maximal 171
bpm and MHR 78.8±13.6 bpm) and large heart rate fluctuations
(22.2±23.4 bpm) during scanning in the patients, 98.2% (671/683)
yielded high quality images. No coronary segments were considered
non-diagnostic due to elevated MHR or HRV, indicating that the
image quality obtained by CorAdSeq scanning was not significantly
affected by increased heart rate or arrhythmia. In the present
study, the overall average image score for all the patients was
4.80±0.41.
Numerous factors affect CTCA radiation dose,
including scan length, scan speed and tube voltage (18). The biggest difference between
CorAdSeq and DSCT retrospective ECG-gated spiral scanning is
CordAdSeq’s CARE Dose 4D technique. CARE Dose 4D is based on the
approach of modulating the tube current and keeping the image noise
constant from patient to patient and over the whole scan. The
reference current is adjusted automatically according to the
anatomy of the patient’s body and organs. In slim patients, the
CARE Dose 4D automatically reduces the current in the CTCA
scanning. In obese patients, it increases the current when CTCA
scanning and so is able to further reduce the radiation dose. SAS
CTCA has attracted interest as a technique for reducing radiation
exposure while preserving diagnostic image quality. However, SAS
CTCA is currently limited to selected patients with low and regular
heart rates only (9). The present
findings confirm and corroborate those of previous reports
(7,9,12)
investigating prospective ECG gating and demonstrate the clinical
feasibility of the technique as an effective method for reducing
radiation exposure without affecting image quality. It should,
however, be emphasized that these results were obtained in a
selected groups of patients. If the prospective gating technique is
applied to patients with low (<70 bpm) and regular heart rates,
that would only demonstrate that this technology is applicable to
such patients. More significantly, the radiation dose of such a
method remains higher. Under the same conditions, in the present
study of patients with a BMI <25.0 kg/m2, the ED of
was 2.57 mSv±1.01, while for those with a BMI ≥25.0
kg/m2, the ED was 6.36 mSv±1.88, although the average
DLP and ED were slightly lower than in relevant studies (10,11)
and significantly reduced compared with retrospective ECG-gated
scanning or 64-MDCT (19,20).
The present study had certain limitations. Firstly,
the classification of the subgroups was arbitrary and was not
categorized according to MHR and HRV. Secondly, evaluation was not
performed between the image quality and diagnostic accuracy. The
association between the two should be the subject of further
studies.
In conclusion, using CTCA with the new generation
DSCT adaptive perspective CorAdSeq is feasible in patients without
heart rate control. This greatly widens the scope of its
applications with increased image quality and reduced radiation
exposure in coronary artery imaging.
References
|
1.
|
Schoepf UJ, Zwerner PL, Savino G, Herzog
C, Kerl JM and Costello P: Coronary CT angiography. Radiology.
244:48–63. 2007. View Article : Google Scholar
|
|
2.
|
Budoff MJ, Achenbach S, Blumenthal RS, et
al: Assessment of coronary artery disease by cardiac computed
tomography: a scientific statement from the American Heart
Association Committee on Cardiovascular Imaging and Intervention,
Council on Cardiovascular Radiology and Intervention, and Committee
on Cardiac Imaging, Council on Clinical Cardiology. Circulation.
114:1761–1791. 2006.
|
|
3.
|
Scheffel H, Alkadhi H, Plass A, et al:
Accuracy of dual-source CT coronary angiography: first experience
in a high pre-test probability population without heart rate
control. Eur Radiol. 16:2739–2747. 2006.PubMed/NCBI
|
|
4.
|
Brenner DJ and Hall EJ: Computed
tomography - an increasing source of radiation exposure. N Engl J
Med. 357:2277–2284. 2007.PubMed/NCBI
|
|
5.
|
Hausleiter J, Meyer T, Hermann F, et al:
Estimated radiation dose associated with cardiac CT angiography.
JAMA. 301:500–507. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Cademartiri F, Mollet NR, Runza G, et al:
Improving diagnostic accuracy of MDCT coronary angiography in
patients with mild heart rhythm irregularities using ECG editing.
AJR Am J Roentgenol. 186:634–638. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Shuman WP, Branch KR, May JM, et al:
Prospective versus retrospective ECG gating for 64-detector CT of
the coronary arteries: comparison of image quality and patient
radiation dose. Radiology. 248:431–437. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Herzog BA, Wyss CA, Husmann L, et al:
First head-to-head comparison of effective radiation dose from
low-dose 64-slice CT with prospective ECG-triggering versus
invasive coronary angiography. Heart. 95:1656–1661. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Scheffel H, Alkadhi H, Leschka S, et al:
Low-dose CT coronary angiography in the step-and-shoot mode:
diagnostic performance. Heart. 94:1132–1137. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Mulkens TH, Bellinck P, Baeyaert M, et al:
Use of an automatic exposure control mechanism for dose
optimization in multidetector row CT examinations: clinical
evaluation. Radiology. 237:213–223. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Austen WG, Edwards JE, Frye RL, et al: A
reporting system on patients evaluated for coronary artery disease.
Report of the Ad Hoc Committee for Grading of Coronary Artery
Disease, Council on Cardiovascular Surgery, American Heart
Association. Circulation. 51(Suppl 4): 5–40. 1975. View Article : Google Scholar
|
|
12.
|
Earls JP, Berman EL, Urban BA, et al:
Prospectively gated transverse coronary CT angiography versus
retrospectively gated helical technique: improved image quality and
reduced radiation dose. Radiology. 246:742–753. 2008. View Article : Google Scholar
|
|
13.
|
Nakayama Y, Awai K, Funama Y, et al: Lower
tube voltage reduces contrast material and radiation doses on
16-MDCT aortography. AJR Am J Roentgenol. 187:W490–W497. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Valentin J; International Commission on
Radiation Protection: Managing patient dose in multi-detector
computed tomography (MDCT). ICRP Publication 102 Ann ICRP. 37:1–79.
2007.PubMed/NCBI
|
|
15.
|
Lang RM, Bierig M, Devereux RB, et al:
Recommendations for chamber quantification: a report from the
American Society of Echocardiography’s Guidelines and Standards
Committee and the Chamber Quantification Writing Group, developed
in conjunction with the European Association of Echocardiography, a
branch of the European Society of Cardiology. J Am Soc
Echocardiogr. 18:1440–1463. 2005.PubMed/NCBI
|
|
16.
|
Ropers U, Ropers D, Pflederer T, et al:
Influence of heart rate on the diagnostic accuracy of dual-source
computed tomography coronary angiography. J Am Coll Cardiol.
50:2393–2398. 2007.PubMed/NCBI
|
|
17.
|
Johnson TR, Nikolaou K, Wintersperger BJ,
et al: Dual-source CT cardiac imaging: initial experience. Eur
Radiol. 16:1409–1415. 2006.PubMed/NCBI
|
|
18.
|
Deetjen A, Möllmann S, Conradi G, et al:
Use of automatic exposure control in multislice computed tomography
of the coronaries: comparison of 16-slice and 64-slice scanner data
with conventional coronary angiography. Heart. 93:1040–1043. 2007.
View Article : Google Scholar
|
|
19.
|
Fink C, Krissak R, Henzler T, et al:
Radiation dose at coronary CT angiography: second-generation
dual-source CT versus single-source 64-MDCT and first-generation
dual-source CT. AJR Am J Roentgenol. 196:W550–W557. 2011.PubMed/NCBI
|
|
20.
|
Lu B, Lu JG, Sun ML, et al: Comparison of
diagnostic accuracy and radiation dose between prospective
triggering and retrospective gated coronary angiography by
dual-source computed tomography. Am J Cardiol. 107:1278–1284.
2011.PubMed/NCBI
|