1. Introduction
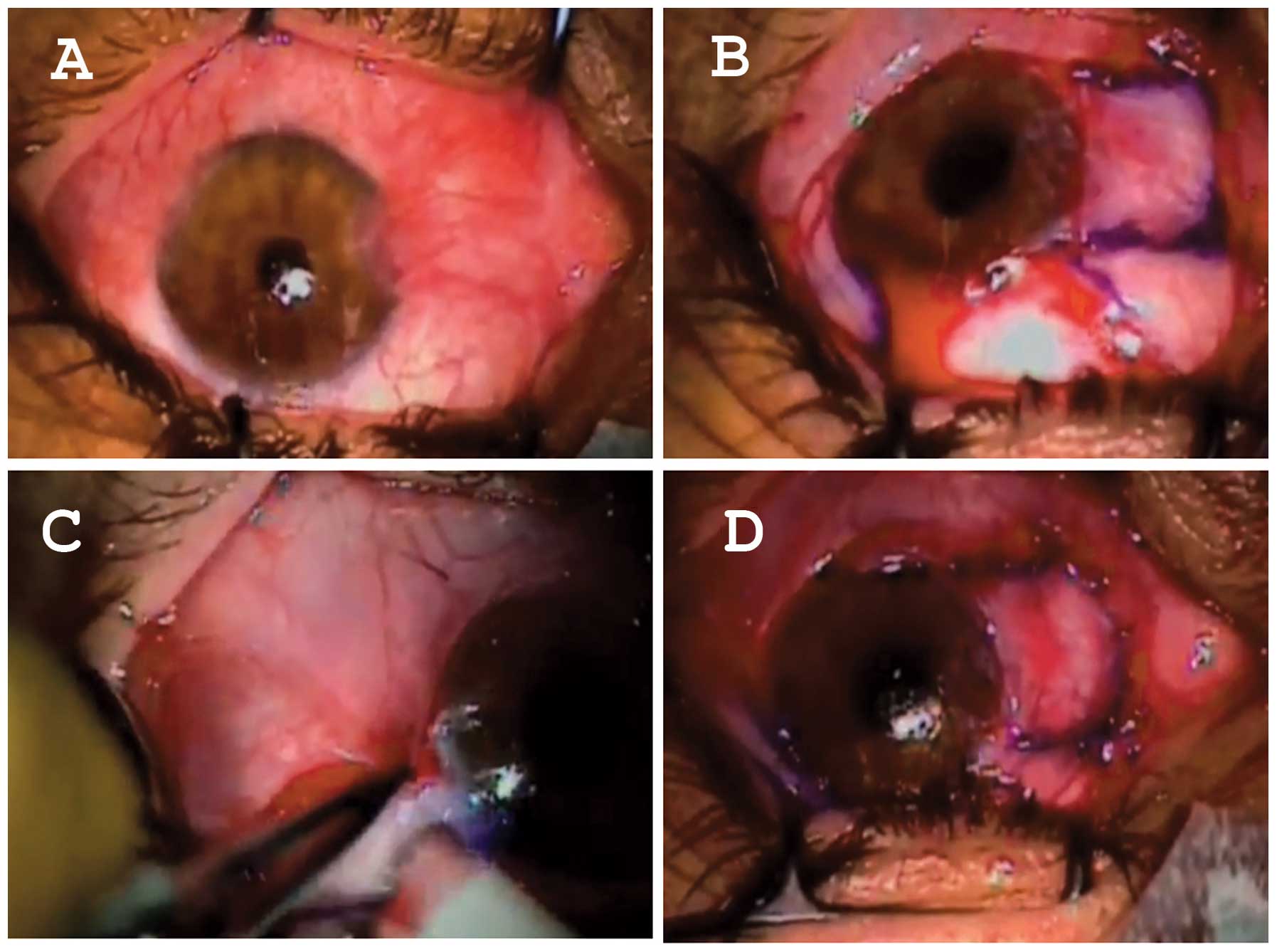
Pterygium is a wing-shaped fibrovascular lesion of
the ocular surface of unknown origin and pathogenesis. It grows at
the inter-palpebral conjunctival area, more often nasally, and
invades adjacent corneal epithelium (Fig. 1). Pterygium growth can cause
irregular astigmatism, corneal scarring, restriction of ocular
motility, or chronic ocular surface inflammation (1). Treatment thus far is exclusively
surgical, however, pterygium often tends to recur aggressively.
This has lead to the use of sophisticated surgical techniques in an
effort to reduce recurrence rates (Fig. 2) (2).
Although pterygium pathogenesis remains an enigma,
epidemiologic studies suggest that it is a sun-related eye disease
(ophthalmoheliosis). In fact, the prevalence of pterygium seems to
be associated with geographical latitude, with higher prevalences
in areas located within 40º above and below the equator, suggesting
that prolonged exposure to ultraviolet (UV) radiation may promote
its development. In addition, repeated micro-trauma, mediated by
exposure to dust, chronic conjunctival inflammation, genetic
predisposition and ocular dryness have all been reported to be
involved in pterygium, indicating a multifactorial pathogenesis
(1,3). Evidence suggests that genetically
altered limbal epithelial stem cells may play a critical role
through a process of Bowman's layer dissolution, matrix remodeling,
cell proliferation and angiogenesis, possibly with the involvement
of cytokines, matrix metalloproteinases and growth factors
(4–10). Notably, among the various theories
proposed for pterygium pathogenesis thus far, the possibility of an
infectious (probably viral) mechanism in at least a subgroup of
pterygia has also recently gained ground. This possibility is
important because, should it prove valid, it could justify
non-invasive or minimally invasive treatment options through
anti-viral medications.
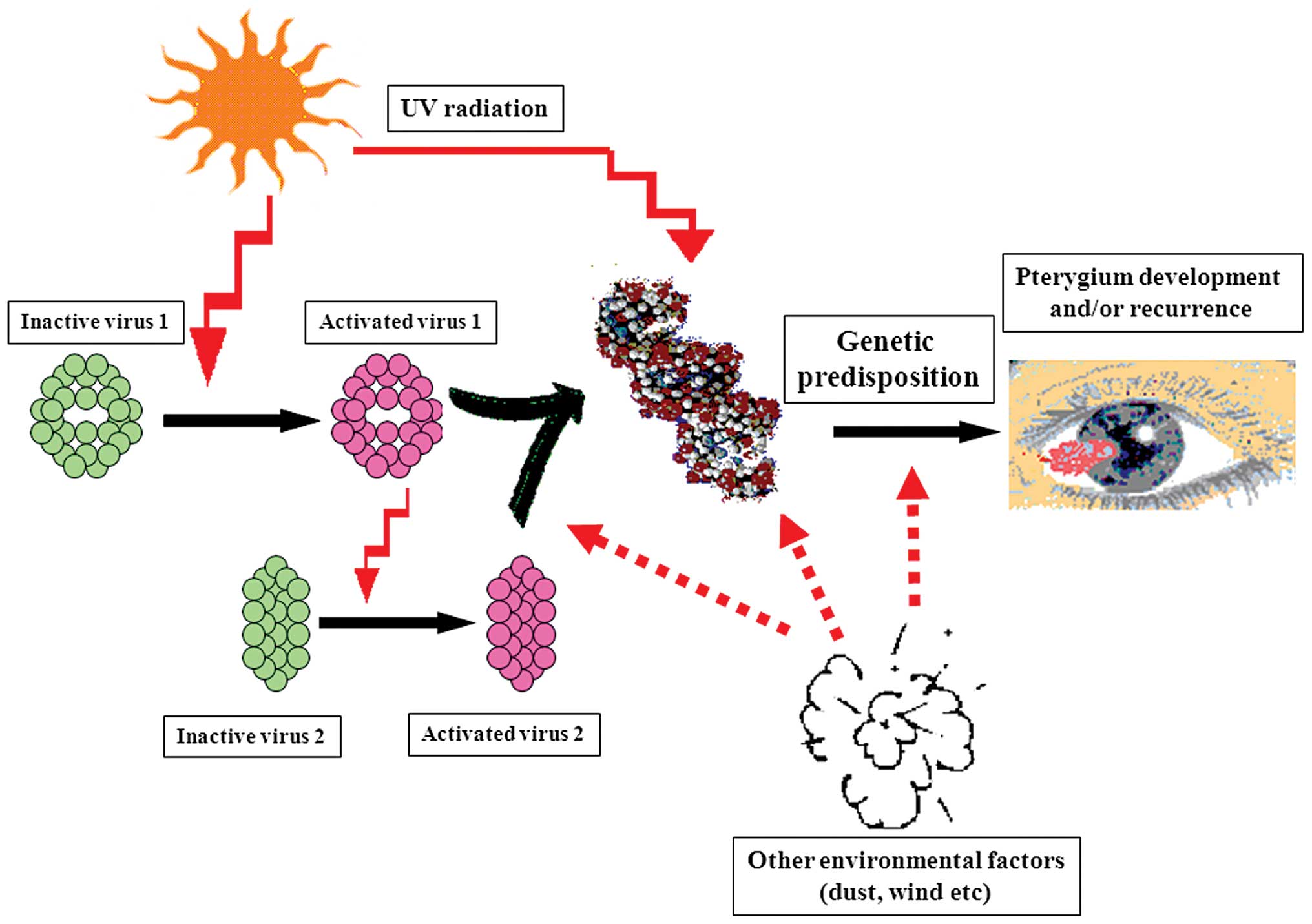
2. Theories of infectious pathogenetic
co-factors in pterygium
Pterygium has been previously considered a
degenerative condition. This hypothesis, however, has been
challenged in recent years by the detection of important molecular
genetic alterations in pterygium, including loss of heterozygosity
(LOH) of microsatellite DNA or the overexpression of mutated
versions of p53 with compromised function, which could promote
tumor growth (11–14). Accordingly, a multi-step
pathogenetic process, with the participation of genetic
inheritance, UV radiation and, importantly, oncogenic viral
infection has been proposed for the pathogenesis of pterygium
(Fig. 3). According to this
‘two-hit’ hypothesis, inherited genetic alterations or exposure to
environmental factors such as UVR could predispose individuals to
this benign neoplastic disease (‘first hit’). Oncogenic viruses, or
additional UVR exposure, adding further damage to an already
susceptible genetic material, may be the stimulus for the outset of
development or recurrence of pterygium (‘second hit’) (15). This theoretical model has been
recently supported by the detection of HPV strains considered
high-risk for cancer development, including 16 and 18, encoding E6
and E7 proteins which interfere with p53 function (16,17).
3. Virus detection in pterygium
Many studies have been conducted to investigate the
involvement of a variety of oncogenic viruses, including HPV, CMV,
HSV or EBV, in the development and recurrence of pterygium
(Table I). HPV presence in
pterygium has been reported by several studies, with prevalence
ranging from very low to almost 100% of cases (16,18–27). The prevalence of various
herpes-viruses in pterygium also differs considerably among
reports. Studies from Greece detected HSV in 22–45% and CMV in 40%
of examined pterygia (18,28).
On the other hand, in a study conducted in Taiwan Chen et al
investigated the role of HSV in pterygium, where a prevalence of
only 5% was reported (29).
Another study from Turkey detected EBV-DNA in 10% of the pterygia
examined (25). Such a disparity
in the prevalence of oncogenic virus detection in pterygium may
partly be explained by ethnic or geographical factors or by
laboratory techniques. However, it may also reflect the
heterogeneous nature of pterygium pathogenesis and the possibility
that oncogenic viruses affect only a sub-group of ophthalmic
pterygia.
 | Table IPrevalence of pterygium-associated
viruses in various studies. |
Table I
Prevalence of pterygium-associated
viruses in various studies.
|
Authors/(Refs.) | Date of
publication | HPV prevalence | HSV prevalence | CMV prevalence | EBV prevalence | Country of the
study | Method of
detection |
|---|
| Spandidos, et
al(28) | 1994 | - | 45% | 40% | 0% | Greece | PCR |
| Detorakis, et
al(18) | 2001 | 24% | 22% | - | - | Greece | PCR |
| | (Type 18) | | - | - | | |
| Gallagher, et
al(19) | 2001 | 50% | - | - | - | UK | PCR |
| | (Types
6,11,16) | | | | | |
| Piras, et
al(20) | 2003 | 100% | - | - | - | Italy | PCR-
sequencing |
| | 21% | | | | Equador |
| | (Types 52, 54,
candHPV90, unknown) | | | | |
| Schellini, et
al(21) | 2006 | 0% | - | - | - | Brazil | PCR |
| Sjö, et
al(34) | 2007 | 4.4%a | - | - | - | Denmark | PCR-ISH |
| | (Type 6) | | | | | |
| Chen, et
al(29) | 2008 | - | 5%a | - | - | Taiwan | PCR-ISH |
| Takamura, et
al(23) | 2008 | 4.8%b | - | - | - | Japan | PCR-HC II |
| Rodrigues, et
al(24) | 2008 | 58.3% | | | | Brazil | PCR |
| | (Types 1, 2,
16) | | | | | |
| Otlu, et
al(25) | 2009 | 0% | - | - | 10% | Turkey | Real-time PCR |
| Tsai, et
al(16) | 2009 | 24% | - | - | - | Taiwan | Nested-PCR |
| | (Types 16, 18) | - | - | - | Poland | PCR |
| Piecyk-Sidor, et
al(26) | 2009 | 27.6% | | | | | |
| | (Types 5, 6, 11,
16, 18, 31, 52, 59) | | | | | |
| Hsiao, et
al(27) | 2010 | 3% | - | - | - | Taiwan | PCR-ISH |
| | (Type 18) | | | | | |
4. Current status on HPV detection in
pterygium
Taking into account that HPV is by far the most
commonly reported oncogenic virus associated with ophthalmic
pterygium, several studies have focused on HPV detection and typing
to assess the potential role HPV plays in the pathogenetic process
leading to pterygium development. Of note, certain studies (such as
those of Sjö et al from Denmark, Takamura et al from
Japan or Hsiao et al from Taiwan) have failed to detect HPV
or report very low prevalences of HPV in examined pterygia
(21–23,25,27). Moreover, Dushku et al
detected p53 overexpression in the limbal epithelium of the
pterygia studied with all the samples being negative for HPV DNA,
suggesting that factors other than HPV infection were responsible
for the p53 overexpression (12).
To investigate the role of HPV and the variance in its prevalence
in pterygium in the different studies, Piras et al(20) selected patients from two distant
geographically populations, Italy and Ecuador. HPV was detected in
all the pterygia of Italian patients, but in only 21% of the
pterygia from Ecuador. In that study, geographic and ethnic factors
were proposed as a possible explanation for differences in HPV
prevalence in pterygium, supporting its multi-factorial
pathogenesis (20).
5. HPV detection in ocular surface
lesions
Over the past three decades HPV DNA has been
detected in various ophthalmic lesions of the ocular surface and
even in phenotypically normal conjunctiva (30,31). HPV infection has been strongly
correlated with the pathogenesis and recurrence of conjunctival
papillomas, conjunctival intraepithelial neoplasia (CIN) and even
squamous cell carcinoma of the conjunctiva (SCCC) (32–36). HPV may also co-exist in SCCC
lesions with other oncogenic viruses, such as HIV, thus it is
difficult to determine the importance of HPV per se in the
development of these lesions (36). The fact that pterygium has also
often been reported to co-exist with ocular surface neoplastic
lesions (37,38), supports the hypothesis of
oncogenic viral infection or co-operation as a pathogenetic model.
Obtaining cells from the ocular surface via non-invasive
methodologies, including exfoliation cytology techniques (39), may enable the detection of
HPV-infected pterygia.
6. Methodologies for HPV detection in
pterygium
HPVs are non-enveloped viruses with icosahedral
symmetry, composed of a circular double-stranded DNA genome. HPVs
cause infections of the skin and the mucous membranes of the
anogenital region and the oropharynx. Over 100 types have been
fully sequenced and some seem to play an important role in the
development of tumors. According to their oncogenic potential, HPVs
are divided into low- and high-risk types (oncogenic/high-risk
types: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82
and potentially oncogenic types: 26, 53, 66) (17,40,41).
Diagnosis of the viral infection is based on the
detection of the HPV-DNA. However, the mode of sample collection,
the quantity of the HPV-DNA of the isolated sample and the use of
various HPV-DNA detection techniques with different sensitivity and
specificity, are factors that may significantly affect the
detection rates of HPV infections (40).
HPV-DNA can be directly isolated from a biopsy
specimen with in situ hybridization (ISH), Southern blotting
and dot blot hybridization. However, these techniques are
laborious, need a large quantity of purified DNA and their
sensitivity is limited (40).
In cases where the biopsy specimen is small with a
limited quantity of HPV-DNA, nucleic acid amplification assays can
be used to increase the sensitivity and specificity of the test.
Hybrid Capture II (HC-II) is a non-radioactive signal amplification
technique, accurate for mucosal lesions, that distinguishes
high-risk from low-risk HPV-types, but is not appropriate for
genotyping (40–42).
Due to its high sensitivity, polymerase chain
reaction (PCR) is frequently associated with a high rate of
false-positive results (43).
Southern blot, dot blot, reverse dot blot, digestion with
restriction endonucleases or direct sequence analysis performed
after DNA amplification can help increase the sensitivity and
specificity of the test (41,42). Real-time PCR or quantitative PCR
(qPCR) permits rapid detection and quantification of the viral load
during the various cycles of the PCR process (real-time) (43). Reverse transcriptase-PCR (RT-PCR)
is a qualitative assay that permits the identification of viral
gene expression with the use of reverse transcriptase. The
combination of the two techniques, quantitative RT-PCR or real-time
RT-PCR (qRT-PCR), is considered to be the first choice assay for
the detection of viral gene expression as it combines quantitative
and qualitative advantages of the two methods (44,45).
7. Potential therapeutic interventions in
HPV-infected pterygium
Current treatment of pterygium includes surgical
excision and occasionally adjunctive therapy. Several surgical
techniques have been described: bare sclera closure, sliding
conjunctival flaps, use of autologous conjunctival and limbal
grafts or amniotic membranes (2,46)
(Fig. 2). Due to the possible
complications and costs of surgical treatment and the risk of
recurrence, often aggressive, various adjunctive therapies have
been proposed, including β-irradiation and the use of mitomycin C
or 5-fluorouracil. However these methods have been associated with
corneoscleral necrosis and melting, limbal stem cell deficiency and
variable recurrence rates. B-irradiation has also been associated
with cataract formation (2,46).
Interferons are a family of proteins with antiviral,
antiproliferative, antiangiogenetic and immunomodulatory
properties, produced from the organism in response to various
stimuli (47). The recombinant
form α-2b (IFN-α-2b) has been used for the treatment of condylomata
acuminata, chronic hepatitis B and C, Kaposi sarcoma, malignant
melanoma, hairy cell leukemia and follicular lymphoma (47). Unlike mitomycin C and
5-fluorouracil, adverse effects associated with the topical or
sub-conjunctival administration of IFN-α-2b are less severe
(48–52). IFN-α-2b in the form of eye drops
has successfully been used thus far in the management of CIN and
conjunctival papilloma (48–51). IFN-α-2b has also been reported to
prevent the recurrence of pterygium (52). However, additional investigation
is required to fully assess the value of this treatment modality in
the treatment of pterygium.
8. Conclusion
Despite controversies in the medical literature
concerning HPV involvement in pterygium (possibly due to racial
susceptibility or methodological differences), most studies agree
that HPV is detected in at least a sub-group of pterygia and that
HPV infection may affect both pathogenesis and clinical behaviour
(including recurrence) of these lesions. Accordingly, it would be
interesting to explore the possibility of anti-viral medications or
even vaccination, which may represent novel options in the therapy
of selected, HPV-infected pterygia.
References
|
1
|
Detorakis ET and Spandidos DA:
Pathogenetic mechanisms and treatment options for ophthalmic
pterygium: Trends and perspectives (Review). Int J Mol Med.
23:439–447. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hirst LW: The Treatment of pterygium. Surv
Ophthalmol. 48:145–180. 2003. View Article : Google Scholar
|
|
3
|
Coroneo MT: Pterygium as an early
indicator of ultraviolet insolation: a hypothesis. Br J Ophthalmol.
77:734–739. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chui J, Coroneo MT, Tat LT, Crouch R,
Wakefield D and Di Girolamo N: Ophthalmic pterygium: a stem cell
disorder with premalignant features. Am J Pathol. 178:817–827.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Detorakis ET, Zaravinos A and Spandidos
DA: Growth factor expression in ophthalmic pterygia and normal
conjunctiva. Int J Mol Med. 25:513–516. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Di Girolamo N, Wakefield D and Coroneo MT:
Differential expression of matrix metalloproteinases and their
tissue inhibitors at the advancing pterygium head. Invest
Ophthalmol Vis Sci. 41:4142–4149. 2000.PubMed/NCBI
|
|
7
|
Tsai YY, Chiang CC, Yeh KT, Lee H and
Cheng YW: Effect of TIMP-1 and MMP in pterygium invasion. Invest
Ophthalmol Vis Sci. 51:3462–3467. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aspiotis M, Tsanou E, Gorezis S, Ioachim
E, Skyrlas A, Stefaniotou M and Malamou-Mitsi V: Angiogenesis in
pterygium: study of microvessel density, vascular endothelial
growth factor, and thrombospondin-1. Eye (Lond). 21:1095–1101.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Solomon A, Li DQ, Lee SB and Tseng SC:
Type plasminogen activator in primary pterygium body fibroblasts by
inflammatory cytokines. Invest Ophthalmol Vis Sci. 41:2154–2163.
2000.PubMed/NCBI
|
|
10
|
Solomon A, Grueterich M, Li DQ, Meller D,
Lee SB and Tseng SC: Overexpression of insulin-like growth
factor-binding protein-2 in pterygium body fibroblasts. Invest
Ophthalmol Vis Sci. 44:573–580. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Detorakis ET, Sourvinos G, Tsamparlakis J
and Spandidos DA: Evaluation of loss of heterozygosity and
microsatellite instability in human pterygium: clinical
correlations. Br J Ophthalmol. 82:1324–1328. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dushku N, Hatcher SL, Albert DM and Reid
TW: P53 expression and relation to human papillomavirus infection
in pingueculae, pterygia, and limbal tumors. Arch Ophthalmol.
117:1593–1599. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Soussi T, Dehouche K and Béroud C: P53
website and analysis of P53 gene mutations in human cancer: forging
a link between epidemiology and carcinogenesis. Hum Mutat.
15:105–113. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Freed-Pastor WA and Prives C: Mutant p53:
one name, many proteins. Genes Dev. 26:1268–1286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Detorakis ET, Drakonaki EE and Spandidos
DA: Molecular genetic alterations and viral presence in ophthalmic
pterygium. Int J Mol Med. 6:35–41. 2000.PubMed/NCBI
|
|
16
|
Tsai YY, Chang CC, Chiang CC, Yeh KT, Chen
PL, Chang CH, Chou MC, Lee H and Cheng YW: HPV infection and p53
inactivation in pterygium. Mol Vis. 15:1092–1097. 2009.PubMed/NCBI
|
|
17
|
Burk RD, Chen Z and Van Doorslaer K: Human
papillomaviruses: genetic basis of carcinogenicity. Public Health
Genomics. 12:281–290. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Detorakis ET, Sourvinos G and Spandidos
DA: Detection of herpes simplex virus and human papilloma virus in
ophthalmic pterygium. Cornea. 20:164–167. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gallagher MJ, Giannoudis A, Herrington CS
and Hiscott P: Human papillomavirus in pterygium. Br J Ophthalmol.
85:782–784. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Piras F, Moore PS, Ugalde J, Perra MT,
Scarpa A and Sirigu P: Detection of human papillomavirus DNA in
pterygia from different geographical regions. Br J Ophthalmol.
87:864–866. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schellini SA, Hoyama E, Shiratori CA,
Sakamoto RH and Candeias JM: Lack of papillomavirus (HPV) in
pterygia of a Brazilian sample. Arq Bras Oftalmol. 69:519–521.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sjö NC, von Buchwald C, Prause JU, Norrild
B, Vinding T and Heegaard S: Human papillomavirus and pterygium. Is
the virus a risk factor? Br J Ophthalmol. 91:1016–1018.
2007.PubMed/NCBI
|
|
23
|
Takamura Y, Kubo E, Tsuzuki S and Akagi Y:
Detection of human papillomavirus in pterygium and conjunctival
papilloma by hybrid capture II and PCR assays. Eye (Lond).
22:1442–1445. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rodrigues FW, Arruda JT, Silva RE and
Moura KK: Polymorphism and human papillomavirus DNA associated with
pterygium. Genet Mol Res. 7:1251–1258. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Otlu B, Emre S, Turkcuoglu P, Doganay S
and Durmaz R: Investigation of human papillomavirus and
Epstein-Barr virus DNAs in pterygium tissue. Eur J Ophthalmol.
19:175–179. 2009.PubMed/NCBI
|
|
26
|
Piecyk-Sidor M, Polz-Dacewicz M, Zagórski
Z and Zarnowski T: Occurrence of human papillomavirus in pterygia.
Acta Ophthalmol. 87:890–895. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hsiao CH, Lee BH, Ngan KW, Chuang WY,
Yeung L, Yeh LK, Tan HY, Hui-Kang D and Lin KK: Presence of human
papillomavirus in pterygium in Taiwan. Cornea. 29:123–127. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Spandidos D, Xinarianos G, Ergazaki M,
Giannoudis A and Tsamparlakis J: The presence of herpesviruses in
pterygium. Int J Oncol. 5:749–752. 1994.PubMed/NCBI
|
|
29
|
Chen YF, Hsiao CH, Ngan KW, Yeung L, Tan
HY, Yang KH, Huang SC and Lin KK: Herpes simplex virus and
pterygium in Taiwan. Cornea. 27:311–313. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Karcioglu ZA and Issa TM: Human papilloma
virus in neoplastic and non-neoplastic conditions of the external
eye. Br J Ophthalmol. 81:595–598. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
McDonnell JM, McDonnell PJ and Sun YY:
Human papillomavirus DNA in tissues and ocular surface swabs of
patients with conjunctival epithelial neoplasia. Invest Ophthalmol
Vis Sci. 33:184–189. 1992.PubMed/NCBI
|
|
32
|
Saegusa M, Takano Y, Hashimura M, Okayasu
I and Shiga J: HPV type 16 in conjunctival and junctional
papilloma, dysplasia, and squamous cell carcinoma. J Clin Pathol.
48:1106–1110. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sjö NC, Heegaard S, Prause JU, von
Buchwald C and Lindeberg H: Human papillomavirus in conjunctival
papilloma. Br J Ophthalmol. 85:785–787. 2001.
|
|
34
|
Sjö NC, von Buchwald C, Cassonnet P,
Norrild B, Prause JU, Vinding T and Heegaard S: Human
papillomavirus in normal conjunctival tissue and in conjunctival
papilloma: types and frequencies in a large series. Br J
Ophthalmol. 91:1014–1015. 2007.PubMed/NCBI
|
|
35
|
Kiire CA and Dhillon B: The aetiology and
associations of conjunctival intraepithelial neoplasia. Br J
Ophthalmol. 90:109–113. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ateenyi-Agaba C, Franceschi S,
Wabwire-Mangen F, Arslan A, Othieno E, Binta-Kahwa J, van Doorn LJ,
Kleter B, Quint W and Weiderpass E: Human papillomavirus infection
and squamous cell carcinoma of the conjunctiva. Br J Cancer.
102:262–267. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hirst LW, Axelsen RA and Schwab I:
Pterygium and associated ocular surface squamous neoplasia. Arch
Ophthalmol. 127:31–32. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Artornsombudh P, Sanpavat A,
Tinnungwattana U, Tongkhomsai V, Sansopha L and Tulvatana W:
Prevalence and clinicopathologic findings of conjunctival
epithelial neoplasia in pterygia. Ophthalmology. 120:1337–1340
|
|
39
|
Bandyopadhyay R, Nag D, Mondal SK,
Gangopadhyay S, Bagchi K and Bhaduri G: Ocular surface disorder in
pterygium: role of conjunctival impression cytology. Indian J
Pathol Microbiol. 53:692–695. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Abreu AL, Souza RP, Gimenes F and
Consolaro ME: A review of methods for detect human Papillomavirus
infection. Virol J. 9:2622012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Molijn A, Kleter B, Quint W and van Doorn
LJ: Molecular diagnosis of human papillomavirus (HPV) infections. J
Clin Virol. 32(Suppl 1): S43–S51. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Leto Md, Santos Júnior GF, Porro AM and
Tomimori J: Human papillomavirus infection: etiopathogenesis,
molecular biology and clinical manifestations. An Bras Dermatol.
86:306–317. 2011.(In English, Portuguese).
|
|
43
|
Mackay IM: Real-time PCR in the
microbiology laboratory. Clin Microbiol Infect. 10:190–212. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Bustin SA, Benes V, Nolan T and Pfaffl MW:
Quantitative real-time RT-PCR - a perspective. J Mol Endocrinol.
34:597–601. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Jensen EC: Real-time reverse transcription
polymerase chain reaction to measure mRNA: use, limitations, and
presentation of results. Anat Rec (Hoboken). 295:1–3. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Todani A and Melki SA: Pterygium current
concepts in pathogenesis and treatment. Int Ophthalmol Clin.
49:21–30. 2009.PubMed/NCBI
|
|
47
|
Jonasch E and Haluska FG: Interferon in
oncological practice: review of interferon biology, clinical
applications, and toxicities. Oncologist. 6:34–55. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Vann RR and Karp CL: Perilesional and
topical interferon alfa-2b for conjunctival and corneal neoplasia.
Ophthalmology. 106:91–97. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Karp CL, Moore JK and Rosa RH Jr:
Treatment of conjunctival and corneal intraepithelial neoplasia
with topical interferon alpha-2b. Ophthalmology. 108:1093–1098.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Schechter BA, Schrier A, Nagler RS, Smith
EF and Velasquez GE: Regression of presumed primary conjunctival
and corneal intraepithelial neoplasia with topical interferon
alpha-2b. Cornea. 21:6–11. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Schechter BA, Rand WJ, Velazquez GE,
Williams WD and Starasoler L: Treatment of conjunctival papillomata
with topical interferon Alfa-2b. Am J Ophthalmol. 134:268–270.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Esquenazi S: Treatment of early pterygium
recurrence with topical administration of interferon alpha-2b. Can
J Ophthalmol. 40:185–187. 2005. View Article : Google Scholar : PubMed/NCBI
|