Introduction
Metformin is an oral biguanide agent widely used for
the treatment of type 2 diabetes mellitus (1). Several studies have indicated that
metformin lowers the risk of developing several types of cancer,
including those of the breast, the colon and the prostate (2–5).
Furthermore, metformin has been shown to inhibit cancer cell
proliferation and tumor growth in animal models (6–8).
The mechanisms underlying the anticancer effects of metformin vary
(8,9); among these, the activation of
AMP-activated protein kinase (AMPK) is pivotal (9,10).
AMPK is composed of a catalytic subunit (α1 or α2) and 2 regulatory
subunits (β1 or β2 and γ1, γ2 or γ3) (11). Previous studies have confirmed
that the activation of AMPK by metformin is involved in mediating
the anticancer effects of metformin, with metformin-induced AMPK
activation leading to the inhibition of mTOR and a reduction in
global translation initiation (12,13).
The Sonic hedgehog (Shh) signaling pathway is
critical to cell growth and differentiation during embryonic
development (14). The Shh
signaling cascade is initiated when the Shh ligand binds to the
cell surface receptor Patched (Ptc), which then releases its
inhibitory hold on Smo. Subsequently, Smo attains the ability to
transduce the signal by activating the transcriptional activator
form of Gli-1, which regulates the expression of target genes that
control cell growth, survival and differentiation in various types
of tissue (15–17). Previous studies have demonstrated
the ligand-dependent constitutive activation of the Shh pathway in
several types of tumors, including those of the breast (18,19). Another study further demonstrated
that a high mRNA expression of Shh, Ptc, Gli-1 and Smo in breast
cancer tissue correlates with breast cancer cell invasiveness
(20). Therefore, targeting the
aberrant activation of the Shh signaling pathway may represent a
novel treatment regime for breast cancer. Moreover, metformin has
been found to have an effect on the Shh signaling pathway. A recent
study indicated that metformin suppresses Shh expression in
pancreatic cancer cells (21).
However, it only showed that metformin reduced the expression of
Shh in the BxPC3 pancreatic cancer cell line. It still remains
unclear as to whether metformin exerts anticancer effects through
the Shh pathway.
Breast cancer is derived from and maintained by a
fraction of self-renewing tumor-initiating cells, referred to as
cancer stem cells (CSCs) (22–24). Similar to other stem cells, CSCs
possess the ability of self-renewal and can differentiate into
various types of cancer cells (25,26). Pervious studies have identified
pivotal roles for CSCs in tumor growth, invasion, metastasis and
resistance to chemotherapy (27,28). A human breast cancer cell
population characterized by a CD44+/CD24−
surface marker profile has been reported to be highly enriched in
CSCs (25,29). However, the molecular mechanisms
regulating the maintenance, self-renewal and differentiation of
breast CSCs (BCSCs) remain poorly understood.
While an increasing number of studies have
demonstrated the antitumor effects of metformin, little is known
regarding the underlying mechanisms through which metformin affects
breast cancer development. In particular, the role of the Shh
signaling pathway in the anticancer effects of metformin in breast
cancer remains unclear. In the present study, we initially
investigated whether metformin decreases neoplastic cell
proliferation and selectively kills CSCs through the Shh signaling
pathway in human breast cancer. We also explored the possible
association between the Shh signaling pathway and AMPK.
Materials and methods
Cell culture
The MDA-MB-231, MCF-7 and BT-549 human breast cancer
cell lines were obtained from the American Type Culture Collection
(ATCC; Manassas, VA, USA). The MDA-MB-231 and BT-549 cells were
cultured in RPMI-1640 medium (Invitrogen, Carlsbad, CA, USA)
supplemented with 10% fetal bovine serum (FBS; Gibco, Carlsbad, CA,
USA) and 1% penicillin/streptomycin. The MCF-7 cells were grown in
Dulbecco’s modified Eagle’s medium (DMEM; Invitrogen, Carlsbad, CA,
USA) supplemented with 10% FBS and 1% penicillin/streptomycin. The
cells were maintained at 37°C in a humidified atmosphere with 5%
CO2.
RNA interference
Small interfering RNA (siRNA) specific to AMPKα1 was
synthesized by Shanghai GeneChem Co., Ltd. (Shanghai, China) with
the following target sequences: PRKAA1-RNAi-24250-1 (siAMPK#1),
TAAAGTAGCTGTGAAGATA; PRKAA1-RNAi-24251-1 (siAMPK#2),
ATGCAAAGATAGCTGATTT; PRKAA1-RNAi-24252-1 (siAMPK#3),
GGTCCATAGAGATTTGAAA; control siRNA (siAMPK Ctr),
TTCTCCGAACGTGTCACGT. The cells were seeded in dishes until they
grew to 80% confluence, and at the appointed time they were
transfected with AMPKα1 siRNA or siCtr using Lipofectamine 2000
transfection reagent (Invitrogen) according to the manufacturer’s
instructions. The AMPKα1 siRNA that effectively inhibited the
expression of AMPK at the protein level was used in the following
experiments. MDA-MB-231 cells not transfected with AMPKα1 siRNA or
siCtr were used as negative controls.
RNA extraction and reverse
transcription-polymerase chain reaction (RT-PCR)
Total cellular RNA was extracted from the untreated
(controls) and metformin-treated (metformin was obtained from Sigma
Chemical, St. Louis, MO, USA) breast cancer cells using TRIzol
reagent according to the manufacturer’s instructions (Invitrogen).
The RNA was reverse-transcribed with SuperScript II Reverse
Transcriptase (Invitrogen) in the presence of oligo-dT and random
primers. PCR amplifications of Shh cDNA generated a product of 477
bp using the forward primer, 5′-CGCACGGGGACAGCTCGGAAGT-3′ and the
reverse primer, 5′-CTGCGCGGCCCTCGTAGTGC-3′. The product of Smo was
322 bp with the forward primer, 5′-TTACCTTCAGCTGCCACTTCTACG-3′ and
the reverse primer, 5′-GCCTTGGCAATCATCTTGCTCTTC-3′. The product of
Ptc was 215 bp with the forward primer, 5′-TCTGCAGCAACTATACGAGC-3′
and the reverse primer, 5′-GAACAGCTCGACCGTCATCA-3′. The product of
Gli-1 was 363 bp with the forward primer, 5′-GGACAACCGCCATCC
AGACT-3′ and the reverse primer, 5′-GCCAGGGACACCTCCATCTC-3′. The
product of GAPDH was 697 bp with the forward primer,
5′-TCACCATCTTCCCAGGAGCGAG-3′ and the reverse primer,
5′-TGTCGCTGTTGAAGTCAGAG-3′. The PCR products were analyzed by DNA
gel electrophoresis on a 1% agarose gel and the intensity of each
band was quantified using BandScan software. The relative
expression levels of Shh, Smo, Ptc and Gli-1 were normalized to the
intensity of the GAPDH bands, which served as a loading control;
data are presented as the means ± standard deviation (SD).
Western blot analysis
Cells in a monolayer culture were washed 3 times
with ice-cold PBS and lysed in RIPA buffer containing protease
inhibitor cocktail (Roche Diagnostics Corp., Indianapolis, IN,
USA). The cell debris was removed by centrifugation at 14,000 × g
for 20 min at 4°C. Protein concentrations were determined using an
enhanced BCA protein assay kit (Beyotime Institute of
Biotechnology, Jiangsu, China). The lysates were dissolved in
Laemmli buffer, boiled for 5 min and separated (20–30 µg
protein per lane) by SDS-PAGE (10%), followed by electrotransfer
onto polyvinylidene difluoride membranes. After blocking in 5%
bovine serum albumin (BSA) in Tris-buffered saline containing
Tween-20 (TBST) for 2 h at room temperature, the membranes were
incubated with primary antibody at 4°C overnight. Subsequently, the
membranes were washed with TBST 3 times followed by incubation with
peroxidase-conjugated secondary anti-mouse (sc-390944) or
anti-rabbit (sc-292373) antibodies (1:10,000; Santa Cruz
Biotechnology, Inc., Santa Cruz, CA, USA) at room temperature for 1
h. After washing again with TBST 3 times, proteins were detected
using the ECL Western blotting detection kit (Bio-Rad Laboratories,
Hercules, CA, USA). The primary antibodies employed included
anti-β-actin (1:2,000; Cat. no. 3700s; Cell Signaling Technology,
Danvers, MA, USA), anti-Smo (1:1,000; ab-38686; Cell Signaling
Technology), anti-Gli-1 (1:1,000; Cat. no. 3538s; Cell Signaling
Technology), anti-Ptc (1:1,000; Cat. no. 2468s; Cell Signaling
Technology), anti-AMPK (1:1,000; Cat. no. 2795s; Cell Signaling
Technology) and anti-Shh (1:1,000; Cat. no. sc-9024; Santa Cruz
Biotechnology, Inc.) antibodies.
Cell proliferation assay
The cells were seeded in 96-well plates in complete
culture medium, and after 24 h of growth, the cells were exposed to
recombinant human Shh (rhShh) (1 µg/ml; R&D Systems,
Minneapolis, MN, USA), metformin (3 mM) or a combination of both.
Following further incubation at 37°C in a humidified atmosphere
with 5% CO2, 50 µl of
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
stock solution (5 mg/ml; Sigma Chemical) were added to each well at
the 0, 12, 24, 48 or 72 h time points, and the plates were
incubated for an additional 4 h at 37°C. The solution was then
removed from each well, and 150 µl of dimethyl sulfoxide
were added. Following gentle agitation, the absorbance at 490 nm
was measured using an EL800 microplate reader (Bio-Tek Instruments,
Winooski, VT, USA). Experiments were independently performed in
triplicate, and 4 parallel samples were measured each time.
Colony formation assay
The MCF-7 and MDA-MB-231 cells were trypsinized, and
500 viable cells were subcultured in 60-mm plates containing
complete medium. Each treatment condition was conducted in
triplicate. After 3 weeks of growth, the cells were fixed and
stained with a solution containing 0.5% crystal violet and 25%
methanol in water. After staining, the cells were washed with PBS.
Visible colonies were macroscopically counted according to the cell
numbers in each colony. All experiments were repeated 3 times.
Tumor xenografts in BALB/c-nu mice
Six-week-old female BALB/c-nu mice were obtained
from the Shanghai Slac Laboratory Animal Co., Ltd.
(Shanghai,China). The mice were maintained in a specific
pathogen-free facility. All experimental protocols were reviewed by
the Committee on the Ethics of Animal Experiments of Shandong
University (Jinan, China) and were carried out according to the
Guidelines for Animal Experiments of Shandong University.
MDA-MB-231 cells (1.0×106) expressing green fluorescent
protein (GFP) were injected subcutaneously into the abdominal
mammary fat pads of these mice after they had become accommodated
to their new environment. The mice had continuous free access to
sterilized food and autoclaved water. When the tumor size was
approximately 4 mm in diameter, the animals were randomly divided
into 4 groups (3 mice per group), and treatment was initiated via
intratumoral injections of rhShh alone (1 mg/kg body weight, once
daily for 28 days;), oral gavage of metformin alone (100 mg/kg body
weight, once daily for 28 days), as previously described (30), or a combination of both drugs.
Tumor growth was compared with that of the controls (untreated
mice). The mice were observed daily for any discomfort and were
weighed every third day in order to detect tumor growth.
Detection of bioluminescence
The mice were anesthetized with a 2% isoflurane/air
mixture and were administered a single intraperitoneal dose of 150
mg/kg D-luciferin (Promega, Madison, WI, USA) in PBS. Images were
acquired between 5 and 15 min following the administration of
luciferin, and the peak luminescence signal was recorded using the
in vivo bioluminescence imaging system (IVIS) (IVIS
Spectrum; Xenogen, Hopkinton, MA, USA). The Living Image software
package was used to measure photon flux within a region of interest
to quantify the bioluminescence imaging signals emanating from the
tumors.
Immunohistochemical analysis
Following bioluminescence imaging, the mice were
sacrificed by exposure to 1-3% isoflurane and the tumor tissues
were excised, fixed and serially sectioned. Tumors derived from the
transplanted cells were fixed in 10% buffered neutralized formalin
for 48 h and embedded in paraffin. Consecutive sections
(4-µm-thick) were cut and processed for immunohistochemistry
with anti-Gli-1 antibodies (1:100 dilution). Briefly, the tissue
sections were deparaffinized with xylene, dehydrated with a graded
series of alcohols and then incubated in 3% (v/v) hydrogen peroxide
for 10 min at room temperature. Following 3 washes of 3 min each in
PBS, the tissue sections were microwaved for 20 min in 10 mM
citrate buffer (pH 6.0). Subsequently, the sections were washed a
further 3 times in PBS for 5 min each, and incubated with normal
goat serum to reduce non-specific binding. The tissue sections were
then incubated with rabbit polyclonal anti-Gli-1 antibodies (1:100
dilution) at 4°C overnight. The sections were washed 3 times in PBS
and biotinylated goat anti-mouse serum IgG (SP-9000; Beijing
Zhongshan Golden Bridge Biotechnology, Beijing, China) was used as
a secondary antibody. After washing 3 times in PBS, the sections
were incubated in streptavidinbiotin conjugated with horseradish
peroxidase, and the peroxidase reaction was developed with
3,3′-diaminobenzidine tetrahydro-chloride. Nuclei were
counterstained with hematoxylin. The slides were examined under a
light microscope, and representative images were captured from a
minimum of 5 different slides from each group. Gli-1 immunostaining
was regarded as positive with brown granules exhibited in the
cytoplasm of a cell.
Scratch-wound assay for the measurement
of cell migration
The cells were plated in 60-mm culture dishes, and
wounds were inflicted upon the cell monolayers using a sterile
plastic 200-µl micropipette tip. Phase-contrast microscopy
images were obtained immediately after wounding and again 48 h
later. The experiments were independently performed in triplicate,
and the migration distance under each condition was assessed by
analyzing the images using Adobe Photoshop (Adobe Systems, San
Jose, CA, USA).
Cell invasion assay
BD Matrigel-coated (BD Biosciences, San Jose, CA,
USA) Transwell inserts (6.5 mm; Corning Costar Corp., Cambridge,
MA, USA) containing polycarbonate filters with 8-µm pores
were used in the assay. The inserts were coated with 50 µl
of Matrigel matrix (1 mg/ml) according to the manufacturer’s
recommendations. The cells were seeded in the inserts, placed in
the upper chambers at a density of 2×105 cells in 200
µl serum-free medium, and 600 µl normal growth medium
was placed in the lower chambers. Following 24 h of treatment, the
cells on the upper surface of the membrane were removed, and the
cells on the lower chamber were fixed in 4% paraformaldehyde and
stained with 0.5% crystal violet. For each membrane, the number of
migratory and invasive cells in 5 random fields was counted at ×40
magnification. The experiments were performed in triplicate.
Mammosphere culture
The cells were trypsinized and mechanically
disrupted to obtain single-cell suspensions. The single-cell
suspensions were then plated in Ultra-Low attachment multi-well
plates (96-well plates; Corning Costar Corp.) at different
densities of viable cells in serum-free mammary epithelial growth
medium supplemented with 1:50 B27 (Invitrogen), 20 ng/ml epithelial
growth factor, 20 ng/ml basic fibroblast growth factor (BD
Biosciences) and 10 µg/ml heparin (Sigma) for 7-10 days. The
mammospheres were imaged and counted under a phase-contrast
microscope (IX70; Olympus, Tokyo, Japan).
Flow cytometric analysis of CD44 and CD24
expression
Cells growing in 60-mm dishes were washed once with
PBS and then harvested with 0.05% trypsin/0.025% EDTA. The cell
suspensions were washed with PBS and resuspended in wash buffer (1%
BSA in PBS). The cells (106/100 µl) were then incubated with
combinations of fluorochrome-conjugated monoclonal antibodies
against human CD44-APC (Cat. no. 559942; BD Biosciences), CD24-PE
(Cat. no. 555428; BD Biosciences) or IgG isotype controls for APC
and PE (BD Biosciences) in the dark for 30 min on ice. The labeled
cells were washed with PBS and then analyzed using a FACSCalibur
flow cytometer (BD Biosciences).
Statistical analysis
Data are presented as the means ± SD with experiment
numbers indicated in the figure legends. Differences between means
were assessed using the Student’s two-tailed t-test. The level of
significance was set at P<0.05. Statistical analysis was
performed using SPSS/Win11.0 software (SPSS, Inc., Chicago, IL,
USA).
Results
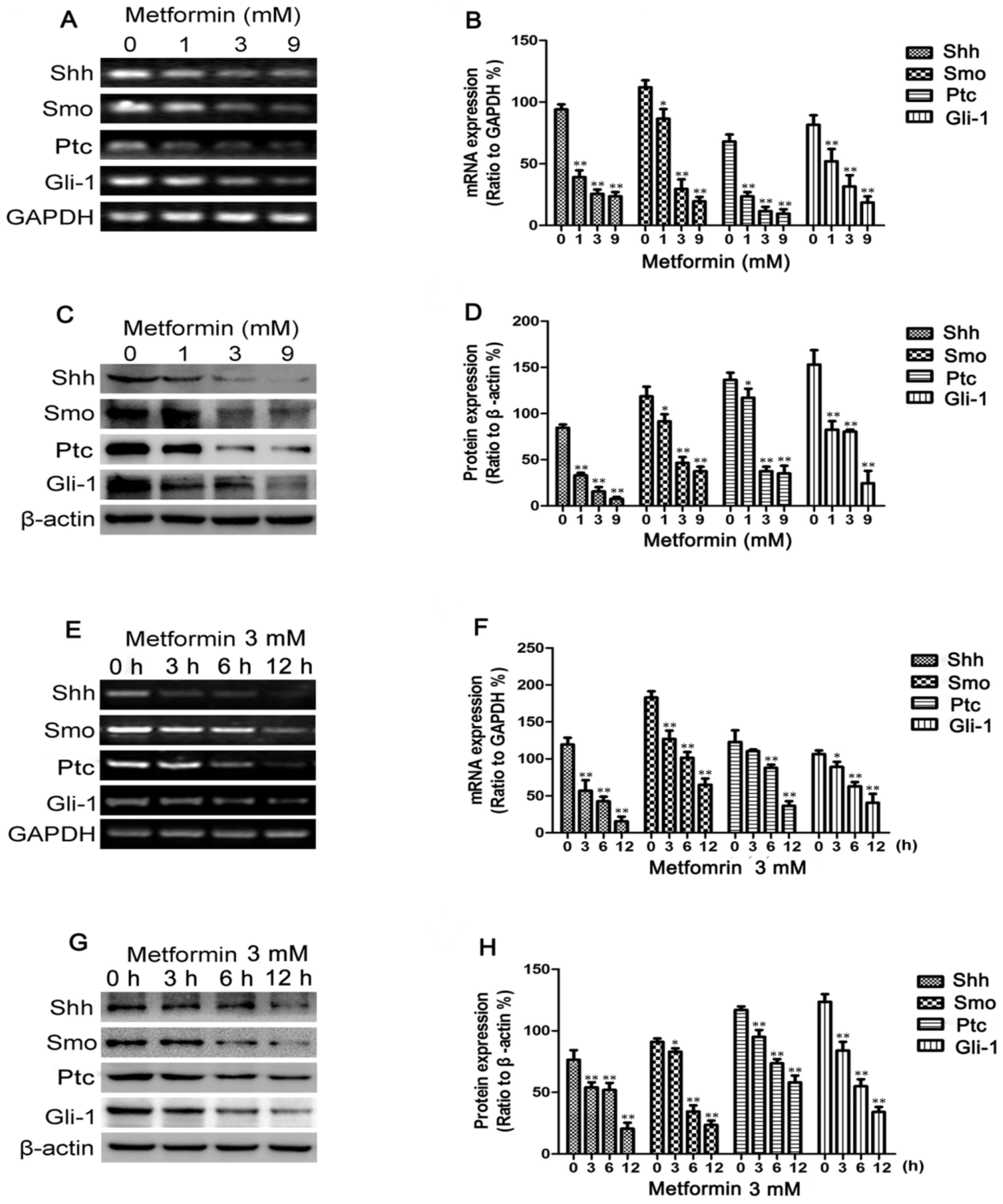
Metformin decreases Shh, Smo, Ptc and
Gli-1 expression in breast cancer cells
To determine whether metformin inhibits the Shh
signaling pathway in breast cancer cells, RT-PCR was employed to
measure the Shh, Smo, Ptc and Gli-1 mRNA levels following treatment
with metformin. The MDA-MB-231 cells were treated with various
concentrations of metformin (0–9 mmol/l), as previously described
(31), for 12 h or with 3 mM
metformin for different periods of time (0–12 h). As shown in
Fig. 1A and E, the mRNA
expression levels of Shh, Smo, Ptc and Gli-1 decreased in a dose-
and time-dependent manner following treatment with metformin. The
changes in Shh, Smo, Ptc and Gli-1 protein expression observed in
these cells following incubation with various concentrations of
metformin for 12 h or with 3 mM metformin for different periods of
time (0–12 h) were then determined by western blot analysis.
Metformin also decreased the protein levels in a dose- and
time-dependent manner (Fig. 1C and
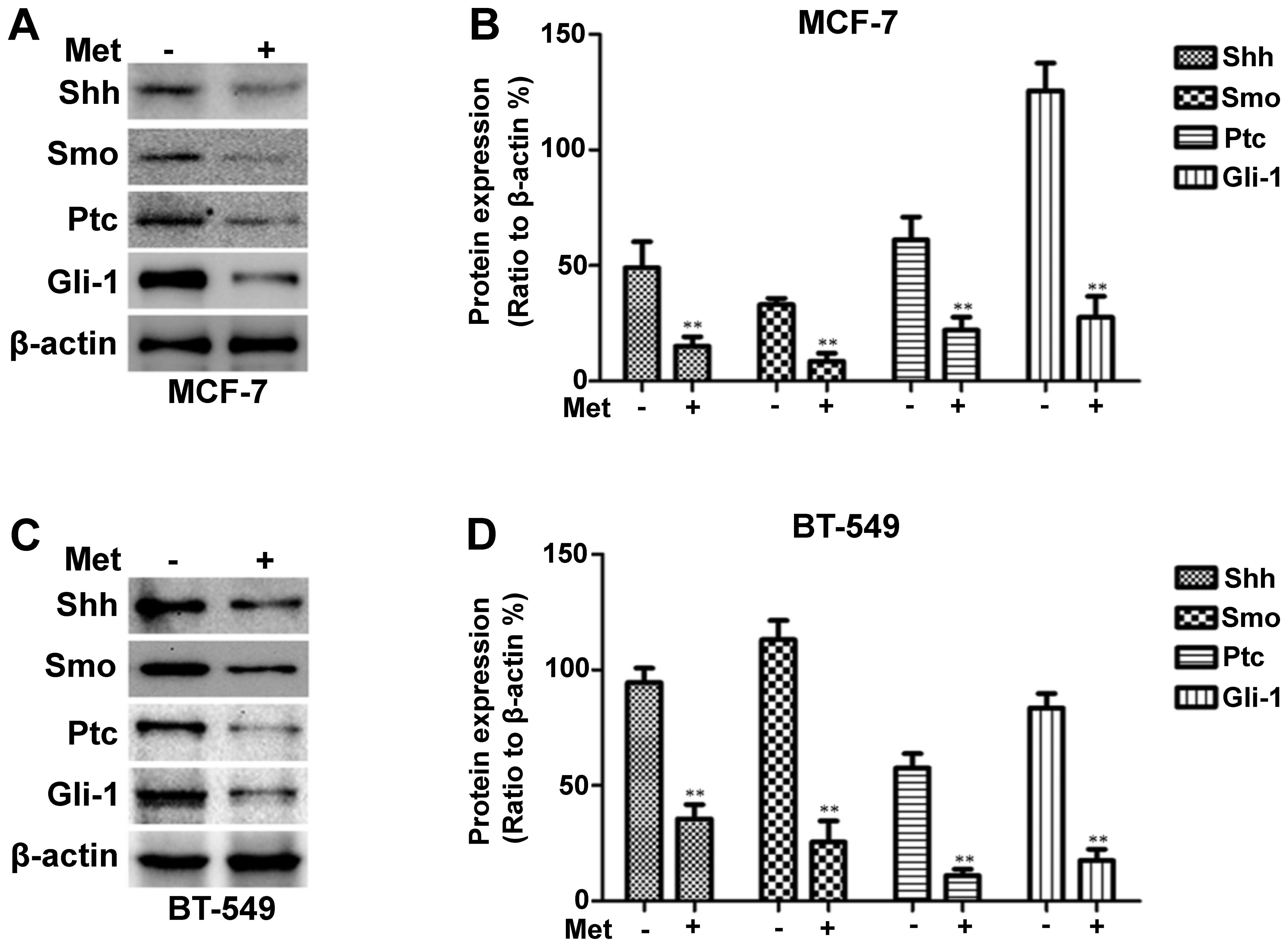
G). Treatment with metformin also suppressed Shh, Smo, Ptc and
Gli-1 protein expression in the MCF-7 and BT-549 cells, as shown in
Fig. 2.
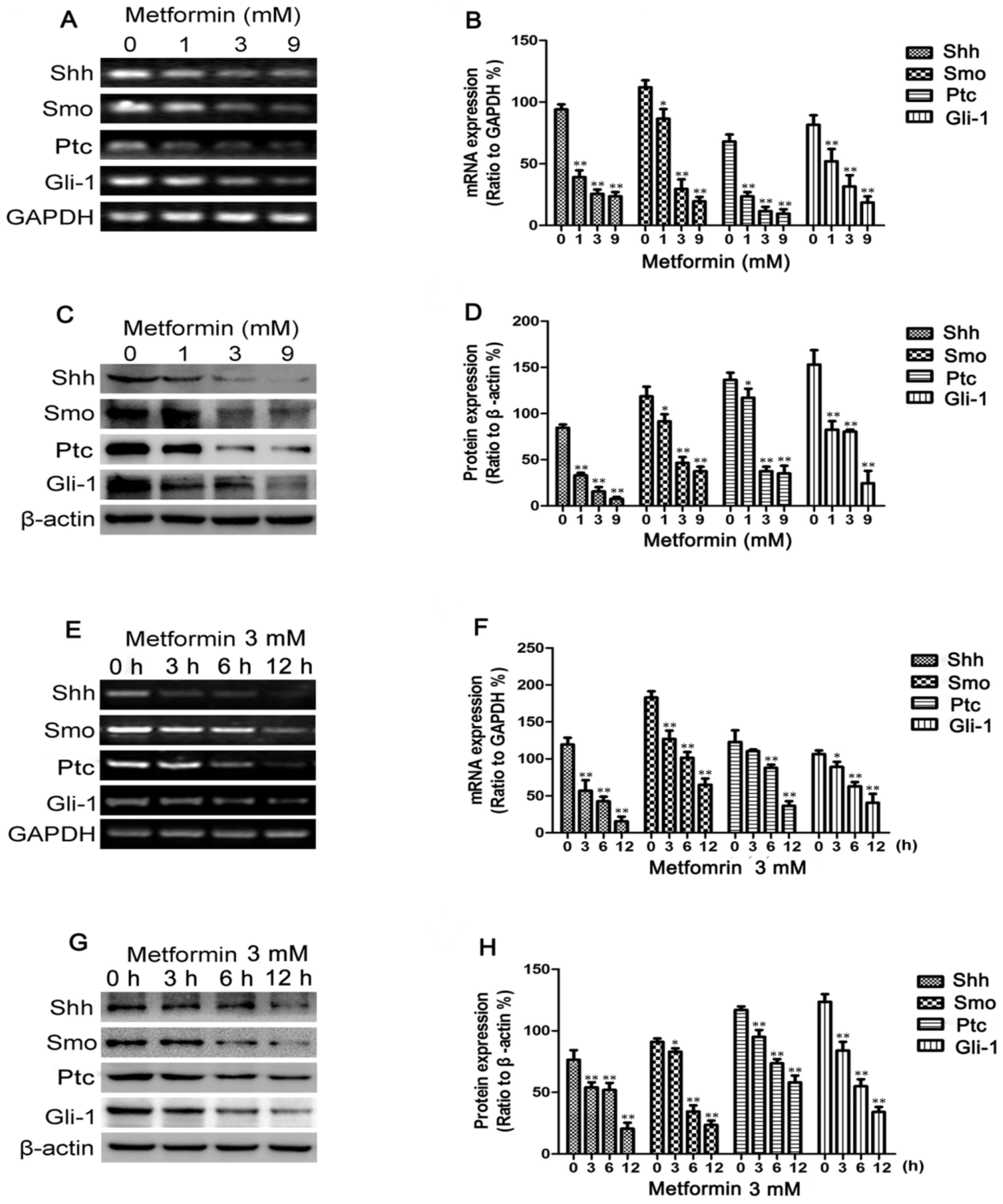 | Figure 1Metformin decreases Sonic hedgehog
(Shh), Smo, Patched (Ptc) and Gli-1 expression in MDA-MB-231 cells.
MDA-MB-231 cells were treated with metformin at concentrations of
0, 1, 3 or 9 mM for 12 h or with 3 mM of metformin for 0, 3, 6 and
12 h. (A and E) The mRNA levels of Shh, Smo, Ptc and Gli-1 were
measured by RT-PCR; GAPDH served as a control. (C and G) The
protein levels of Shh, Smo, Ptc and Gli-1 were measured by western
blot analysis; β-actin levels were measured as a loading control.
Histograms illustrate the (B and F) mRNA levels relative to those
of GAPDH and (D and H) protein expression relative to that of
β-actin. All data are presented as the means ± SD of 3 independent
experiments. *P<0.05 vs. the control group;
**P<0.01 vs. the control group. |
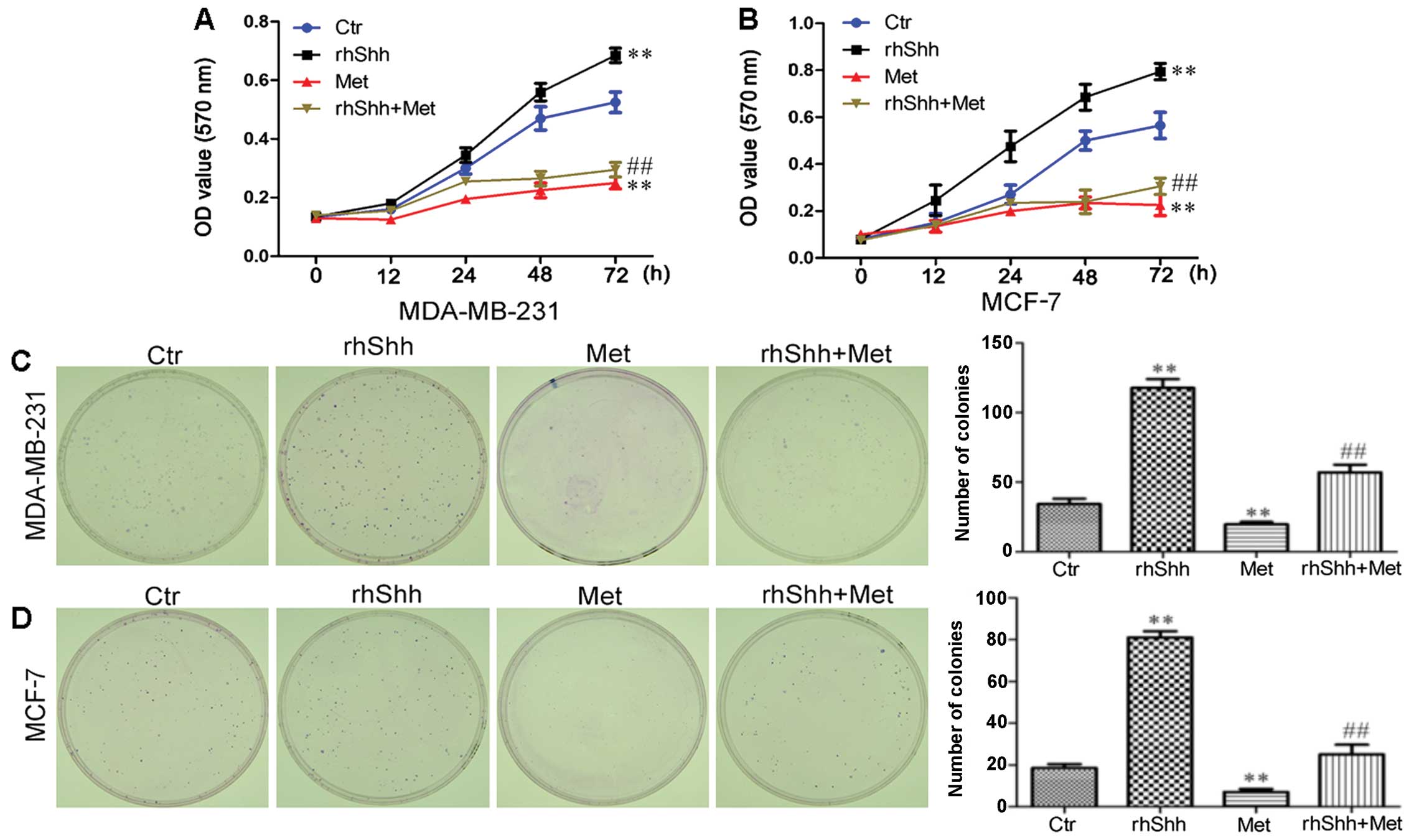
Metformin inhibits the rhShh-induced
proliferation of breast cancer cells
To determine whether the suppression of Shh
signaling by metformin contributes to the anticancer effects of the
latter, we treated the cells with rhShh, a specific activator of
the Shh signaling pathway. The effect of rhShh, metformin and rhShh
combined with metformin on the proliferation of MCF-7 and
MDA-MB-231 breast cancer cells was assessed by MTT assay. Treatment
with 1 µg/ml of rhShh increased the proliferation of these
cells in a time-dependent manner, while treatment with metformin
significantly decreased the growth of MDA-MB-231 and MCF-7 cells at
48 and 72 h after treatment (P<0.01 compared to control;
Fig. 3A and B). We also found
that treatment with 3 mM of metformin inhibited the effect of rhShh
in both the MDA-MB-231 and MCF-7 cells, with a statistically
significant difference identified at 72 h (P<0.01 compared to
rhShh treatment; Fig. 3A and B).
The proliferative potential of the breast cancer cells under the
same conditions was also assessed by a colony formation assay.
Incubation with metformin resulted in a significant decrease in
both the number and size of colonies compared with the control
group. In agreement with the results obtained by MTT assay,
treatment with 3 mM of metformin inhibited the increase in the
number and size of the colonies induced by rhShh when compared to
treatment with rhShh alone (Fig. 3C
and D).
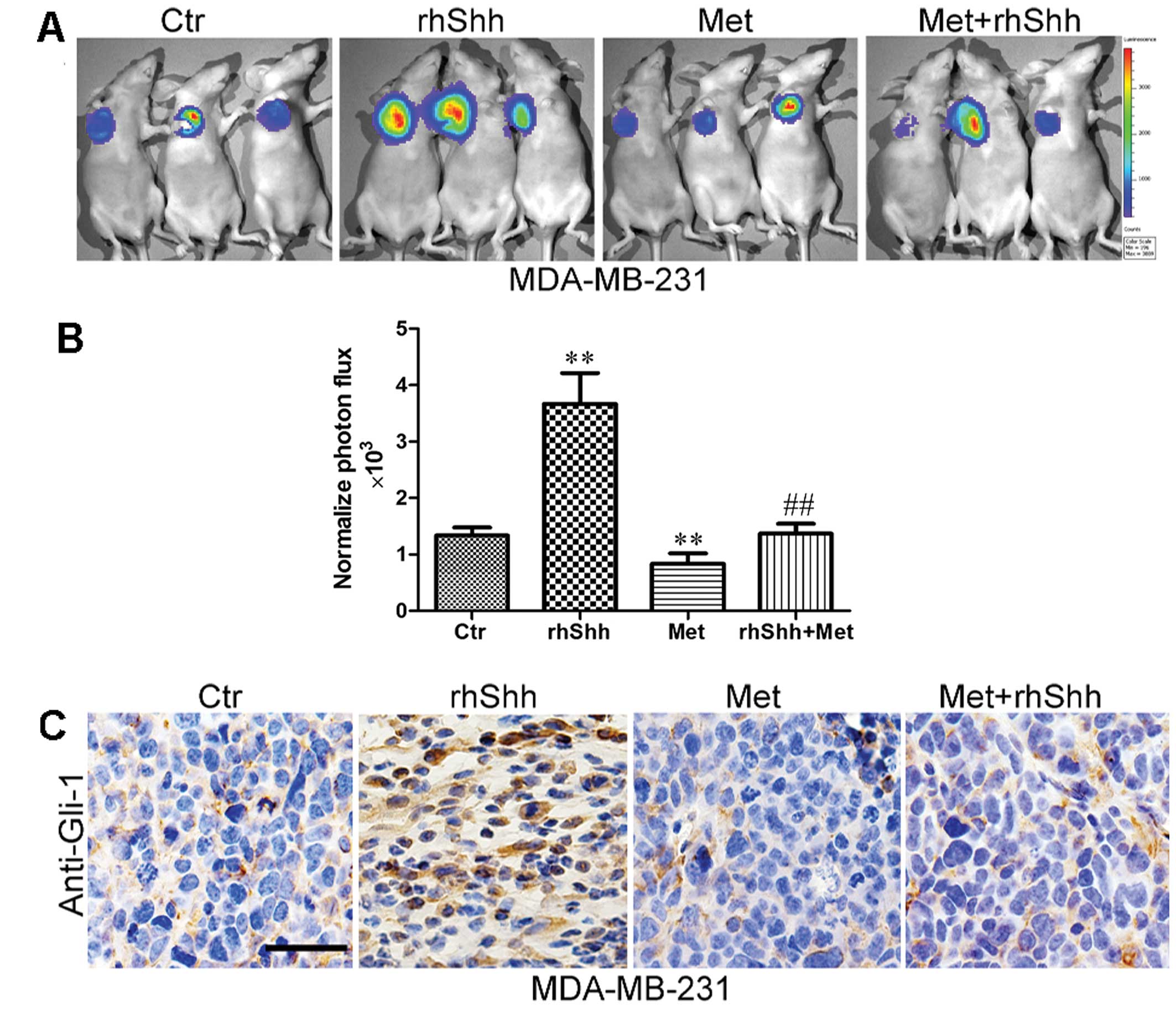
Metformin inhibits rhShh-induced tumor
growth in vivo
To examine the effects of metformin on rhShh-induced
tumor growth in vivo, a total of 1.0×106
MDA-MB-231 cells expressing GFP were implanted into the mammary fat
pads of BALB/c-nu mice. We then used IVIS to measure tumor growth
in order to improve the quality of the quantitative results. An
analysis of the bioluminescence imaging data indicated that the
rhShh treatment group generated significantly larger tumors than
the control group. However, the administration of metformin
significantly inhibited tumor growth (Fig. 4A). Furthermore, the mice in the
combined treatment group presented with tumors much smaller than
those of the mice in the rhShh treatment group (Fig. 4A). An approximately 2.3-fold
difference in the average signal intensity was observed between the
rhShh treatment group and the combination treatment group
(P<0.01; Fig. 4B).
Following bioluminescence imaging, the mice were
sacrificed by exposure to 1-3% isoflurane and the tumor tissues
were excised, fixed and serially sectioned. The expression levels
of Gli-1 in the sections were detected using immunohistochemistry.
The results revealed that Gli-1 expression was higher in the rhShh
treatment group, but lower in the metformin treatment group when
compared with the control group (Fig.
4C). Similarly, a lower expression of Gli-1 was observed in the
sections from the mice administered combination treatment than in
those in the rhShh treatment group (Fig. 4C).
Metformin suppresses rhShh-induced breast
cancer cell migration and invasion
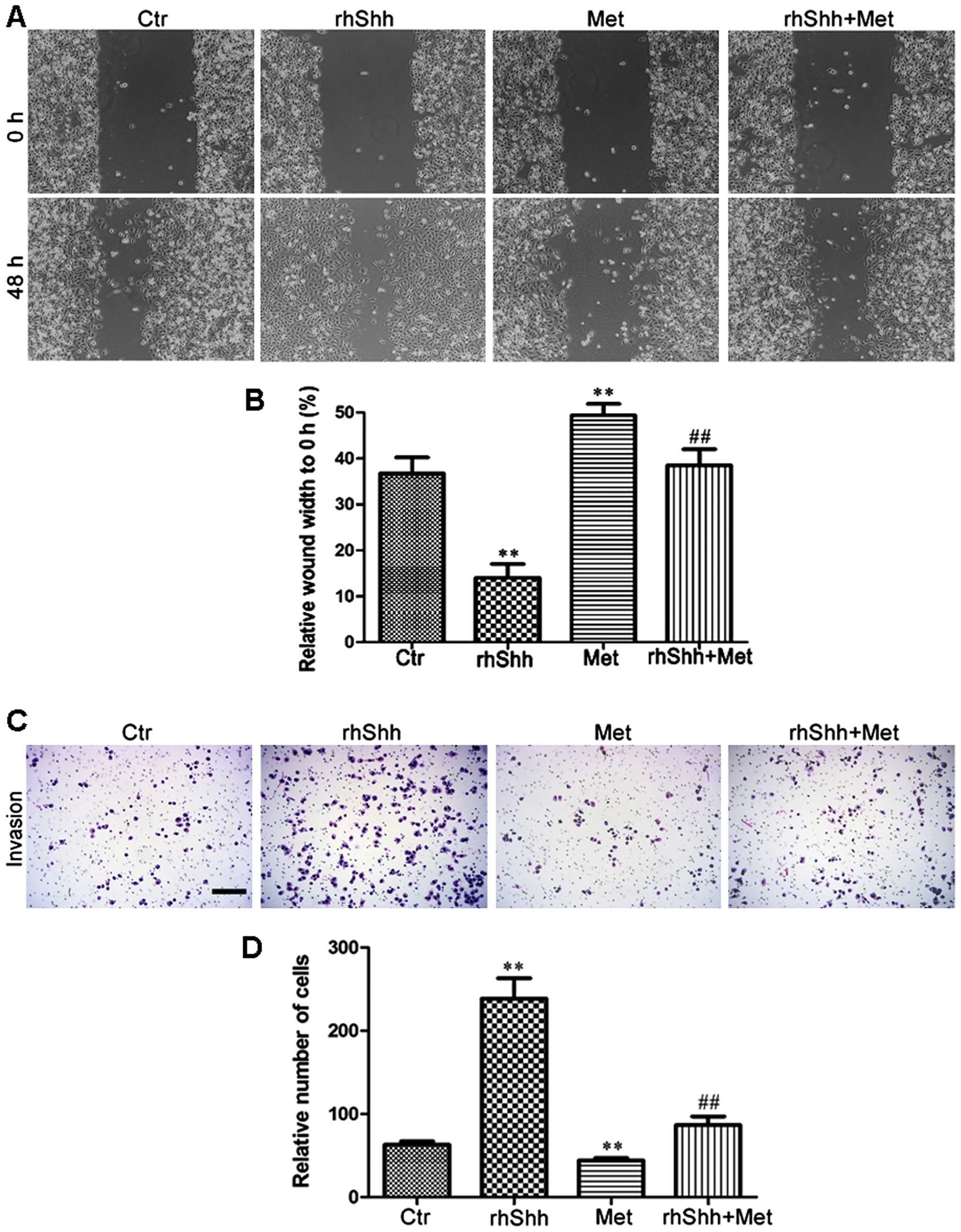
We then investigated the effects of metformin on the
migration potential of the MDA-MB-231 cells using the scratch-wound
assay (for cell migration). The cells were seeded in 6-well plates,
grown to confluence, and scratched using a 200-µl pipette
tip to create a wound. The cells were then incubated for 48 h in
the presence of rhShh (1 µg/ml), metformin (3 mM), or a
combination of both. Phase-contrast images were obtained at the 0-
and 48-h time points. When compared with the control group, the
rhShh-treated MDA-MB-231 cells displayed a higher rate of migration
(P<0.01), and the leading edges along the scraped area had
almost integrated at 48 h (Fig. 5A
and B). By contrast, treatment with metformin resulted in a
significant decrease in cellular migration compared with the
control group, and combination treatment with rhShh and metformin
led to a marked inhibition of the rhShh-induced wound gap closure
(P<0.01; Fig. 5A and B). A
Transwell invasion assay was also performed to analyze the effects
of treatment with rhShh (1 µg/ml), metformin (3 mM), or
their combination on the invasive capacity of the cells. The number
of rhShh-treated cells that had migrated across both the Matrigel
and the insert was 3-fold higher than that of the control group,
while the number of migratory metformin-treated cells was
approximately 70% that of the control group (P<0.01; Fig. 5C and D). The cells administered
the combined treatment showed a markedly reduced invasive capacity
compared with those treated with rhShh alone (Fig. 5C and D). These results suggest
that metformin impairs the effects of rhShh in promoting cell
invasion.
Metformin inhibits rhShh-induced CSC
stemness
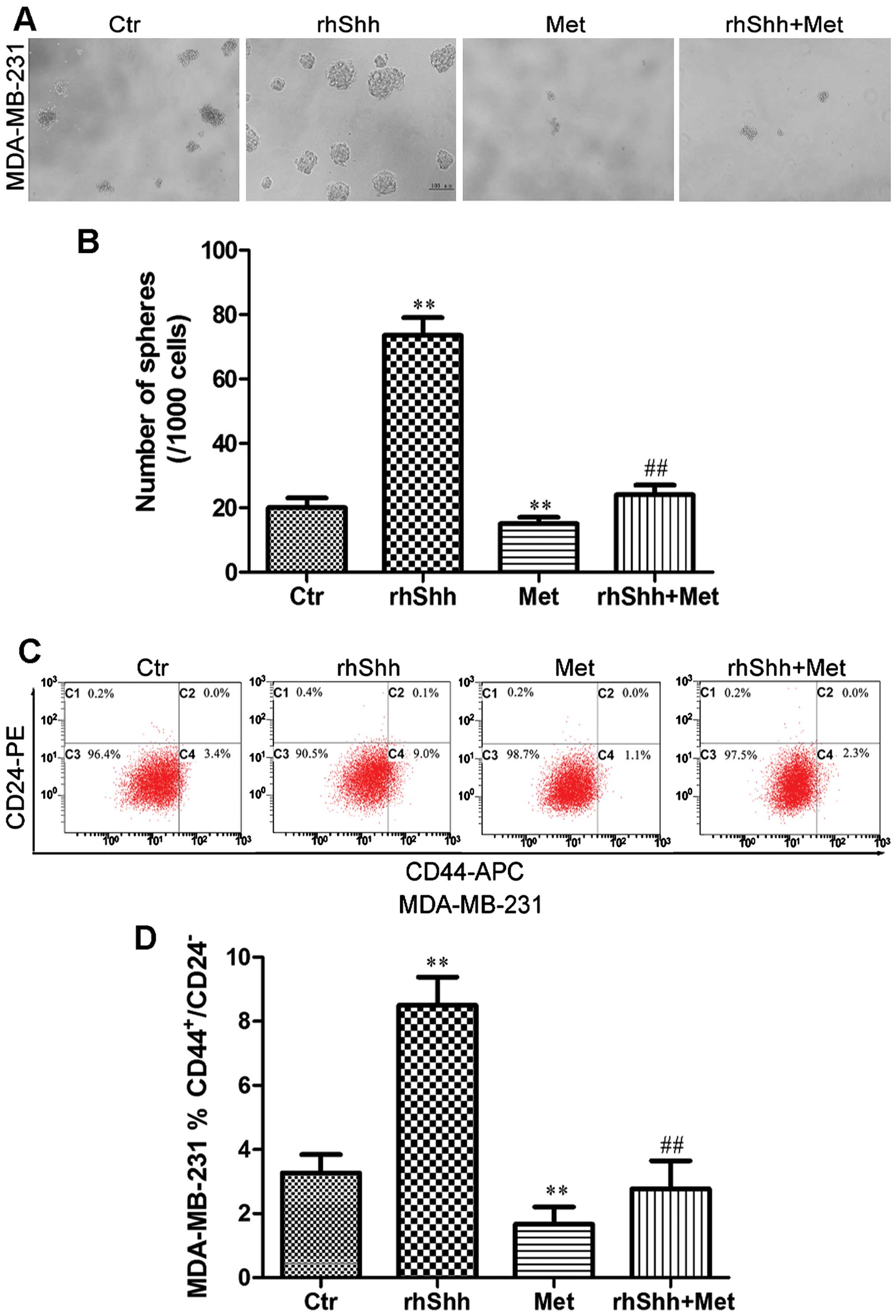
To determine whether metformin inhibits the stemness
of breast cancer cells through the suppression of the Shh signaling
pathway, the MDA-MB-231 cells were cultured at a very low density
(1 cell/µl) in 96-well plates containing serum-free medium
with rhShh (1 µg/ml) alone, metformin (3 mM) alone, or a
combination of both for 7 days. The cells treated with rhShh
produced a greater number of and larger spheres compared with
control cells (Fig. 6A and B).
Treatment with metformin significantly reduced the number and size
of these spheres compared with the control cells, and also
inhibited the rhShh-induced development of a greater number of and
larger spheres (P<0.01; Fig. 6A
and B).
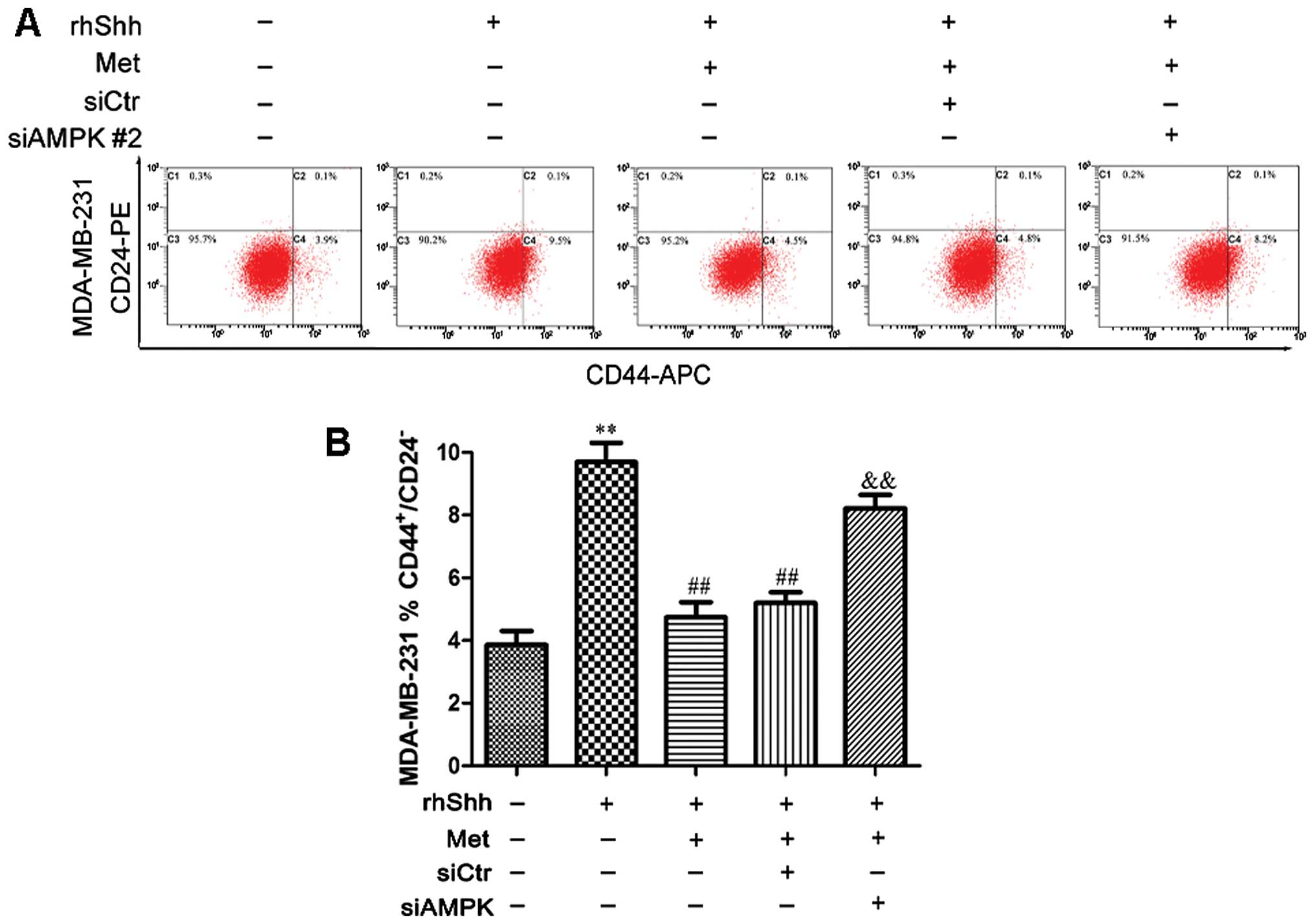
Subsequently, the MDA-MB-231 breast cancer cells
were incubated with rhShh (1 µg/ml), metformin (3 mM), or a
combination of both for 48 h. The population of
CD44+/CD24− cells was then measured using
flow cytometry. The cells which were exposed to rhShh had a higher
proportion of CD44+/CD24− cells compared to
the controls (from 3.4 to 9.0%; P<0.01; Fig. 6C and D). Treatment with metformin
induced a statistically significant decrease in the
CD44+/CD24− cell population, and combination
treatment led to a marked inhibition of the increase in the
proportion of CD44+/CD24− cells induced by
rhShh (P<0.01; Fig. 6C and
D).
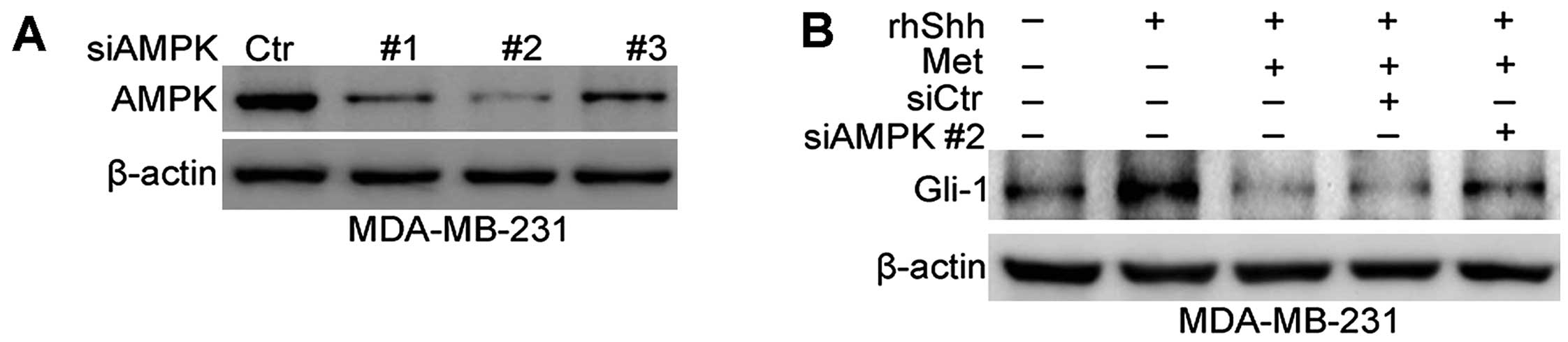
AMPK is involved in the inhibition of the
Shh signaling pathway by metformin
Previous studies have found that AMPK plays a
critical role in facilitating the anticancer effects of metformin
(9,10). Therefore, we then investigated
whether the metformin-mediated inhibition of the Shh signaling
pathway is dependent on AMPK. To inhibit AMPK expression, siRNA was
used. Fig. 7A shows that the 3
sequences of AMPK siRNA (siAMPK#1, siAMPK#2 and siAMPK#3)
effectively depleted AMPK expression at the protein level in the
transfected MDA-MB-231 cells compared with cells transfected with
siCtr. The sequence siAMPK#2-transfected cells were selected to
examine the role of AMPK in the metformin-mediated inhibition of
the Shh signaling pathway. Western blot analysis revealed a
significant increase in Gli-1 expression following the combined
treatment of MDA-MB-231 cells with rhShh and metformin, and
transfection with siAMPK#2 compared with the cells transfected with
siCtr or in the untransfected cells (Fig. 7B).
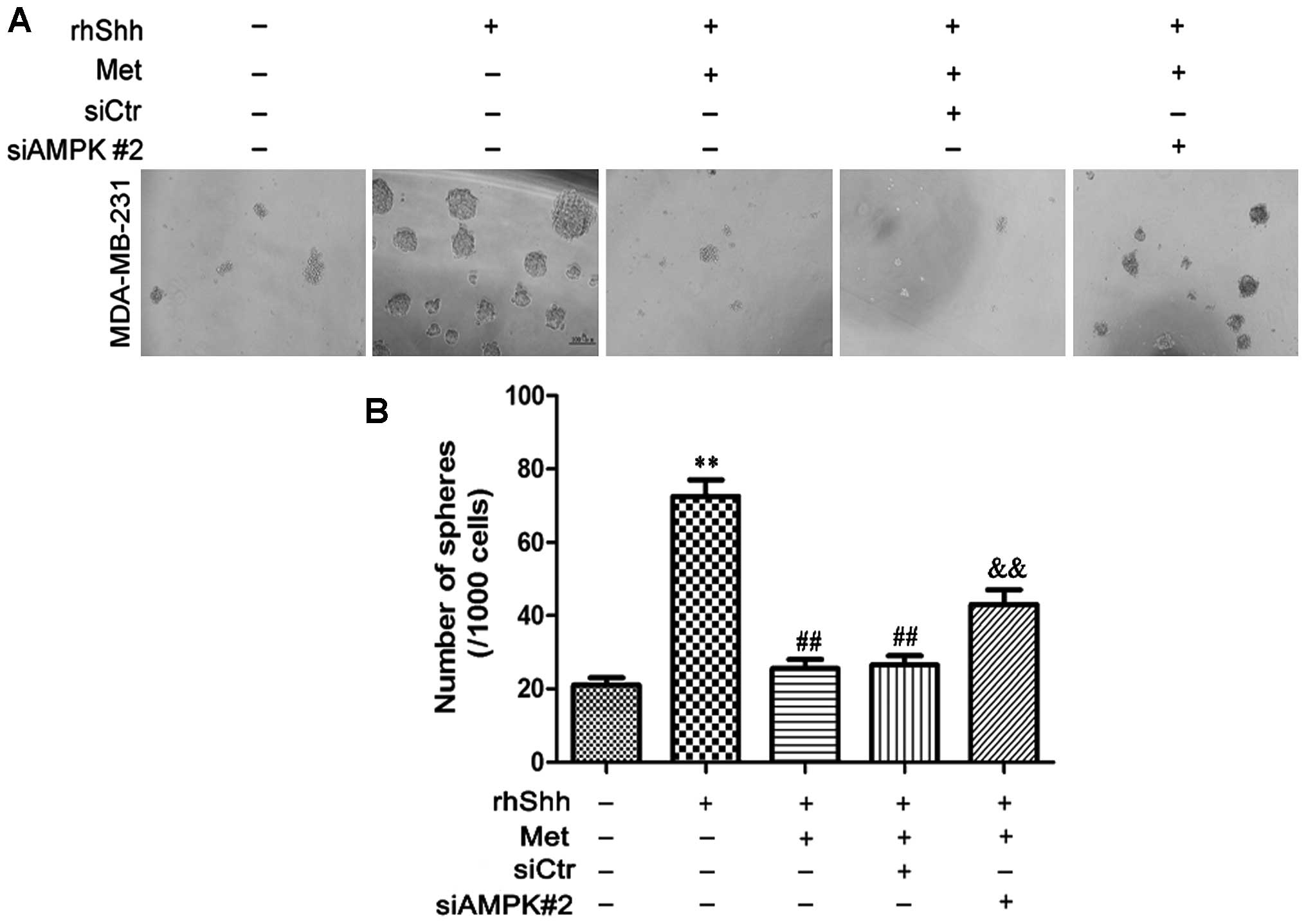
We subsequently determined whether AMPK is involved
in the metformin-mediated suppression of BCSC stemness through the
Shh signaling pathway. In the presence of rhShh and metformin, the
siAMPK#2-transfected cells produced a greater number of and larger
spheres compared with both the siCtr-transfected cells and the
untransfected cells (P<0.01; Fig.
8). In the presence of rhShh and metformin, the
siAMPK#2-transfected cells exhibited a significantly greater
proportion of CD44+/CD24− stem cell-like
cells compared with both the siCtr-transfected cells and
untransfected cells (P<0.01; Fig.
9). These results indicate that AMPK is involved in the
inhibition of the Shh pathway by metformin.
Discussion
The findings of the present study suggest that
metformin significantly inhibits the Shh signaling pathway. Most
importantly, our findings, to the best of our knowledge, for the
first time demonstrate that metformin exerts anticancer effects
through the inhibition of the Shh signaling pathway in breast
cancer. Metformin is a widely used and well-tolerated oral
antidiabetic agent used in the treatment of type 2 diabetes. A
previous study identified that the use of metformin in patients
with type 2 diabetes was associated with a lower risk of breast
cancer (32). Furthermore,
metformin has been found to inhibit the growth of breast cancer
(33) and selectively kill CSCs
(7,34). Our findings are in agreement with
those of previous studies (7,33)
showing that treatment with metformin significantly inhibits the
growth of breast cancer cells in both MTT and colony formation
assays. We further examined the effects of metformin on tumor
growth in vivo, and showed that the tumors exposed to
metformin were significantly smaller than the relevant control
tumors. Additionally, we demonstrated that treatment with metformin
inhibited breast cancer cell migration and invasion as well as CSC
survival and self-renewal.
Studies have demonstrated that the dysregulation of
the Shh signaling pathway contributes to the formation and
progression of human cancers, including breast cancer (18,35). Recently, Nakamura et al
(21) demonstrated that metformin
reduces the expression of Shh in pancreatic cancer cells,
suggesting that the suppression of Shh signaling is a possible
mechanism through which metformin mediates its anticancer effects.
We further extended this previous research to investigate the role
of the Shh signaling pathway in the anticancer effects of
metformin. In our analysis, a significant dose- and time-dependent
decrease in the expression levels of Shh, Smo, Ptc and Gli-1 was
observed in the breast cancer cells treated with metformin. In
order to examine the correlation between the anticancer effects of
metformin and its inhibitory effect on the Shh signaling pathway
more thoroughly, we treated the cells with rhShh (a specific
activator of the Shh signaling pathway). We observed that metformin
significantly impaired the rhShh-induced cell proliferation in
vitro and in vivo, and inhibited the migratory and
invasive capacity of the cells treated with rhShh. Metformin also
suppressed the increase in the proportion of
CD44+/CD24− cells and the development of a
greater number of and larger spheres induced by rhShh. These
findings support a central role for the inhibition of the Shh
signaling pathway in mediating the anticancer effects of metformin
in breast cancer.
Based on the aforementioned findings, we further
investigated whether the metformin-mediated inhibition of the Shh
signaling pathway is AMPK-dependent. The activation of AMPK was
identified as pivotal in enabling the anticancer effects of
metformin. Following the downregulation of AMPKα1 expression by
siRNA, the cells were treated with rhShh and metformin. A
significant increase in Gli-1 expression was observed in the cells
transfected with siRNA against AMPKα1 compared with the cells
transfected with the control siRNA or the untransfected cells. The
downregulation of AMPKα1 expression reversed the inhibitory effects
of metformin on rhShh-induced Gli-1 expression. AMPK was also shown
to be involved in the metformin-mediated suppression of BCSC
stemness through the Shh signaling pathway. This suggests that the
inhibition of the Shh signaling pathway mediated by metformin
occurred through an AMPK-dependent mechanism.
Although further research is required to clarify the
mechanisms underlying the anticancer effects of metformin, the
present study demonstrates that the inhibition of the Shh signaling
pathway is a significant contributing factor to the anticancer
effects of metformin in breast cancer. Additionally, we identified
that the metformin-mediated inhibition of the Shh signaling pathway
is dependent on AMPK.
In conclusion, to the best of our knowledge, the
present study is the first to identify that metformin exerts
anticancer effects through the inhibition of the Shh signaling
pathway in breast cancer. The downregulation of Shh signaling by
metformin inhibited the proliferation of cancer cells both in
vitro and in vivo, impaired cellular migration and
invasion, and reduced BCSC survival and self-renewal capacity.
Furthermore, the metformin-mediated inhibition of the Shh signaling
pathway was partially dependent on AMPK. However, further research
is required on the molecular mechanisms of the association between
the anticancer effects of metformin and the Shh signaling
pathway.
Acknowledgments
The present study was supported by the National
Natural Science Foundation of China (grant no. 30672434).
References
|
1
|
Alexander GC, Sehgal NL, Moloney RM and
Stafford RS: National trends in treatment of type 2 diabetes
mellitus, 1994–2007. Arch Intern Med. 168:2088–2094. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bosco JL, Antonsen S, Sørensen HT,
Pedersen L and Lash TL: Metformin and incident breast cancer among
diabetic women: A population-based case-control study in Denmark.
Cancer Epidemiol Biomarkers Prev. 20:101–111. 2011. View Article : Google Scholar
|
|
3
|
Kisfalvi K, Eibl G, Sinnett-Smith J and
Rozengurt E: Metformin disrupts crosstalk between G protein-coupled
receptor and insulin receptor signaling systems and inhibits
pancreatic cancer growth. Cancer Res. 69:6539–6545. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hosono K, Endo H, Takahashi H, Sugiyama M,
Sakai E, Uchiyama T, Suzuki K, Iida H, Sakamoto Y, Yoneda K, et al:
Metformin suppresses colorectal aberrant crypt foci in a short-term
clinical trial. Cancer Prev Res (Phila). 3:1077–1083. 2010.
View Article : Google Scholar
|
|
5
|
Azoulay L, Dell’Aniello S, Gagnon B,
Pollak M and Suissa S: Metformin and the incidence of prostate
cancer in patients with type 2 diabetes. Cancer Epidemiol
Biomarkers Prev. 20:337–344. 2011. View Article : Google Scholar
|
|
6
|
Ben Sahra I, Laurent K, Loubat A,
Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le
Marchand-Brustel Y and Bost F: The antidiabetic drug metformin
exerts an antitumoral effect in vitro and in vivo through a
decrease of cyclin D1 level. Oncogene. 27:3576–3586. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hirsch HA, Iliopoulos D, Tsichlis PN and
Struhl K: Metformin selectively targets cancer stem cells, and acts
together with chemotherapy to block tumor growth and prolong
remission. Cancer Res. 69:7507–7511. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Buzzai M, Jones RG, Amaravadi RK, Lum JJ,
DeBerardinis RJ, Zhao F, Viollet B and Thompson CB: Systemic
treatment with the antidiabetic drug metformin selectively impairs
p53-deficient tumor cell growth. Cancer Res. 67:6745–6752. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shackelford DB and Shaw RJ: The LKB1-AMPK
pathway: Metabolism and growth control in tumour suppression. Nat
Rev Cancer. 9:563–575. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zheng L, Yang W, Wu F, Wang C, Yu L, Tang
L, Qiu B, Li Y, Guo L, Wu M, et al: Prognostic significance of AMPK
activation and therapeutic effects of metformin in hepatocellular
carcinoma. Clin Cancer Res. 19:5372–5380. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kahn BB, Alquier T, Carling D and Hardie
DG: AMP-activated protein kinase: Ancient energy gauge provides
clues to modern understanding of metabolism. Cell Metab. 1:15–25.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rocha GZ, Dias MM, Ropelle ER,
Osório-Costa F, Rossato FA, Vercesi AE, Saad MJ and Carvalheira JB:
Metformin amplifies chemotherapy-induced AMPK activation and
antitumoral growth. Clin Cancer Res. 17:3993–4005. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dowling RJ, Zakikhani M, Fantus IG, Pollak
M and Sonenberg N: Metformin inhibits mammalian target of
rapamycin-dependent translation initiation in breast cancer cells.
Cancer Res. 67:10804–10812. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ingham PW and McMahon AP: Hedgehog
signaling in animal development: Paradigms and principles. Genes
Dev. 15:3059–3087. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Varjosalo M and Taipale J: Hedgehog:
Functions and mechanisms. Genes Dev. 22:2454–2472. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhu AJ, Zheng L, Suyama K and Scott MP:
Altered localization of Drosophila Smoothened protein activates
Hedgehog signal transduction. Genes Dev. 17:1240–1252. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Murone M, Rosenthal A and de Sauvage FJ:
Hedgehog signal transduction: From flies to vertebrates. Exp Cell
Res. 253:25–33. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kubo M, Nakamura M, Tasaki A, Yamanaka N,
Nakashima H, Nomura M, Kuroki S and Katano M: Hedgehog signaling
pathway is a new therapeutic target for patients with breast
cancer. Cancer Res. 64:6071–6074. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Onishi H and Katano M: Hedgehog signaling
pathway as a therapeutic target in various types of cancer. Cancer
Sci. 102:1756–1760. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jeng KS, Sheen IS, Jeng WJ, Yu MC, Hsiau
HI and Chang FY: High expression of Sonic Hedgehog signaling
pathway genes indicates a risk of recurrence of breast carcinoma.
Onco Targets Ther. 7:79–86. 2013. View Article : Google Scholar
|
|
21
|
Nakamura M, Ogo A, Yamura M, Yamaguchi Y
and Nakashima H: Metformin suppresses sonic hedgehog expression in
pancreatic cancer cells. Anticancer Res. 34:1765–1769.
2014.PubMed/NCBI
|
|
22
|
Visvader JE: Keeping abreast of the
mammary epithelial hierarchy and breast tumorigenesis. Genes Dev.
23:2563–2577. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dontu G, Abdallah WM, Foley JM, Jackson
KW, Clarke MF, Kawamura MJ and Wicha MS: In vitro propagation and
transcriptional profiling of human mammary stem/progenitor cells.
Genes Dev. 17:1253–1270. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bombonati A and Sgroi DC: The molecular
pathology of breast cancer progression. J Pathol. 223:307–317.
2011. View Article : Google Scholar :
|
|
25
|
Al-Hajj M, Wicha MS, Benito-Hernandez A,
Morrison SJ and Clarke MF: Prospective identification of
tumorigenic breast cancer cells. Proc Natl Acad Sci USA.
100:3983–3988. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
O’Brien CA, Kreso A and Jamieson CH:
Cancer stem cells and self-renewal. Clin Cancer Res. 16:3113–3120.
2010. View Article : Google Scholar
|
|
27
|
Ailles LE and Weissman IL: Cancer stem
cells in solid tumors. Curr Opin Biotechnol. 18:460–466. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kakarala M and Wicha MS: Implications of
the cancer stem-cell hypothesis for breast cancer prevention and
therapy. J Clin Oncol. 26:2813–2820. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gupta PB, Onder TT, Jiang G, Tao K,
Kuperwasser C, Weinberg RA and Lander ES: Identification of
selective inhibitors of cancer stem cells by high-throughput
screening. Cell. 138:645–659. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rattan R, Graham RP, Maguire JL, Giri S
and Shridhar V: Metformin suppresses ovarian cancer growth and
metastasis with enhancement of cisplatin cytotoxicity in vivo.
Neoplasia. 13:483–491. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Rattan R, Giri S, Hartmann LC and Shridhar
V: Metformin attenuates ovarian cancer cell growth in an AMP-kinase
dispensable manner. J Cell Mol Med. 15:166–178. 2011. View Article : Google Scholar
|
|
32
|
Bodmer M, Meier C, Krähenbühl S, Jick SS
and Meier CR: Long-term metformin use is associated with decreased
risk of breast cancer. Diabetes Care. 33:1304–1308. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zakikhani M, Dowling R, Fantus IG,
Sonenberg N and Pollak M: Metformin is an AMP kinase-dependent
growth inhibitor for breast cancer cells. Cancer Res.
66:10269–10273. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Janzer A, German NJ, Gonzalez-Herrera KN,
Asara JM, Haigis MC and Struhl K: Metformin and phenformin deplete
tricarboxylic acid cycle and glycolytic intermediates during cell
transformation and NTPs in cancer stem cells. Proc Natl Acad Sci
USA. 111:10574–10579. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ramaswamy B, Lu Y, Teng KY, Nuovo G, Li X,
Shapiro CL and Majumder S: Hedgehog signaling is a novel
therapeutic target in tamoxifen-resistant breast cancer aberrantly
activated by PI3K/AKT pathway. Cancer Res. 72:5048–5059. 2012.
View Article : Google Scholar : PubMed/NCBI
|