Introduction
Congenital heart defects (CHDs) are among the most
common malformations in live-born infants. Complicated structural
and functional cardiovascular fetal malformations have high rates
of mortality and morbidity, and may result in fetal, neonatal or
adolescent fatality, stillbirth, preterm labor or disability.
Studies in the USA and China have reported that the prevalence of
CHD is 4–8 in every 1,000 live births (1–3).
This may be as high as 19–74 in every 1,000 live births when
particular minor malformations are included, such as bicuspid
aortic valves (4,5). The number of reported cases of CHD in
China is 1.98–13.8 per 1,000 live births (6) and in large areas of China, CHDs are
the most common birth defects (7).
However, these results have been obtained from epidemiological
studies within small areas and this area of investigation lacks
systematic nation-wide epidemiological research.
CHDs occur due to a number of factors; 90% of CHDs
result from multifactorial disorders, 8% from single gene disorders
and 2% from environmental teratogens (8). The current predominant method of
correcting CHD is through cardiac surgery. The development of
techniques and equipment has enabled doctors to execute more
complicated heart operations and surgery is performed earlier;
where as it used to be conducted in childhood, it is now carried
out at the neonatal and even the prenatal stage. Early diagnosis
allows surgeons to pay close attention to the classification and
severity of the cardiac malformations and to plan treatment
accordingly. Notably, 20–45% children with CHDs also present with
extracardiac defects (9,10), which may be caused by genetic
factors (11–13). CHDs are commonly observed in
fetuses or neonates with chromosomal abnormalities, such as trisomy
21, trisomy 18, trisomy 13, chromosome 4P− syndrome,
Cri-du-chat syndrome and DiGeorge syndrome.
22q11 microdeletion syndrome may present as DiGeorge
syndrome or velocardiofacial syndrome (also termed conotruncal
anomaly face syndrome), and the prevalence is ~1 in 4,000–6,000
live births (14,15). The syndrome is caused by a
microdeletion on chromosome 22 at the q11.2 band. The majority of
affected individuals have an identical 3 megabase deletion, which
encompasses a region containing 30–40 genes. 22q11 microdeletion is
commonly accompanied by CHD (75–100% cases), immunodeficiency (~80%
cases), neonatal hypocalcemia (49–60% cases), palate anomalies (81%
cases, in particular, submucous cleft palate), renal and skeletal
anomalies, feeding disorders, growth retardation, speech and
language disabilities, and behavioral and psychiatric disorders
(14,16–18).
As heart surgery may not improve the prognosis of
CHD fetuses with additional problems, it is important to evaluate
the requirement for cardiac surgery taking into account the results
of genetic screening, and to explore other options, such as
termination. Accurate and prompt genetic diagnosis of a fetus with
CHDs may aid parents in making such a decision. In the majority of
countries, chromosome analysis and 22q11 microdeletion detection
are commonly investigated in children or adolescents, but are not
routinely used on fetuses with CHDs, therefore chromosomal
abnormalities may not be detected. A study by Zyblewski et
al (19) found that, compared
with the severity of the heart defect, the influence of fetal
chromosomal abnormality was more significant on the parental
decision to terminate the pregnancy or provide special postnatal
nursing (20). In China,
>50,000 CHD surgeries are performed annually (21). Among these, ~50% of operations are
conducted on infants aged 1–2 years. Cardiac surgery is currently
following a trend towards operating on younger patients, thus the
proportion of surgical procedures performed on newborns is
increasing. Appropriate genetic tests are hypothesized to become an
important method of diagnosis and vital in evaluating fetal
prognosis.
The etiology of CHD may correspond to the area of
residence and ethnicity of the patient due to the multiple factors
involved in development of the disease. Beijing Obstetrics and
Gynecology Hospital (Beijing, China) is the biggest specialist
hospital in Obstetrics and Gynecology in the North of China and
thus may provide important information regarding the detection of
CHD in a large area. The aim of the present study was to analyze
chromosomal abnormalities and 22q11 microdeletions in fetuses with
CHD, in order to evaluate fetal prognosis, and to inform the
parents and the cardiac surgeons of the result.
Materials and methods
Study group
The study was conducted between January 2010 and
December 2011. Subsequent to obtaining written informed consent,
all 113 pregnant females with fetuses with heart malformations
detected by routine prenatal diagnostic ultrasound screening that
consented to further investigation were enrolled in the study group
in the Beijing Obstetrics and Gynecology Hospital (Beijing, China);
there were no exclusions. Fetal samples were collected from either
amniotic fluid or umbilical cord blood according to gestational
age: Amniotic fluid cells were collected from patients with
gestational age 16–23 weeks and cord blood cells were collected
from patients with gestational age 24–35 weeks. G-banding
chromosome karyotyping was performed. The 101 cases with apparently
normal chromosomes were then further investigated for the 22q11
microdeletion following the obtention of written informed consent a
second time. The parents of the 22q11 microdeletion-positive
fetuses were then investigated themselves for the same
microdeletion. The study was approved by the Beijing Obstetrics and
Gynecology Hospital Medical Ethics Committee of Capital Medical
University (Approval ID: Ky200912).
Echocardiographic methods
The cardiac defects of all 113 fetuses were
diagnosed by certified ultrasound specialists in the prenatal
diagnostic center using ultrasound equipment (Philips iU22, GE V730
and Voluson E8; Philips, Amsterdam, The Netherlands). The
cardiovascular malformations were screened by a two-dimensional
color Doppler appliance (Philips iU22, Amsterdam, The Netherlands)
and then confirmed by fetal echocardiography (GE V730, GE,
Fairfield, CT, USA). The types of CHD detected were grouped
according to ‘Fetal heart screening guidelines’ (22). Real-time examination included
four-chamber, left- and right- heart, long-axis, short-axis, aortic
arch and arterial duct views. The different types of cardiac
abnormalities were recorded.
Cytogenetic methods
Following genetic consultation and informed consent,
amniotic fluid cells were collected from the 48 cases with a
gestational age of 16–23 weeks. In addition, cord blood cells were
collected from the remaining 65 cases with a gestational age of
24–35 weeks. Chromosomal analysis was conducted using standard
methods, including cell culturing, harvesting and histology
(23). G-banded metaphase
chromosomes were screened at 500–550-band level. The chromosomes
were analyzed and karyotyped according to the International System
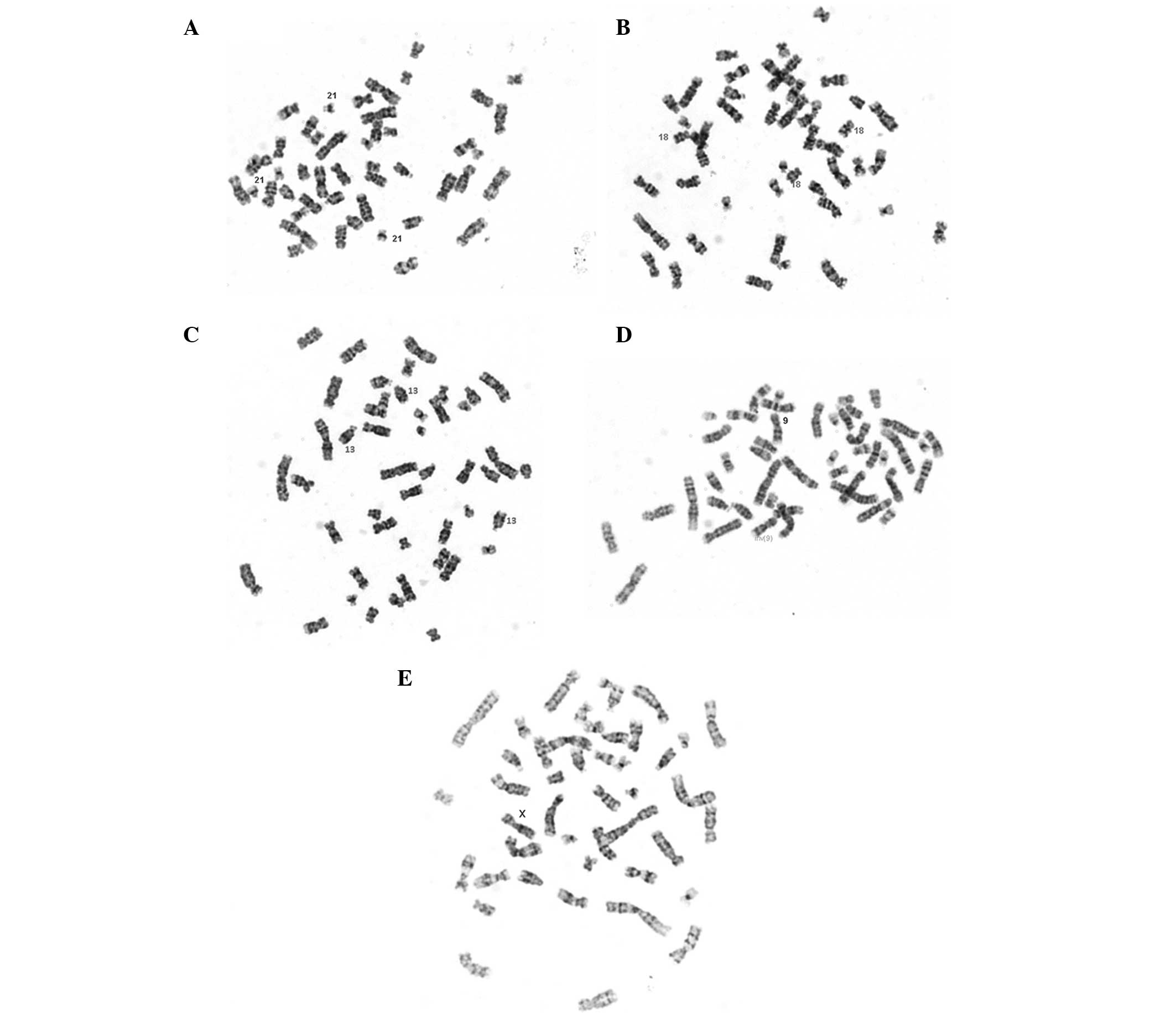
for Human Cytogenetic Nomenclature (ISCN 1995; Fig. 1) and the results were recorded.
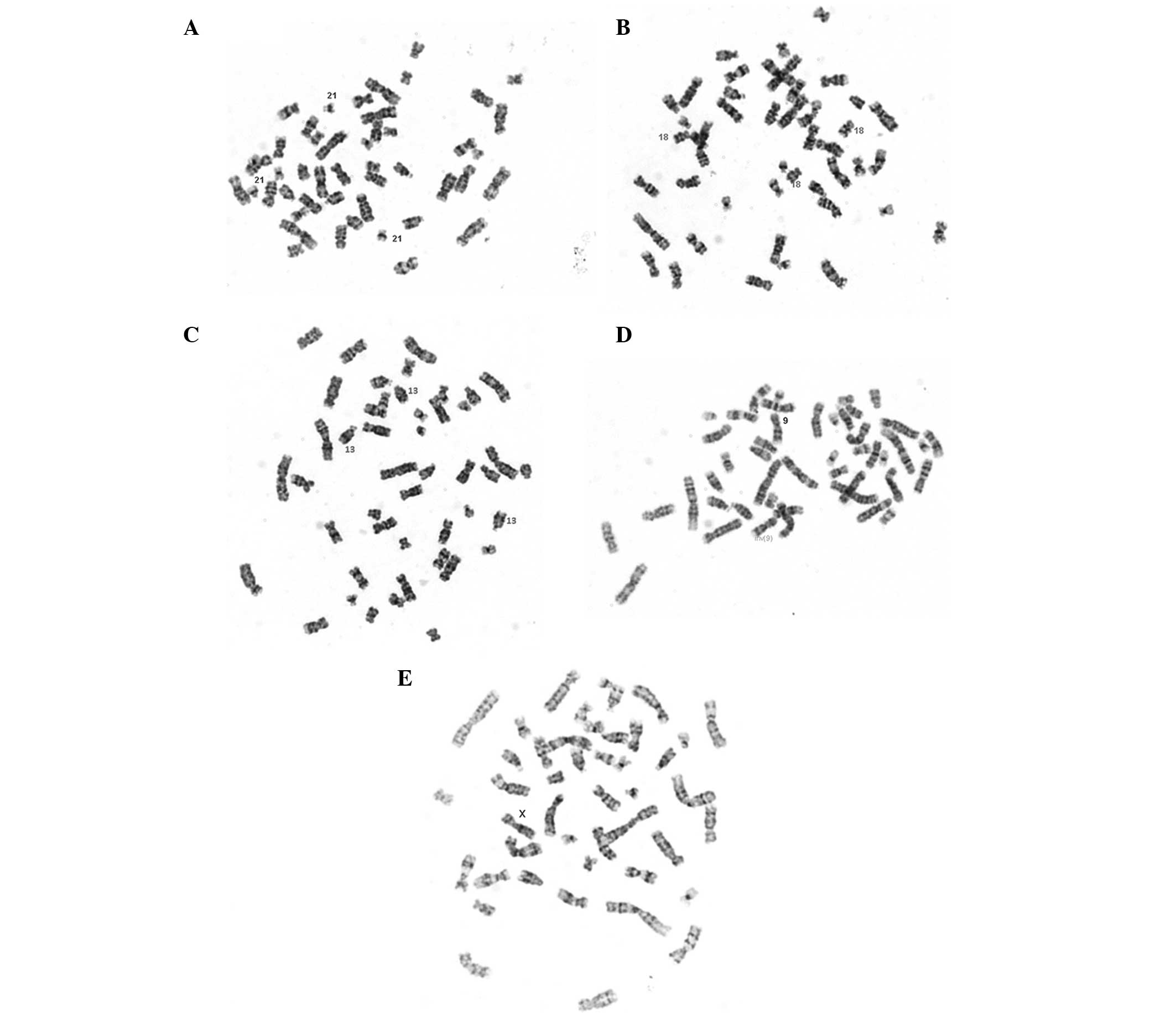 | Figure 1Examples of karyotyping. (A) Trisomy
21 karyotyping (original magnification, ×1,000). (B) Trisomy 18
karyotyping (original magnification, ×1,000). (C) Trisomy 13
karyotyping (original magnification, ×1,000). (D) Inversion 9
karyotyping (original magnification, ×1,000). (E) 45, X karyotyping
(original magnification, ×1,000). |
Fluorescence in situ hybridization (FISH)
methods
FISH analysis of samples collected from the 101
pregnant females whose fetus had normal chromosomes and the 12
parents whose fetus exhibited the 22q11 microdeletion was
performed. The analysis was performed on metaphase chromosome
spreads using a domestically manufactured probe (Beijing Jinpujia
Medical Technology Co., Ltd., Beijing, China), which maps to the
TUPLE1 region (22q11.2, spectrum red), combined with the ARSA
region (22q11.3, spectrum green) as a control probe (24,25).
FISH analysis was conducted as follows: Following
extraction, 5–10 ml amniotic fluid sample was centrifuged at 900 ×
g for 8 min, and the supernatant was removed and discarded. The
pelleted cells were incubated in 5 ml hypotonic 0.075 mol/l KCl
solution at 37°C for 12 min and then 2 ml Carnoy’s fixative
(methanol:acetic acid=3:1) was added. The cells were then pelleted
by centrifugation at 250 × g for 10 minutes, and fixed twice for 8
min with Carnoy’s fixative at room temperature. Fresh Carnoy’s
fixative was added to adjust the final volume to provide an optimal
cell concentration for cell spreading and mixing when the cell
suspension was dripped onto a microscope slide. For hybridization,
the prepared slides were rinsed twice with 2X saline-sodium citrate
(SSC; pH 7.0) for 5 min at room temperature, treated with 0.1 mol/l
HCl for 5 min, then incubated with pepsin in 0.01 mol/l HCl at 37°C
for 12 min. The slides were rinsed again with 2X SSC for 5 min at
room temperature, then dehydrated with a series of ethanol
dilutions at 70, 85 and 100% in sequence, air-dried and heated to
56°C prior to hybridization. The probe mixture (containing 2 ml
probe, 7 ml hybridizing buffer and 1 ml deionized water), was
denatured at 76°C for 5 min. The slides were denatured separately
in 70% formamide/2X SSC at 76°C for 5 min and then dehydrated with
−20°C precooled ethanol at 70, 85 and 100% in sequence and
air-dried. The denatured probe mixture was dropped onto the cell
smear on each prepared slide, covered with a cover slip and sealed
with sealing glue. The hybridization was performed in a wet chamber
at 42°C overnight. On the second day, with the cover slip removed,
subsequent to washing three times with 50% formamide/2X SSC at 46°C
for 10 min, 2X SSC for 10 min and 2X SSC/0.1% NP-40 for 5 min, the
air-dried slides were restained with 15 μl
4′,6-diamidino-2-phenylindole dihydrochloride for 10–20 min prior
to analysis.
The slides were observed with a fluorescence
microscope (Olympus BX51; Olympus, Tokyo, Japan); the filters used
were MBE44720, MBE45600 and MBE41300. For each specimen, at least
50 nuclei were evaluated. If 90% cells detected were normal, the
specimen was classified as normal (Fig. 2A). If 60% cells were abnormal, the
specimen was diagnosed as affected (Fig. 2B). In cases where there was any
doubt, the number of cells evaluated increased to 100 cells and
results were reported as uninformative if the above criteria were
not met.
Statistical analysis
The data are presented as the mean ± standard
deviation for continuous variables. Differences in categorical
variables were measured using the χ2 test. Analyses were
performed with SPSS 17.0 (SPSS, Inc., Chicago, IL, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
Clinical characteristics of the study
group
A total of 113 fetuses with major structural CHD
were identified at 16 to 35 (25.12±4.37) weeks gestation. The age
of the pregnant females ranged between 20 and 47 years (mean,
30.73±4.59). A total of 98 of the pregnant females (86.7%) were
primipara and the remaining 15 pregnant females were pluripara
(13.3%). A total of 67 fetuses were identified as male and 42
female, while the genders of the remaining 4 were unknown, since
terminations of the pregnancies occurred at an early gestational
stage. The basic clinical data are listed in Table I.
 | Table IClinical data for 113 pregnant females
carrying fetuses with CHD. |
Table I
Clinical data for 113 pregnant females
carrying fetuses with CHD.
| Factor | Parameter |
|---|
| Age, mean±SD
(range) | 30.73±4.59
(20–47) |
| Gestational weeks,
mean±SD (range) | 25.12±4.37
(16–35) |
| Parity, n (%) |
| Primipara | 98 (86.7) |
| Pluripara | 15 (13.3) |
| Gender of fetus, n
(%) |
| Male | 67 (59.3) |
| Female | 42 (37.2) |
| Unknown | 4 (3.5) |
Ultrasound characteristics of study
group
The classification of CHDs is determined by the
International Paediatric and Congenital Cardiac Code. This divides
all types of CHD into 10 categories and 23 subcategories according
to a multi-dimensional approach encompassing anatomic, diagnostic
and therapeutic criteria (26). Of
the fetuses with non-cyanotic cardiac defects, 47 cases (41.6% of
the whole group) of ventricular septal defects (VSD) were
identified, followed by 11 cases (9.7%) with atrial septal defects
(ASD), seven cases (6.2%) with pulmonary stenosis, four cases
(3.5%) with pulmonary valve stenosis, two cases with aortic
stenosis, two cases with aortic valve stenosis, three cases with
tricuspid valve dysplasia, two cases with aortic widening, two
cases with major blood vessel abnormality and one case with
acleistocardia.
Of the fetuses with cyanotic cardiac defects, 17
cases (15.0%) with tetralogy of Fallot (TOF) were detected,
followed by 10 cases (8%) with endocardial cushion defects, five
cases (4.4%) with transposition of the great arteries, four cases
(3.5%) with a uniatrial heart, four cases (3.5%) with a
univentricular heart, four cases (3.5%) with hypoplastic left heart
syndrome, three cases with truncus arteriosus, two cases with a
double outlet right ventricle and two cases with hypoplastic right
heart syndrome. The types and numbers of CHDs are listed in
Table II.
 | Table IIClassification of CHDs in 113
fetuses. |
Table II
Classification of CHDs in 113
fetuses.
| Types of CHD | n | % |
|---|
| Non-cyanotic |
| Ventricular septal
defect | 47 | 41.6 |
| Atrial septal
defect | 11 | 9.7 |
| Pulmonary
stenosis | 7 | 6.2 |
| Pulmonary valve
stenosis | 4 | 3.5 |
| Aortic stenosis | 2 | 1.8 |
| Aortic valve
stenosis | 2 | 1.8 |
| Tricuspid valve
dysplasia | 3 | 2.7 |
| Aortic widened | 2 | 1.8 |
| Major blood vessel
abnormality | 2 | 1.8 |
| Acleistocardia | 1 | 0.9 |
| Cyanotic |
| Tetralogy of
Fallot | 17 | 15.0 |
| Endocardial cushion
defect | 10 | 8.0 |
| Transposition of the
great arteries | 5 | 4.4 |
| Uniatrial heart | 4 | 3.5 |
| Univentricular
heart | 4 | 3.5 |
| Hypoplastic left
heart syndrome | 4 | 3.5 |
| Truncus
arteriosus | 3 | 2.7 |
| Double outlet right
ventricle | 2 | 1.8 |
| Hypoplastic right
heart syndrome | 2 | 1.8 |
| Total number of
fetuses affected | 113 | |
CHD type and chromosomal abnormalities in
the study group
The associations among CHD type, the incidence of
chromosomal abnormalities and the 22q11 microdeletion are shown in
Table III. Twelve patients
(10.6%) had chromosomal abnormalities and 6 patients (5.3%)
exhibited the classic 22q11 microdeletion.
 | Table IIIChromosome analysis and 22q11
microdeletion results of each cardiac defect. |
Table III
Chromosome analysis and 22q11
microdeletion results of each cardiac defect.
| Chromosomal
abnormality | |
|---|
|
| |
|---|
| Type of CHD | Type | n | 22q11 microdeletion
(n) |
|---|
| VSD | Trisomy 21 | 2 | 2 |
| Trisomy 18 | 4 | |
| Trisomy 13 | 1 | |
| Inv (9) | 1 | |
| 45, X | 1 | |
| PS | Trisomy 21 | 1 | |
| AW | Trisomy 21 | 1 | 1 |
| TOF | Trisomy 18 | 1 | 2 |
| ECD | Trisomy 21 | 1 | 1 |
| DORV | | | 1 |
| TGA | | | 1 |
| UA | | | 2 |
| UV | | | 2 |
| Total number of
fetuses affected | 12 (10.6%) | | 6 (5.3%) |
Table IV reveals
the number of the CHD cases that presented with extracardiac
abnormalities. The incidence of chromosomal abnormalities was
significantly higher in the CHD with extracardiac abnormalities
group, than in the CHD without extracardiac abnormalities group
(P<0.001); however, the difference in the incidence of the 22q11
microdeletion was not significant between these two groups
(P=0.583). The parents of the six fetuses with the 22q11
microdeletion did not present with the same microdeletion.
 | Table IVGenetic testing of fetuses with CHD
for extracardiac abnormalities. |
Table IV
Genetic testing of fetuses with CHD
for extracardiac abnormalities.
| Extracardiac
abnormalities | Cases (n) (% of
group) | Chromosomal
abnormalities (n) (% of group) | 22q11 microdeletion
(n) (% of group) |
|---|
| With | 15 (13.2) | 8 (53.3) | 1 (6.7) |
| Without | 98 (86.8) | 4 (4.1) | 5 (5.1) |
| Total | 113 (100) | 12 (10.6) | 6 (5.3) |
| P value | | <0.001 | 0.583 |
Discussion
The present study was conducted in order to
investigate chromosomal abnormalities and the 22q11 microdeletion
in CHD fetuses in a Chinese population. The genetic results
revealed 12 patients (10.6%) had chromosomal abnormalities and 6
patients (5.3%) exhibited the classic 22q11 microdeletion.
Altogether, ~1 in 6 (18/113) of the CHD cases may be explained by
genetic factors. Therefore, genetic factors are likely to be
important in CHD etiology.
In total, of the 15 CHD cases exhibiting
extracardiac anomalies, eight (53.3%) had chromosomal
abnormalities, while among the remaining 98 CHD cases without
extracardiac defects, only four (4.1%) exhibited chromosomal
abnormalities (P<0.001), suggesting that CHD fetuses with
extracardiac defects are more likely to have chromosomal
abnormalities than those fetuses with cardiac defects only. Of the
113 CHD cases, six (5.3%) were identified to have the 22q11
microdeletion. Among the 15 CHD cases with extracardiac defects,
only one (6.7%) was found to have the 22q11 microdeletion, while in
the remaining 98 cases without extracardiac defects, five (5.1%)
exhibited the 22q11 microdeletion; the difference between the two
groups was not significant (P=0.583). This finding is consistent
with the results of studies conducted by Hartman et al
(27) and Lammer et al
(28), but contradicts those of
studies by Fokstuen et al (29) and Borgmann et al (30), who observed that all cases of CHD
caused by the 22q11 microdeletion presented with extracardiac
defects. However, these authors analyzed unwell infants with CHD,
whose extracardiac anomalies were comparatively easy to diagnose;
the present study focused on fetuses in the second and third
trimesters. Considering the difficulty in ultrasound diagnosis of
typical fetal structural malformations, including palate anomalies
(particularly submucous cleft palates), renal anomalies and
skeletal anomalies, it is difficult to detect all abnormalities
during routine ultrasound screening. Song et al (31) demonstrated that as many as 46.4% of
fetal abnormalities are not identified prior to birth. The present
study is also not in accordance with the study by Bellucco et
al (32), who failed to detect
any 22q11.2 deletions. This may be associated with the smaller
sample size in that study and ethnic differences in the study
populations.
Isolated heart defects, such as ASD, VSD and TOF,
are rectified quite well by surgery following birth, with good
prognosis. However, an infirm infant with genetic abnormalities
commonly presents with a complicated clinical syndrome, with
intelligence defects, immunodeficiency and endocrinology
abnormalities, as well as behavioral and psychiatric disorders, and
the prognosis may not be markedly improved by cardiac surgery
alone. In the present study, among 47 fetuses with VSDs, 11 (23.4%)
exhibited genetic abnormalities, while in 17 fetuses with TOF,
three (17.6%) had genetic abnormalities. Thus, CHDs accompanied by
extracardiac defects should become an indicator of the requirement
for chromosome analysis, while fetuses with cardiac defects alone
should be an indicator for investigating for the presence of the
22q11 microdeletion during pregnancy. With this extra information,
parents are fully informed and consulted as to whether the fetuses
will undergo surgery, particularly intrauterine operations; and can
make an informed decision regarding termination.
In the present study, the 12 parents of the six
fetuses (5.3%) with the 22q11 microdeletion exhibited negative
results for the same microdeletion, suggesting that these six cases
occurred de novo; this is concurrent with previous reports
demonstrating that ~90% microdeletion cases occurred de
novo, with no known family history (14). Therefore, routine screening of the
parents is not required to detect fetuses that may have this
microdeleiton. In the future, the use of novel technology (e.g.
chromosomal microarray) may allow more sensitive detection of
abnormalities and thus may increase the identified contribution of
chromosomal abnormalities further.
The sample size in the present study was relatively
small, thus, further studies are required to determine the exact
frequency of chromosomal abnormalities and microdeletions, since
the etiology of cardiac defects may vary in different ethnic
groups.
In conclusion, CHD is currently the most common
birth defect in numerous areas of the world, including China, and
genetic factors are important in the etiology. As such
abnormalities are not rectified without surgery, it is essential to
identify the genetic factors involved, including chromosomal
abnormalities and the 22q11 microdeletion, a process essential in
determining fetal prognosis. These tests provide information
allowing appropriate prenatal consultation and assessment of the
recurrent risk.
References
|
1
|
Goldmuntz E: The epidemiology and genetics
of congenital heart disease. Clin Perinatol. 28:1–10. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
American Heart Association. FACTS Small
Hearts - Big Challenges Congenital Heart Defects (CHD) in Children,
Youth and Adults. http://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_304875.pdf.
Accessed March 18, 2013
|
|
3
|
Yang XY, Li XF, Lü XD and Liu YL:
Incidence of congenital heart disease in Beijing, China. Chin Med J
(Engl). 122:1128–1132. 2009.PubMed/NCBI
|
|
4
|
Hoffman JI and Kaplan S: The incidence of
congenital heart disease. J Am Coll Cardiol. 39:1890–1900. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gill HK, Splitt M, Sharland GK and Simpson
JM: Patterns of recurrence of congenital heart disease: an analysis
of 6,640 consecutive pregnancies evaluated by detailed fetal
echocardiography. J Am Coll Cardiol. 42:923–929. 2003. View Article : Google Scholar
|
|
6
|
Li S, Hong SX and Zhao P: The prevalence
of congenital heart defect in small infants of four cities
including Shijiazhuang. Chinese Journal of Pediatrics. 6:375–377.
1999.(In Chinese).
|
|
7
|
Zhu H, Kartiko S and Finnell RH:
Importance of gene-environment interactions in the etiology of
selected birth defects. Clin Genet. 75:409–423. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Payne RM, Johnson MC, Grant JW and Strauss
AW: Toward a molecular understanding of congenital heart disease.
Circulation. 91:494–504. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Noonan J: Associated noncardiac
malformations in children with congenital heart disease. J Pediatr.
63:468–470. 1963.
|
|
10
|
Greenwood RD, Rosenthal A, Parisi L, Fyler
DC and Nadas AS: Extracardiac abnormalities in infants with
congenital heart disease. Pediatrics. 55:485–492. 1975.PubMed/NCBI
|
|
11
|
Pierpont ME, Basson CT, Benson DW Jr, et
al: American Heart Association Congenital Cardiac Defects
Committee; Council on Cardiovascular Disease in the Young: Genetic
basis for congenital heart defects: current knowledge: a scientific
statement from the American Heart Association Congenital Cardiac
Defects Committee, Council on Cardiovascular Disease in the Young:
endorsed by the American Academy of Pediatrics. Circulation.
115:3015–3038. 2007.
|
|
12
|
Chaoui R, Körner H, Bommer C, et al:
Prenatal diagnosis of heart defects and associated chromosomal
aberrations. Ultraschall Med. 20:177–184. 1999.(In German).
|
|
13
|
Paladini D, Russo M, Teodoro A, et al:
Prenatal diagnosis of congenital heart disease in the Naples area
during the years 1994–1999 - the experience of a joint
fetal-pediatric cardiology unit. Prenat Diagn. 22:545–552.
2002.PubMed/NCBI
|
|
14
|
Botto LD, May K, Fernhoff PM, et al: A
population-based study of the 22q11.2 deletion: phenotype,
incidence, and contribution to major birth defects in the
population. Pediatrics. 112:101–107. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Manji S, Roberson JR, Wiktor A, et al:
Prenatal diagnosis of 22q11.2 deletion when ultrasound examination
reveals a heart defect. Genet Med. 3:65–66. 2001. View Article : Google Scholar
|
|
16
|
Goldmuntz E: DiGeorge syndrome: new
insights. Clin Perinatol. 32:963–978. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moore JW, Binder GA and Berry R: Prenatal
diagnosis of aneuploidy and deletion 22q11.2 in fetuses with
ultrasound detection of cardiac defects. Am J Obstet Gynecol.
191:2068–2073. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tan KB, Chew SK and Yeo GS: 22q11.2
deletion syndrome in Singapore (2000–2003): a case for active
ascertainment. Singapore Med J. 49:286–289. 2008.PubMed/NCBI
|
|
19
|
Zyblewski SC, Hill EG, Shirali G, et al:
Chromosomal anomalies influence parental treatment decisions in
relation to prenatally diagnosed congenital heart disease. Pediatr
Cardiol. 30:1105–1111. 2009. View Article : Google Scholar
|
|
20
|
Soares G, Alvares S, Rocha C, et al:
Congenital heart defects and chromosomal anomalies including 22q11
microdeletion (CATCH 22). Rev Port Cardiol. 24:349–371.
2005.PubMed/NCBI
|
|
21
|
Tang CZ, Zhao H, Gao WG and Hu D: The
status of surgical therapy in Congenital heart defect in China.
Chin J Evid Based Cardiovasc Med. 1:70–71. 2009.(In Chinese).
|
|
22
|
International Society of Ultrasound in
Obstetrics and Gynecology. Cardiac screening examination of the
fetus: guidelines for performing the ‘basic’ and ‘extended basic’
cardiac scan. Ultrasound Obstet Gynecol. 27:107–113. 2006.
|
|
23
|
Robers E and Warburton S: Laboratory
techniques. Genetics in Practice: A Clinical Approach for
Healthcare Practitioners. Haydon J: Wiley-Blackwell; Hoboken, NJ:
pp. 49–53. 2007, View Article : Google Scholar
|
|
24
|
Jia CW, Wang SY, Ma YM, et al:
Fluorescence in situ hybridization in uncultured amniocytes for
detection of aneuploidy in 4210 prenatal cases. Chin Med J (Engl).
124:1164–1168. 2011.PubMed/NCBI
|
|
25
|
Liu T, Liu Q, Wang YX, et al: Use of
amniocytes for prenatal diagnosis of 22q11.2 microdeletion
syndrome: a feasibility study. Chin Med J (Engl). 123:438–442.
2010.PubMed/NCBI
|
|
26
|
Houyel L, Khoshnood B, Anderson RH, et al:
Population-based evaluation of a suggested anatomic and clinical
classification of congenital heart defects based on the
International Paediatric and Congenital Cardiac Code. Orphanet J
Rare Dis. 6:642011. View Article : Google Scholar
|
|
27
|
Hartman RJ, Rasmussen SA, Botto LD, et al:
The contribution of chromosomal abnormalities to congenital heart
defects: a population-based study. Pediatr Cardiol. 32:1147–1157.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lammer EJ, Chak JS, Iovannisci DM, et al:
Chromosomal abnormalities among children born with conotruncal
cardiac defects. Birth Defects Res A Clin Mol Teratol. 85:30–35.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fokstuen S, Arbenz U, Artan S, et al:
22q11.2 deletions in a series of patients with non-selective
congenital heart defects: incidence, type of defects and parental
origin. Clin Genet. 53:63–69. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Borgmann S, Luhmer I, Arslan-Kirchner M,
Kallfelz HC and Schmidtke J: A search for chromosome 22q11.2
deletions in a series of 176 consecutively catheterized patients
with congenital heart disease: no evidence for deletions in
non-syndromic patients. Eur J Pediatr. 158:958–963. 1999.
View Article : Google Scholar
|
|
31
|
Song MS, Hu A, Dyamenahalli U, et al:
Extracardiac lesions and chromosomal abnormalities associated with
major fetal heart defects: comparison of intrauterine, postnatal
and postmortem diagnoses. Ultrasound Obstet Gynecol. 33:552–559.
2009. View
Article : Google Scholar
|
|
32
|
Bellucco FT, Belangero SI, Farah LM, et
al: Investigating 22q11.2 deletion and other chromosomal
aberrations in fetuses with heart defects detected by prenatal
echocardiography. Pediatr Cardiol. 31:1146–1150. 2010. View Article : Google Scholar : PubMed/NCBI
|