Introduction
Chronic obstructive pulmonary disease (COPD) is
characterized by an airflow obstruction that is partly reversible.
This is mainly attributable to the airway narrowing caused by wall
remodeling and the wall collapsibility in expiration due to loss of
alveolar attachment and elastic recoil of the small airways
(1). Spirometry is the ‘gold
standard’ that is used to assess airflow obstruction in COPD
patients. Forced expiration is used as part of spirometry in the
diagnosis and staging of COPD. This procedure is difficult for
patients to perform as it is effort-dependent and can alter the
bronchomotor tone. Body plethysmography is an alternative to the
pulmonary function testing technique and allows the assessment of
airway resistance and conductance. However, it can be technically
demanding for patients to perform this test as it requires complex
‘panting’ maneuvers. Thus, there is a requirement to find easy and
physiologically accurate methods to assess pulmonary mechanics in
COPD patients.
The forced oscillation technique (FOT) was developed
in 1956 (2). FOT measures the
impedance of the respiratory system by applying small oscillation
pressures on the mouth during a normal breathing forced oscillation
technique (3). FOT systems use
pseudorandom noise signals to enable simultaneous measurement of
respiratory resistance (Rrs) and reactance (Xrs). It has been
reported that FOT measurements are associated with traditional lung
function measurements in patients with obstructive lung disease
(4,5) and it has been shown that in COPD
patients, FOT resistance measurements can be used to accurately
diagnose mild COPD. However, reactance measurements are better for
grading the severity of disease (6). The impulse oscillometry system (IOS)
(7) is a type of FOT but has two
important differences: (i) Rectangular waveform impulses are used
instead of pseudorandom noise signals and (ii) the IOS has a
different set of data output. Hellincx et al (8) reported that IOS provides similar but
not identical Rrs and reactance measurements when compared with
FOT. Thus, this study showed that these two techniques may generate
different results. Theoretically, the elastic property of the lung
is reflected by the low oscillatory frequencies of reactance, while
the inertial properties are dominantly reflected in the high
oscillatory frequency range of reactance (9). In obstructive lung disease, further
increases in Rrs and changes of Xrs to a more negative value at
lower oscillatory frequencies have been reported (10). Additionally, it has been reported
that the within-breath changes in Xrs5 (ΔXrs5; the difference
between expiratory and inspiratory reactance) have been indicated
to represent the overall distribution of expiratory flow limitation
during tidal breathing (10–12).
COPD and asthma studies have shown that IOS measurements are more
sensitive than forced expiratory volume in 1 sec (FEV1) for
measuring the pulmonary effects of bronchodilator drugs (13–15).
Additionally, IOS measurements can also be used to sensitively
diagnose obstructive lung disease (16,17).
Thus, the understanding of which IOS measurements are correlated
with the degree of airflow obstruction (as measured by FEV1) and
which measurements are correlated with the degree of hyperinflation
(measured by lung volumes) is required. The present study describes
the correlation of IOS measurements to other pulmonary function
measurements in a large cohort of COPD patients (n=180). A set of
patients was followed-up for 1 year and the changes in IOS and
spirometry measurements were compared over that period.
Subjects and methods
Subjects
Patients (n=180) with COPD were selected for the
measurement of pulmonary function (see Table I for demography). All the patients
were invited for follow-up 1 year following the initial tests; 95
patients agreed to participate, while the remaining patients were
unable to do so. All the patients with COPD had smoking-related
COPD without α1-antitrypsin deficiency and had a smoking history of
>30 pack-years (packs smoked per day × year). COPD was diagnosed
based on a clinical history of exertional dyspnea and pulmonary
function characterized by a partly reversible airflow obstruction.
Partly reversible airflow obstruction is defined as FEV1/FVC
<70% following the inhalation of a β2-agonist and subsequent to
treatment with bronchodilators in accordance with the Global
Initiative for Chronic Obstructive Lung Disease guidelines
(1). Patients with a clinical
history of asthma, an exacerbation or any change in their COPD
therapy within 4 weeks of the study, or a history of lung cancer
were excluded. Written informed consent was obtained from the
patients and the Ethics Committee of Tongji University, Shanghai,
China approved the study (K14-135).
 | Table IPatient demographics at baseline. |
Table I
Patient demographics at baseline.
| Characteristic | Value |
|---|
| Gender |
| Male | 157 |
| Female | 23 |
| Age, years | 61.56±9.20 |
| Current smokers | 125 |
| Male | 109 |
| Female | 16 |
| Ex-smokers | 55 |
| Male | 48 |
| Female | 7 |
| ICS + LABA |
| Use | 166 |
| No use | 14 |
| LANC |
| Use | 86 |
| No use | 94 |
| Oral
theophylline |
| Use | 42 |
| No use | 83 |
Study design
Each patient performed pulmonary function tests in
the following order: IOS, body plethysmography (including
measurement of lung volumes) and spirometry.
Pulmonary function measurements
IOS (Masterscreen IOS, Erich Jaeger, Hoechberg,
Germany) measurements were performed as described previously
(15) and the actual values of Rrs
at 5 and 20 Hz (R5 and R20, respectively), reactance at 5 Hz (X5)
and the resonant frequency (Fres) were recorded. Forced
end-expiratory flow (FEF)75 and total inspiratory resistance (Rtot)
were measured in a constant volume plethysmograph (Sensormedics
Vmax 6200; SensorMedics Corporation, Yorba Linda, CA, USA), and the
total lung capacity (TLC) and residual volume (RV) were then
calculated from these parameters. IOS and body plethysmograph
measurements were repeated three times and the mean value was used
for further analysis. FEV1 was measured using the spirometry system
on the Masterscreen (CareFusion, Berlin, Germany). The readings
were obtained three times and the highest FEV1 was recorded.
Statistical analysis
The Kolmogorove-Smirnov test was applied to
determine the normality of the data. Pearson’s or Spearman’s
correlation tests were applied to determine the correlation between
the baseline IOS and pulmonary function measurements, and the
correlation between the change in FEV1 and in IOS over 1 year. The
paired t-test or the Wilcoxon matched pair test was performed in
order to determine the differences between the initial scores and
the scores at the 1-year follow up. P<0.05 was considered to
indicate a statistically significant difference. Statistical
analyses were performed using SPSS 13.0 (SPPS Inc., Chicago, IL,
USA).
Results
Baseline patient demographics and
pulmonary function measurements (Tables I and II, respectively)
The correlation between IOS and other pulmonary
function measurements was analyzed. R5, X5 and Fres were all
significantly associated with FEV1 (P<0.05) and the correlation
coefficients were −0.496, 0.635 and −0.721, respectively. However,
R20 was not correlated with FEV1 (P>0.05; Fig. 1). R5, X5 and Fres were all
associated with FEF75 (P<0.05) and the correlation coefficients
were −0.468, 0.505 and −0.629, respectively. There was a lower
correlation between R20 and FEF75 and the correlation coefficient
was −0.197 (P<0.05; Fig. 2).
R5, X5 and Fres were all associated with RV (P<0.05) and the r
values were 0.326, −0.485 and 0.570, respectively. However, that
was not the case with R20 (Fig.
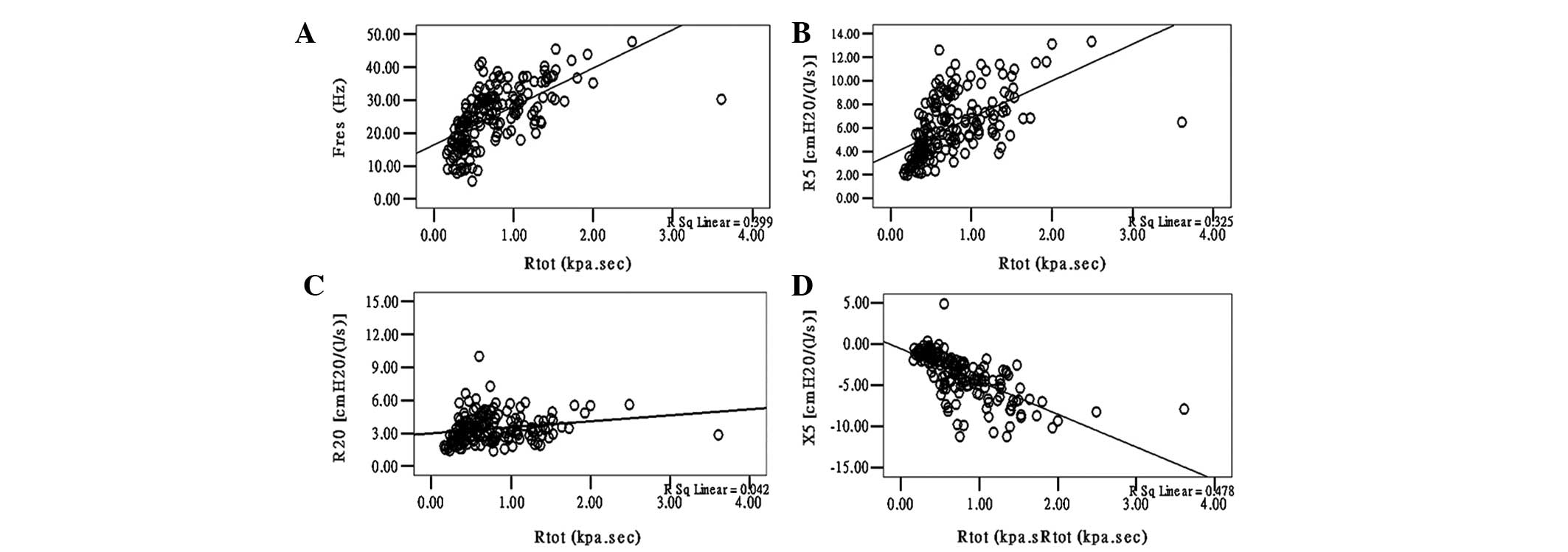
3). R5, X5, Fres and R20 were all significantly associated with
Rtot (P<0.05) and the correlation coefficients were 0.570,
−0.691, 0.632 and 0.206, respectively (Fig. 4).
Comparison of FEV1, RV and IOS
measurements at initial tests and at 1-year follow up
In order to compare the changes in FEV1, RV and IOS
measurements at 1-year follow up in the 95 patients, the changes as
group statistics and changes for each individual were considered.
Regarding the overall group mean or median values, there was a
statistically significant increase in the FEV1, RV and X5 after 1
year, but not in the R5, R20 and Fres (Table II).
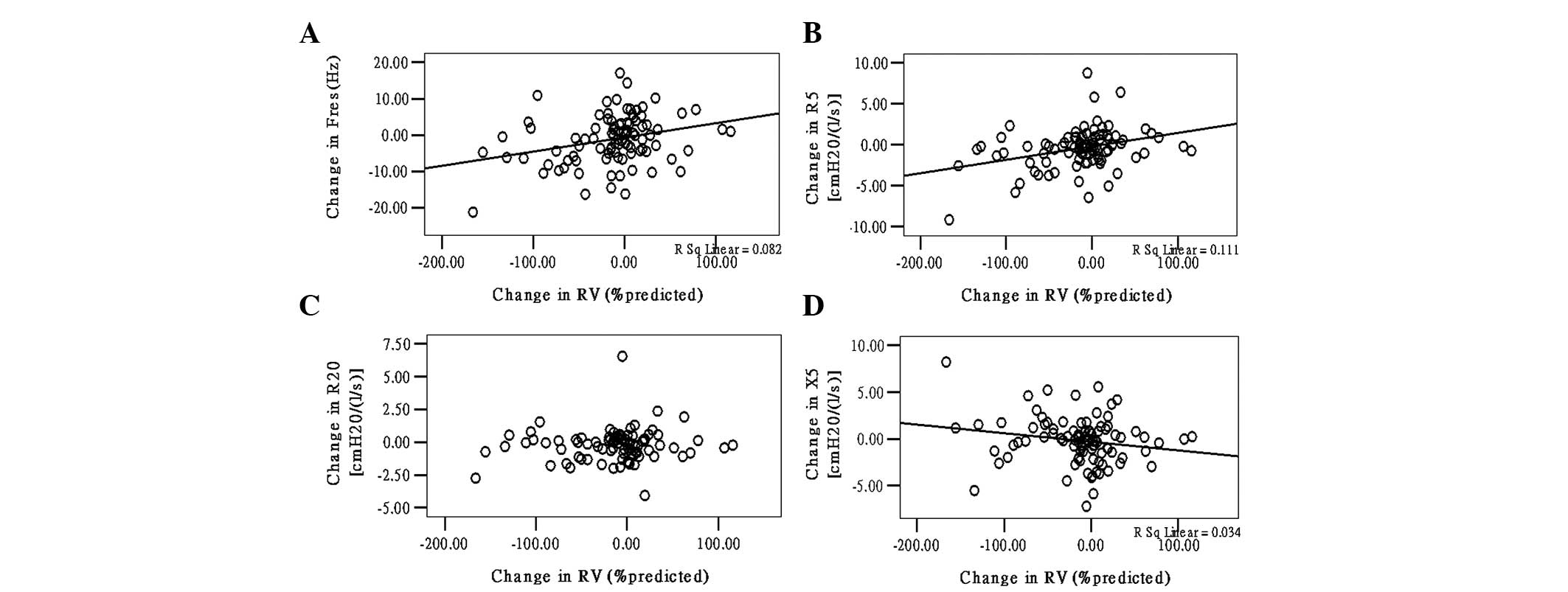
The correlation between changes in FEV1 and IOS
measurements within each individual over 1 year are shown in
Fig. 5. The changes in X5, R5 and
Fres were significantly correlated with the changes in FEV1;
however, there was no correlation between R20 and FEV1. Similarly,
the RV changes were significantly correlated with R5, X5 and Fres
changes over 1 year, while there was no correlation between R20 and
RV (Fig. 6).
Discussion
A total of 180 patients were selected with moderate
to severe COPD, and pulmonary function and IOS tests were conducted
in order to determine the correlation between these parameters and
the change in the measurement values after 1 year. In total, 95
patients completed the study by returning for the 1-year follow up
tests. Fres, R5 and X5 were identified to be significantly
correlated with FEV1, with airflow obstruction (FEF75, Rtot) and
with over inflation (RV). However, R20 had no correlation with FEV1
and RV, while it had a low degree of correlation with FEF75 and
Rtot. FEV1 is a recognized indicator of airflow obstruction and FEF
is used to determine the common indicators of small airflow
function. Rtot, the total airway resistance, caused by airflow
obstruction is one of the reasons for the increase in airway
resistance. Therefore, one of the major findings of the present
study is that IOS resistance in patients with airflow obstruction
in COPD due to respiratory mechanics is significant. Subsequent to
follow-up of the 95 patients at 1 year, a close correlation of the
reactor with FEV1 was identified. After 1 year, FEV1 marginally
increased when compared with the previous value. RV was marginally
reduced, but X5 was increased in comparison to the previous value.
The changes of X5 and FEV1 were significantly associated as were X5
and RV. R20 was not associated with FEV1 and RV. The present study
was the second major study that identified X5 in the evaluation of
airflow obstruction, and demonstrated that X5 reactance was more
valuable than the other reactances.
As it is known, due to peripheral airway obstruction
in patients with COPD, the respiratory compliance is reduced, the
lung elastic recoil force is decreased and the elastic resistance
is increased. X5 represents the peripheral reactance (capacitive
and inertial reactance) and it positively correlates with FEV1
(r=0.635). At the 1 year follow-up, X5 and FEV1 were significantly
increased when compared with the first visit and these two changes
were significantly correlated. This result indicated that X5 can be
used for the evaluation of COPD in patients with airway
obstruction. Previous studies by Di Mango et al (6) and Kolsum et al (19) showed that on the first visit and at
the 1 year follow-up appointment, FEV1 and X5 were significantly
correlated and FEV1 was raised after one year while X5 was not. The
results of the present study results were consistent with the
findings of Di Mango et al and Kolsum et al. With the
use of FOT methods, Di Mango et al reported that reactance
measurements were better than resistance measurements for grading
the severity of airflow obstruction in COPD patients (6).
The strength of the correlation between FEV1 and the
reactance measurements (r=0.635 for X5 and r=−0.721 for Fres) and
between FEF75 (r=0.505 for X5 and r=−0.629 for Fres) or Rtot
(r=−0.691 for X5 and r=0.632 for Fres) and reactance measurements
indicates a moderate association between the IOS airway reactance
measurements and airflow obstruction, regardless of whether
measurements were assessed by FEV1 or FEF75. IOS is therefore not a
replacement for FEV1, but as previously pointed out for classic FOT
methods, it provides complimentary information on respiratory
mechanics. IOS reactance measurements provide insights into changes
in pulmonary compliance associated with the severity of airflow
obstruction. By contrast, IOS reactance measurements appear to be
less indicative of mechanical changes due to hyperinflation.
Xrs by capacity and inertial reactance is composed
of two parts. Capacity reactance and compliance are reciprocal and
more negative values reveal that the compliance is lower. MacLeod
et al (9) found that the
inertial reactance was of little clinical significance and that the
Xrs changes mainly depend on the compliance of respiratory system
changes. Borrill et al (15) considered that in emphysema
patients, although there is a destruction of lung parenchyma, there
is an increased lung compliance and that in COPD patients due to
the presence of airway obstruction, the total respiratory
compliance is reduced. In the present study, the stronger
correlation between X5 and PFT parameters can not only be used for
reflecting the respiratory compliance changes but also for the
evaluation of COPD patients with airway obstruction together with
FEV1.
With an increase in the Fres, the X5 becomes more
negative and indicates a decrease in compliance. The present study
found that Fres and X5 were not only associated with FEV1 but were
also significantly associated with RV. Van Noord et al
(4) considered that the X5 decline
was sensitive enough for the diagnosis of emphysema. The
correlation between X5 and RV also confirmed this point. In COPD
patients, the presence of emphysema led to an increase in pulmonary
compliance. However, Fres and FEV1 were negatively correlated and
this was due to lung hyperinflation, which resulted in the
destruction of the lung parenchyma. Therefore in the present study,
the correlation of IOS reactance (X5) and lung volume (RV) in COPD
patients was due to lung hyperinflation caused by airflow
obstruction. The significant correlation between Fres and Rtot also
verified that Fres, which reflects an increase in airway
resistance, was the most sensitive index.
Previous studies by Clement et al (18) have demonstrated that peripheral
airway obstruction was characterized by a greater increase in the
resistance at low frequencies (R5) when compared with the higher
frequencies (R20). This is often referred to as the frequency
dependence of resistance (20). R5
represents the total airway resistance whereas R20 represents
proximal airway resistance. Since there is a frequency-dependent
R-value, airway resistance in COPD patients depends on the R5 and
not R20. Helinckx et al (8)
found that R5 and Rtot were apparently correlated and that the R5
value was marginally greater than the Rtot. The present study found
that R5 was significantly associated with Rtot and that R20 and
Rtot were not significant, and this confirmed that R5 was more
suitable than R20 to reflect airway obstruction in COPD patients.
Duiverman et al (21) found
that the airway resistance at low frequency distinguished patients
with obstructive disease from healthy patients, which supports the
findings of the present study. The current study also showed that
R5, but not R20, was associated with FEV1 at the baseline visit,
which adds further weight to the evidence that low frequency IOS
resistance measurements can be used to assess peripheral airway
obstruction in COPD patients (22). By contrast, R20 measurements appear
to be unrelated to airflow obstruction in COPD patients and the
value of these measurements in COPD patients are questionable.
In conclusion, it has been demonstrated that X5, R5
and Fres are IOS measurements most closely associated with more
traditional measurements of pulmonary function in COPD patients.
Subsequent to one year of follow-up, changes of X5 and FEV1 were
identified to be closely correlated, which indicated that X5 was
not only sensitive to detect airflow obstruction in COPD patients,
but could provide an improved evaluation of the changes in airflow
obstruction. In view of the correlation with RV, X5 was also
available as an indicator to evaluate the hyperinflation in
patients with COPD. Thus, the reactance measurement of X5 offers an
alternative to FEV1. The ease of use of IOS and the sensitivity of
this technique to measure the effects of therapeutic interventions
in COPD patients may provide a basis for the increased use of this
method in clinical practice.
Acknowledgements
This study was supported by the Young Foundation of
Sanitary Bureau of Shanghai (grant no. 20124Y117).
References
|
1
|
Rabe KF, Hurd S, Anzueto A, et al: Global
strategy for the diagnosis, management, and prevention of chronic
obstructive pulmonary disease: GOLD executive summary. Am J Respir
Crit Care Med. 176:532–555. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cogswell JJ: Forced oscillation technique
for determination of resistance to breathing in children. Arch Dis
Child. 48:259–266. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dubois AB, Brody AW, Lewis DH, et al:
Oscillation mechanics of lungs and chest in man. J Appl Phys.
8:587–594. 1956.PubMed/NCBI
|
|
4
|
Van Noord JA, Clément J, Van de Woestijne
KP, et al: Total respiratory resistance and reactance in patients
with asthma, chronic bronchitis, and emphysema. Am Rev Respir Dis.
143:922–927. 1991.PubMed/NCBI
|
|
5
|
Zerah F, Lorino AM, Lorino H, et al:
Forced oscillation technique vs spirometry to assess
bronchodilatation in patients with asthma and COPD. Chest.
108:41–47. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Di Mango AM, Lopes AJ, Jansen JM, et al:
Changes in respiratory mechanics with increasing degrees of airway
obstruction in COPD: detection by forced oscillation technique.
Respir Med. 100:399–410. 2006.PubMed/NCBI
|
|
7
|
Goldman MD: Clinical application of forced
oscillation. Pulm Pharmacol Ther. 14:341–350. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hellinckx J, Cauberghs M, De Boeck K, et
al: Evaluation of impulse oscillation system: comparison with
forced oscillation technique and body plethysmography. Eur Respir
J. 18:564–570. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
MacLeod D and Birch M: Respiratory input
impedance measurement: forced oscillation methods. Med Biol Eng
Comput. 39:505–516. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dellacà RL, Santus P, Aliverti A, et al:
Detection of expiratory flow limitation in COPD using the forced
oscillation technique. Eur Respir J. 23:232–240. 2004.
|
|
11
|
Dellacà RL, Rotger M, Aliverti A, et al:
Noninvasive detection of expiratory flow limitation in COPD
patients during nasal CPAP. Eur Respir J. 27:983–991.
2006.PubMed/NCBI
|
|
12
|
Dellacà RL, Duffy N, Pompilio PP, et al:
Expiratory flow limitation detected by forced oscillation and
negative expiratory pressure. Eur Respir J. 29:363–374.
2007.PubMed/NCBI
|
|
13
|
Houghton CM, Woodcock AA and Singh D: A
comparison of lung function methods for assessing dose-response
effects of salbutamol. Br J Clin Pharmacol. 58:134–141. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Houghton CM, Woodcock AA and Singh D: A
comparison of plethysmography, spirometry and oscillometry for
assessing the pulmonary effects of inhaled ipratropium bromide in
healthy subjects and patients with asthma. Br J Clin Pharmacol.
59:152–159. 2005. View Article : Google Scholar
|
|
15
|
Borrill ZL, Houghton CM, Woodcock AA, et
al: Measuring bronchodilation in COPD clinical trials. Br J Clin
Pharmacol. 59:379–384. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Park JW, Lee YW, Jung YH, et al: Impulse
oscillometry for estimation of airway obstruction and
bronchodilation in adults with mild obstructive asthma. Ann Allergy
Asthma Immunol. 98:546–552. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Al-Mutairi SS, Sharma PN, Al-Alawi A, et
al: Impulse oscillometry: an alternative modality to the
conventional pulmonary function test to categorise obstructive
pulmonary disorders. Clin Exp Med. 7:56–64. 2007. View Article : Google Scholar
|
|
18
|
Clément J, Làndsér FJ and Van de Woestijne
KP: Total resistance and reactance in patients with respiratory
complaints with and without airways obstruction. Chest. 83:215–220.
1983.PubMed/NCBI
|
|
19
|
Kolsum U, Borrill Z, Roy K, et al: Impulse
oscillometry in COPD: Identification of measurements related to
airway obstruction, airway conductance and lung volumes. Respir
Med. 103:136–143. 2009.PubMed/NCBI
|
|
20
|
Lándsér FJ, Nagles J, Demedts M, et al: A
new method to determine frequency characteristics of the
respiratory system. J Appl Physiol. 41:101–106. 1976.PubMed/NCBI
|
|
21
|
Duiverman EJ, Neijens HJ, Van der Snee-van
Smaalen M, et al: Comparison of forced oscillometry and forced
expirations for measuring dose-related responses to inhaled
methacholine in asthmatic children. Bull Eur Physiopathol Respir.
22:433–436. 1986.PubMed/NCBI
|
|
22
|
Ortiz G and Menendez R: The effects of
inhaled albuterol and salmeterol in 2- to 5-year-old asthmatic
children as measured by impulse oscillometry. J Asthma. 39:531–536.
2002.
|