Introduction
Paraneoplastic neurological syndrome (PNS) is a
neurological syndrome, which is closely associated with malignancy.
Among the various types of malignant tumor that cause PNS, small
cell lung cancer (SCLC) is the most common (1). Several studies have suggested that
cross immunoreaction, caused by common antigens expressed in the
neuron and tumor cells of patients with PNS, is directed at the
tumor and the nervous system, limiting tumor growth and leading to
the occurrence of PNS (2).
Previous studies have indicated that inside the body of patients
with PNS, numerous neuron-specific antibodies exist, including the
anti-Hu antibody, and these studies demonstrated that humoral
immunity has an important function in the incidence of PNS
(3,4). However, a number of studies have
suggested that humoral immunity is not the only pathogenic factor
and that T cell-mediated cytoimmunity is also involved in the
pathogenesis of PNS (5,6). The present study used the
Avidin-Biotin Complex (ABC) immunohistochemical method and western
blot analysis to detect neuron-specific antibodies (anti-Hu
antibody) in the serum of patients with PNS. The positive antibody
of peripheral blood mononuclear cells (PBMCs) and SCLC cell lines
(H446) from patients with PNS were co-cultured in vitro. The
present study aimed to observe whether PBMC was able to inhibit the
growth of H446. In addition, the percentage of CD4+ and
CD8+ T cells following stimulation with interleukin
(IL)-2 was monitored, based on humoral and cellular immunity, to
examine the pathogenesis of PNS.
Materials and methods
Subjects
PNS group
A total of seven patients with SCLC and PNS with a
high titer of anti-Hu antibodies were enrolled from the Department
of Neurology, The First Affiliated Hospital of Bengbu Medical
College (Bengbu, China). Among these patients, five were male and
two were female with an average age of 57.7±8.4 years (mean ±
standard deviation). Among these patients, three had paraneoplastic
sensory neuropathy two had paraneoplastic limbic lobe cephalitis
and two had paraneoplastic encephalomyelitis.
SCLC group
A total of six SCLC patients without PNS (anti-Hu
antibody negative) were included from the same hospital. Of these
patients, four were male and two were female with an average age of
55.1±9.0 years (mean standard ± deviation). The present study was
conducted in accordance with the Declaration of Helsinki and was
conducted with approval from The Ethics Committee of Bengbu Medical
College (Bengbu, China). Written informed consent was obtained from
all patients.
Control group
A total of eight health workers from The First
Affiliated Hospital of Bengbu Medical College were included,
comprising five males and three females with an average age of
48.8±8.5 years (mean ± standard deviation).
All PNS patients were diagnosed using the criteria
for PNS (7). The lung primary
tumors removed from patients during surgery were confirmed to be
SCLC following pathological examination.
Immunohistochemical method
Frozen sections (6 μm) of a healthy brain (obtained
within 6 h mortality and without infectious disease or PNS) were
obtained. Following drying at room temperature for 10 min, the
sections were fixed with acetone (Tianjin TBD Biotechnology
Development Center, Tianjin, China) for 10 min and then blocked for
30 min in 10% calf serum albumin (Hangzhou sijiqing Biological
Engineering Materials Co., Hangzhou, China) dissolved in
phosphate-buffered saline (PBS; Tianjin TBD Biotechnology
Development Center). The sections were incubated overnight at 4°C
following the addition of several different serum dilutions and
were then incubated with polyclonal goat anti-human IgG (cat no.
BA-3000; Vector Laboratories, Inc., Burlingame, CA, USA) at room
temperature for 30 min and with ABC (cat no. PK-4000; Vector
Laboratories, Inc.) for 40 min. The reaction was terminated with
PBS following staining of the slides using benzidine (Sigma, Santa
Clara, CA, USA) for 5 min. Finally, the slides were dehydrated
using alcohol and xylene (Fengyuan Pharmaceutical Co., Bengbu,
China) and were then assessed using a conventional microscope
(WJ12-50, XSB-14; Shanghai Precision Instrument Co., Shanghai,
China).
Western blot analysis
Neuronal nucleus extraction
Nuclei were extracted from healthy neurons via the
improved Blomstrand and Hamberger method (8). The neuron extracts were abstracted
via sodium dodecyl sulfate-polyacrylamide gel electrophoresis
(SDS-PAGE; Fengyuan Pharmaceutical Co.) and transferred onto a
nitrocellulose membrane (Shanghai Tuoran Biological Technology Co.,
Shanghai, China) based on the Towbin method (9). These were then fixed in 5% skimmed
milk and dissolved in PBS for 60 min, following which a variety of
serum dilutions [≥1:1,000; 1 g bovine serum albumin + 0.01 PBS (100
ml) + 0.08g NaN3] were added prior to incubation
overnight at 4°C. The reaction was terminated with PBS and compared
with the standard protein following incubation of the extracts with
polyclonal goat anti-human IgG at room temperature for 30 min and
with ABC for 40 min. The extracts were then colored using benzidine
(Fengyuan Pharmaceutical Co.) for 5–8 min.
HuD cloning method for purification of
proteins
The HuD cloning purified protein, a product of
genetic engineering obtained from Professor Jean-Yves Delattre
(Salpetriere Medical College of Curie University, Paris, France),
was separated via SDS-PAGE. The following steps were identical to
those described above in the method for the neuronal nuclei
extraction.
Culture of cells and staining with
carboxyfluorescein diacetate succinimidyl ester (CFSE)
The PBMCs were separated from the venous blood via
gradient centrifugation (778 g for 20 min at 20°C) and seeded in
24-well plates. CD3 monoclonal antibody (obtained from Professor
Carding, Department of Medical Microbiology, University of
Pennsylvania, Philadelphia, USA), at a final concentration of 5
g/ml and rhIL-2 (Changsheng Gene Pharmaceutical Co., Changchun,
China), at a final concentration of 50 μg/ml, were placed in each
well. The PBMCs and H446 cells were cultured in RPMI 1640 cell
culture fluid (10% new-born calf serum +150,000U/l gentamicin) in 5
% CO2 saturated humidity incubator at 37°C for 5–7 days and H446
was obtained and conventionally cultured. The PBMCs and H446 cells
were diluted with PBS at densities of 5×106 and
3×106/ml, respectively. The cell suspensions were
stained using CFSE (Molecular Probes, Carlsbad, CA, USA; final
concentration 1 μmol/l) at 37°C for 10 min and rinsed twice with
PBS. The cell suspensions of PBMCs and H446 were detected using
flow cytometry (FACS Calibur; BD Biosciences, Franklin Lakes, NJ,
USA) and the initial fluorescence intensity was analyzed using
Modifit software (Pc Win98/NT; Verity Software House, Inc.,
Topsham, ME, USA) and preserved. Followed staining with CFSE, the
PBMC and H446 cells were cultured together at densities of
2×105 and 5×104/ml, respectively, for 3
days.
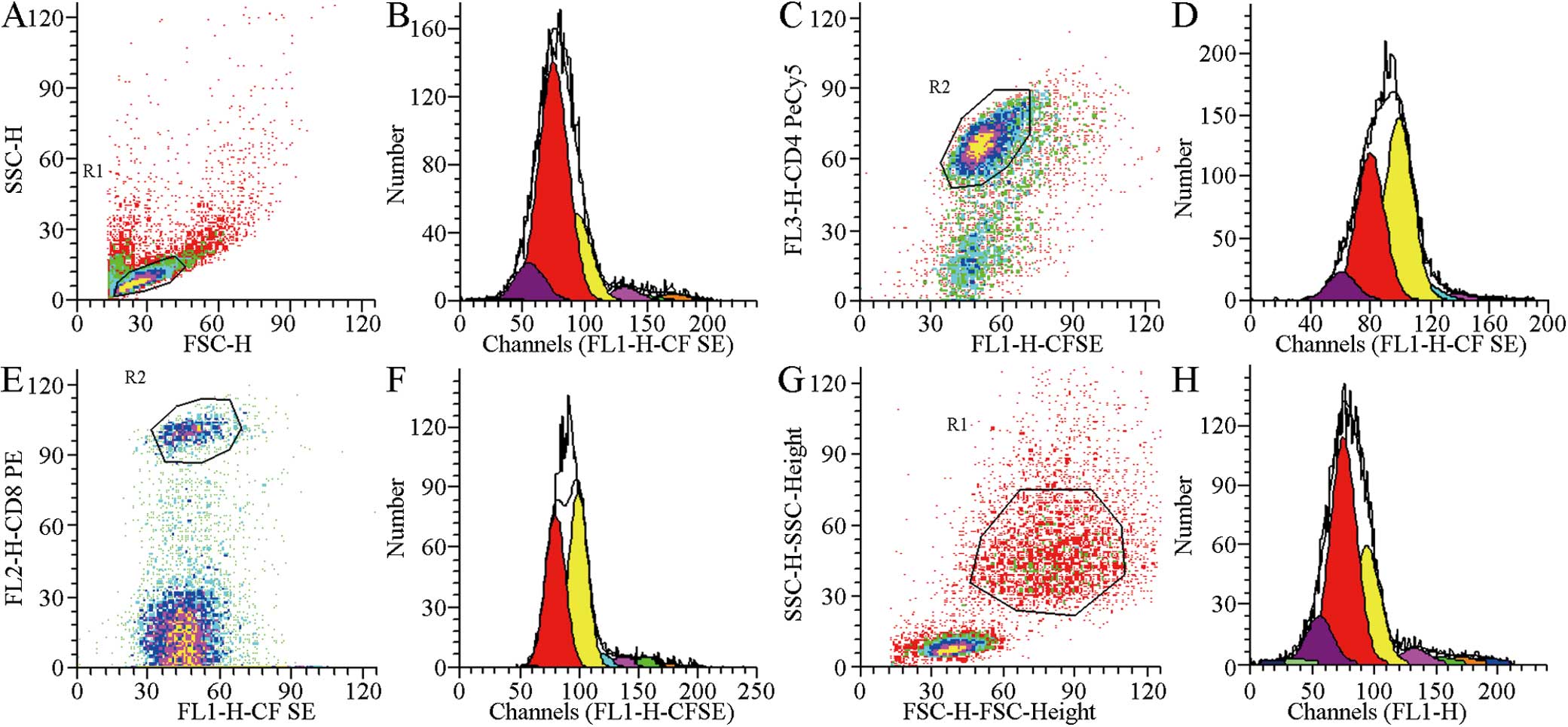
Assessment of cell proliferation
Following culture, the cell suspensions were added
to different fluorescent labeled monoclonal antibodies, namely,
IgG1/IgG2, CD3/CD4 and CD3/CD8 (BD Biosciences). The CFSE
fluorescence intensity was detected and compared with the initial
fluorescence and the proliferation index of total PBMC,
CD4+ and CD8+ T cells and H446 cells were
obtained using ModFit software. The proportion of each PBMC
subgroup was analyzed using CellQuest software (BD
Biosciences).
Statistical analysis
The statistical significance of differences in the
proliferation index between two types of culture was assessed using
a Wilcoxon matched-pair signed-rank test. Differences between three
groups were assessed via Kruskal Wallis H test. For all statistical
analyses, P<0.05 was considered to indicate a statistically
significant difference.
Results
ABC
From screening a total of 20 patients with PNS and
120 patients with SCLC, staining was observed in the neuronal
nuclei of the frozen sections of normal brain in 89% of the PNS
patients and 40% of the SCLC patients, with negative nucleoli. No
reaction was observed with glial cells in the nervous tissue or in
the liver and kidney tissue. The antibody concentration in the
serum of the PNS group was 1:1,000–64,000, whereas the value in the
SCLC group was 1:1,000–8,000. No staining was observed in the
control groups (Fig. 1).
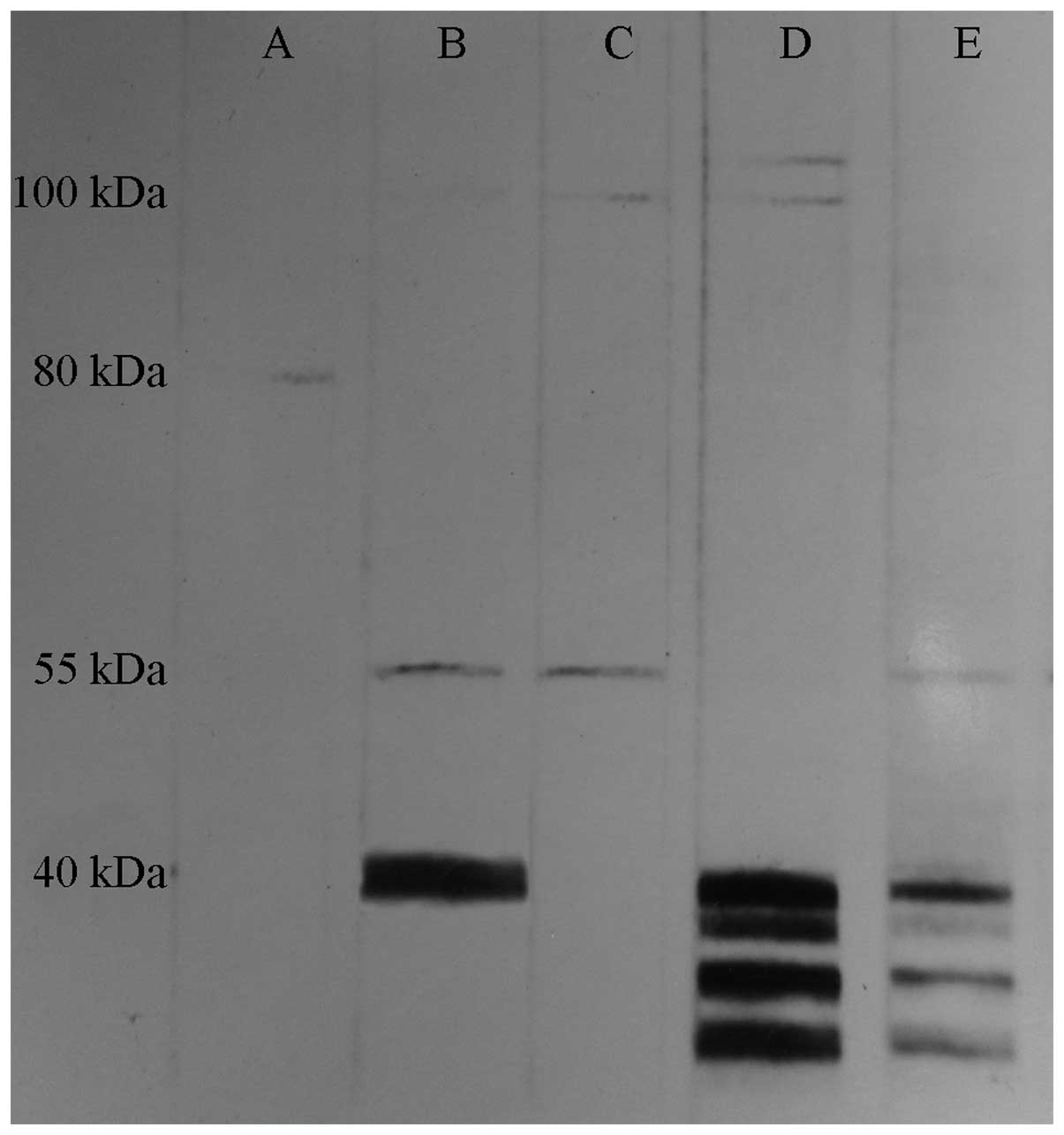
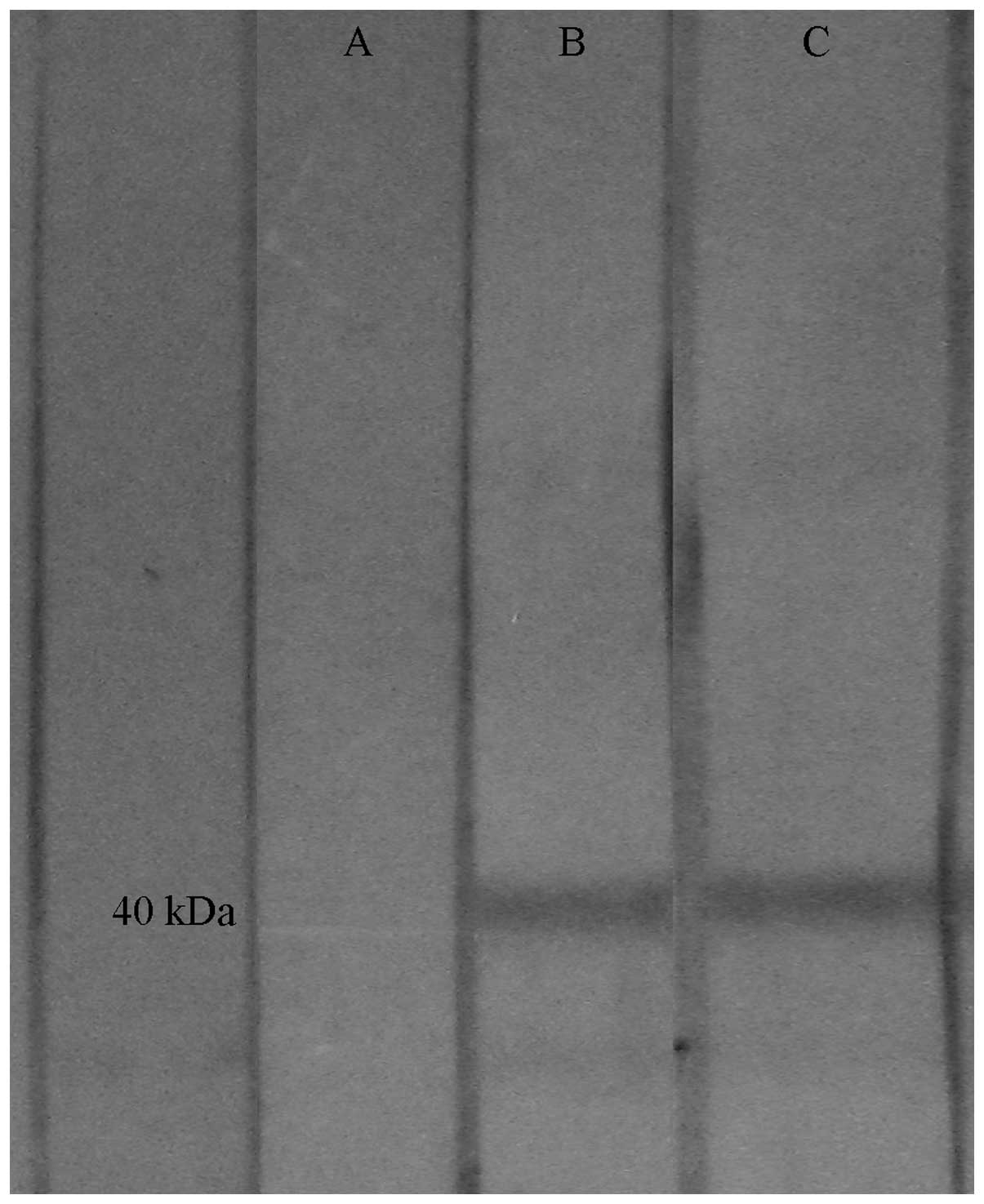
Neuronal nucleus extraction
The anti-Hu antibody identified mainly protein
antigen with a molecular weight (MW) between 35,000 and 40,000 Da
in the neuronal nuclei extract. The serum from a total of two SCLC
and 16 PNS patients had the above-mentioned specific bands, whereas
these bands were not observed in the control group (Fig. 2).
Purification of proteins
The anti-Hu antibodies and cloned HuD purified
protein formed a single band at 40,000 Da. The band observed in the
PNS and SCLC patients was identical to that obtained in the
neuronal nuclei extract method, whereas these bands were not
observed in the control group (Fig.
3).
Cell proliferation index
In the PNS and SCLC groups, no significant
differences were observed in the proliferation index of the H446,
total PBMCs, CD4+ and CD8+ T cells between
the mixed cultures and separate cultures. In the control group, the
proliferation index of the total PBMCs, CD4+ and
CD8+ T cells was increased significantly when the PBMC
and H446 cells were cultured together compared with when they were
cultured separately (P<0.05). The proliferation index of the
H446 cells decreased significantly (P<0.05; Table I and Fig. 4).
 | Table IComparison of the cell proliferation
index in the control group by two culture methods (mean ± standard
deviation; n=8). |
Table I
Comparison of the cell proliferation
index in the control group by two culture methods (mean ± standard
deviation; n=8).
| Training method | H446 | Total PBMCs | CD4+ T
cell | CD8+ T
cell |
|---|
| Separate culture | 8.56±3.34 | 8.05±5.51 | 7.43±4.63 | 7.69±5.84 |
| Mixed culture | 6.97±2.52a | 8.90±5.67a | 8.60±4.83a | 8.93±5.73a |
Comparison of the percentages of each
subgroup
Following separate cultivation or co-culture with
H446, the proportion of CD4+ T cells increased
significantly in the PNS group compared with the control group. The
proportion of CD4+ and CD4+/CD8+ T
cells increased significantly and the proportion of CD8+
T cells decreased significantly in the SCLC group (P<0.05). The
proportion of CD4+ and CD4+/CD8+ T
cells in the SCLC group increased significantly and the proportion
of CD8+ T cells decreased significantly compared with
those in the PNS group (P<0.05–0.01). No significant difference
was observed between the separate culture and mixed culture in the
same group (Table II and Fig. 5).
 | Table IIComparison of CD4+,
CD8+ and CD4+/CD8+ ratio in the
three different groups (mean ± standard deviation). |
Table II
Comparison of CD4+,
CD8+ and CD4+/CD8+ ratio in the
three different groups (mean ± standard deviation).
| CD4+ T
cells (%) | CD8+ T
cells (%) |
CD4+/CD8+ ratio |
|---|
|
|
|
|
|---|
| Group | Separate
Training | Mixed Training | Separate
Training | Mixed Training | Separate
Training | Mixed Training |
|---|
| Control | 56.01±18.62 | 51.75±17.3 | 37.30±21.3 | 36.02±18.71 | 2.64±2.83 | 2.15±1.88 |
| PNS | 82.4 ±5.12a | 76.54±3.96a | 14.51±3.26 | 17.41±7.31 | 5.18±2.39 | 4.74±2.42 |
| SCLC | 88.99±2.61bc | 89.36±3.77bd | 9.72±2.49bc | 7.91±1.56bd | 9.74±2.85bc | 11.61±1.95bd |
Discussion
Cross immunoreaction triggered by a common antigen
is involved in the pathogenesis of numerous autoimmune diseases
(10). Previous studies have
indicated that the appearance of PNS is also associated with cross
immunoreaction (11,12). It has been previously demonstrated
that following repeated administration of serum immunoglobulin G
from patients with PNS into animals, neuromuscular junction
abnormalities were observed in the electrophysiology (13). It has also been observed that
particular anti-Hu antibody-positive SCLC patients have an improved
status compared with antibody-negative patients (14). Therefore, it has been hypothesized
that cross immunoreaction, which is directed at the tumor and the
nervous system, exists in patients with PNS, thereby limiting tumor
growth and resulting in the occurrence of PNS (15).
With the development of immunotechnology, the
neuron-specific anti-Hu antibody, has been identified inside
several patients with PNS. Several studies have demonstrated that
the appearance of PNS is closely associated with the immune
response of antibodies mediated in the body (16). Previous studies have revealed that
subgroups of anti-Hu antibodies are widely distributed in the
serum, nervous system and tumor tissue via the immunohistochemical
method (17,18). The present study demonstrated that
anti-Hu antibodies reacted significantly with the neuronal nuclei
of the central nervous system and reacted weakly with the
cytoplasm. The results of the western blot analysis indicated that
anti-Hu antibodies in the serum recognized protein antigens with a
relative MW between 35,000 and 40,000 Da in the neuronal extract
from the human cerebral cortex. Therefore, detecting anti-Hu
antibodies may be a promising method in the early diagnosis of PNS
(19).
To investigate the proliferation of lymphocytes and
tumor cells in an accurate manner, flow cytometry was performed to
detect cell proliferation. CFSE stably combines the proteins in
cells to produce fluorescence. Fluorescence intensity is reduced by
half when cells divide in half. Flow cytometry detects fluorescence
and cell surface molecules, which enables analysis of the
proliferation kinetics of the lymphocytes subgroup (20). The results demonstrated that in a
mixed culture in vitro, the H446 cells accelerated the
proliferation of PBMCs among healthy individuals and the
proliferation of PBMCs inhibited the growth of H446 cells. However,
a similar condition was not observed in the PNS and SCLC patients,
possibly due to the following reasons. Previous studies have
demonstrated that the percentage of CD4+ T cells and the
ratio of CD4+/CD8+ decreased in patients with
PNS, which in turn led to reduced immune function; therefore, the
PNS PBMC showed now clear inhibitory effects on tumor cells in
vitro (21,22). Another study demonstrated that, in
the peripheral blood of PNS patients, the percentage of
CD4+ T cells and the ratio of
CD4+/CD8+ cells is decreased, leading to a
degree of immune function inhibition in patients with PNS, but no
clear inhibitory effects on tumor cells cultured in vitro.
Healthy individuals have normal immune function and cell
proliferation. In the H446 culture, the immune function may respond
against tumor cells and inhibit the growth of H446.
Although the proportion of CD4+ T cells
and the ratio of CD4+/CD8+ T cells in PNS and
SCLC patients decrease, clone amplification may be prioritized in
this part of the cell body if sensitization of the antigen specific
T lymphocytes occurs inside. The present study demonstrated that
stimulating the activation of cell proliferation is prioritized due
to IL-2, regardless of the culture condition. The CD4+ T
cell ratio of PNS patients was significantly higher compared with
healthy individuals following culture, subsequent to augmenting
PBMCs with IL-2 for 5–7 days. In addition, the percentage of
CD4+ T cells and the ratio of
CD4+/CD8+ cells in the patients with SCLC
were higher compared with those of healthy individuals. Therefore,
the sensitized specific T cells in the PBMC of patients with PNS
and SCLC were predominantly composed of CD4+ T cells.
Previous studies have revealed that the immune response associated
with anti-Hu antibody syndrome involves the participation of
cellular and humoral immunities (23,24).
Studies have found that IgGl and IgG3 activate complement, however,
the reaction is weak and is confined to a small area of the nervous
system. In addition, natural killer cells have not yet been found
(25,26). This reaction may be a
non-complement mediated cytotoxicity reaction and non-antibody
dependent cell-mediated cytotoxicity (25). Anti-Hu antibodies can identify
antigens, including HuD and HuC. HuD is considered to be the only
antigen that is expressed in patients with SCLC (27). Previous investigation of the
peripheral blood lymphocyte membrane phenotype of anti-Hu antibody
syndrome patients has demonstrated that CD4+ T cells can
directly attack the HuD antigen and are involved in cell-mediated
nervous system damage and anti-tumor effects (28). In addition, based on pathological
results, the number of brainstem and spinal cord neurons of
patients with PNS is significantly decreased, with a large number
of inflammatory lymphocytes infiltrating the blood vessels, similar
to that of lymphocyte distribution in the sleeve sample. The
majority of inflammatory lymphocytes are CD19+ B and
CD4+ T cells (15).
This previous study also demonstrated that CD4+ T cells
are involved in cell-mediated damage of the nervous system. The
results revealed that sensitized specific T cells in patients with
PNS and SCLC were mainly CD4+ T cells in the body
(15). This observation is similar
to that of a previous study, showing that CD4+ T cells
have an important function in antitumor immunity (28).
The present study demonstrated that, following
culture in vitro, the proportion of CD4+ T cells
and CD4+/CD8+ T cells in the SCLC group was
significantly higher than that in the PNS group and the ratio of
CD8+ T cells was decreased significantly. The specific
reasons for this require further investigation.
Acknowledgements
This study was supported by the Anhui
Provincial-Level Natural Science Foundation Project (grant no.
03043715) and the Anhui Provincial Science and Technology Agency
Key Research Project (grant no. 03023049). The authors would like
to thank Professor France-Yves Delattre of Curie University (Paris,
France) for providing HuD cloning purified protein, Professor
Carding (Department of Medical Microbiology, University of
Pennsylvania) for providing CD3 monoclonal antibody, Professor
Jiangning Zhou (Department of Life Sciences, University of Science
and Technology of China) for providing fresh brain tissue and
Professor Baiqing Li (Immune Experiment Center, Bengbu, China) for
providing specific guidance and assistance in subject research and
flow cytometry.
References
|
1
|
Gandhi L and Johnson BE: Paraneoplastic
syndromes associated with small cell lung cancer. J Natl Compr Canc
Netw. 4:631–638. 2006.PubMed/NCBI
|
|
2
|
Poepel A, Jarius S, Heukamp LC, et al:
Neurological course of long-term surviving patients with SCLC and
anti-Hu syndrome. Neurol Sci. 263:145–148. 2007. View Article : Google Scholar
|
|
3
|
Hoffmann LA, Jarius S, Pellkofer HL, et
al: Anti-Ma and anti-Ta associated paraneoplastic neurological
syndromes: 22 newly diagnosed patients and review of previous
cases. J Neurol Neurosurg Psychiatry. 79:767–773. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cadavid D, Diaz JC, Masaru Shinchi A and
Jesualdo Ariza Y: Rapid, severe neurological impairment associated
with paraneoplastic cerebellar degeneration and anti-Yo antibodies.
Neurologia. 29:128–129. 2014. View Article : Google Scholar
|
|
5
|
Tani T, Tanaka K, Idezuka J and Nishizawa
M: Regulatory T cells in paraneoplastic neurological syndromes. J
Neuroimmunol. 196:166–169. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Carpenter EL, Vance BA, Klein RS, et al:
Functional analysis of CD8+ T cell responses to the onconeural self
protein cdr2 in patients with paraneoplastic cerebellar
degeneration. J Neuroimmunol. 193:173–182. 2008. View Article : Google Scholar
|
|
7
|
Blaes F: Paraneoplastic neurological
syndromes - diagnosis and management. Curr Pharm Des. 18:4518–4525.
2012. View Article : Google Scholar
|
|
8
|
Blomstrand C and Hamberger: A protein
turnover cell-riched factions from rabbit brain. J Neurochem.
16:1401–1407. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Towbin H, Staehelin T and Gordon J:
Electrophoretic transfer of proteins from polyacrylamide gels to
nitrocellurose sheets: procedure and some applications. Proc Natl
Acad Sci USA. 76:4350–4354. 1979. View Article : Google Scholar
|
|
10
|
Weissert R: The immune pathogenesis of
multiple sclerosis. J Neuroimmune Pharmacol. 8:857–866. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Johnson V, Friedman N, Haller NA and Hagel
C: Immune mediated neurologic dysfunction as a paraneoplastic
syndrome in renal cell carcinoma. J Neurooncol. 90:279–281. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hadjivassiliou M: Immune-mediated acquired
ataxias. Handb Clin Neurol. 103:189–199. 2012. View Article : Google Scholar
|
|
13
|
Sommer C, Weishaupt A, Brinkhoff J, et al:
Paraneoplastic stiff-person syndrome: passive transfer to rats by
means of IgG antibodies to amphiphysin. Lancet. 365:1406–1411.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hassan KA, Kalemkerian GP and Trobe JD:
Long-term survival in paraneoplastic opsoclonus-myoclonus syndrome
associated with small cell lung cancer. J Neuroophthalmol.
28:27–30. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tanaka K: A study on pathomechanisms of
paraneoplastic neurological syndrome. Rinsho Shinkeigaku.
41:1150–1152. 2001.(In Japanese).
|
|
16
|
Fukami Y, Umemura T, Shimono T, Yokoi T,
Kamijo M and Sakakibara T: Following sensory neuropathy, anti-Hu
antibody-positive paraneoplastic neurological syndrome presenting
with limbic encephalitis occurs after complete remission. Rinsho
Shinkeigaku. 53:287–292. 2013.(In Japanese). View Article : Google Scholar
|
|
17
|
Rauer S and Andreou I: Tumor progression
and serum anti-HuD antibody concentration in patients with
paraneoplastic neurological syndromes. Eur Neurol. 47:189–195.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Douglas CA and Ellershaw J: Anti-Hu
antibodies may indicate a positive response to chemotherapy in
paraneoplastic syndrome secondary to small cell lung cancer.
Palliat Med. 17:638–639. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wymenga AN, Slebos DJ, van der Naalt J,
van Putten JW and Peters FT: Abdominal complaints and neurological
symptoms as an early sign of lung cancer: a manifestation of the
anti-Hu syndrome. Ned Tijdschr Geneeskd. 147:616–619. 2003.(In
Dutch). PubMed/NCBI
|
|
20
|
Mannering SI, Morris JS, Jensen KP, et al:
A sensitive method for detecting proliferation of rare autoantigen
- specific human T cells. J Immunol Methods. 283:173–183. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Karagöz B, Bilgi O, Gümüs M, et al:
CD8+CD28− cells and
CD4+CD25+ regulatory T cells in the
peripheral blood of advanced stage lung cancer patients. Med Oncol.
27:29–33. 2010. View Article : Google Scholar
|
|
22
|
Pranzatelli MR, Travelstead AL, Tate ED,
et al: Immunophenotype of blood lymphocytes in
neuroblastoma-associated opsoclonus-myoclonus. Pediatr Hematol
Oncol. 26:718–23. 2004. View Article : Google Scholar
|
|
23
|
Hayashi Y and Inuzuka T: Paraneoplastic
neurological syndrome and autoantibodies. Brain Nerve. 65:385–393.
2013.PubMed/NCBI
|
|
24
|
de Graaf M, de Beukelaar J, Bergsma J, et
al: B and T cell imbalances in CSF of patients with Hu-antibody
associated PNS. J Neuroimmunol. 195:164–170. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Billet SE, Grando SA and Pittelkow MR:
Paraneoplastic autoimmune multiorgan syndrome: review of the
literature and support for a cytotoxic role in pathogenesis.
Autoimmunity. 39:617–630. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sehgal VN and Srivastava G: Paraneoplastic
pemphigus/paraneoplastic autoimmune multiorgan syndrome. Int J
Dermatol. 48:162–169. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Trier NH, Hansen PR, Vedeler CA, Somnier
FE and Houen G: Identification of continuous epitopes of HuD
antibodies related to paraneoplastic diseases/small cell lung
cancer. J Neuroimmunol. 243:25–33. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
de Jongste AH, de Graaf MT, Martinuzzi E,
et al: Three sensitive assays do not provide evidence for
circulating HuD-specific T cells in the blood of patients with
paraneoplastic neurological syndromes with anti-Hu antibodies.
Neuro Oncol. 14:841–848. 2012. View Article : Google Scholar : PubMed/NCBI
|