Introduction
Corneal thickness (CT) is frequently used as a
potential determinant of the safety of corneal refractive surgery
(1). Accurate determination of CT
prior to corneal refractive surgery has been proposed for the
determination of the corneal ablation rate, as well as for the
evaluation of postoperative refractive stability and safety
(1). Thus, measurement of the CT
prior to the initiation of corneal refractive surgery is
crucial.
The wearing of soft contact lenses (SCLs) has been
reported to affect the normal physiological structure of the
cornea, in particular the CT. Prior to corneal refractive surgery,
a large variance was observed in the CT of individuals following
discontinuation of long-term SCL wear. By contrast, the effects of
corneal contact lenses on CT largely depended on the duration of
wear, mode and the quality of the lenses (2). A study by Liu and Pflugfelder
(3) using the Orbscan corneal
topography system reported that long-term wear of corneal contact
lenses decreased overall CT. Conversely, an instant increase in CT
was observed in short-term SCL wearers (4). Optical coherence tomography (OCT), a
technique for performing high-resolution cross-sectional imaging,
is frequently used as an alternative to Orbscan tomography as it
has demonstrated higher reproducibility and accuracy (5).
Following advances in corneal biomechanics, corneal
surface ablation techniques including Epipolis laser in situ
keratomileusis (EPI-LASIK) and transepithelial photorefractive
keratectomy (T-PRK) have been frequently used in corneal refractive
surgery (6). Additionally,
ultra-LASIK techniques such as Femtosecond laser-assisted
Sub-Bowman’s Keratomileusis (SBK) have also been used (7).
The corneal epithelium, as the first protective
barrier of the cornea, has a vital function in the prevention of
pathogenic microorganism invasion (8). The corneal epilthelium also functions
as an essential optical transduction and refraction media with a
marked capacity for regeneration and repair (9). It has been proposed that the
measurement of corneal epithelial thickness (CET) is significant in
the early diagnosis of keratoconus and in epithelial healing
following corneal refractive surgery (10–12).
Although studies have been performed to measure the CET,
measurements were limited to the central region of the cornea
(11,13,14).
It is therefore necessary to measure the whole CET, in order to
investigate the characteristics of the thickness across the entire
cornea.
In the present study, Fourier-domain anterior
segment OCT was used to evaluate the CT and CET in SCL wearers
prior to being subjected to corneal refractive surgery. The present
study aimed to elucidate the normal ranges and distribution
characteristics of CT and CET in myopic subjects, and therefore
provide guidance for ophthalmologists in order to improve the
safety, predictability and stability of corneal refractive
surgeries.
Subjects and methods
Subjects
Prospective patients for refractory surgery at the
excimer laser treatment center at Jinan Mingshui Eye Hospital
(Zhangqiu, China) from April to July 2013 were included in this
study. The inclusion criterion was the wearing of SCLs for >two
years. Patients with ocular diseases were excluded from the present
study. A total of 56 right eyes of 56 subjects were enrolled. CT
and CET were measured prior to refractory surgery in subjects
immediately following discontinued SCL wear (group I, 56 eyes), and
subsequently following discontinued SCL wear for >two weeks
(group II, 56 eyes). Ninety-four eyes of 94 subjects with no
history of wearing corneal contact lenses were enrolled as a normal
control group. Informed consent was obtained from all subjects. The
present study was consistent with the Declaration of Helsinki, and
was approved by the Ethics Committee of Zhangqiu Mingshui Hospital
(Zhangqiu, China).
Anterior segment OCT examination
Imaging of the anterior segment was performed using
the RTVue-100 Fourier-domain anterior segment OCT system (Optovue
Inc., Fremont, CA, USA) by an experienced ophthalmologist. The OCT
was performed based on the optical Fourier-domain imaging technique
(15). Briefly, subjects were
required to watch the indicator light under natural conditions. On
this basis, Pachymetry and corneal power scanning modes were
selected for the scanning and the scanning diameter was set at 6
mm. Eight meridians were selected with 1024 axial scans per
meridian. The full procedure was repeated five times. The center of
the pupil was set as the focus site. To eliminate the potential
effects caused by the dodging of the eyelash or eyelid during CT
determination, subjects were required to open their eyes widely.
RTVue-CAM software (Version 6.11; Optovue Inc.) automatically
processed the OCT scan, provided the pachymetry (corneal thickness)
map and indicated CT and CET ranges at the positions with radii of
0.0–1.0, 1.0–2.5 (divided into eight quadrants) and 2.5–3.0 mm
(divided into eight quadrants) from the corneal center (Fig. 1). This procedure was performed in
triplicate.
Statistical analysis
All values are expressed as the mean ± standard
deviation. Data analysis was performed using SPSS 19.0 software
(International Business Machines, Armonk, NY, USA). Student’s
t-test was used for the inter-group comparison of CT and CET.
Paired sample t-test was performed for the CT and CET between two
subgroups. Spearman’s correlation analysis was applied to analyze
the correlation between CT and CET. P<0.05 was considered to
indicate a statistically significant difference between values.
Results
Subject information
In total, 94 eyes of 94 subjects (male, 71; female,
23) were enrolled in the control group. The age range of subjects
in the control group was 18–32 years with a mean age of 21.26±5.01
years. In the study group, 56 eyes of 56 subjects (male, 24;
female, 32) were enrolled. The age range of subjects in the study
group was 18–35 years with a mean age of 22.02±4.52 years. In the
study group, the duration of SCL wear was 2–9 years with a mean of
3.86±2.15 years.
Correlation between the central corneal
thickness (CCT) and epithelial thickness of the central cornea
In the control group, the mean CCT was 533.56±27.42
μm in a position with a radius of 1 mm from the central cornea,
while the mean epithelial thickness of the central cornea was
55.05±2.71 μm. A small positive correlation was observed between
the CCT and the epithelial thickness of the central cornea
(r=0.237, P=0.022; Table I).
 | Table ICT and CET in regions with a radius of
0–1 mm from the corneal center in myopic subjects. |
Table I
CT and CET in regions with a radius of
0–1 mm from the corneal center in myopic subjects.
| Groups | CT | CET |
|---|
| Control | 533.56±27.42 | 55.05±2.71 |
| Group I | 529.31±27.94 | 49.78±3.82a |
| Group II |
521.45±25.99ab | 51.18±2.22ab |
The mean CCT of group I was 529.31±27.94 μm, which
indicated no significant difference compared with that of the
control group (t=0.903, P=0.368). In group II, the mean CCT was
521.45±25.99 μm. Compared with the control group, a reduced CCT
(2.27%) was observed in group II (t=2.689, P=0.008). Furthermore, a
significant difference was noted between the CCT of group I and
that of group II (t=5.859, P<0.001).
A statistically significant difference was observed
in the central thickness of the corneal epithelium in group I
compared with that of the control group (49.78±3 μm vs 55.05±2.71
μm, t=8.986, P<0.001). In addition, there was a statistically
significant difference in the central thickness of the corneal
epithelium in group II compared with that of the control group
(51.18±2.22 μm vs 55.05±2.71 μm; t=9.447, P<0.001). Moreover, a
significant difference was observed between the central thickness
of the corneal epithelium of group I and that of group II
(t=−3.683, P=0.001).
Effects of SCLs on CT
The CTs of the control and study groups are
presented in Tables I and II. For the CT in a location with a
radius of 1.0–2.5 or 2.5–3.0 mm from the corneal center, the
minimal CT was observed in the inferior temporal area and the
maximal CT was observed in the superior area (Tables I and II). The CT was decreased in the study
groups. In group II, the CT in the location with a radius of
1.0–2.5 mm from the corneal center was significantly decreased
compared with that obtained prior to discontinuation of SCL wear
(P<0.05). For the CT in a location with a radius of 2.5–3.0 mm
from the corneal center, there was no statistical difference in the
CT in the superior region and the nasal region prior to and
following discontinuation of SCL wear (P>0.05). However,
significant differences were observed in the CT in other regions
(Tables II and III; Figs.
2 and 3).
 | Table IICT in regions with a radius of
1.0–2.5 mm from the corneal center in myopic subjects. |
Table II
CT in regions with a radius of
1.0–2.5 mm from the corneal center in myopic subjects.
| Groups | S (μm) | SN (μm) | N (μm) | IN (μm) | I (μm) | IT (μm) | T (μm) | ST (μm) |
|---|
| Control | 567.60±28.20 | 566.06±28.17 | 555.91±28.36 | 548.26±28.75 | 541.67±29.38 | 538.49±28.89 | 542.59±28.34 | 556.96±28.06 |
| Group I | 560.36±29.13 | 558.04±28.36 | 549.89±26.80 | 543.78±25.91 | 538.70±25.83 | 534.45±26.50 | 537.43±27.60 | 550.86±28.98 |
| Group II |
555.53±27.09ab |
553.28±26.03ab |
543.63±25.11ab |
536.61±24.53ab |
530.39±24.63ab |
526.86±24.90ab |
530.04±26.04ab |
544.68±26.84ab |
 | Table IIICT in regions with a radius of
2.5–3.0 mm from the corneal center in myopic subjects. |
Table III
CT in regions with a radius of
2.5–3.0 mm from the corneal center in myopic subjects.
| Groups | S (μm) | SN (μm) | N (μm) | IN (μm) | I (μm) | IT (μm) | T (μm) | ST (μm) |
|---|
| Control | 600.84±29.49 | 596.00±29.55 | 581.96±29.57 | 572.76±30.22 | 566.50±31.05 | 558.10±30.42 | 560.39±29.38 | 582.50±28.69 |
| Group I |
587.18±31.88a |
579.98±29.03a | 573.73±26.12 | 565.44±26.21 | 561.09±25.41 | 552.05±25.16 | 556.54±27.18 | 576.85±29.91 |
| Group II |
586.51±29.83a |
577.29±28.17a |
569.21±25.46ab |
559.98±24.21ab |
553.94±24.89ab |
545.20±24.77ab |
550.18±26.08ab |
572.94±28.43b |
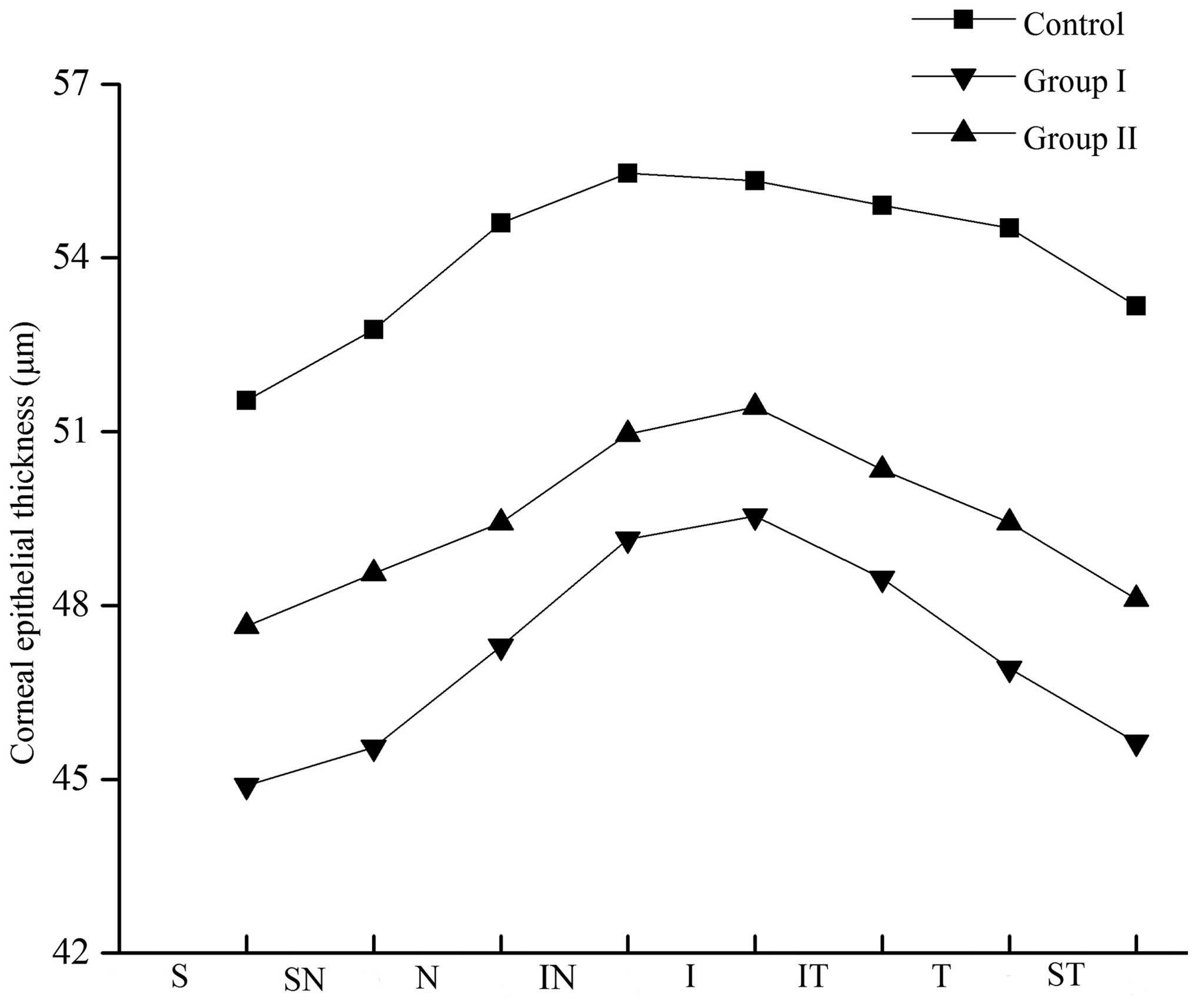
Effects of SCLs on CET
In all corneal regions, the CET at a position with a
radius of 1.0–2.5 mm and 2.5–3.0 mm from the corneal center
indicated that the CET was comparatively thicker in the inferior
section and thinner in the superior section. In the study group,
the CET was decreased in all regions. However, the CET increased
following discontinuation of SCL wear, though the thickness was
unable to return to the normal range. Differences in CET were
statistically significant in these corneal regions (P<0.05;
Tables IV and V; Figs.
4 and 5).
 | Table IVCET in regions with a radius of
1.0–2.5 mm from the corneal center in myopic subjects. |
Table IV
CET in regions with a radius of
1.0–2.5 mm from the corneal center in myopic subjects.
| Groups | S (μm) | SN (μm) | N (μm) | IN (μm) | I (μm) | IT (μm) | T (μm) | ST (μm) |
|---|
| Control | 53.42±2.53 | 53.96±2.46 | 54.83±2.70 | 55.47±2.64 | 55.54±2.74 | 55.19±2.81 | 54.85±2.84 | 54.03±2.63 |
| Group I | 46.68±3.66a | 47.23±3.97a | 48.29±4.20a | 49.75±4.39a | 50.18±4.22a | 49.36±3.99a | 48.18±3.95a | 47.28±3.65a |
| Group II | 48.78±2.33ab | 49.32±2.38ab | 50.32±2.39ab | 51.44±2.59ab | 51.80±2.75ab | 50.98±2.36ab | 50.14±2.35ab | 49.32±2.38ab |
 | Table VCET in regions with a radius of
2.5–3.0 mm from the corneal center in myopic subjects. |
Table V
CET in regions with a radius of
2.5–3.0 mm from the corneal center in myopic subjects.
| Groups | S (μm) | SN (μm) | N (μm) | IN (μm) | I (μm) | IT (μm) | T (μm) | ST (μm) |
|---|
| Control | 51.54±3.12 | 52.76±2.75 | 54.60±2.73 | 55.46±2.61 | 55.33±2.71 | 54.91±2.74 | 54.52±2.69 | 53.17±2.56 |
| Group I | 44.89±3.93a | 45.55±4.25a | 47.30±4.55a | 49.14±4.84a | 49.54±4.24a | 48.47±3.95a | 46.91±4.11a | 45.64±3.67a |
| Group II | 47.64±2.59ab | 48.55±2.62ab | 49.43±2.57ab | 50.96±2.63ab | 51.43±2.93ab | 50.34±2.68ab | 49.43±2.81ab | 48.11±2.42ab |
Discussion
SCLs provide a straightforward option for the
correction of visual acuity whilst maintaining a satisfactory
aesthetic appearance and are therefore popular amongst individuals
with myopia, particularly teenagers (16). Corneal refractive surgery provides
an alternative option for the correction of visual acuity of myopic
patients. According to clinical data, numerous myopia patients with
experience of wearing SCLs have resorted to corneal refractive
surgery to obtain satisfactory visual acuity (17). In order to perform safe and
successful corneal refractive surgery, CT and CET must be
accurately measured so that the appropriate type of surgery can be
selected, cutting parameters can be determined and postoperative
refractive stability and corneal remodeling can be monitored.
Therefore, evaluating the effects of SCLs on CT and CET is
essential in order to guarantee the safety and accuracy of corneal
refractive surgeries.
To date, measurement of CT has largely depended on
ultrasound and optical techniques. For example, the development of
instruments including optical coherence tomography (10,11,18,19),
ultrasonic thickness gauges (13)
and confocal microscopes (14,20)
have contributed to innovations in CT determination.
Anterior segment OCT, a novel technique for
quantitative analysis of ocular parameters, is able to accurately
measure CT and CET and has the advantages of requiring no contact
and being non-invasive as well as simpler to perform. Anterior
segment OCT is divided into time-domain OCT and Fourier-domain OCT
according to the measurement principles utilized.
In the present study, Fourier-domain OCT with a
scanning frequency of 26,000 sweeps/sec was used for the
determination of CT and CET. The axial resolution was elevated to 3
μm. Moreover, CT and CET were automatically calculated by the
installed software, which may have reduced the potential errors
caused by conventional manual software. The CT and CET data were
presented in regions and quadrants.
In a previous study, Hashemi et al (21) determined that the time required to
reach corneal stability following discontinued daily wearing of
SCLs was a two-week contact lens-free period. Nourouzi et al
(22) reported that a 2–15 day
cessation of SCL wear was required to eliminate the corneal edema
associated with SCL wear. Furthermore, a stable CT was achieved in
74% of patients within one week, and in a further 26% of patients
during the second week. The present study hypothesized that a
stable CT was achieved within two weeks of discontinued SCL wear,
however, individual variation could not be excluded.
Corneal oxygen uptake has a crucial role in the
energy metabolism and maintenance of transparency of the cornea
(23,24). Corneal oxygen uptake is mainly
dependent upon the exchange with the outside air or blood vessels
located in the palpebral conjunctiva (23,25,26).
Under normal conditions, corneal oxygen uptake is obstructed by
eye-closing in the evening, which induces a disorder of the
sodium-potassium pump and leads to corneal edema (27). On this basis, corneal edema occurs
with a rate of 5–6% (27);
however, is completely reversed in the waking state as sufficient
oxygen is obtained (25,26).
Corneal oxygen uptake is obstructed due to SCL wear
when eyes are open or closed (28). This disruption of corneal oxygen
supply may lead to physiological metabolic disorders, including
corneal edema and increased corneal thickness. In the present
study, the CT in group II was thicker than that of group I
(P<0.05), which confirmed the presence of corneal edema during
long-term SCL wear. In addition, the thickness of the corneal
epithelium in group II was greater than that of group I, which
demonstrated that the chronic corneal edema induced by SCL wear
occurred mainly in the corneal stroma.
A study reported a significant decrease in the CET
of individuals with long-term or occasional SCL wear compared with
that of control subjects (18). In
a retrospective analysis, pachymetry measurement was performed in
order to compare the CT of spectacle-wearing control eyes with
those of SCL wearers and rigid gas-permeable contact lens wearers
(29). It was concluded that there
was a significant reduction in the CT of full-time contact
lens-wearing subjects. In the present study, a clear decrease was
observed in the CT of subjects in group II compared with that of
subjects in the control group and group I. These results appear to
confirm that the CT was decreased following long-term SCL wear.
Taking the CT in these groups into consideration, it was concluded
that decreased CT and concurrent edema were identified in myopic
subjects following long-term SCL wear.
The potential mechanisms of corneal edema and
thinning are varied. For example, Wang et al (30) reported an increased CT in subjects
with short-term SCL wear, using the OCT technique, and thus
demonstrated the presence of corneal edema. Furthermore, chronic
corneal edema was frequently identified in long-term SCL wearing
subjects, which led to biochemical changes in the corneal stroma
and a significant reduction in the CT (31.32). It has additionally
been reported that enhanced tear osmotic pressure was present in
SCL wearers, leading to thinning of the whole cornea (33). A further potential mechanism is
that long-term SCL wear may induce reversible corneal epithelial
compression, necrosis and collapse of the corneal epithelium, or
cell apoptosis of the corneal stroma (3). In subjects with long-term and/or
prolonged SCL wear, several factors have been reported to be
associated with the cellular apoptosis of cornea and CT reduction,
including changes in the microenvironment of the ocular surface,
chronic microlesion in the corneal tissues and chronic hypoxia
(34).
Extensive studies have focused on the measurement of
CT, and in particular CCT; however, it is necessary to measure the
CET of various regions for the accurate analysis of CET
distribution (35,36). To date, the thickness evaluation
has been performed in the peripheral region of the corneal
epithelium and the majority of the data were obtained from the
inferior and/or superior region of the cornea (2,10,22,29).
A previous study aimed to measure the CET in the vertical and
horizontal meridians of the cornea and demonstrated that the
corneal epithelial thinning was topographically uniform (19,37).
By contrast, Simon et al (38) suggested that no layer of uniform
thickness was formed by the corneal epithelium over Bowman’s layer.
Furthermore, the changes of the CET distribution mainly resulted
from the verified corneal surface power, and the orientation of the
astigmatism axis. Using the RTVue-100 system, the results of the
present study indicated that the CET was not evenly distributed, as
the CET in the inferior cornea was comparatively thicker than that
of the superior cornea.
A previous study indicated a 6% decrease in the CET
of subjects with long-term SCL wear (39). Consistent with the results by
Liesegang (39), the CET obtained
in group I was markedly thinner than that in the control group. It
was hypothesized that the CET reduction observed may be associated
with corneal epithelial microlesions caused by mechanical
irritation of the epithelial surface during long-term SCL wear
(40–42). Amongst SCL wearers, dissection and
denaturation of corneal epithelial cells were observed using
scanning electron microscopy. Simultaneously, a mild separation was
noticed in the intercellular space of the corneal epithelial cells
observed through a transmission electron microscope. In the
presence of corneal epithelial microlesion, permeability of corneal
epithelial cells was increased as a result of decreased corneal ion
pump function, which resulted in dehydrolysis. Therefore, chronic
hypoxia has a marked influence on physiological function (40).
In the present study, a significant increase in CET
was demonstrated in group II compared with that of group I
(P<0.05). It was hypothesized that this was mainly due to the
regeneration of the corneal epithelium. Following discontinuation
of SCL wear, the associated hypoxia and mechanical irritation were
eliminated and therefore, partial self-repair and reproduction may
be induced in the corneal epithelium.
In the present study, the changes in CT and CET were
analyzed in long-term SCL-wearing subjects. The results of the
present study demonstrated edema and thinning of the corneal stroma
in myopia long-term SCL-wearing subjects. Furthermore, thinning of
the corneal epithelium was noted in these subjects.
In conclusion, based on the results of the present
study it was proposed that in clinical practices, for myopic
patients with long-term SCL wear, determination of CT and CET
should be performed two weeks following discontinuation of SCL
wear, once a stable CT and CET are obtained. On this basis,
surgical strategy may be reliably established. Greater attention
should be paid to patients with reduced CT, irregular cornea, and
severe astigmatism, as well as those with corneal ectasia or
keratoconus to avoid postoperative secondary keratoconus.
References
|
1
|
Reinstein DZ, Srivannaboon S, Archer TJ,
Silverman RH, Sutton H and Coleman DJ: Probability model of the
inaccuracy of residual stromal thickness prediction to reduce the
risk of ectasia after LASIK part I: quantifying individual risk. J
Refract Surg. 22:851–860. 2006.PubMed/NCBI
|
|
2
|
Walline JJ, Gaume A, Jones LA, Rah MJ,
Manny RE, Berntsen DA, Chitkara M, Kim A and Quinn N: Benefits of
contact lens wear for children and teens. Eye Contact Lens.
33:317–321. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liu Z and Pflugfelder SC: The effects of
long-term contact lens wear on corneal thickness, curvature, and
surface regularity. Ophthalmology. 107:105–111. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bonanno JA and Polse KA: Central and
peripheral corneal swelling accompanying soft lens extended wear.
Am J Optom Physiol Opt. 62:74–81. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fujimoto JG, Pitris C, Boppart SA and
Brezinski ME: Optical coherence tomography: an emerging technology
for biomedical imaging and optical biopsy. Neoplasia. 2:9–25. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stillitano I, Yamazaki E, Melo LA Jr,
Bottos J and Campos M: Wavefront-guided refractive surgery results
of training-surgeons. Arq Bras Oftalmol. 73:323–328. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sia RK, Coe CD, Edwards JD, Ryan DS and
Bower KS: Visual outcomes after Epi-LASIK and PRK for low and
moderate myopia. J Refract Surg. 28:65–71. 2012. View Article : Google Scholar
|
|
8
|
Bergmanson JP: Histopathological analysis
of the corneal epithelium after contact lens wear. J Am Optom
Assoc. 58:812–818. 1987.PubMed/NCBI
|
|
9
|
Lu L, Reinach PS and Kao WW: Corneal
epithelial wound healing. Exp Biol Med (Maywood). 226:653–664.
2001.
|
|
10
|
Li Y, Tan O, Brass R, Weiss JL and Huang
D: Corneal epithelial thickness mapping by Fourier-domain optical
coherence tomography in normal and keratoconic eyes. Ophthalmology.
119:2425–2433. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Haque S, Jones L and Simpson T: Thickness
mapping of the cornea and epithelium using optical coherence
tomography. Optom Vis Sci. 85:E963–E976. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huang D, Tang M and Shekhar R:
Mathematical model of corneal surface smoothing after laser
refractive surgery. Am J Ophthalmol. 135:267–278. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Reinstein DZ, Archer TJ, Gobbe M,
Silverman RH and Coleman DJ: Epithelial thickness in the normal
cornea: three-dimensional display with Artemis very high-frequency
digital ultrasound. J Refract Surg. 24:571–581. 2008.PubMed/NCBI
|
|
14
|
Li HF, Petroll WM, Møller-Pedersen T,
Maurer JK, Cavanagh HD and Jester JV: Epithelial and corneal
thickness measurements by in vivo confocal microscopy through
focusing (CMTF). Curr Eye Res. 16:214–221. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ramos JL, Li Y and Huang D: Clinical and
research applications of anterior segment optical coherence
tomography - a review. Clin Experiment Ophthalmol. 37:81–89. 2009.
View Article : Google Scholar :
|
|
16
|
Ehsaei A, Chisholm CM, MacIsaac JC, Mallen
EA and Pacey IE: Central and peripheral visual performance in
myopes: contact lenses versus spectacles. Cont Lens Anterior Eye.
34:128–132. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lim L and Wei RH: Laser in situ
keratomileusis treatment for myopia in a patient with partial
limbal stem cell deficiency. Eye Contact Lens. 31:67–69. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feng Y and Simpson TL: Comparison of human
central cornea and limbus in vivo using optical coherence
tomography. Optom Vis Sci. 82:416–419. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang J, Fonn D, Simpson TL, Sorbara L,
Kort R and Jones L: Topographical thickness of the epithelium and
total cornea after overnight wear of reverse-geometry rigid contact
lenses for myopia reduction. Invest Ophthalmol Vis Sci.
44:4742–4746. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Patel SV, McLaren JW, Hodge DO and Bourne
WM: Confocal microscopy in vivo in corneas of long-term contact
lens wearers. Invest Ophthalmol Vis Sci. 43:995–1003.
2002.PubMed/NCBI
|
|
21
|
Hashemi H, Firoozabadi MR, Mehravaran S
and Gorouhi F: Corneal stability after discontinued soft contact
lens wear. Cont Lens Anterior Eye. 31:122–125. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nourouzi H, Rajavi J and Okhovatpour MA:
Time to resolution of corneal edema after long-term contact lens
wear. Am J Ophthalmol. 142:671–673. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen Y, Thompson DC, Koppaka V, Jester JV
and Vasiliou V: Ocular aldehyde dehydrogenases: protection against
ultraviolet damage and maintenance of transparency for vision. Prog
Retin Eye Res. 33:28–39. 2013. View Article : Google Scholar :
|
|
24
|
Thiel HJ: Epithelium of the cornea and its
significance for transparency. Dtsch Med Wochenschr. 99:1630–1635.
1974.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Takatori SC, de la Jara PL, Holden B,
Ehrmann K, Ho A and Radke CJ: In vivo oxygen uptake into the human
cornea. Invest Ophthalmol Vis Sci. 53:6331–6337. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Weissman BA, Fatt I and Rasson J:
Diffusion of oxygen in human corneas in vivo. Invest Ophthalmol Vis
Sci. 20:123–125. 1981.PubMed/NCBI
|
|
27
|
Efron N and Carney LG: Oxygen levels
beneath the closed eyelid. Invest Ophthalmol Vis Sci. 18:93–95.
1979.PubMed/NCBI
|
|
28
|
Ichijima H, Hayashi T, Mitsunaga S and
Hamano H: Determination of oxygen tension on rabbit corneas under
contact lenses. CLAO J. 24:220–226. 1998.PubMed/NCBI
|
|
29
|
Braun DA and Anderson Penno EE: Effect of
contact lens wear on central corneal thickness measurements. J
Cataract Refract Surg. 29:1319–1322. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang J, Fonn D, Simpson TL and Jones L:
The measurement of corneal epithelial thickness in response to
hypoxia using optical coherence tomography. Am J Ophthalmol.
133:315–319. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hutchings N, Simpson TL, Hyun C, Moayed
AA, Hariri S, Sorbara L and Bizheva K: Swelling of the human cornea
revealed by high-speed, ultrahigh-resolution optical coherence
tomography. Invest Ophthalmol Vis Sci. 51:4579–4584. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Efron N, Perez-Gomez I and Morgan PB:
Confocal microscopic observations of stromal keratocytes during
extended contact lens wear. Clin Exp Optom. 85:156–160. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cerretani C, Peng CC, Chauhan A and Radke
CJ: Aqueous salt transport through soft contact lenses: an
osmotic-withdrawal mechanism for prevention of adherence. Cont Lens
Anterior Eye. 35:260–265. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
McMonnies CW, Chapman-Davies A and Holden
BA: The vascular response to contact lens wear. Am J Optom Physiol
Opt. 59:795–799. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kanellopoulos AJ and Asimellis G: Anterior
segment optical coherence tomography: assisted topographic corneal
epithelial thickness distribution imaging of a keratoconus patient.
Case Rep Ophthalmol. 4:74–78. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhou W and Stojanovic A: Comparison of
corneal epithelial and stromal thickness distributions between eyes
with keratoconus and healthy eyes with corneal astigmatism ≥ 2.0 D.
PLoS One. 9:e859942014. View Article : Google Scholar
|
|
37
|
Pérez JG, Méijome JM, Jalbert I, Sweeney
DF and Erickson P: Corneal epithelial thinning profile induced by
long-term wear of hydrogel lenses. Cornea. 22:304–307. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Simon G, Ren Q, Kervick GN and Parel JM:
Optics of the corneal epithelium. Refract Corneal Surg. 9:42–50.
1993.PubMed/NCBI
|
|
39
|
Liesegang TJ: Physiologic changes of the
cornea with contact lens wear. CLAO J. 28:12–27. 2002.PubMed/NCBI
|
|
40
|
Pearlman E, Sun Y, Roy S, Karmakar M, Hise
AG, Szczotka-Flynn L, Ghannoum M, Chinnery HR, McMenamin PG and
Rietsch A: Host defense at the ocular surface. Int Rev Immunol.
32:4–18. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Markoulli M, Papas E, Cole N and Holden B:
Corneal erosions in contact lens wear. Cont Lens Anterior Eye.
35:2–8. 2012. View Article : Google Scholar
|
|
42
|
Brewitt H: Contact lenses. 2: Contact lens
associated infections. Klin Monbl Augenheilkd. 211:aA7–A10.
1997.(In German). PubMed/NCBI
|