Introduction
Alendronate (Ald), is a molecule belonging to the
amino-bisphosphonate family and is commonly used in the clinical
treatment of osteoporosis and other bone disorders, including
Paget's disease (1,2). Ald acts by reducing the resorptive
activity and inducing accelerated programmed cell death of
osteoclasts. Besides the well-known antibone resorption activity,
the side effects of aminobisphosphonates have been investigated
previously and contrasting findings report their pro-inflammatory
effects, renal toxicity and adverse reaction in the upper
gastrointestinal tract of patients and animal models, although with
certain differences depending on the compound and the type of
administration (3–6).
These effects are caused, at a molecular level, by
the inhibition of the farnesyl pyrophosphate synthase enzyme in the
mevalonate pathway. The decreased number of prenylated GTP-binding
proteins anchored to the membrane of osteoclasts (7,8) may
induce apoptosis and therefore, reduce bone resorption.
Malfunctions in the post-translational modification
known as prenylation and the overproduction of several
pro-inflammatory cytokines, including IL-1β, are also suggested to
be at the basis of Mevalonate Kinase Deficiency (MKD) (9). MKD is an autosomal
recessively-inherited disease (OMIM #610377) caused by mutations in
the MVK gene (12q24.11), which encodes the enzyme,
mevalonate kinase (MK) in the mevalonate pathway (Fig. 1) (10–13).
Our previous studies developed cellular and animal
models of MKD obtained following administration of the
aminobisphosphonate, Ald or lovastatin (Lova). These inhibit the
mevalonate pathway and allow partial reproduction of the
biochemical defect characterizing patients with MKD (14,15).
However, Cantarini et al (16) described a case report in which Ald
was administered to a patient with MKD to prevent skeletal and bone
fractures and this treatment markedly rescued the inflammatory
symptoms and led to a disease remission period of several months
(16). The positive effects of Ald
suggested that this may be used as a potential therapeutic drug for
MKD and not exclusively for bone disorders (16). However, this raises the issue of
the apparently opposite roles of Ald in MKD. This
aminobisphosphonate appears to exhibit contrasting effects, while
having been reported to improve the clinical features of one
patient, it has been extensively used to inhibit the mevalonate
pathway in vivo and in vitro (14,15).
The intriguing observation that Ald antagonizes the
pro-inflammatory effects of the inhibited mevalonate pathway,
prompted the present study to re-assess the activity of this
compound, using an MKD cellular model (murine Raw 264.7
monocyte-macrophage cell line) and monocytes isolated from two
patients with MKD.
Additionally, to avoid compound-dependent results
and dissipate any question or controversy of the findings obtained,
the pathway was inhibited using two different compounds, Ald and
Lova. Once the pathway was inhibited, the acute phase was mimicked
by administering a pro-inflammatory stimulus, lipopolysaccharide
(LPS), shortly followed by the therapeutic administration of Ald.
The analysis of four pro-inflammatory cytokines, interleukin
(IL)-1α, IL-1β, IL-6 and tumor necrosis factor (TNF)-α, and
programmed cell death (PCD), was used to assess the potential
anti-inflammatory effects of Ald on these cell models of MKD.
Materials and methods
Chemicals
Unless otherwise stated, the reagents were purchased
from Sigma-Aldrich (Milan, Italy). LPS (E. coli serotype
055:B5; 1 mg/ml stock in H2O), Ald (30 mM) and Lova (50
mM) were dissolved in saline solution (Diaco SpA, Trieste,
Italy).
Cell culture
The raw 264.7 cells (murine monocyte/macrophage cell
line; Sigma-Aldrich) were cultured at 2.5×105 cells/ml
in Dulbecco's modified Eagle's medium, supplemented with 10% fetal
bovine serum (FBS; Euroclone Spa, Milan, Italy) and 100 µM
Ald or 20 µM Lova for 20 h at 37°C in a 5% CO2
incubator. Following incubation, 10 µg/ml LPS was added for
an additional 24 h. Where appropriate, Ald was added at three
different concentrations (25, 50 or 100 µM) together with
LPS in order to analyze its potential anti-inflammatory
properties.
Two patients with MKD were diagnosed during the
first year of life and followed-up at the Institute for Maternal
and Child Health, IRCCS 'Burlo Garofolo', Trieste, Italy. The MKD
diagnosis was confirmed by genetic analysis (Table I). These two patients were
recruited to the present study at the age of 24 and 13. They had no
recurrent infections and were not in the acute phase of the disease
at the time of enrollment. The present study was approved by the
ethical and scientific review board of the Institute for Maternal
and Child Health, IRCCS 'Burlo Garofolo' (no. 185/8; 19/08/2008).
For a child to be eligible, informed consent had to be obtained
from the parents or caregivers. Monocytes were isolated from the
two patients with MKD by selection with monoclonal CD14 antibody
(mouse IgG2a)-conjugated microbeads (Miltenyi Biotec, Bergisch
Gladbach, Germany), performed with manual columns, according to the
manufacturer's instructions. The cells were subsequently cultured
at 2.5×105 cells/ml in RPMI-1640 medium, containing 10%
FBS (Euroclone Spa) and 1 µg/ml LPS for 24 h. As for the Raw
264.7 cells, 50 µM Ald was added together with LPS, where
appropriate
 | Table IMVK gene mutations. |
Table I
MVK gene mutations.
| Patient | Mutation |
|---|
| 1 | S135L/V377I |
| 2 | V377I/I268T |
At the end of the incubation periods, the
supernatant was collected for the cytokine assay and the cells were
pelleted for the PCD assay.
PCD assay
The PCD of the Raw 264.7 cells and the patient
isolated monocytes were monitored by flow cytometry using double
staining with Annexin V-fluorescein isothiocyanate and propidium
iodide (PI; Apoptosis Detection kit; Immunostep, Salamanca, Spain),
according to the manufacturer's instructions. The fluorescence was
measured with a Cyan ADP cytometer and Summit version 4.3 software
(Beckman Coulter, Fort Collins, CO, USA), and was subsequently
analyzed with FlowJo 7.6 software (TreeStar Inc., Ashland, OR,
USA). This technique was used to assess the effect of the
treatments on cell viability. Debris were excluded from the plot
based on the scatter (FSC vs. SSC) and the apoptotic (Annexin V
positive, A+; PI negative, PI− and positive,
PI+) and the necrotic (A− and PI+)
cells were characterized based on the fluorescence emitted.
Cytokine production assay
The analysis of four pro-inflammatory cytokines,
IL-1α, IL-1β, IL-6 and TNF-α, was performed on culture medium from
the Raw 264.7 cells and the patient isolated monocytes, using
magnetic bead-based multiplex immunoassays (Bio-Plex; Bio-Rad
Laboratories, Milano, Italy), according to the manufacturer's
instructions. The data from the reactions were acquired using the
Bio-Plex 200 reader, a digital processor managed the data output
and Bio-Plex Manager 6.0 software (Bio-Rad) presented data as the
Median Fluorescence Intensity and concentration (pg/ml).
Statistical analysis
The statistical significance was calculated using
one-way analysis of variance and Bonferroni post-hoc test
correction in the case of multiple comparisons, using GraphPad
Prism v5.0 software (GraphPad Software Inc., La Jolla, CA). The
data are expressed as the mean ± standard deviation. P<0.05 was
considered to indicate a statistically significant difference.
Results
PCD
The Raw 264.7 cells demonstrated a statistically
significant increase in PCD following the addition of a specific
inhibitor (Ald or Lova) in addition to LPS. The Ald + LPS-treated
or Lova + LPS-treated cells produced comparable results
demonstrating that PCD was independent of the compound used to
inhibit the pathway (Fig. 2A).
Additionally, the production of the pro-inflammatory cytokines,
IL-1α, IL-1β, IL-6 and TNF-α, was not normalized by the presence of
Ald, regardless of which inhibitor was previously used (Fig. 2B).
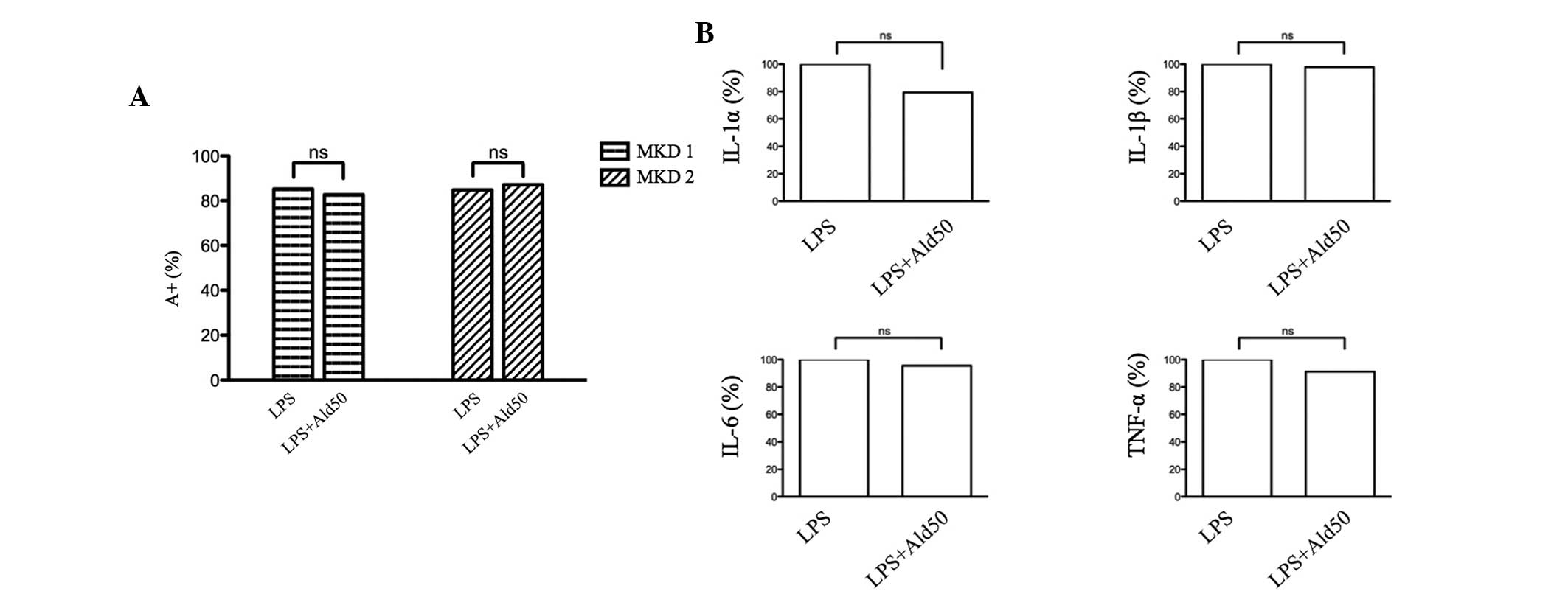
 | Figure 2Raw 264.7 cells were incubated with
100 µM Ald (left, grey) or 20 µM Lova (right, black)
and subsequently with 10 µg/ml LPS and Ald (25, 50 or 100
µM). (A) The percentage of apoptotic cells was detected by
positive Annexin V staining (A+) and the data are
expressed as the mean ± standard deviation (B) The levels of IL-1α,
IL-1β, IL-6 and TNF-α in the supernatant was assessed. The data are
demonstrated as the percentage of levels compared to the standard
value (100%). One-way analysis of variance and Bonferroni post-hoc
test was performed for three independent experiments
(*P<0.05, **P<0.01 and
***P<0.001, compared with the untreated group). Ald,
alendronate; Lova, lovastatin; LPS, lipopolysaccharide; ns, not
significant. |
Anti-inflammatory effect of Ald
In order to establish the potential
anti-inflammatory effect of Ald, the drug was assessed at different
concentrations (25, 50 and 100 µM) in the murine cellular
model. No affect was observed at any concentration with regards to
the decrease of PCD or the secretion of pro-inflammatory cytokines
(Fig. 2A and B).
Therapeutic activity of Ald
The effects of Ald on monocytes isolated from two
different patients with MKD (Table
I) were assessed. Following the addition of the
pro-inflammatory stimulus, LPS, the potential therapeutic activity
of Ald was assessed. As previously observed in the murine cell
line, Ald revealed no improvement in the PCD in the monocytes from
the patients with MKD, however, increased the percentage of
apoptotic cells (Fig. 3A).
Cytokine levels
The production levels of the cytokines IL-1α, IL-1β,
IL-6 and TNF-α were determined in the supernatant of the monocytes
from the patients. The sensitivity of the specific human kit and
their ranges were as follows: IL-1α (1.4-22569 pg/ml), IL-1β
(3.2-3261 pg/ml), IL-6 (2.3-28880 pg/ml) and TNF-α (5.8-95484
pg/ml). The results were in the range of the limits of
quantification and therefore, the data obtained demonstrated the
inefficacy of Ald treatments in decreasing inflammation (P>0.05)
(Fig. 3B).
Discussion
Despite the positive result described by Cantarini
et al (16) in their case
study, the present study failed to reproduce the anti-inflammatory
effects of Ald in vitro, using a murine cell line or
monocytes isolated from two patients with MKD. By contrast,
treatment with Ald continued to be associated with increased levels
of PCD and the production of inflammatory cytokines, suggesting the
lack of anti-inflammatory activity for this compound, at least
in vitro. A possible explanation for these contrasting
findings may reside in the different backgrounds of the MVK gene.
Indeed, the patient described by Cantarini et al and the two
patients in the present study carry different mutations, the first
being homozygous for V377I (16)
and the latter being compound heterozygous (S135L/V377I and
I268T/V377I).
In addition, patients with MKD exhibit a
heterogeneous clinical phenotype, characterized by recurrent
episodes of fever, irritability, lymphadenopathy, abdominal pain,
diarrhoea and skin rash, which differs in terms of intensity and
frequency from one patient to the other. Additionally, patients
with MKD also exhibit marked variability in the response to
therapies (statins and biological drugs) designed to rescue the
inflammatory phenotype (17–19).
According to Hoffmann et al (20), it is inappropriate to administer
statins and/or aminobisphosphonate to patients with MKD exhibiting
a genetically determined inhibited mevalonate pathway. However, the
same author, reported discordant effects following the
administration of statins. Indeed, certain patients with MKD
exhibited an improvement of the clinical features, while other
patients exhibited detrimental effects, including a marked increase
of febrile attacks (20).
Despite isolated cases in which a variety of
compounds have been demonstrated to improve the symptoms exhibited
by patients, MKD still lacks standardized and targeted therapies
and remains a neglected and disease, without a recommended
therapeutic agent. Since our previous study reported an in
vitro model useful to assess aminobisphosphonates, it was
suggested to physicians to perform in vitro assays on
monocytes isolated from patients with MKD. Therefore, a preliminary
evaluation of the proper anti-inflammatory action of treatments may
be obtained prior to treating patients themselves.
Being aware of all the limitations represented by
cell models, in which the mevalonate pathway has been biochemically
inhibited, the present study suggested that the in vitro
model may contribute to identifying a common therapeutic strategy
for patients with MKD.
Acknowledgments
This study was supported by a grant from the
Institute for Maternal and Child Health, IRCCS 'Burlo Garofolo'
(grant no. RC 42/11).
References
|
1
|
Maeda SS and Lazaretti-Castro M: An
overview on the treatment of postmenopausal osteoporosis. Arq Bras
Endocrinol Metabol. 58:162–171. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Silverman SL: Paget disease of bone:
therapeutic options. J Clin Rheumatol. 14:299–305. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sugawara S, Shibazaki M, Takada H, Kosugi
H and Endo Y: Contrasting effects of an aminobisphosphonate, a
potent inhibitor of bone resorption, on lipopolysaccharide-induced
production of interleukin-1 and tumour necrosis factor alpha in
mice. Br J Pharmacol. 125:735–740. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Amagase K, Inaba A, Senta T, et al:
Gastric ulcerogenic and healing impairment effects of risedronate,
a nitrogen-containing bisphosphonate in rats. Comparison with
alendronate and minodronate. J Physiol Pharmacol. 62:609–618.
2011.
|
|
5
|
Richards PJ, Amos N, Williams AS and
Williams BD: Pro-inflammatory effects of the aminobisphosphonate
ibandronate in vitro and in vivo. Rheumatology (Oxford).
38:984–991. 1999. View Article : Google Scholar
|
|
6
|
Diel IJ, Bergner R and Grötz KA: Adverse
effects of bisphosphonates: current issues. J Support Oncol.
5:475–482. 2007.
|
|
7
|
Watts NB and Diab DL: Long-term use of
bisphosphonates in osteoporosis. J Clin Endocrinol Metab.
95:1555–1565. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fleisch H: Bisphosphonates: mechanisms of
action. Endocr Rev. 19:80–100. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Frenkel J, Rijkers GT, Mandey SH, et al:
Lack of isoprenoid products raises ex vivo interleukin-1beta
secretion in hyperimmunoglobulinemia D and periodic fever syndrome.
Arthritis Rheum. 46:2794–2803. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Goldstein JL and Brown MS: Regulation of
the mevalonate pathway. Nature. 343:425–430. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Drenth JP, van Deuren M, van der
Ven-Jongekrijg J, Schalkwijk CG and van der Meer JW: Cytokine
activation during attacks of the hyperimmunoglobulinemia D and
periodic fever syndrome. Blood. 85:3586–3593. 1995.PubMed/NCBI
|
|
12
|
Haas D and Hoffmann GF: Mevalonate kinase
deficiencies: from mevalonic aciduria to hyperimmunoglobulinemia D
syndrome. Orphanet J Rare Dis. 1:132006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mandey SH, Kuijk LM, Frenkel J and
Waterham HR: A role for geranylgeranylation in interleukin-1beta
secretion. Arthritis Rheum. 54:3690–3695. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Marcuzzi A, Piscianz E, Kleiner G, et al:
Clinical genetic testing of periodic Fever syndromes. Biomed Res
Int. 2013:5013052013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tricarico PM, Marcuzzi A, Piscianz E, et
al: Mevalonate kinase deficiency and neuroinflammation: balance
between apoptosis and pyroptosis. Int J Mol Sci. 14:23274–23288.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cantarini L, Vitale A, Magnotti F, et al:
Weekly oral alendronate in mevalonate kinase deficiency. Orphanet J
Rare Dis. 8:1962013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Attout H, Guez S, Ranaivo I, Jameerbaccus
N and Series C: A patient with hyper-IgD syndrome responding to
simvastatin treatment. Eur J Intern Med. 19:e82–e83. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Simon A, Drewe E, van der Meer JW, et al:
Simvastatin treatment for inflammatory attacks of the
hyperimmunoglobulinemia D and periodic fever syndrome. Clin
Pharmacol Ther. 75:476–483. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van der Hilst JC, Bodar EJ, Barron KS, et
al: Long-term follow-up, clinical features and quality of life in a
series of 103 patients with hyperimmunoglobulinemia D syndrome.
Medicine (Baltimore). 87:301–310. 2008. View Article : Google Scholar
|
|
20
|
Hoffmann GF, Charpentier C, Mayatepek E,
et al: Clinical and biochemical phenotype in 11 patients with
mevalonic aciduria. Pediatrics. 91:915–921. 1993.PubMed/NCBI
|