Introduction
Vascular dementia (VaD) is the second most common
type of dementia after Alzheimer's disease (AD) among the elderly,
accounting for approximately a quarter of all cases of dementia in
developed countries (1). The
disease is characterized by a progressive impairment of memory,
which severally interferes with the life quality of the patients
and their families when the loss develops to a certain degree
(2). At present, VaD has become a
major public problem and a challenging clinical one (3) with a marked increase among the
elderly population in spite of limited success in the improvement
of memory impairment.
VaD is considered to be caused by a variety of
cerebral vascular diseases, including cerebral infarction and
cerebral hemorrhage due to vascular lesions which restrict blood
supply and damage the brain regions being important for memory,
cognition and behavior (4,5). Although the exact pathogenesis has
not yet been fully elucidated, it is now apparent that cerebral
hypoperfusion is a main underlying mechanism for VaD.
Ischemia/reperfusion leads to energy metabolic dysfunction and
oxidant stress, thus triggering cell apoptosis and subsequent
impairment of the brain, including the hippocampus, which has a key
role in the regulation of memory function (6,7).
Apoptosis is an active process of cell death which occurs in
numerous important physiological and pathophysiological conditions.
Following ischemia/reperfusion, the expression of
apoptosis-associated proteins, including B-cell lymphoma 2 (Bcl-2),
Bcl-2-associated X protein (Bax) and P53, are altered, which
triggers and deteriorates apoptosis (8,9).
Therefore, inhibiting apoptosis is a feasible strategy for the
treatment of VaD.
Furthermore, accumulating evidence indicated that
the cyclic adenosine monophosphate (cAMP)/protein kinase A
(PKA)/cAMP-responsive element binding protein (CREB) signal
transduction system has a close association with learning and
memory function in mammals (10–12).
cAMP is a ubiquitous secondary messenger that is strongly
associated with hippocampal synaptic plasticity and memory
(13). Elevated cytoplasmic cAMP
promotes the activity of PKA, and PKA subsequently phosphorylates
and activates CREB (12,14). Activated CREB consequently binds to
the cAMP response element (CRE) of target genes, thus regulating
memory, particularly long-term memory formation (10). Injection of cAMP into the lateral
ventricle was shown to ameliorate experimental amnesia in mice
(13), while PKA inhibitors
impaired long-term memory formation in day-old chicks (14). Moreover, intra-hippocampal infusion
of CREB antisense oligonucleotides significantly impaired long-term
memory in rats (15). In rats with
microsphere embolism-induced cerebral ischemia and memory defects,
the activity of cAMP/PKA/CREB was significantly decreased in the
hippocampus, as indicated by decreased cAMP content, PKA levels and
CREB phosphorylation, while enhancement of the activity of this
signaling pathway improved the memory function in rats (16,17).
In China, herbal medicines have been widely used to
treat dementia for hundreds of years, and are believed to achieve
beneficial outcomes; however, scientific evidence for their potency
is currently lacking. Recently, Yifei Xuanfei Jiangzhuo formula
(YXJF), a Chinese herbal decoction composed of nine Chinese herbs
based on the differentiation of symptoms embodying the theory of
Traditional Chinese Medicine, is used to treat VaD. A previous
study by our group reported that the memory as well as life quality
of patients with VaD were significantly improved after YXJF
treatment (18), suggesting that
YXJF is likely to be suitable for VaD treatment. However, the
underlying mechanisms have yet to be fully elucidated. The present
study aimed to investigate the effects of YXJF on memory impairment
in a rat model of cerebral ischemia/reperfusion-induced VaD and to
explore the underlying mechanisms, including anti-apoptotic effects
and enhancement of cAMP/PKA/CREB signal transduction, which
provided convincing evidence for the clinical efficacy of YXJF.
Materials and methods
Materials and reagents
Huperzine A was purchased from Shanghai Fudan
Forward Pharmaceutical Co., Ltd. (Shanghai, China). Piracetam was
obtained from Northeast General Pharmaceutical Factory (Shenyang,
China). The In situ Cell Death Detection kit, peroxidase was
from Roche (Basel, Switzerland). Protein lysis buffer for western
blot was provided by Solarbio Science & Technology Co., Ltd.
(Beijing, China). Antibodies directed to Bax (rabbit anti-rat; cat.
no. 2772S; 1:800), c-Jun (mouse anti-rat; cat. no. 2315S; 1:500),
Bcl-2 (rabbit anti-rat; cat. no. 2876S; 1:1,000), PKA C-α (rabbit
anti-rat; cat. no. 4782S; 1:600), CREB (rabbit anti-rat; cat. no.
4820; 1:800), and phosphorylated CREB (p-CREB; rabbit anti-rat;
cat. no. 4276; 1:500) were all from Cell Signaling Technology
(Danvers, MA, USA). An antibody against β-actin (mouse anti-rat;
cat. no. TA-09; 1:1,000) and secondary antibodies against
peroxidase-conjugated goat anti-mouse IgG (cat. no. ZB-2305;
1:3,000) and peroxidase-conjugated goat anti-rabbit IgG (cat. no.
ZB-2301; 1:3,000) were obtained from Zhongshan Jinqiao
Biotechnology Co., Ltd. (Beijing, China). Notoginsenoside R1,
astragaloside IV, amygdalin, platycodin D and ginsenoside Rg1 were
purchased from Chengdu Must Biotechnology Co., Ltd. (Chengdu,
China). Ginsenoside Rb1 was from National Institutes for Food and
Drug Control (Beijing, China).
Preparation of the decoction
YXJF, the Chinese herbal decoction, was produced by
extraction of the following nine Chinese herbs: The tuberous root
of Platycodon gradiflorus (Jacq.) A. DC.
(Campanulaceae), the seed of Prunus armeniacae L.
(Rosaceae), the rhizome of Panax ginseng C. A. Mey.
(Araliaceae), the tuberous root of Ophiopogon
japonicas (L. f) Ker-Gawl. (Liliaceae), the root of
Astragalus membranaceus (Fisch.) Bge. var. mongholicus
(Bge.) Hsiao (Leguminosae), the rhizome of Panax
notoginseng (Burk.) F. H. Chen (Araliaceae), the dried
fruit of Perilla frutescens (L.) Britt. (Labiatae),
the rhizome of Acorus tatarinowii Schott (Araceae),
and the rhizome (stir-fried with wine) of Rheum palmatum L.
(Polygonaceae). The herbs were purchased from Jiangyin
Tianjiang Pharmaceutical Co., Ltd. (Jiangyin, China), and the
voucher specimens were deposited at the First Affiliated Hospital,
Guangxi University of Chinese Medicine (Nanning, China). All herbs
were authenticated by Professor Lin Wu. The processed herbs were
normatively prepared following the Good Manufacturing Practice
specific to Chinese Herbal Medicine (19). In the decoction using water as a
solvent, the percent ratios based on weight of the nine herbs were
8.62, 8.62, 12.93, 12.93, 12.93, 12.93, 12.93, 12.93 and 5.18,
respectively. The concentration of the herbs in the formula was
3.39 g/ml, and the decoction was kept in the fridge at 4°C. The
decoction was warmed in water at 37°C for 10 min prior to its
administration to the rats. High performance liquid chromatography
(HPLC; Milford, MA, USA), including Binary HPLC Pump 1525, a
Photodiode Array Detector 2998 and a SunFire™ C18 column
(4.6 mm × 250 mm; 5 µm) was employed to analyze the chemical
profile of the decoction. The mobile phase was pumped at a
flow-rate of 1 ml/min and a 20 µl sample was injected into
the system. The chemical structure of each component and the HPLC
chromatogram are shown in Fig. 1.
Comparison with the reference compounds showed that the decoction
contained notoginsenoside R1, astragaloside IV, ginsenoside Rg1,
ginsenoside Rb1, amygdalin, platycodin D and other unidentified
components.
VaD rat model and treatments
Male Sprague-Dawley rats (n=210; age, 8-weeks old;
weight, 200–230 g) were purchased from Hunan Slaccas Jingda
Laboratory Animal Co., Ltd. (Changsha, China). The rats were housed
in a room with a 12-h light/dark cycle and temperature- and
humidity-control (24±2°C and 65±5%). All rats had free access to
food and water throughout the experiments. After 1 week of
acclimatization, the rats were subjected to the Morris water maze
test to ensure their normal memory. Then, a rat model of VaD was
induced by repeated occlusion of the common carotid artery followed
by reperfusion, as previously described, with certain modifications
(20,21). Briefly, the animals were randomly
divided into sham-operated and operated groups. The rats were
firstly anesthetized with chloral hydrate (300 mg/kg, i.p.;
Beyotime Institute of Biotechnology Co., Ltd., Shanghai, China),
and then bilateral common carotid arteries of rats in the operated
group were ligated with 0 type surgical silk through a midline neck
incision, and 0.3 ml blood was obtained from the tail vein. After
20 min, bilateral common carotid arteries were opened for 10 min by
loosening the silk. This course was repeated three times, which
resulted in cerebral ischemia/reperfusion in the rats. The rats in
the sham-operated group received the same surgical operation
without occlusion of the common carotid arteries. During the
surgical procedures, the carotid sheath and the vagus nerve of rats
were preserved from damage.
After 10 days of operation, all animals performed
the Morris water maze test. The rats in the operated group (OPER;
n=120) were randomly assigned to six sub-groups based on various
treatments: The model group (MOD; n=20) receiving an equal volume
of distilled water by oral gavage, the low-dose YXJF group (LDY;
n=20) receiving low-dose YXJF (6.09 g/kg/day), the medium-dose YXJF
group (MDY; n=20) receiving a medium dose YXJF (12.18 g/kg/d), the
high-dose YXJF group (HDY; n=20) receiving high-dose YXJF (24.36
g/kg/day), the huperzine A group (HUA; n=20) receiving huperzine A
(0.15 mg/kg/day) and the piracetam group (PIR; n=20) receiving
piracetam (0.20 g/kg/day). The rats in the sham-operated group
(SHAM; n=22) were, as the control, given an equal volume of
distilled water. After 30 days of treatment, the rat memory was
evaluated using the Morris water maze test.
The experiments were approved by the Ethics
Committee of Guangxi University of Chinese Medicine (Nanning,
China). All procedures were conducted in accordance with the
internationally accepted Principles for Laboratory Animal use and
Care and the Chinese Animal Welfare Legislation.
Morris water maze test
Spatial learning and memory was evaluated by the
Morris water maze test according to a previously described
procedure with certain modifications (22). The maze consisted of a grey
circular tank of 120 cm in diameter and 50 cm in height. The tank
was filled with water kept at 22±1°C and divided into four
quadrants. A circular platform of 10 cm in diameter was in the
center of the second quadrant and submerged ~2.0 cm below the water
surface. To ensure the platform was invisible to the rats, the
water was made opaque using a non-toxic water-soluble black dye
(carbon black ink; 1 ml/56 l; Guilin Fuxuan Stationary Co., Ltd.,
Guilin, China). All rats were released into the water (facing the
sidewall) to search for the hidden platform at four distinct
starting quadrant points, respectively, and each rat was given four
trials a day (one trial for each quadrant). The time that rats took
to find the submerged platform was recorded as the escape latency.
Each rat was allowed to reach the platform within 60 sec and remain
on it for 10 sec. If the rat did not find the platform within 60
sec, it was manually directed toward the platform and placed on the
platform for 10 sec, and the escape latency was recorded as 60 sec.
The rats were trained over five consecutive days. On day six, the
platform was removed, and it was determined whether the rats found
the expected location of the platform in a memory-dependent manner.
The frequency at which the rat passed the targeted point where the
platform had been located within 60 sec was recorded. The
performance of the rats was recorded using a video camera and
analyzed using WMT-100 Morris software (Chengdu Taimeng Software
Co., Ltd., Chengdu, China).
Transmission electron microscopic
observation
After treatment and subsequent memory evaluation,
the rats were randomly selected to be anesthetized with chloral
hydrate (300 mg/kg, i.p.) and then perfused transcardially with
normal saline followed by ~200 ml 2% paraformaldehyde and 2.5%
glutaraldehyde (Tianjin Yongda Chemical Reagent Development Centre,
Tianjin, China) to pre-fix the brain tissue. The brains were
removed and fixed in 3% glutaraldehyde. The neuron ultrastructure
in the hippocampal CA1 region was observed by transmission electron
microscopy (TEM) according to a previously described method with
certain modifications (23). In
brief, the hippocampal CA1 area of the rats was rapidly excised,
and then cut into pieces of 1 mm × 1 mm × 2 mm. The pieces were
fixed in 3% glutaraldehyde for 2 h and post-fixed in 1% osmic acid
(Beijing Zhongjingkeyi Technology Co., Ltd., Beijing, China) for
1.5 h. After that, the pieces were de-hydration-fixed by
conventional ethanol and acetone treatments, embedded in ethoxyline
resin 618 (Beijing Zhongjingkeyi Technology Co., Ltd.) and sliced
using an ultra-thin slicer (UC7; Leica Microsystems, Wetzlar,
Germany). Finally, the slices were double-stained with uranyl
acetate (Beijing Zhongjingkeyi Technology Co., Ltd.) and lead
citrate (Beijing Zhongjingkeyi Technology Co., Ltd.), and observed
and filmed under a Hitachi-7650 TEM (Hitachi, Tokyo, Japan).
Apoptosis analysis by terminal
deoxynucleotidyl transferase-mediated (dUTP) nick end labeling
(TUNEL) staining
Apoptosis was analyzed using TUNEL staining on
paraffin-embedded sections according to a previously described
procedure with certain modifications (24). Briefly, the rats were randomly
selected to be anesthetized with chloral hydrate, and then perfused
transcardially with normal saline followed by ~200 ml 4%
paraformaldehyde (Tianjin Yongda Chemical Reagent Development
Centre) to pre-fix the brain tissue. The brains were excised and
fixed in 4% paraformaldehyde, embedded in paraffin and then cut
into a series of sections. After de-paraffinization and
re-hydration, the sections were rinsed in 0.1 M phosphate buffered
saline (PBS) twice and incubated in Proteinase K working solution
(10 µg/ml in 10 mM Tris/HCl, pH 7.4–8.0) for 15 min at 37°C.
After being rinsed in PBS again, the sections were treated with
fluorescein (green)-labeled dUTP solution containing 10% TdT. A
negative control was produced using dUTP, while a positive control
was produced using DNase 1. The hippocampal CA1 region was observed
and photographed at a magnification of ×200 using a fluorescence
microscope (Olympus BX-60; Olympus, Tokyo, Japan), with green
fluorescence indicating TUNEL-positive cells. After imaging,
converter-POD was added on the slides. The sections were then
counterstained with diaminobenzidine and hematoxylin (Sinopharm
Chemical Reagent Co., Ltd., Shanghai China). Apoptotic cells
represented by TUNEL-positive cells with fluorescent granules in
the nuclei were observed using a microscope (BX-60; Olympus, Tokyo,
Japan). At a magnification of ×400, five microscopic fields were
randomly selected to count the TUNEL-positive cells.
Western blot analysis
Protein expression in hippocampal tissue was
analyzed by western blotting (25). The hippocampal homogenates were
prepared using protein lysis buffer for western blot, and tissue
debris was subsequently removed by centrifugation (12,000 × g for
10 min). The protein concentration of each sample was analyzed.
After addition of sample buffer, the protein was heated for 10 min
at 95°C and then separated by SDS-PAGE (Sigma-Aldrich, St. Louis,
MO, USA). The protein was transferred to a polyvinylidene
difluoride membrane (EMD Millipore, Billerica, MA, USA). The
membrane was incubated with the appropriate primary antibody
overnight at 4°C and then with the horseradish
peroxidase-conjugated secondary antibody for 1.5 h at room
temperature. The targeted proteins were detected by enhanced
chemiluminescence (Amersham, Piscataway, NJ, USA) and images were
obtained and analyzed using UVP GDS-8000 system (Thermo Fisher
Scientific, Rockford, IL, USA).
Statistical analysis
Values are expressed as the mean ± standard error.
When multiple comparisons were performed, the significance was
determined using one-way analysis of variance. Student's t-test was
used to analyze differences between two groups. P<0.05 was
considered to indicate a statistically significant difference. All
data were analyzed with SPSS 16.0 for Windows (SPSS, Inc., Chicago,
IL, USA).
Results
YXJF improves memory impairment in rats
with cerebral ischemia/reperfusion
In the present study, a rat model of VaD was
established by cerebral ischemia reperfusion. After operation
(prior to treatment), the escape latency of the rats in the
operated group was significantly longer than that in the
sham-operated group (all P<0.01; Fig. 2A) within five consecutive training
days, and the frequency at which the rats passed the potential
platform was significantly decreased compared to that in the
sham-operated group (P<0.01; Fig.
2B). The results indicated that the memory function of rats was
severely impaired by cerebral ischemia/reperfusion, suggesting that
the animal model of VaD was successfully induced.
Administration of YXJF markedly shortened the escape
latency in a dose-dependent manner when compared to that in the
model group (P<0.05 or P<0.01; Fig. 3A) within five consecutive trial
days, and remarkably increased the frequency at which the rats
passed the hypothetical platform within 60 sec (P<0.05 or
P<0.01; Fig. 3B). In addition,
the escape latency and frequency in the high-dose YXJF group were
similar to those in the huperzine A group (P>0.05), while the
escape latency was shorter and the frequency was higher compared
with that in the piracetam group (all P<0.01). There was no
difference in escape latency or frequency between the medium-dose
YXJF group and the piracetam group (all P>0.05). These results
demonstrated that YXJF improved cerebral
ischemia/reperfusion-induced memory impairment in rats, providing
evidence for the potential anti-dementia action of YXJF.
 | Figure 3Effects of YXJF on the memory
function of rats with cerebral ischemia/reperfusion. After
treatment for 30 days, memory function of rats was evaluated by the
Morris water maze test. (A) Escape latency. (B) Frequency of the
rats passing the potential platform within 60 sec. Values are
expressed as the mean ± standard error (n=20-22).
*P<0.05, **P<0.01 vs. SHAM;
#P<0.05, ##P<0.01 vs. MOD;
&P<0.05, &&P<0.01 vs. HUA;
▲P<0.05, ▲▲P<0.01 vs. PIR. MOD, model
group; LDY, low-dose YXJF group; MDY, medium-dose YXJF group; HDY,
high-dose YXJF group; HUA, huperzine A group; PIR, piracetam group;
YXJF, Yifei Xuanfei Jiangzhuo formula. |
YXJF inhibits apoptosis in the
hippocampal CA1 region
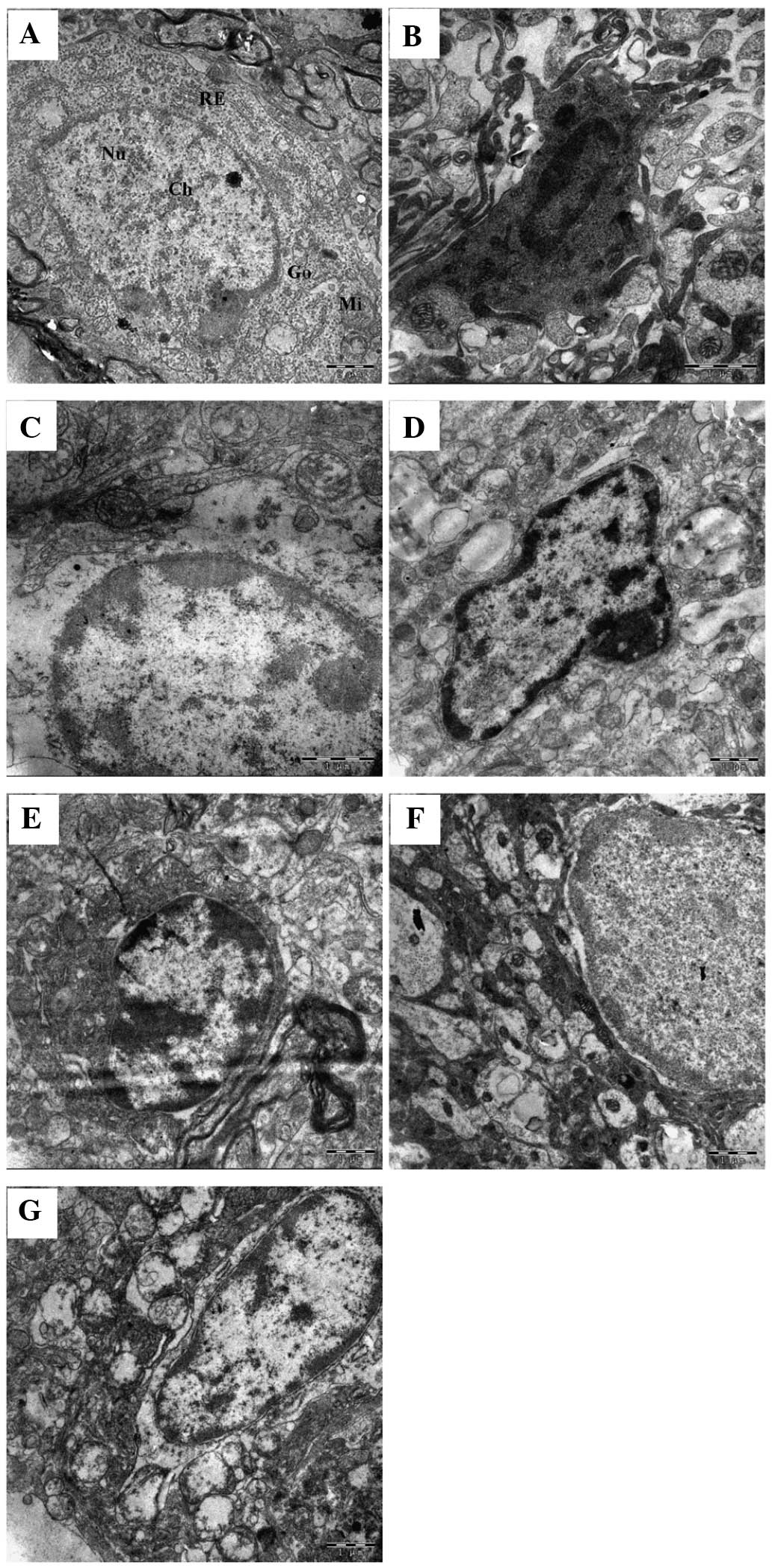
As shown in Fig. 4,
the neurons in the hippocampal CA1 region in the model group
(Fig. 4B) exhibited typical
ultrastructural characteristics of apoptosis, including smaller
cells with nuclear condensation, chromatin margination, unchanged
mitochondria and increased blebbing compared to that in the
sham-operated group (Fig. 4A).
After YXJF treatment (Fig. 4C–E),
the neuronal ultrastructure was significantly improved, indicating
a reduction of apoptosis. In addition, huperzine A (Fig. 4F) and piracetam (Fig. 4G) also ameliorated the
apoptosis-associated ultrastructural changes in the neurons.
In order to further confirm the anti-apoptotic
action of YXJF, apoptosis in the hippocampal CA1 region was
analyzed by TUNEL staining. Fig. 5
shows that TUNEL-positive cells in the model group (Fig. 5B and H) were significantly
increased compared to those in the sham-operated group (P<0.01;
Fig. 5A and H), suggesting that
cerebral ischemia/reperfusion led to apoptosis in the hippocampus.
In the treatment groups, YXJF inhibited apoptosis in a
dose-dependent manner (Fig. 5C–E and
H), as indicated by fewer TUNEL-positive cells compared with
those in the model group (P<0.05 or P<0.01). In addition,
huperzine A (Fig. 5F and H) and
piracetam (Fig. 5G and H) also
reduced apoptosis with no difference in TUNEL-positive cells
between the high-dose YXJF and the huperzine A groups, as well as
between the medium-dose YXJF and the piracetam groups (Fig. 5H). These results indicated that
YXJF inhibited apoptosis in the hippocampal CA1 region of rats with
cerebral ischemia/reperfusion.
 | Figure 5Apoptosis analysis by TUNEL staining.
After treatment and subsequent memory evaluation, apoptosis in
hippocampus CA1 region was analyzed by TUNEL staining. Green
fluorescence indicates TUNEL-positive cells in each group. (A) SHAM
group; (B) MOD group; (C) LDY group; (D) MDY group; (E) HDY group;
(F) HUA group; and (G) PIR group (magnification, ×200). (H) Number
of TUNEL-positive cells per field counted at a magnification of
×400 in each group. Values are expressed as the mean ± standard
error. *P<0.05, **P<0.01 vs. SHAM;
#P<0.05, ##P<0.01 vs. MOD;
&P<0.05, &&P<0.01 vs. HUA;
▲P<0.05 vs. PIR. MOD, model group; LDY, low-dose YXJF
group; MDY, medium-dose YXJF group; HDY, high-dose YXJF group; HUA,
huperzine A group; PIR, piracetam group; YXJF, Yifei Xuanfei
Jiangzhuo formula. |
Effects of YXJF on the expression of
apoptosis-associated proteins in the hippocampus
To explore the underlying mechanisms of the
inhibition of apoptosis by YXJF, the protein expression of Bax,
Bcl-2,and c-Jun in the hippocampus was analyzed (Fig. 6). Compared with that in the
sham-operated group, the protein expression of Bax and c-Jun in the
model group was significantly increased, while that of Bcl-2 was
markedly reduced, suggesting that cerebral
ischemia/reperfusion-induced apoptosis was mediated by changes in
the protein expression of Bax, Bcl-2 and c-Jun in the hippocampus.
Administration of YXJF obviously decreased the protein expression
of Bax and c-Jun, while enhancing Bcl-2 protein expression.
Huperzine A significantly reduced Bax, but decreased c-Jun and
increased Bcl-2 protein expression only to a certain extent, while
piracetam markedly restrained Bax and c-Jun, and promoted Bcl-2
protein expression. Treatment with high-dose YXJF and piracetam had
similar effects on the protein expression of the three apoptotic
proteins. These results supported that YXJF inhibits apoptosis
through reducing the protein expression of Bax and c-Jun, and
promoting Bcl-2 protein expression, and its mechanism of action
appears to be more similar to that of piracetam than that of
huperzine A.
 | Figure 6Protein expression of Bax, Bcl-2 and
c-Jun in the hippocampus. (A) After treatment and subsequent memory
evaluation, the hippocampus was harvested and the protein
expression was assessed by western blot analysis. (B-D) Quantified
protein levels of (B) Bax (C) c-Jun and (D) Bcl-2 normalized to
β-actin. Values are expressed as the mean ± standard
error.*P<0.05, **P<0.01 vs. SHAM;
#P<0.05, ##P<0.01 vs. MOD;
&&P<0.01 vs. HUA; ▲P<0.05,
▲▲P<0.01 vs. PIR. Bcl-2, B-cell lymphoma 2; Bax,
Bcl-2-associated X protein; MOD, model group; LDY, low-dose YXJF
group; MDY, medium-dose YXJF group; HDY, high-dose YXJF group; HUA,
huperzine A group; PIR, piracetam group; YXJF, Yifei Xuanfei
Jiangzhuo formula. |
Effects of YXJF on the protein expression
of PKA, CREB and phosphorylated CREB in the hippocampus
The present study further analyzed the protein
expression of PKA, CREB and p-CREB in the hippocampus. Compared to
the sham group, cerebral ischemia/reperfusion decreased the protein
expression of the PKA C-α sub-unit (Fig. 7A and B) and CREB (Fig. 7A and C), and reduced CREB
phosphorylation (Fig. 7A and D).
Of note, YXJF treatment significantly ameliorated PKA C-α sub-unit
and CREB protein expression, and promoted CREB phosphorylation in a
dose-dependent manner. Huperzine A significantly increased CREB
protein expression, but did not obviously promote PKA C-α protein
expression or CREB phosphorylation, while piracetam markedly
enhanced CREB protein expression and its phosphorylation, and, to a
certain extent, promoted PKA C-α protein expression. These results
suggested that YXJF improved memory impairment of rats with
cerebral ischemia/reperfusion, at least in part through enhancing
PKA/CREB signal transduction.
 | Figure 7Protein expression of PKA, CREB and
p-CREB in the hippocampus. (A) After treatment and subsequent
memory evaluation, hippocampi were harvested and the protein
expression was analyzed by western blotting. (B-D) Quantified
protein levels of (B) PKA (C) CREB and (D) p-CREB normalized to
β-actin. Values are expressed as the mean ± standard error.
**P<0.01 vs. SHAM; ##P<0.01 vs. MOD;
&P<0.05, &&P<0.01 vs. HUA;
▲P<0.05, ▲▲P<0.01 vs. PIR. MOD, model
group; LDY, low-dose YXJF group; MDY, medium-dose YXJF group; HDY,
high-dose YXJF group; HUA, huperzine A group; PIR, piracetam group;
YXJF, Yifei Xuanfei Jiangzhuo formula; PKA, protein kinase A;
p-CREB, phosphorylated cyclic adenosine monophosphate-responsive
element binding protein. |
Discussion
Medications currently used in the treatment of VaD,
including cholinesterase inhibitors such as donepezil and
non-cholinergics such as memantine (26,27),
have been proven to be efficient to a certain extent. Owing to the
limitations of these drugs (28),
however, an increasing number of patients and clinician have
resorted to using herbal medications to treat VaD.
Chinese herbs have been widely used to treat VaD in
clinical practice in China. Although a previous clinical study by
our group showed that the Chinese herbal decoction YXJF was
efficient in the treatment of VaD (18), further studies on YXJF are required
to provide additional convincing evidence and reveal the underlying
mechanism of action. It is well known that cerebral hypoperfusion
is a common physiopathological condition contributing to
neurodegenerative diseases including VaD (29). Therefore, a rat model of VaD was
successfully induced in the present study by repeated occlusion of
the common carotid artery followed by reperfusion, which resulted
in memory impairment, which was in accordance with the results of
previous studies (20,21). Administration of YXJF significantly
alleviated memory impairment in the model rats to a similar extent
to that of the treatment with huperzine A and piracetam, the two
currently used anti-dementia drugs (30,31),
in agreement with the previous study by our group (18). These results suggested that YXJF
has marked anti-VaD activity and is an alternative choice for the
treatment of VaD.
The hippocampus, the key site of memory function, is
highly sensitive to ischemia/hypoxia, and usually suffers the
greatest injury during cerebral hypoperfusion (28,32).
Apoptosis is an essential function for the normal development of
any multicellular organism. In healthy organisms, apoptotic and
anti-apoptotic proteins are balanced; however, through shifting
this equilibrium, apoptosis can be upregulated during degenerative
conditions and amplification of apoptosis through factors including
pathological stimuli contributes to autoimmune disorders and
cognitive deficits (33–35). It is generally accepted that
cerebral ischemia/reperfusion injury is closely associated with
apoptosis, thus resulting in the death of hippocampal CA1 neurons
(36). To reveal the mechanism of
action of YXJF, the present study assessed the occurrence of
apoptosis in the hippocampal CA1 region through investigating the
neuronal ultrastructure by TEM as well as TUNEL staining. As
expected, cerebral ischemia/reperfusion caused apoptosis in the
hippocampal CA1 region, and YXJF inhibited apoptosis in a
dose-dependent manner. The present study used huperzine A and
piracetam as positive controls for testing the efficacy of YXJF.
Huperzine A is an inhibitor of acetylcholinesterase (AChE) isolated
from Chinese folk medicine Huperzia serrata and piracetam is
a derivative of the neurotransmitter gamma-aminobutyric acid
(GABA); the two drugs have been proved to perform anti-apoptotic
functions (37,38) and are widely applied in the
clinical treatment of brain dysfunction. The positive control drugs
indeed restrained apoptosis to a similar extent to that of YXJF,
suggesting the anti-apoptotic action of YXJF.
It is well known that apoptosis is a strictly
controlled process involving multiple changes in the expression of
certain proteins, including Bcl-2 family proteins. Bcl-2 and Bax
belong to the Bcl-2 family, and Bcl-2 exerts a survival function in
response to a wide range of apoptotic stimuli through inhibition of
Bax translocation and mitochondrial cytochrome c release
(39), while Bax forms oligomers
and translocates from the cytosol to the mitochondrial membrane
upon apoptotic stimulation, thus leading to increases in
mitochondrial membrane permeability, the release of cytochrome
c from mitochondria, and subsequent activation of the
apoptotic program (40,41). In addition, c-Jun, a member of the
Jun family, dimerizes with Fos to form activator protein-1, a
transcription factor that regulates genes and subsequently exerts
diverse biological functions, including cell proliferation,
differentiation and apoptosis (42). To further reveal the mechanism by
which YXJF inhibits apoptosis, the expression of Bax, c-Jun and
Bcl-2 was determined by western blot anaysis. In the present study,
cerebral ischemia/reperfusion caused an increase in the protein
expression of Bax and c-Jun, as well as a reduction in Bcl-2
expression in the hippocampus. Previous studies reported that
upregulating the expression of Bcl-2 can protect neuronal cells
from apoptosis (43), and that
decreased Bax or increased Bcl-2 indicate anti-apoptotic
neuroprotective effects in a rat model of VaD (44), while the activity of c-Jun was
found to be increased in rats with cerebral ischemia/reperfusion
(45), which was in accordance
with the results of the present study. Of note, administration of
YXJF decreased the protein expression of Bax and c-Jun, and
increased Bcl-2 expression in the hippocampus. The results of the
present study implied that YXJF alleviates memory impairment, at
least in part, through inhibiting apoptosis in rats with cerebral
ischemia reperfusion.
In the present study, huperzine A and piracetam were
used as positive control drugs for YXJF; the former is an inhibitor
of AChE, while the latter is a derivative of GABA. The improvement
of memory impairment and apoptosis by huperzine A and piracetam
clearly confirmed the potency of the decoction. According to
previous studies, huperzine A was able to inhibit the upregulation
of Bax and c-Jun, and reverse the downregulation of Bcl-2 in
vivo and in vitro (37,46),
while piracetam attenuates increases in the expression of Bax
(47). In the present study,
however, piracetam markedly inhibited Bax and c-Jun protein
expression in hippocampi of rats with cerebral
ischemia/reperfusion, and significantly increased Bcl-2, while
huperzine A only had a marked effect in terms of decreasing Bax
levels. Due to the similar effects on the protein expression of
Bax, c-Jun and Bcl-2 between YXJF and piracetam, it was inferred
that the two drugs may share a similar mechanism of action of
alleviating memory impairment in rats following cerebral
ischemia/reperfusion.
It is generally accepted that hippocampal
cAMP/PKA/CREB signaling has a key role in memory formation
(16,17). In this pathway, PKA is composed of
two regulatory sub-units (R) and two catalytic sub-units (C). The C
sub-unit exists in three isoforms (C-α, C-β, and C-γ). In the
inactive state, the R sub-units block the active sites on the C
sub-units. Upon increases in cAMP levels, the binding between cAMP
and R sub-units reduces the auto-inhibitory contact, and active
monomeric C sub-units are released, thus leading to the activation
of PKA. Activated PKA promotes CREB phosphorylation at Ser133
(48) and subsequently regulates
memory formation. Nefiracetam, a piracetam-like drug, was reported
to improve memory function via cAMP/PKA/CREB signaling in rats with
sustained cerebral ischaemia, showing increased cAMP levels, PKA
C-α/β protein expression and CREB phosphorylation (17). Moreover, piracetam increased the
cAMP concentration in the brain of guinea pigs (49), and promoted PKA C-β and CREB
phosphorylation in aged rats (50). Therefore, piracetam improves memory
impairment, partly through enhancing cAMP/PKA/CREB signaling. In
the present study, piracetam was shown to have these effects, and
YXJF treatment similarly increased PKA C-α and CREB protein
expression, and promoted CREB phosphorylation. The results of the
present study further confirmed that YXJF shares similar mechanisms
of action with piracetam regarding their improvement of memory
impairment in rats following cerebral ischemia/reperfusion.
In conclusion, the present study indicated that the
Chinese herbal decoction YXJF improves memory impairment through
anti-apoptotic mechanisms and through enhancing PKA/CREB signal
transduction in rats with cerebral ischemia/reperfusion, which
suggested the potential uses of YXJF, or compounds derived thereof,
against cognitive deficits in VaD.
Acknowledgments
The present study was supported by the National
Natural Science Foundation of China (no. 81160435), Guangxi
Department of Health (no. GZKZ-Z1102) and the Guangxi Key
Laboratory of Chinese Medicine Foundation Research (Guangxi
University of Chinese Medicine; nos. 14-045-42 and 13-051-35). The
authors would like to thank Dr Yue-Qiang Hu (Department of Internal
Neurology, the First Affiliated Hospital, Guangxi University of
Chinese Medicine, Nanning, China) and Professor Bu-Ming Liu
(Guangxi Key Laboratory of Traditional Chinese Medicine Quality
Standards, Nanning, China) for their technical assistance.
References
|
1
|
Román GC: Vascular dementia may be the
most common form of dementia in the elderly. J Neurol Sci.
203–204:7–10. 2002. View Article : Google Scholar
|
|
2
|
Iemolo F, Duro G, Rizzo C, Castiglia L,
Hachinski V and Caruso C: Pathophysiology of vascular dementia.
Immun Ageing. 6:132009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zekry D, Herrmann FR, Graf CE, Giannelli
S, Michel JP, Gold G and Krause KH: Mild cognitive impairment,
degenerative and vascular dementia as predictors of intra-hospital,
short- and long-term mortality in the oldest old. Aging Clin Exp
Res. 23:60–66. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ekonomou A, Ballard CG, Pathmanaban ON,
Perry RH, Perry EK, Kalaria RN and Minger SL: Increased neural
progenitors in vascular dementia. Neurobiol Aging. 32:2152–2161.
2011. View Article : Google Scholar
|
|
5
|
Poels MM, Ikram MA, van der Lugt A, Hofman
A, Niessen WJ, Krestin GP, Breteler MM and Vernooij MW: Cerebral
micro-bleeds are associated with worse cognitive function: The
Rotterdam Scan Study. Neurology. 78:326–333. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu CX, Liu R, Gao M, Zhao G, Wu S, Wu CF
and Du GH: Pinocembrin protects brain against ischemia/reperfusion
injury by attenuating endoplasmic reticulum stress induced
apoptosis. Neurosci Lett. 546:57–62. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nishio K, Ihara M, Yamasaki N, Kalaria RN,
Maki T, Fujita Y, Ito H, Oishi N, Fukuyama H, Miyakawa T, et al: A
mouse model characterizing features of vascular dementia with
hippocampal atrophy. Stroke. 41:1278–1284. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen CH, Jiang Z, Yan JH, Yang L, Wang K,
Chen YY, Han JY, Zhang JH and Zhou CM: The involvement of
programmed cell death 5 (PDCD5) in the regulation of apoptosis in
cerebral ischemia/reperfusion injury. CNS Neurosci Ther.
19:566–576. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eberspächer E, Werner C, Engelhard K, Pape
M, Gelb A, Hutzler P, Henke J and Kochs E: The effect of
hypothermia on the expression of the apoptosis-regulating protein
Bax after incomplete cerebral ischemia and reperfusion in rats. J
Neurosurg Anesthesiol. 15:200–208. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bernabeu R, Bevilaqua L, Ardenghi P,
Bromberg E, Schmitz P, Bianchin M, Izquierdo I and Medina JH:
Involvement of hippocampal cAMP/cAMP-dependent protein kinase
signaling pathways in a late memory consolidation phase of
aversively motivated learning in rats. Proc Natl Acad Sci USA.
94:7041–7046. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Abel T, Nguyen PV, Barad M, Deuel TA,
Kandel ER and Bourtchouladze R: Genetic demonstration of a role for
PKA in the late phase of LTP and in hippocampus-based long-term
memory. Cell. 88:615–626. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hagiwara M, Brindle P, Harootunian A,
Armstrong R, Rivier J, Vale W, Tsien R and Montminy MR: Coupling of
hormonal stimulation and transcription via the cyclic AMP-reponsive
factor CREB is rate limited by nucluear entry of protein kinase A.
Mol Cell Biol. 13:4852–4859. 1993.PubMed/NCBI
|
|
13
|
Chutae DL, Villiger JW and Kirton NF:
Testing cyclic AMP mediation of memory: Reversal of
alpha-methyl-p-tyrosine-induced amnesia. Psychopharmacology (Berl).
74:129–131. 1981. View Article : Google Scholar
|
|
14
|
Zhao WQ, Polya GM, Wang BH, Gibbs ME,
Sedman GL and Ng KT: Inhibitors of cAMP-dependent protein kinase
impair long-term memory formation in day-old chicks. Neurobiol
Learn Mem. 64:106–118. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guzowski JF and McGaugh JL: Antisense
oligodeoxynu-cleotide-mediated disruption of hippocampal cAMP
response element binding protein levels impairs consolidation of
memory for water maze training. Proc Natl Acad Sci USA.
94:2693–2698. 1997. View Article : Google Scholar
|
|
16
|
Nagakura A, Niimura M and Takeo S: Effects
of a phosphodiesterase IV inhibitor rolipram on microsphere
embolism-induced defects in memory function and cerebral cyclic AMP
signal transduction system in rats. Br J Pharmacol. 135:1783–1793.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takeo S, Niimura M, Miyake-Takagi K,
Nagakura A, Fukatsu T, Ando T, Takagi N, Tanonaka K and Hara J: A
possible mechanism for improvement by a cognition-enhancer
nefiracetam of spatial memory function and cAMP-mediated signal
transduction system in sustained cerebral ischaemia in rats. Br J
Pharmacol. 138:642–654. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li TW, Tang N and Zhao QS: Clinical
observation of Yifei Xuanfei Jiangzhuo Formula treated vascular
dementia. Guangxi J Trad Chin Med. 37:105–107. 2014.In Chinese.
|
|
19
|
Leung KS, Bian ZX, Moher D, Dagenais S, Li
YP, Liu L, Wu TX and Miao JX: Improving the quality of randomized
controlled trials in Chinese herbal medicine, part III: Quality
control of Chinese herbal medicine used in randomized controlled
trials. J Chin Integr Med. 4:225–232. 2006. View Article : Google Scholar
|
|
20
|
Alipanahzadeh H, Soleimani M, Soleimani
Asl S, Pourheydar B, Nikkhah A and Mehdizadeh M: Transforming
growth factor-α improves memory impairment and neurogenesis
following ischemia reperfusion. Cell J. 16:315–324. 2014.PubMed/NCBI
|
|
21
|
Wu YY, Wu WY, Gong HL, Li WZ and Yin YY:
Astragalosides attenuate learning and memory impairment in rats
following ischemia-reperfusion injury. Mol Med Rep. 9:1319–1324.
2014.PubMed/NCBI
|
|
22
|
Langdon KD, Granter-Button S, Harley CW,
Moody-Corbett F, Peeling J and Corbett D: Cognitive rehabilitation
reduces cognitive impairment and normalizes hippocampal CA1
architecture in a rat model of vascular dementia. J Cereb Blood
Flow Metab. 33:872–879. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Li H and Xin X: Nitrogen dioxide (NO(2))
pollution as a potential risk factor for developing vascular
dementia and its synaptic mechanisms. Chemosphere. 92:52–58. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang S, Qi Y, Xu Y, Han X, Peng J, Liu K
and Sun CK: Protective effect of flavonoid-rich extract from Rosa
laevigata Michx on cerebral ischemia-reperfusion injury through
suppression of apoptosis and inflammation. Neurochem Int.
63:522–532. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Feng XT, Wang TZ, Chen Y, Liu JB, Liu Y
and Wang WJ: Pollen Typhae total flavone improves insulin-induced
glucose uptake through the β-arrestin-2-mediated signaling in C2C12
myotubes. Int J Mol Med. 30:914–922. 2012.PubMed/NCBI
|
|
26
|
Zekry D: Is it possible to treat vascular
dementia? Front Neurol Neurosci. 24:95–106. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Baskys A and Hou AC: Vascular dementia:
Pharmacological treatment approaches and perspectives. Clin Interv
Aging. 2:327–335. 2007.PubMed/NCBI
|
|
28
|
Malykh AG and Sadaie MR: Piracetam and
piracetam-like drugs: From basic science to novel clinical
applications to CNS disorders. Drugs. 70:287–312. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hartman RE, Lee JM, Zipfel GJ and Wozniak
DF: Characterizing learning deficits and hippocampal neuron loss
following transient global cerebral ischemia in rats. Brain Res.
1043:48–56. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Xing SH, Zhu CX, Zhang R and An L:
Huperzine a in the treatment of Alzheimer's disease and vascular
dementia: A meta-analysis. Evid Based Complement Alternat Med.
2014:3639852014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
He Z, Liao Y, Zheng M, Zeng FD and Guo LJ:
Piracetam improves cognitive deficits caused by chronic cerebral
hypoperfusion in rats. Cell Mol Neurobiol. 28:613–627. 2008.
View Article : Google Scholar
|
|
32
|
Lee JY, Lee HE, Kang SR, Choi HY, Ryu JH
and Yune TY: Fluoxetine inhibits transient global ischemia-induced
hippo-campal neuronal death and memory impairment by preventing
blood-brain barrier disruption. Neuropharmacology. 79:161–171.
2014. View Article : Google Scholar
|
|
33
|
Carson DA and Ribeiro JM: Apoptosis and
disease. Lancet. 341:1251–1254. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
O'Reilly LA and Strasser A: Apoptosis and
autoimmune disease. Inflamm Res. 48:5–21. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Fang M, Li J, Tiu SC, Zhang L, Wang M and
Yew DT: N-methyl-D-aspartate receptor and apoptosis in Alzheimer's
disease and multiinfarct dementia. J Neurosci Res. 81:269–274.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Espinosa-García C, Vigueras-Villaseñor RM,
Rojas-Castañeda JC, Aguilar-Hernández A, Monfil T, Cervantes M and
Moralí G: Post-ischemic administration of progesterone reduces
caspase-3 activation and DNA fragmentation in the hippocampus
following global cerebral ischemia. Neurosci Lett. 550:98–103.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhou J and Tang XC: Huperzine A attenuates
apoptosis and mitochondria-dependent caspase-3 in rat cortical
neurons. FEBS Lett. 526:21–25. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gabryel B, Adamek M, Pudełko A, Małecki A
and Trzeciak HI: Piracetam and vinpocetine exert cytoprotective
activity and prevent apoptosis of astrocytes in vitro in hypoxia
and reoxy-genation. Neurotoxicology. 23:19–31. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Murphy KM, Ranganathan V, Farnsworth ML,
Kavallaris M and Lock RB: Bcl-2 inhibits Bax translocation from
cytosol to mitochondria during drug-induced apoptosis of human
tumor cells. Cell Death Differ. 7:102–111. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jürgensmeier JM, Xie Z, Deveraux Q,
Ellerby L, Bredesen D and Reed JC: Bax directly induces release of
cytochrome C from isolated mitochondria. Proc Natl Acad Sci USA.
95:4997–5002. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Narita M, Shimizu S, Ito T, Chittenden T,
Lutz RJ, Matsuda H and Tsujimoto Y: Bax interacts with the
permeability transition pore to induce permeability transition and
cytochrome c release in isolated mitochondria. Proc Natl Acad Sci
USA. 95:14681–14686. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Shaulian E and Karin M: AP-1 as a
regulator of cell life and death. Nat Cell Biol. 4:E131–E136. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yang S, Zhou G, Liu H, Zhang B, Li J, Cui
R and Du Y: Protective effects of p38 MAPK inhibitor SB202190
against hippocampal apoptosis and spatial learning and memory
deficits in a rat model of vascular dementia. Biomed Res Int.
2013:2157982013. View Article : Google Scholar
|
|
44
|
Sun ZK, Ma XR, Jia YJ, Liu YR, Zhang JW
and Zhang BA: Effects of resveratrol on apoptosis in a rat model of
vascular dementia. Exp Ther Med. 7:843–848. 2014.PubMed/NCBI
|
|
45
|
Zhang TL, Fu JL, Geng Z, Yang JJ and Sun
XJ: The neuroprotective effect of losartan through inhibiting
AT1/ASK1/MKK4/JNK3 pathway following cerebral I/R in rat
hippocampal CA1 region. CNS Neurosci Ther. 18:981–987. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Wang R, Zhang HY and Tang XC: Huperzine A
attenuates cognitive dysfunction and neuronal degeneration caused
by beta-amyloid protein-(1-40) in rat. Eur J Pharmacol.
421:149–156. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
He Z, Hu M, Zha YH, Li ZC, Zhao B, Yu LL,
Yu M and Qian Y: Piracetam ameliorated oxygen and glucose
deprivation-induced injury in rat cortical neurons via inhibition
of oxidative stress, excitatory amino acids release and P53/Bax.
Cell Mol Neurobiol. 34:539–547. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Gonzalez GA and Montminy MR: Cyclic AMP
stimulates somatostatin gene transcription by phosphorylation of
CREB at serine 133. Cell. 59:675–680. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Weth G: The influence of piracetam on the
cyclic adenosine monophosphate (cAMP) concentration in the brain
and colon of guinea pigs. Arzneimittelforschung. 33:812–814.
1983.PubMed/NCBI
|
|
50
|
Yao H, Gu LJ and Guo JY: Study on effect
of astragali radix polysaccharides in improving learning and memory
functions in aged rats and its mechanism. China J Chin Mater Med.
39:2071–2075. 2014.In Chinese.
|