Introduction
Congenital or acquired deformities of the external
ear have significant negative effects on patients (1). The cartilage of the external ear,
classified as elastic cartilage due to the high abundance of
elastic fibers, is known to be avascular, aneural and alymphatic,
and therefore, it is difficult for the external ear to be restored
following being damaged (2). At
present, the most commonly used treatment for deformities of the
external ear is an ear-shaped and hand-carved autologous costal
cartilage graft which (3,4). Despite the high biocompatibility and
immune privilege of this method, it is associated with certain
limitations and degrees of success. During this procedure, it is
rather difficult to sculpt an anatomic-fidelity auricle shape,
possibly resulting in a distorted shape. Furthermore, such method
highly depends on the skill and experience of the surgeon (5,6). All
of these make it difficult to achieve a satisfying cosmetic result
and a shape with long-term stability.
In order to avoid these problems, cell-based tissue
engineering has motivated numerous researchers to explore a cure
for the deformity (7). Considering
the source of cells for tissue-engineered elastic cartilage,
autologous chondrocytes are a sensible choice of cell source due to
their fast proliferation and being established enough in the
generation of auricle cartilage (8). However, it has been reported that
chondroctyes rapidly lose their cobblestone-like appearance and
function under monolayer culture conditions in vitro,
leading to the generation of compromised cartilage tissue (9).
Another candidate cell source are bone
marrow-derived stem cells (BMSCs), characterized by self-renewal, a
rapid proliferative capacity and the potency of differentiating
into chondrocytes (10). At
present, numerous methods are known to induce chondrogenic
differentiation of BMSCs. The application of transforming growth
factor-β (TGF-β) and dexamethasone is a classical method. However,
at the same time, incubation with TGF-β leads to the upregulation
of the expression of certain genes, including collagen X, alkaline
phosphatase and matrix metalloproteinase 13, which indicates
hypotrophic progress, inevitably resulting in calcification and
vascularization of the generated cartilage, which is a major
drawback besides the high cost (11–13).
Co-culture of auricle chondrocytes and BMSCs may
represent a promising method to overcome those hurdles. It has been
reported that the production of extracellular matrix (ECM) in
co-culture occurs earlier than that in chondrocytes or induced
BMSCs alone (14). For the
co-culture system, it has been reported that BMSCs, either through
direct or indirect contact with chondrocytes, are driven to
differentiate towards chondrocytes and produce ECM-assembled
cartilage (15,16). The underlying mechanism of this
inductive effect of chondrocytes on BMSCs is likely to be the
secretion of paracrine by the chondrocytes (17). In addition, Hwang et al
(18) demonstrated that the
supernatant of chondrocytes induced the chondrogenic
differentiation of stem cells. To date, it is has not been reported
that the supernatant of auricle chondrocytes of piglets drives
BMSCs to differentiate towards elastic chondrocytes and produce
elastic cartilage.
The present study utilized the supernatant of
auricle chondrocytes to drive BMSCs to differentiate towards
elastic chondrocytes, and then subjected them to histological and
polymerase chain reaction (PCR) analyses. The feasibility of
fabricating elastic cartilage through this method was examined and
a possible protocol for structuring the desired type of cartilage
was provided.
Materials and methods
Isolation and culture of BMSCs and
auricle chondrocytes
All experimental protocols involving animal tissues
and cells were approved by the Ethics Committee of Shanghai Jiao
Tong University School of Medicine (Shanghai, China).
Bone marrow was obtained from the femur of newborn
piglets as described previously (19). Changfeng hybrid piglets (age, 4–7
days; weight, 2 kg) were purchased from Shanghai Chuansha Breeding
Factory (Shanghai, China). The bone marrow sample was then seeded
into culture dishes for the whole-blood adherent method (20), and complete low-glucose Dulbecco's
modified Eagle's medium (L-DMEM; Gibco-BRL, Invitrogen Life
Technologies, Carlsbad, CA, USA) was added. The complete L-DMEM
contained 10% (v/v) fetal bovine serum (FBS; Gibco-BRL). The cells
were incubated at 37°C in a humidified atmosphere containing 5%
CO2.
Auricle chondrocytes were harvested from the
external auricle of the newborn piglet, which was sacrificed via
the aeroembolism method (21). The
sample was diced into 1×1-mm pieces, which were submerged in
chloromycetin (Sinopharm Chemical Reagent Co., Ltd., Shanghai,
China) for 1 hour, followed by digestion with 0.25% trypsin
(Gibco-BRL). Chondrocytes were isolated from the surrounding matrix
by collagenase II digestion (Sigma-Aldrich, St. Louis, MO, USA) for
30 min at room temperature. The cells were seeded at 5,000
cells/cm2 and expanded in complete H-DMEM
(Gibco-BRL).
Flow cytometric analysis
The BMSCs at primary passage were digested, counted
and suspended at a density of 1–2.5×106 cells/ml.
Subsequently, 200-µl aliquots of the cell suspension were
transferred into 1.5-ml centrifuge tubes, and the cells were
incubated with 1 µl anti-rat CD29, anti-human CD34,
anti-human CD45 or anti-human CD90 (all BD Biosciences, Franklin
Lakes, NJ, USA), respectively, at 4°C for 30 min, during which the
tubes were gently agitated every 10 min. The samples were then
washed three times with phosphate-buffered saline containing 4%
(v/v) FBS. After that, the samples were assessed by flow cytometry
(Beckman Coulter FC 500; Beckman Coulter, Inc., Brea, CA, USA).
Chondrogenic differentiation
Auricle chondrocytes at passage 2 were incubated in
H-DMEM for 48 h, and the supernatant of the cells was harvested.
Following this, the supernatant was centrifuged at 660 ×g for 10
min (17). The second passage of
BMSCs was cultured in the pre-treated supernatant of elastic
chondrocytes, which is being referred to as conditioned medium. The
conditioned medium was changed every three days. After four weeks
of differentiation, BMSCs were digested, suspended and seeded onto
glass slides in culture dishes for the chondrogenic differentiation
test. In the control group, the BMSCs were cultured in DMEM
containing 10% FBS.
Histological and immunohistochemical
staining
After four weeks of culture, the cells were fixed in
4% (w/v) para-formaldehyde (Sigma-Aldrich) for 15 min and then
subjected to hematoxylin and eosin (Goodbio Technology Co., Ltd.,
Wuhan, China) and safranin O (Goodbio Technology Co., Ltd.)
staining, respectively, to assess cell morphology and chondrocytic
differentiation.
Samples were blocked with 3%
H2O2 and heat was used for antigen retrieval.
Antigen retrieval was performed using 0.01 M citrate antigen
retrieval solution (Goodbio Technology Co., Ltd.) in a pressure
cooker at 100°C for 10–15 min. Cells were blocked with 5% bovine
serum albumin (BSA; Sigma-Aldrich) for 30 min and then incubated at
4°C overnight in 0.5% BSA containing the following antibodies: Type
I collagen monoclonal (1:400; ab90395), type II collagen polyclonal
(1:50; ab34712), type X collagen monoclonal (1:500; ab49945) and
elastin polyclonal (1:500; ab21610) (all Abcam, Cambridge, UK),
followed by horseradish peroxidase-conjugated anti-rabbit and
anti-rat antibody (Goodbio Technology Co., Ltd.), respectively
(1:200 in 0.5% BSA). Color development was performed with
diaminobenzidine tetrahydrochloride (DAB; Maibio, Shanghai, China).
Samples were viewed using the Nikon Y-FL 078077 microscope (Nikon,
Tokyo, Japan).
Reverse transcription quantitative
(RT-q)PCR
After chondrogenic induction, total RNA in the
experimental and control groups was extracted from each specimen
and cDNA was obtained by reverse transcription according to
previously described methods (22). PCR was repeated for 40 cycles, and
the PCR cycling conditions were as follows: Initial denaturation at
95°C for 10 min, annealing at 95°C for 15 sec, and elongation at
60°C for 1 min. The chondrogenic genes (collagen I, collagen II,
collagen X and elastin) were assessed to evaluate chondrogenic
differentiation. The primers used in the present study are listed
in Table I.
 | Table IPrimer sequences for reverse
transcription quantitative polymerase chain reaction. |
Table I
Primer sequences for reverse
transcription quantitative polymerase chain reaction.
| Gene | Primer | Product (bp) |
|---|
| COL1A2 | F:
5′-GGTTTCGGCAAAGTTGGAGG-3′ | 218 |
| R:
5′-GCCCTTTCTTGCAGTTGCC-3′ | |
| COL2A1 | F:
5′-CGAGACAGGTGCTGCAAGTC-3′ | 141 |
| R:
5′-TGATCACCTGGTTTCCCACC-3′ | |
| COL10A1 | F:
5′-AAAGGTCATGCTGGAGAGCC-3′ | 239 |
| R:
5′-TCATAGTGCTGTTGCCCGTT-3′ | |
| Elastin | F:
5′-GGAAAGTACCAGGTGTGGGG-3′ | 338 |
| R:
5′-CCCTGTCCCTGTTGGGTAAC-3′ | |
| GAPDH | F:
5′-CCTCAACGACCACTTCGTCA-3′ | 237 |
| R:
5′-GGGTCTGGGATGGAAACTGG-3′ | |
Statistical analysis
Statistical evaluation was performed using Student's
t test. Statistical analysis was performed using SPSS
version 16.0 (SPSS Inc., Chicago, IL, USA). Results are expressed
as the mean ± standard deviation. P<0.05 was considered to
indicate a statistically significant difference between values.
Results
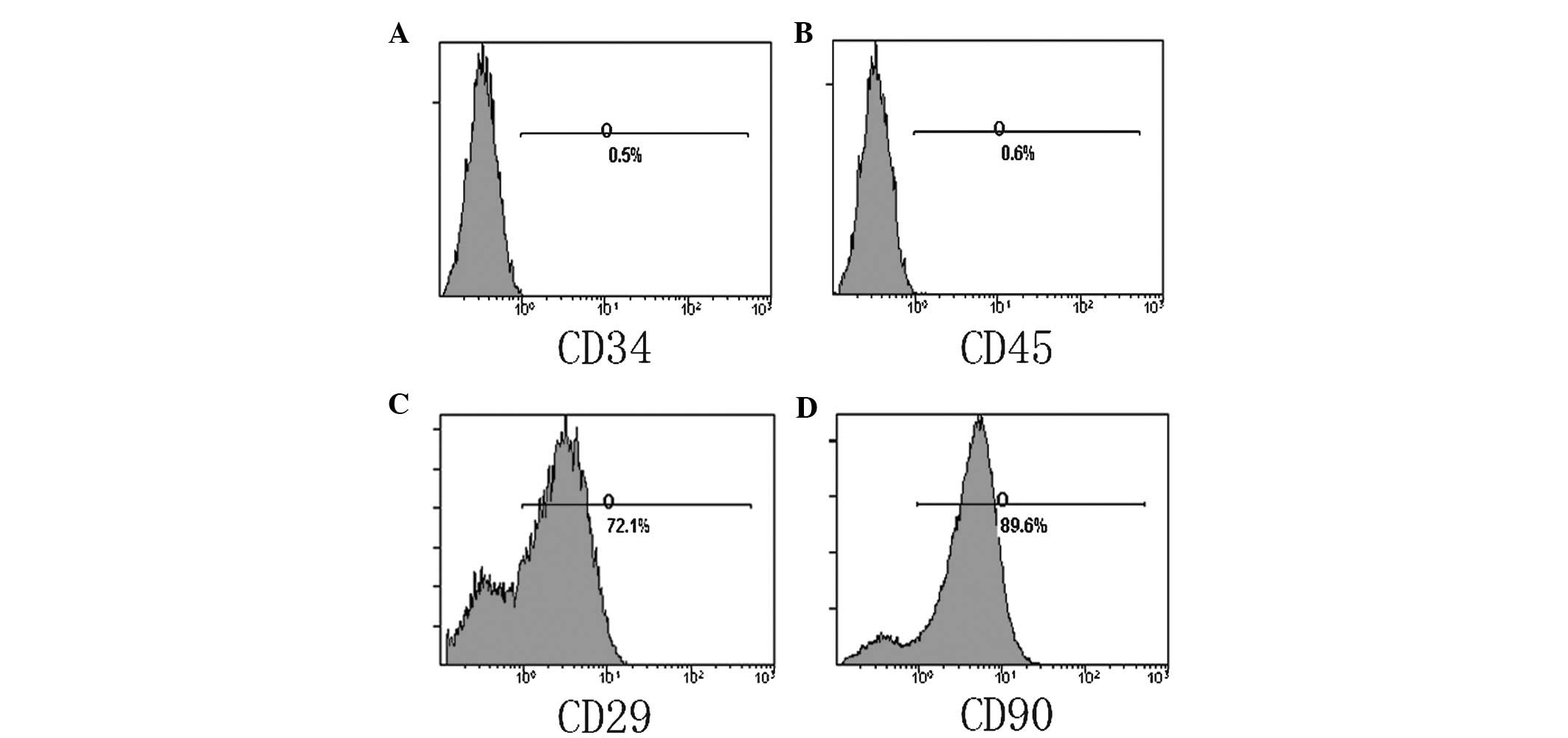
Flow cytometric analysis
Flow cytometry indicated that the cell-surface
markers CD29 and CD90 were highly expressed on BMSCs, while cells
were negative for the hematopoietic cell-specific markers CD34 and
CD45 (Fig. 1).
Cytomorphology
BMSCs cultured in the supernatant of chondrocytes
changed from spindle-shaped into polygonal cells with increasing
induction time, while BMSCs remained in a spindle- or plate-like
shape in the control group (Fig.
2).
In order to investigate the feasibility of
chondrogenesis of BMSCs, they were cultured in the supernatant of
auricle chondrocytes. At the end of the first week, polygonal cells
began to be distinguished, and cells then changed shape from
spindle- to cobblestone-like appearance over the next two weeks
(Fig. 2), which suggested the
positive chondro-induction of the chondrocytic supernatant.
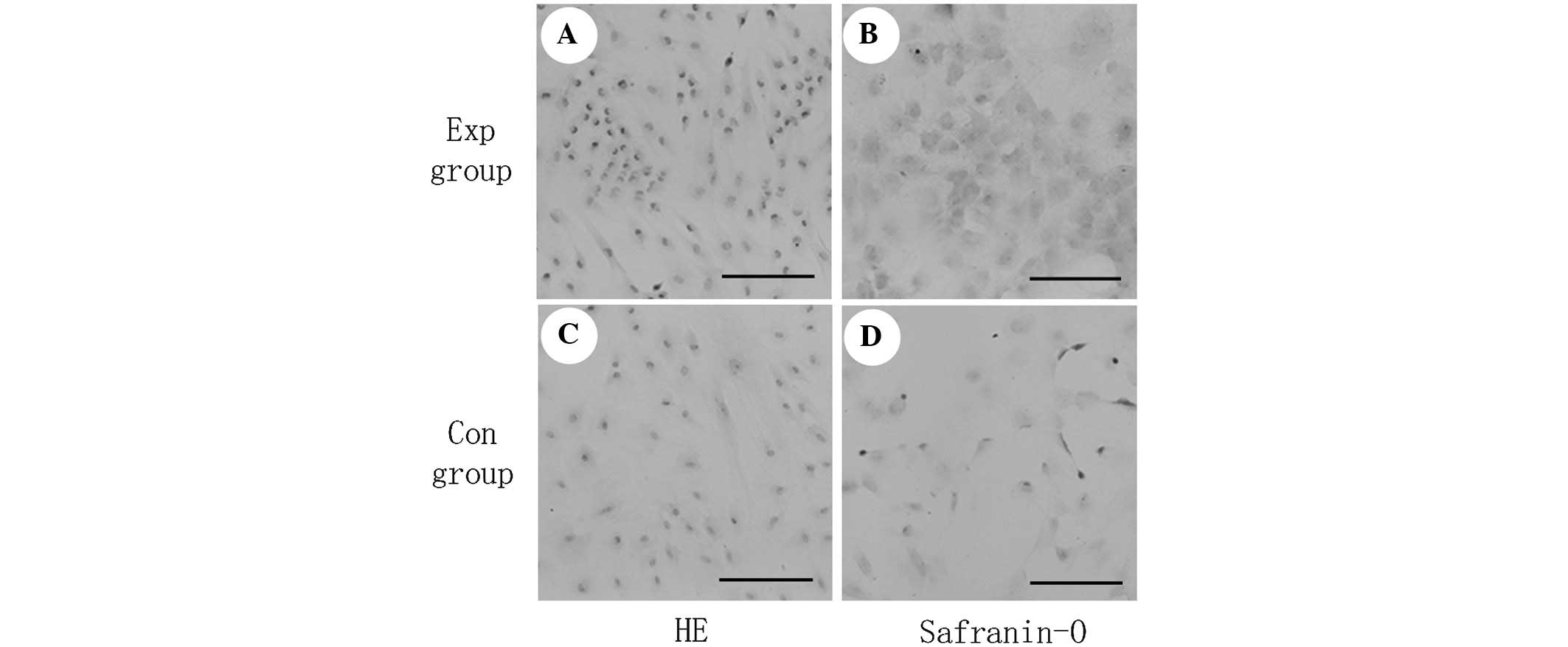
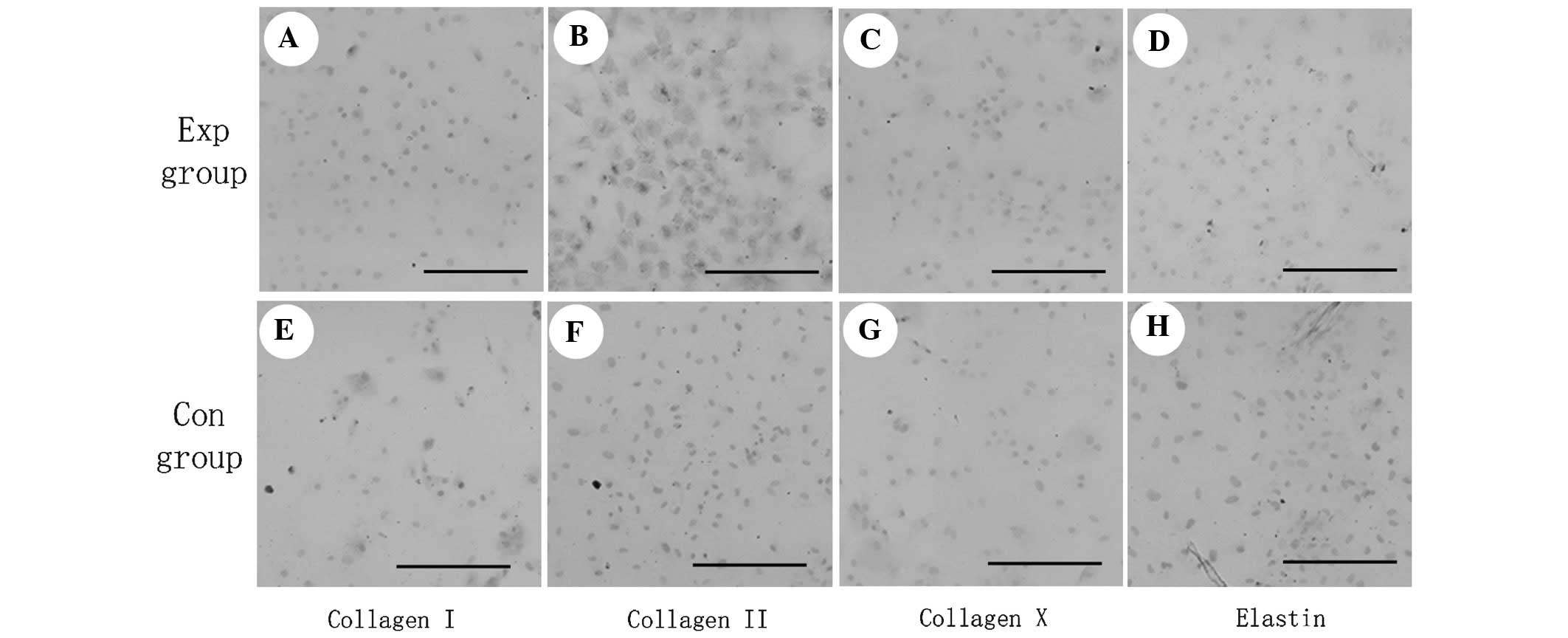
Histological and immunohistochemical
staining
Histological and immunohistochemical tests were
employed to evaluate the chondrogenesis of BMSCs. The pink staining
of safranin O (Fig. 3) revealed
the production of glycosaminoglycan, which was secreted by mature
chondrocytes. Furthermore, alongside the morphological changes,
immunohistochemical analysis showed positive staining for type II
collagen and elastin, whereas the expression of type I and X
collagen was inhibited (Fig. 4).
The above results indicated that the chondrogenic differentiation
of BMSCs was improved by the auricle-chondrocyte supernatant, while
no hypotrophy was present (Fig.
4). It has been reported that collagen I is an
osteogenesis-associated marker and used to assess matrix synthesis
during osteoblastic differentiation of BMSCs (23). In addition, collagen X is an
important hypertrophic marker of MSCs (24).
Gene expression
RT-PCR analysis showed significant upregulation of
type II collagen and elastin, and significant downregulation of
type I and X collagen (P<0.05), which was in agreement with the
results of the immunohistochemical analysis.
Discussion
BMSCs, also known as mesenchymal stem cells (MSCs),
obtained from the aspiration of bone marrow, are multipotent cells
capable of differentiating into cartilage, and are extensively
employed in cartilage tissue engineering (19,22,25).
The chondrogenesis of BMSCs is a complex and tightly regulated
process, and to date, the exact underlying molecular mechanisms
have remain to be fully elucidated. It is challenging to create a
mimetic chondrogenesis microenvironment through application of
TGF-β and dexamethone (26).
Therefore, in the present study, the supernatant of auricle
chondrocytes was used to mimic the chondrogenic differentiation
environment in vitro. The objective of the present study was
to investigate the chondrogenic differentiation of BMSCs cultivated
in the supernatant of auricle chondrocytes. In order to test the
properties of BMSCs, flow cytometry was used to detect stem cell
surface markers. The BMSCs were then subjected to
elastic-chondrocyte differentiation by culturing them in the
supernatant of the auricle chondrocytes. Next, histological
analysis was performed to evaluate the capacity of
elastic-cartilage production. The results showed that the
supernatant of chondrocytes had beneficial effects on the
chondrogenic differentiation of BMSCs.
The whole-blood adherent method was employed in the
present study to obtain BMSCs (27). The surface markers CD29 and CD90
were highly expressed in bone marrow-derived stem cells, while the
hematopoietic cell-specific markers CD34 and CD45 were not
expressed. A previous study demonstrated that CD90 was associated
with the chondrocytic differentiation of MSCs, and it was
predominantly expressed in proliferating cells (28). The finding that the surface marker
CD90 of BMSCs was highly expressed in the present study was in line
with the identification of the capacity of stem cells for
mulltilineage differentiation (10). Furthermore, CD90 is regarded to be
an important indicator of the chondrogenic differentiation of
synovium-derived stem cells (SDSCs) (29). CD29, an integrin sub-unit
associated with cell adhesion, is involved in antigen recognition,
embryogenesis, hemostasis, tissue restoration and cell migration
(27). Apart from that, its
expression was shown to indicate the chondrogenic differentiation
potency of BMSCs, and to have an important role in the
chondrogenesis of SDSCs (27,28).
Direct or indirect chondrocyte-based co-culture of
MSCs is thought to be a protocol to generate tissue-engineered
cartilage (15,17,19).
In the co-culture system, chondrogenic differentiation of MSCs has
been shown to require the use of either high-density cell pellet or
a scaffold allowing for 3-dimensional culture (15,30).
However, Potier et al (31)
reported that micro-aggregates had no positive effects on the
chondrocytic differentiation of BMSCs. There is currently no
consensus regarding the underlying mechanism of the stimulating
effect of chondrocytes on MSC-derived chondrogenesis in co-culture
systems (24,32,33).
Zuo et al (33) suggested
that the direct physical contact between chondrocytes and BMSCs has
an dominant role, while Fischer et al (17) ascribed the effect to parathyroid
hormone-related protein secreted by chondrocytes. The present study
utilized a mono-co-culture system without the presence of
chondrocytes to provide an improved protocol for the chondrogenic
differentiation of BMSCs and to investigate its underlying
mechanism. The results of the present study confirmed that the
inductive effects of chondroctyes on BMSCs to differentiate was
mediated by soluble factors alone, which were present in the
supernatant of chondrocytes used for co-culture.
In the present study, it was observed BMSCs began to
change their appearance in the first week from the original
spindle-like shape to a polygonal shape, and chondrocyte-like cells
accumulated with time. Immunohistochemical analysis of type II
collagen and glycosaminoglycan (GAG) further confirmed that the
supernatant of chondrocytes had an inductive effect on the
differentiation of BMSCs, and the chondrocyte-like cells generated
from BMSCs showed similar features to those of mature chondrocytes
in terms of cartilage-specific collagen production. Collagen type
II, the main collagen of the collagen matrix, is the
cartilage-specific matrix (34,35).
In the present study, type II collagen was present, indicated by an
intensive positive staining in the cytoplasm and the pericellular
space in the cell sheeting, while staining for type I and X
collagen was negative. The ratio of expression of collagen type
II-to-I is a well-defined index of chondrocyte differentiation
(36). Type I collagen, a marker
for de-differentiation and fibration, is the prominent structural
element in fibrous cartilage (36–38).
Collagen X, an important hypertrophic marker of MSCs, was not
present according to immunohistochemical analysis, which suggested
that the soluble factors secreted by chondrocytes were able to
downregulate the expression of type I and X collagen and suppress
hypertrophy of BMSCs (24). The
chondro-induced BMSCs were positive for elastin, an elastic
cartilage-specific marker, following the 28-day culture period. The
highly elastic mechanical character of elastic cartilage attributes
the elasticity of the fiber (39).
In conclusion, the supernatant of elastic cartilage
cells was able to induce BMSCs to differentiate into elastic
cartilage cells, which may be a promising method for constructing
certain sub-types of tissue-engineered cartilage.
Acknowledgments
The present study was supported by grants from the
National Natural Science Foundation of China (grant no. 81272128)
and the National 863 program (grant nos. SS2014 and AA020705). The
authors appreciate the technical support from Mrs. Lijuan Zong, and
Mrs. Juanjuan Wu at the Shanghai Key Laboratory of Tissue
Engineering (Shanghai 9th People's Hospital, Shanghai Jiao Tong
University School of Medicine, Shanghai, China).
References
|
1
|
Hwang CM, Lee BK, Green D, Jeong SY, Khang
G, Jackson JD, Atala A, Lee SJ and Yoo JJ: Auricular reconstruction
using tissue-engineered alloplastic implants for improved clinical
outcomes. Plast Reconstr Surg. 133:360e–369e. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wachsmuth L, Söder S, Fan Z, Finger F and
Aigner T: Immunolocalization of matrix proteins in different human
cartilage subtype. Histol Histopathol. 21:477–485. 2006.PubMed/NCBI
|
|
3
|
Suutarla S, Rautio J and Klockars T: The
learning curve in microtia surgery. Facial Plast Surg. 25:164–168.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wilkes GH: Learning to perform ear
reconstruction. Facial Plast Surg. 25:158–163. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bichara DA, O'Sullivan NA, Pomerantseva I,
et al: The tissue-engineered auricle: past, present and future.
Tissue Eng Part B Rev. 18:51–61. 2012. View Article : Google Scholar
|
|
6
|
Reiffel AJ, Kafka C, Hernandez KA, et al:
High-fidelity tissue engineering of patient-specific auricles for
reconstruction of pediatric microtia and other auricular
deformities. PLoS One. 8:e565062013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sterodimas A, de Faria J, Correa WE and
Pitanguy I: Tissue engineering and auricular reconstruction: a
review. J Plast Reconstr Aesthet Surg. 62:447–452. 2009. View Article : Google Scholar
|
|
8
|
Nayyer L, Patel KH, Esmaeili A, et al:
Tissue engineering: revolution and challenge in auricular cartilage
reconstruction. Plast Reconstr Surg. 129:1123–1137. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Patel KH, Nayyer L and Seifalian AM:
Chondrogenic potential of bone marrow-derived mesenchymal stem
cells on a novel, auricular-shaped, nanocomposite scaffold. J
Tissue Eng. 4:20417314135167822013. View Article : Google Scholar
|
|
10
|
Pittenger MF, Mackay AM, Beck SC, et al:
Multilineage potential of adult human mesenchymal stem cells.
Science. 284:143–147. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Abrahamsson CK, Yang F, Park H, et al:
Chondrogenesis and mineralization during in vitro culture of human
mesenchymal stem cells on three-dimensional woven scaffolds. Tissue
Eng Part A. 16:3709–3718. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mueller MB and Tuan RS: Functional
characterization of hypertrophy in chondrogenesis of human
mesenchymal stem cells. Arthritis Rheum. 58:1377–1388. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pelttari K, Winter A, Steck E, et al:
Premature induction of hypertrophy during in vitro chondrogenesis
of human mesenchymal stem cells correlates with calcification and
vascular invasion after ectopic transplantation in SCID mice.
Arthritis Rheum. 54:3254–3266. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Qing C, Wei-ding C and Wei-min F:
Co-culture of chondrocytes and bone marrow mesenchymal stem cells
in vitro enhances the expression of cartilaginous extracellular
matrix components. Braz J Med Biol Res. 44:303–310. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang L, He A, Yin Z, et al: Regeneration
of human-ear-shaped cartilage by co-culturing human microtia
chondrocytes with BMSCs. Biomaterials. 35:4878–4887. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Acharya C, Adesida A, Zajac P, et al:
Enhanced chondrocyte proliferation and mesenchymal stromal cells
chondrogenesis in coculture pellets mediate improved cartilage
formation. J Cell Physiol. 227:88–97. 2012. View Article : Google Scholar
|
|
17
|
Fischer J, Dickhut A, Rickert M and
Richter W: Human articular chondrocytes secrete parathyroid
hormone-related protein and inhibit hypertrophy of mesenchymal stem
cells in coculture during chondrogenesis. Arthritis Rheum.
62:2696–2706. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hwang NS, Varghese S, Puleo C, Zhang Z and
Elisseeff J: Morphogenetic signals from chondrocytes promote
chondrogenic and osteogenic differentiation of mesenchymal stem
cells. J Cell Physiol. 212:281–284. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xue K, Zhu Y, Zhang Y, Chiang C, Zhou G
and Liu K: Xenogeneic chondrocytes promote stable subcutaneous
chondrogenesis of bone marrow-derived stromal cells. Int J Mol Med.
29:146–152. 2012.
|
|
20
|
Friedenstein AJ, Chailakhjan RK and
Lalykina KS: The development of fibroblast colonies in monolayer
cultures of guinea-pig bone marrow and spleen cells. Cell Tissue
Kinet. 3:393–403. 1970.PubMed/NCBI
|
|
21
|
Xu LQ, Huang Y-W, Luo R-Z and Zhang Y-N:
Establishment of the retroperitoneal lymph node metastasis model of
endometrial VX2 carcinoma in rabbits and observation of its
metastatic features. World J Surg Oncol. 13:1092015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xue K, Qi L, Zhou G and Liu K: A two-step
method of constructing mature cartilage using bone marrow-derived
mesenchymal stem cells. Cells Tissues Organs. 197:484–495. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zheng B, Jiang J, Luo K, Liu L, Lin M,
Chen Y and Yan F: Increased osteogenesis in osteoporotic bone
marrow stromal cells by overexpression of leptin. Cell Tissue Res.
2015.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bian L, Zhai DY, Mauck RL and Burdick JA:
Coculture of human mesenchymal stem cells and articular
chondrocytes reduces hypertrophy and enhances functional properties
of engineered cartilage. Tissue Eng Part A. 17:1137–1145. 2011.
View Article : Google Scholar :
|
|
25
|
He F, Chen X and Pei M: Reconstruction of
an in vitro tissue-specific microenvironment to rejuvenate
synovium-derived stem cells for cartilage tissue engineering.
Tissue Eng Part A. 15:3809–3821. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Vinardell T, Thorpe SD, Buckley CT and
Kelly DJ: Chondrogenesis and integration of mesenchymal stem cells
within an in vitro cartilage defect repair model. Ann Biomed Eng.
37:2556–2565. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yang YH, Lee AJ and Barabino GA:
Coculture-driven mesenchymal stem cell-differentiated articular
chondrocyte-like cells support neocartilage development. Stem Cells
Transl Med. 1:843–854. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lu T, Huang Y, Wang H, Ma Y and Guan W:
Multi-lineage potential research of bone marrow-derived stromal
cells (BMSCs) from cattle. Appl Biochem Biotechnol. 172:21–35.
2014. View Article : Google Scholar
|
|
29
|
Diaz-Romero J, Gaillard JP, Grogan SP,
Nesic D, Trub T and Mainil-Varlet P: Immunophenotypic analysis of
human articular chondrocytes: changes in surface markers associated
with cell expansion in monolayer culture. J Cell Physiol.
202:731–742. 2005. View Article : Google Scholar
|
|
30
|
Albrecht C, Tichy B, Nurnberger S, et al:
Gene expression and cell differentiation in matrix-associated
chondrocyte transplantation grafts: a comparative study.
Osteoarthritis Cartilage. 19:1219–1227. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Potier E, Rivron NC, Van Blitterswijk CA
and Ito K: Micro-aggregates do not influence bone marrow stromal
cell chondrogenesis. J Tissue Eng Regen Med. Apr 2–2014.Epub ahead
of print. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Leppaluoto J, Zeytin F, Ueno N, Ying SY,
Ling N and Guillemin R: Myelin basic protein present in the acid
extracts of rat hypothalami releases insulin and glucagon from
isolated rat pancreatic islets. Acta Physiol Scand. 134:253–261.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zuo Q, Cui W, Liu F, Wang Q, Chen Z and
Fan W: Co-cultivated mesenchymal stem cells support chondrocytic
differentiation of articular chondrocytes. Int Orthop. 37:747–752.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Little CJ, Bawolin NK and Chen X:
Mechanical properties of natural cartilage and tissue-engineered
constructs. Tissue Eng Part B Rev. 17:213–227. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kuhne M, John T, El-Sayed K, et al:
Characterization of auricular chondrocytes and auricular/articular
chondrocyte co-cultures in terms of an application in articular
cartilage repair. Int J Mol Med. 25:701–708. 2010.PubMed/NCBI
|
|
36
|
Hong E and Reddi AH: Dedifferentiation and
redifferentiation of articular chondrocytes from surface and middle
zones: changes in microRNAs-221/-222, -140 and -143/145 expression.
Tissue Eng Part A. 19:1015–1022. 2013. View Article : Google Scholar
|
|
37
|
Cheng T, Maddox NC, Wong AW, Rahnama R and
Kuo AC: Comparison of gene expression patterns in articular
cartilage and dedifferentiated articular chondrocytes. J Orthop
Res. 30:234–245. 2012. View Article : Google Scholar
|
|
38
|
von der Mark K, Gauss V, von der Mark H
and Müller P: Relationship between cell shape and type of collagen
synthesised as chondrocytes lose their cartilage phenotype in
culture. Nature. 267:531–532. 1977. View
Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mizuno M, Takebe T, Kobayashi S, et al:
Elastic cartilage reconstruction by transplantation of cultured
hyaline cartilage-derived chondrocytes. Transplant Proc.
46:1217–1221. 2014. View Article : Google Scholar : PubMed/NCBI
|