Introduction
Rhinosinustitis is one of the most prevalent upper
airway problems (1). Despite the
severe morbidity and impairment to the patient's quality of life,
the therapeutic options are limited and recurrence is common
(2). One of the most severe
subtypes is chronic rhinosinusitis with hyperplastic sinonasal
polyposis, the effects of which is marked as mucosal hyperplasia
and tissue remodeling often exists. Often, the sinonasal polyposis
requires surgical intervention, although recurrence is inevitable
(3). Consequently, it remains
critical to identify an internal medicine therapeutic solution. It
is reported that vascular endothelial growth factor (VEGF) is key
in the promotion of nasal epithelial cell growth and the inhibition
of apoptosis, which results in hyperplastic sinonasal polyposis
(4). Therefore, the present study
hypothesized that downregulation of the local expression of VEGF
may suspend the progress of chronic rhinosinustitis and prevent its
substantial effects.
RNA interference technology represents a novel
target gene silencing method. By internalizing of specific small
interfering RNA (siRNA), it can bind to target mRNA, leading to
cleavage of the mRNA and silencing of the target gene (5). This convenient and effective
technique is extensively used in various areas, including cancer
therapy (6), regenerative medicine
(7), anti-viral therapy (8) and anti-inflammatory treatment
(9), therefore, siRNA targetting
VEGF may be a therapeutic molecule in chronic rhinosinustitis.
Chitosan is a natural cationic polymer with positive charge, and
has been used as an important siRNA non-viral vector due to its
advantages, including lower cost and notable cytocompatibility
(10). A vital property of
chitosan is mucosa adhesion, which suggests that chitosan may be a
suitable drug delivery carrier in mucosa lesions (11). In addition, chitosan-based
thermosensitive hydrogel, also known as injectable hydrogel, which
is fluid at low temperature and solid at body temperature, can
retain siRNA for a prolonged duration (12,13)
and may be suitable for sinus injection.
In the present study, siRNA targeting VEGF (siVEGF)
was delivered into nasal epithelial cells in injectable chitosan
hydrogel to obtain localized sustained VEGF silencing. Subsequent
analysis of cell proliferation and the cytoskeleton were performed
to evaluate the in vitro biofunction, and mucosal thickness
was determined to assess the degree of inflammation following
injection of the hydrogel into the maxillary sinus of a chronic
rhinosinusitis animal model.
Materials and methods
Materials
Chitosan (Mw, 100~300 kDa; DD=93.37%), sodium
β-glycerophosphate (β-GP), 3-(4,5- dimethylthiazol-2yl)-2,
5-diphenyltetrazolium bromide (MTT) and dimethyl sulfoxide (DMSO)
were purchased from MP Biomedicals, Santa Ana, CA, USA. Fluorescein
isothiocyanate (FITC)-conjugated phalloidin, DAPI and the live/dead
cell staining kit were purchased from Nanjing KeyGen Biotech. Co.,
Ltd. (Nanjing China). Human VEGF siRNA (sense
5′-GGAGUACCCUGAUGAGAUCdTdT-3′; antisense
5′-GAUCUCAUCAGGGUACUCCdTdT-3′) and siRNA nega-tive control (sense
5′-UUCUCCGAACGUGUCACGUTT-3′; antisense 5′-ACGUGACACGUUCGGAGAATT-3′)
were purchased from Shanghai Genepharma, Co., Ltd. (Shanghai,
China). The RiboGreen kit and TRIzol reagent was purchased from
Invitrogen Life Technologies (Carlsbad, CA, USA). The PrimeScript™
RT reagent kit and SYBR Premix Ex™ Taq II were purchased from
Takara Bio, Inc. (Otsu, Japan). The Human VEGF Enzyme-Linked
Immunosorbent Assay (ELISA) kit was purchased from
antibodies-online GmbH (Aachen, Germany).
Fabrication of the hydrogel
The injectable chitosan hydrogel was fabricated,
according to a previous report (12). Briefly, chitosan was dissolved in
1% acetic acid at a concentration of 2% w/v. The β-GP was prepared
in distilled water at a 1 mg/ml concentration. To fabricate the
hydrogel, 1.8 ml chitosan solution was stirred constantly at 4°C,
and 0.2 ml β-GP solution was added in a drop-wise manner. The
hydrogel spontaneously became solid during incubation at 37°C for 8
min (Fig. 1). To incorporate the
siRNA, pre-calculated siRNA (5 µg) was added into the 200
µl liquid solution at 4°C prior to the gel formation.
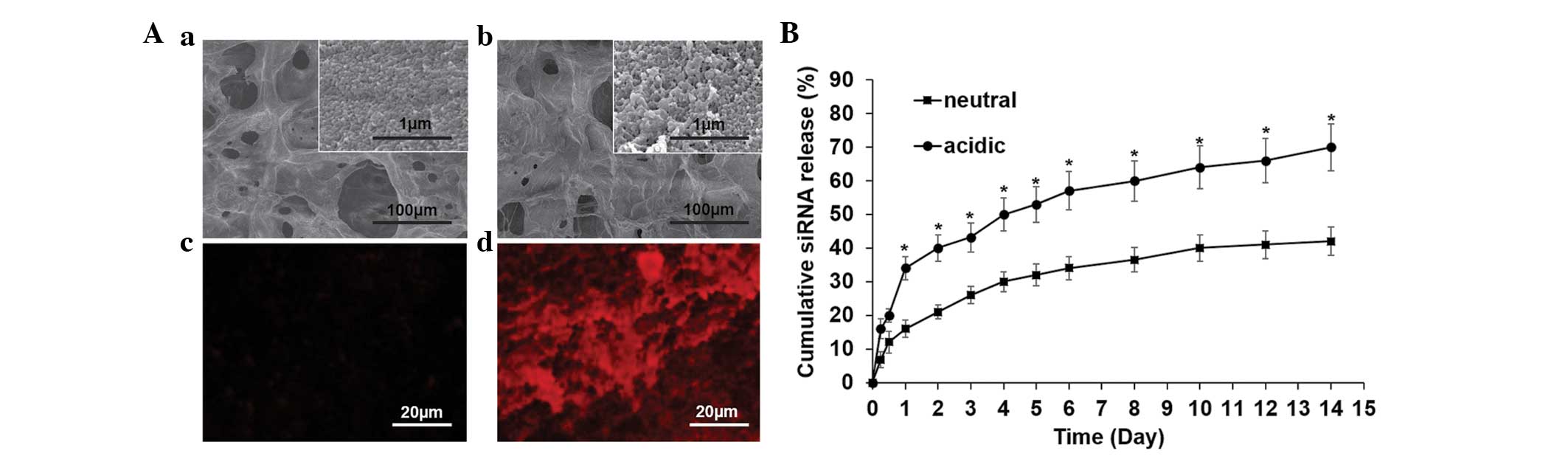
Characterization of the gel
The gels, which had been either loaded with siRNA or
were siRNA-free, were freeze-dried and sputter coated with
platinum. The gels were then observed using a scanning electron
microscope (SEM; S-4800; Hitachi, Ltd., Toyko, Japan). In addition,
Cy3-labeled siRNA (Cy3-siRNA) was used during gel formulation and
was observed using a fluorescence microscope (Olympus Corporation,
Toyko, Japan).
The in vitro siRNA release profile was
determined separately under neutral (pH 7.4) and acidic (pH 5.5)
phosphate-buffered saline (PBS). Specifically, the hydrogel was
soaked in the respective PBS and incubated under cell culture
conditions for 2 weeks. At predetermined time-points, the elution
was collected and replaced with fresh buffer. The released siRNA in
the supernatant was quantified using the RiboGreen kit, according
to the manufacturer's instructions. Briefly, 100 µl sample
was thoroughly mixed with 100 µl RiboGreen in the dark. Each
sample was duplicated three times and the fluorescence intensity
was measured using a fluorescence plate reader (TECAN Infinite
M200; Tecan, Männedorf, Switzerland) at the excitation and emission
wavelengths of 546 and 596 nm, respectively. Fresh PBS was used as
blank control and the relative fluorescent units (RFUs) were
determined by subtracting the blank fluorescence intensity. The
siRNA was calculated using a calibration curve and the percentage
of cumulative release was calculated using Microsoft Excel 2013
(Microsoft, Redmond, VA, USA).
Cell culture and seeding
The 16HBE bronchial epithelial cell line was
cultured in bronchial epithelial basal medium (Biosource,
Camarillo, TX, USA). The cell seeding method used was in accordance
to that of a previous report with modification (14). The culture conditions were 37°C in
5% CO2 and 100% humidity. When the confluence of the
cells was at ~80%, the cells were trypsinized (0.25% trypsin and
0.01% EDTA; GE Healthcare Life Sciences, Logan, UT, USA and the
density adjusted to 2×106 cells/ml. Subsequently, 200
µl was added to the gel and placed in a 24-well tissue
culture plate (TCP), 1 µl medium was supplemented following
4 h attachment.
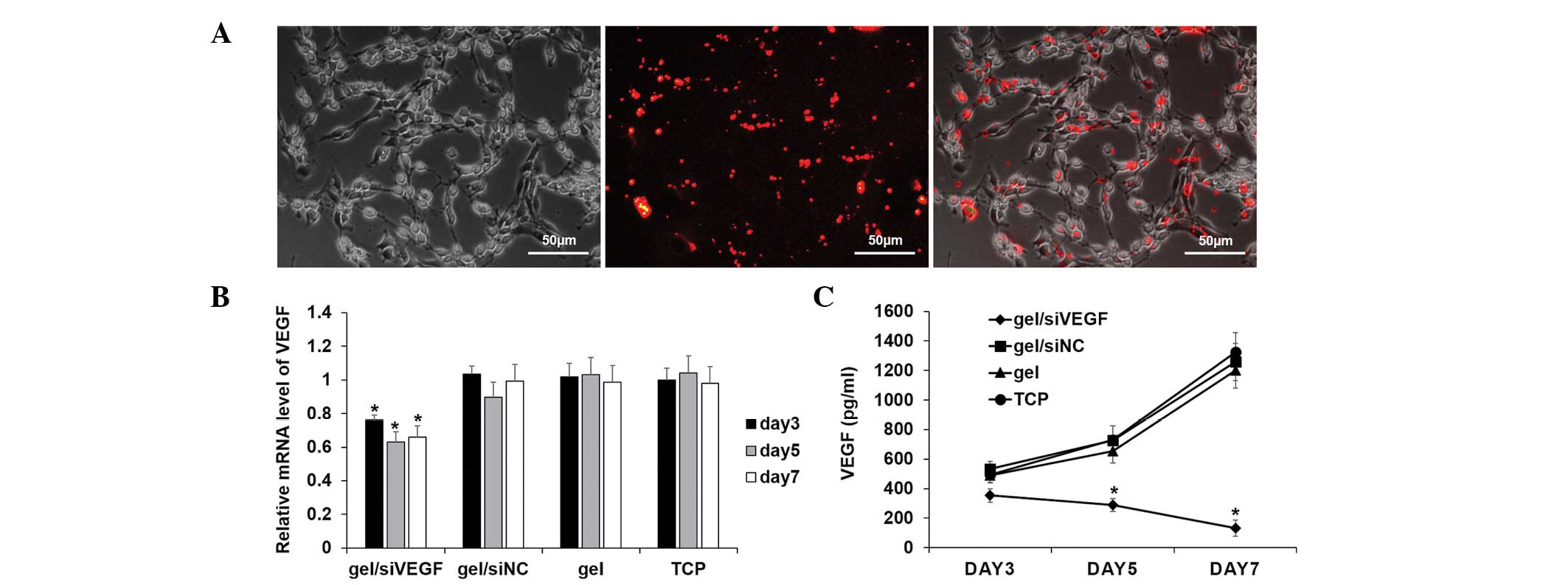
siRNA uptake and gene knockdown
To determine the uptake of siRNA from the gel, the
Cy3-labeled human VEGF siRNA (Cy3-siRNA) was loaded and incubated
with the cells for 24 h. The cells were then trypsinized from the
gel and re-seeded onto the TCP. The cells were allowed to attach
for another 24 h and observed using a fluorescence microscope.
At pre-determined time-points, the cells were lysed
with TRIzol reagent, and the total RNA was extracted using
chloroform and precipitated in isopropanol (Tianjin Kemiou Chemical
Reagent Co., Ltd., Tianjin, China). Following quantification by
measurement of optical density (OD) at the wavelength of 260 nm
using an Epoch plate reader (BioTek Instruments, Winooski, VT,
USA), 1 µg total RNA was used reverse transcribed into cDNA
using the PrimeScript™ RT reagent kit. The mRNA expression of
target VEGF was analyzed using quantitative polymerase chain
reaction (qPCR) with an SYBR Premix ExTM Taq II kit (Takara Bio,
Inc.). The primers used were as follows: Human VEGF sense
5′-GCACCCATGGCAGAAGGAGG-3′ and antisense
5′-CCTTGGTGAGGTTTGATCCGCATA-3′; human GAPDH sense
5′-CGGATTTGGTCGTATTGGGC-3′ and antisense
5′-GTCATACCAGGAAATGAGCTTG-3′. A 10 µl system was used,
containing 5 µl SYBR Premix, 1 µl forward primer, 1
µl reverse primer and 3 µl cDNA. The thermocycling
was repeated between 95°C (15 sec) and 60°C (30 sec) for 40 cycles.
The expression was determined by the threshold cycle (Ct) value of
each well. The protein level of VEGF in cell supernatants were
determined using ELISA kits, according to the manufacturer's
instructions. Briefly, the samples were incubated in human VEGF
antibody-coated wells and colorized using horesradish peroxidase
catalysis. The absorbance was read at 450 nm and the concentration
was calculated based on the calibration curve. Data are expressed
as per µg total protein, which was measured using a
bicinchoninic acid assay kit (Sigma-Aldrich).
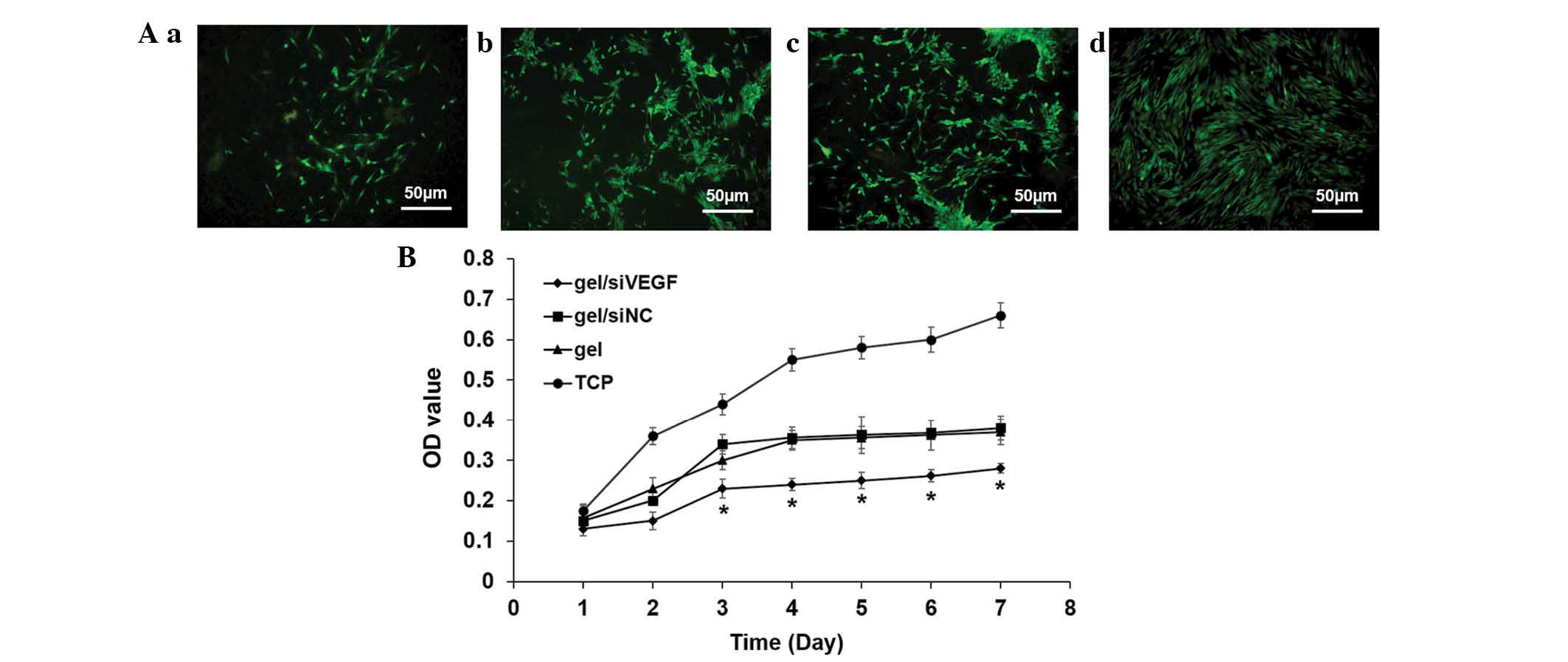
Proliferation analysis and staining for
determination of cell death
The proliferation of the cells grown on the
different substrate gels were analyzed continuously using an MTT
assay. Briefly, the cells were incubated with MTT reaction solution
(5 mg/ml MTT: medium, 1:4) for 4 h at 37°C. Subsequently, the
supernatants were gently removed and the precipitation was
completely dissolved in DMSO. The OD value was measured using a
spectrometer at 490 nm. Following 3 days of culture, the medium was
removed and the cells were rinsed with PBS. The cells were then
stained using the Live/Dead cells staining kit and observed using a
fluorescence microscope.
Actin cytoskeletal staining
Following 3 days of culture on the hydrogel, the
cells were fixed in 4% paraformaldehyde (Beijing Leagene Biotech
Co., Ltd., Beijing, China) and then permeabilized with 0.1%
Triton-X100 (Beijing Leagene Biotech Co., Ltd.). To reveal the
actin cytoskeleton, the cells were stained with FITC-conjugated
phalloidin solution (50 mg/ml in PBS) for 20 min at room
temperature. The unbound dye was washed thoroughly with PBS and the
samples were observed under a fluorescence microscope.
Animal model establishment and hydrogel
injection
The animal procedures used in the present study were
approved by the research ethics committee of the Medical School of
Ningbo University (Ningbo, China). A total of 20 male
Sprague-Dawley rats (6–8 weeks old) were purchased from the School
of Medicine, Ningbo University (Ningbo, China) and each group
contained five rats. The rats were housed separately at 20–25°C
under a 12-h light/dark cycle and fed a normal diet. The chronic
rhinosinusitis animal model was established according to a previous
report (15). Following
establishment of the model, the hydrogel containing the different
siRNA was injected (10 µl), immediately following
formulation, into the bilateral maxillary sinus. The animal was
sacrificed 2 weeks post-injection via intra-abdominal overdose of
pentobarbital sodium solution, and the sinus was isolated carefully
for further analysis.
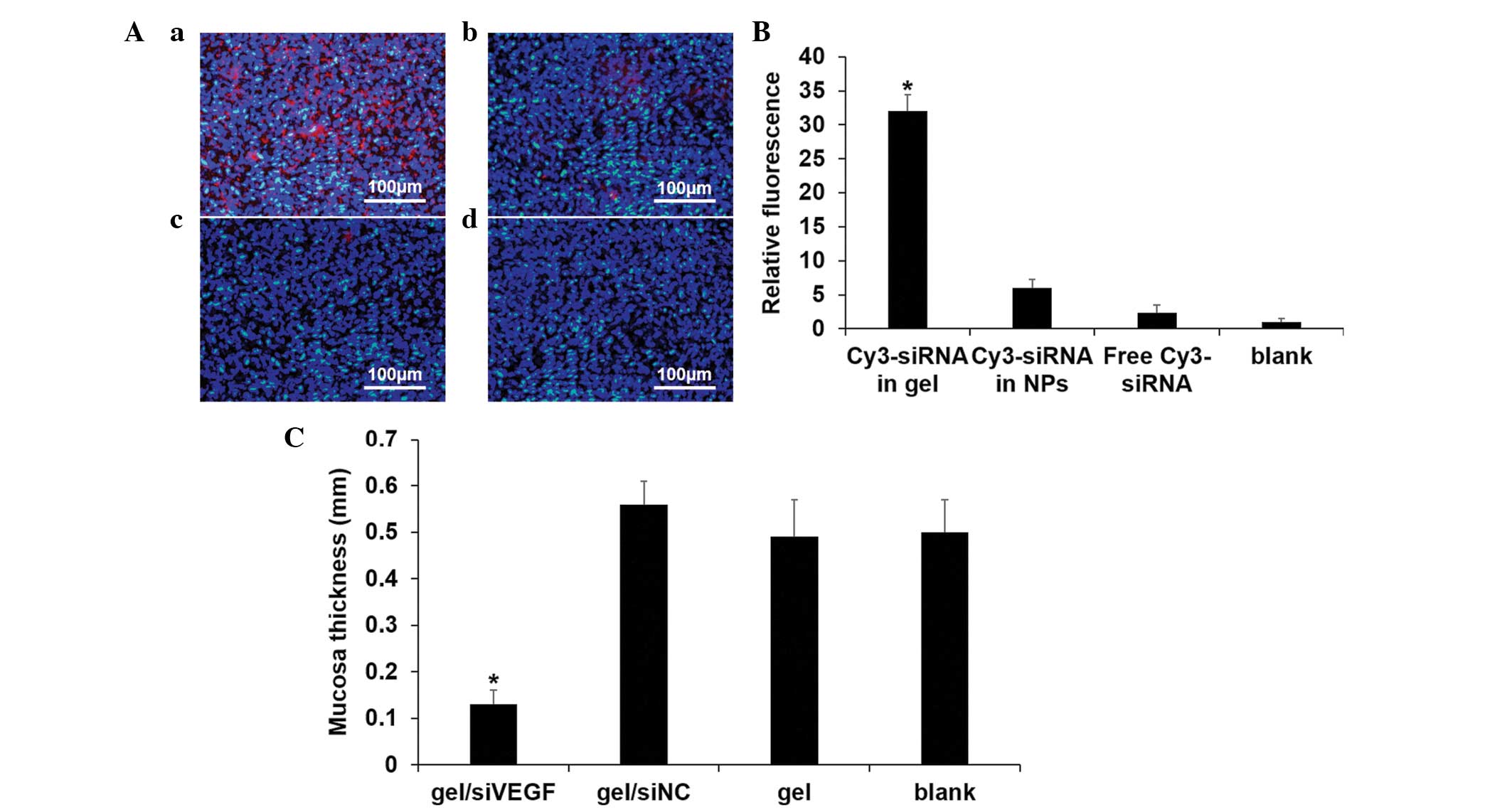
Prolonged mucosal siRNA delivery and
measurement of mucosal thickness
The Cy3-labeled siRNA had been incorporated into the
gel prior to injection, with the same quantity of siRNA in the
chitosan/siRNA nanoparticles (NPs) or free siRNA injected.
Following animal sacrifice, the sinus mucosa was stripped off and
the thickness of the sinus mucosa was measured using graduated
probe at five randomly-selected points. The sample was then fixed
in 4% paraformaldehyde and cryosectioned, followed by DAPI
staining. The quantitative siRNA concentrations were determined
according to previous report (16). Briefly, the mucosa was homogenized
and mixed with lysis buffer (0.1% sodium dodecyl sulfate in PBS;
Beijing Leagene Biotech Co., Ltd.) and incubated at 65°C for 10
min, followed by the addition of methanol and incubation for a
further 10 min. The sample was then centrifuged at 12,000×g for 5
min at 4°C, and 200 µl of the supernatant was transferred to
a black 96-well plate (Corning Incorporated, Corning, NY, USA). The
fluorescence intensity of the sample was measured using an Epoch
plate reader (λex, 554 nm; λem, 568 nm). The concentration of
Cy3-siRNA in each sample was calculated from a standard curve.
Statistical analysis
All experiments were performed triplicates and are
presented as the mean ± standard deviation. One-way analysis of
variance and the Student-Newman-Keuls test were performed to
analyze the data using SPSS 22.0 (IBM SPSS, Armonk, NY, USA).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Characterizations of the hydrogel
The hydrogel was visualized using SEM and a
fluorescence microscope separately (Fig. 2A). The gel exhibited a porous
structure with numerous protuberant particles (Fig. 2Aa). Following the loading of siRNA,
the porous structure exhibited minimal change, however the
particles became more visible (Fig.
2Ab). Compared with the siRNA-free gel (Fig. 2Ac), loading of Cy3-siRNA produced a
self-organized red fluorescence signal (Fig. 2Ad). The siRNA release profile from
the gel was then determined. The release profile under different pH
values was determined within 2 weeks to simulate the natural body
fluid condition. The siRNA release occurred gradually under neutral
conditions, without apparent initial burst release, and siRNA was
maintained for a prolonged duration (Fig. 2B). When the gel was exposed to the
acidic condition, the release rate was markedly increased and a
burst release was observed within the first day (Fig. 2B).
Uptake of siRNA and target gene
silencing
The cells were detached from the Cy3-siRNA-loaded
hydrogel and reattached onto a tissue culture plate to observe the
uptake behavior. As indicated, almost all the red fluorescence
signals were observed within the cells (Fig. 3A). The in vitro capability
of the target silencing effect within the 16HBE cells was first
analyzed (Fig. 3B). The mRNA level
of VEGF was suppressed by ~20% at day 3, and the silencing effect
was higher on days 5 and 7, by ~40% (Fig. 3B). In agreement with the results of
the qPCR analysis, the protein level of VEGF in supernatant was
markedly downregulated on the gel loaded with siVEGF (Fig. 3C).
Inhibition of cell proliferation
Following 3 days culture, the number of living cells
deceased on all the gels, compared with the TCP and was
significantly reduced on the gel loaded with siVEGF (Fig. 4A). The cell vitality was monitored
continuously for 1 week to determine the proliferation. Regardless
of the type of gel loading, the cell proliferation was
down-regulated, compared with the TCP group (Fig. 4B). On the siVEGF-loaded gel, cell
vitality was suppressed significantly, compared with all the other
groups (Fig. 4B).
Actin cytoskeleton arrangement
To examine the spread of the cells grown on the
gels, the actin cytoskeleton was stained. In general, the cells
grown on gels were shrunken and exhibited a spindle-like shape,
whereas the cells grown on TCP were spread widely with high levels
of cell-cell contact (Fig. 5). The
changes were particularly marked on the gel loaded with siVEGF
(Fig. 5).
Sustained delivery of siRNA in vivo and
mucosa thickness measurement
The sinus mucosa was isolated to analyze the gel
function in vivo. Following 2 weeks of intervention, only
the siRNA in the gel was able to co-localize with the mucosal
cells, exhibiting >30-fold higher fluorescence intensity
(Fig. 6Aa). Direct injection of
the chitosan/siRNA NPs were able to co-localize to a certain
degree, however, the long term preserving ability was deficient
(Fig. 6Ab). Quantification is
shown in Fig.6 B. The sinus mucosa
thickness was determined to reflect the inflammation inhibition
capability. The thickness was reduced significantly following the
sustained silencing of VEGF, suggesting that the incrassated mucosa
caused by rhinosinusitis was withdrawn (Fig. 6C).
Discussion
Chronic rhinosinusitis is a debilitating condition
in humans and the enlarged nasal polyposis often requires a
surgical procedure, which is often relapses and can be problematic
(17). Therefore, the
identification of novel internal medical treatments for chronic
rhinosinusitis is imperative. In the present study, downregulation
of the expression of VEGF, one of the key molecules during the
formation of incrassated mucosa, was performed to determine its
effect on rhinosinusitis inhibition. VEGF has a close association
with the development of rhinosinusitis. VEGF is abundantly
expressed by nasal epithelial cells and promotes cell hyperplasia
in polyposis (4), and other
members of the VEGF gene family of ligands and receptors are also
highly expressed (18). In
addition, VEGF can increase vascular permeability and in present in
the nasal secretions produced in rhinosinusitis (19). Therefore, utilization of siVEGF may
inhibit epithelial cell function and thus inhibit the process of
rhinosinusitis. It was also observed in the present study that
epithelial cells proliferation is significantly suppressed
following downregulation if the expression of VEGF and resulted in
a decreased autocrine effect.
In order to obtain sustained localized siRNA
delivery and silencing, the injectable chitosan hydrogel was
selected for use in the present study. As a thermosensitive
hydrogel, which transfers to a solid state under physiological
conditions, it is convenient for localized injection and is
retained in situ without surgical procedure. Notable, the
injectable chitosan hydrogel has been extensively investigated in
several areas, including periodontal regeneration (13), tumor therapy (12) and tissue repair (20). The sinuses are located within the
maxillofacial bones, which are difficult to access in medicine
intervention. Consequently, injectable hydrogel may be preferable
for localized sinuses drug delivery (20). Another beneficial property of
chitosan hydrogel is the long-term preservation of the drugs loaded
onto it, which is ideal for sustained local drug delivery. In the
present study, it was observed that siRNA was released gradually in
neutral conditions and at a higher rate in acidic conditions, which
can be explained by the fast dissolution of chitosan in acidic
conditions. The local pH of tissue is considered to decrease in the
presence of inflammation exists (21). Therefore, it may trigger the burst
release of siRNA from the hydrogel within the lesion area at the
initial stage, which is essential to provide sufficient siRNA
penetration into the mucosa. In the present study, due to the
ability of the hydrogel to provide sustained delivery, the siRNA
collocated with the mucosa cells remained detectable after 2 weeks,
which was not observed following use of the NP system or with free
siRNA. The chitosan molecule is mucoadhesive and as the present
study observed that the siRNA collocated with the mucosa cells,
this suggested that it may be used as a potential mucosa target
drug delivery system (11,22). The mucosal thickness can be used to
reflect the level of inflammation (23) and the present study demonstrated
that it was markedly decreased following siVEGF introducing. In
conclusion, the present study described a convenient chronic
rhinosinusitis therapeutic strategy using the technique of
injecting chitosan hydrogel containing siRNA. This drug delivery
system offers considerable advantages for the specific sinus
structure and may also be used to deliver other bioactive factors
for more beneficial effects.
Acknowledgments
The present study was supported technically by the
State Key Laboratory of Stomatology, the Fourth Military Medical
University.
References
|
1
|
Obaseki D, Potts J, Joos G, Baelum J,
Haahtela T, Ahlström M, Matricardi P, Kramer U, Gjomarkaj M,
Fokkens W, et al: The relation of airway obstruction to asthma,
chronic rhinosinusitis and age: Results from a population survey of
adults. Allergy. 69:1205–1214. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Van Zele T, Holtappels G, Gevaert P and
Bachert C: Differences in initial immunoprofiles between recurrent
and nonrecurrent chronic rhinosinusitis with nasal polyps. Am J
Rhinol Allergy. 28:192–198. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saedi B, Sadeghi M, Akhavan-Khaleghi N and
Seifmanesh H: Impact of endoscopic sinus surgery on the quality of
life of patients with nasal polyposis. B-ENT. 10:59–65.
2014.PubMed/NCBI
|
|
4
|
Lee HS, Myers A and Kim J: Vascular
endothelial growth factor drives autocrine epithelial cell
proliferation and survival in chronic rhinosinusitis with nasal
polyposis. Am J Respir Crit Care Med. 180:1056–1067. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Felipe AV, Oliveira J, Chang PY, Moraes
AA, da Silva TD, Tucci-Viegas VM and Forones NM: RNA interference:
A promising therapy for gastric cancer. Asian Pac J Cancer Prev.
15:5509–5515. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sahin B, Fife J, Parmar MB, Valencia-Serna
J, Gul-Uludağ H, Jiang X, Weinfeld M, Lavasanifar A and Uludağ H:
siRNA therapy in cutaneous T-cell lymphoma cells using polymeric
carriers. Biomaterials. 35:9382–9394. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gu X, Ding F and Williams DF: Neural
tissue engineering options for peripheral nerve regeneration.
Biomaterials. 35:6143–6156. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fu GF, Pan JC, Lin N, Hu HY, Tang WM, Xu
JS, Wang XL, Xu XQ, Qiu T, Liu XY, et al: siRNA against KIR3DL1 as
a potential gene therapeutic agent in controlling HIV-1 infection.
Viral Immunol. 27:207–213. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Howard KA, Paludan SR, Behlke MA,
Besenbacher F, Deleuran B and Kjems J: Chitosan/siRNA
nanoparticle-mediated TNF-alpha knockdown in peritoneal macrophages
for anti-inflammatory treatment in a murine arthritis model. Mol
Ther. 17:162–168. 2009. View Article : Google Scholar
|
|
10
|
Rudzinski WE and Aminabhavi TM: Chitosan
as a carrier for targeted delivery of small interfering RNA. Int J
Pharm. 399:1–11. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gonçalves IC, Henriques PC, Seabra CL and
Martins MC: The potential utility of chitosan micro/nanoparticles
in the treatment of gastric infection. Expert Rev Anti Infect Ther.
12:981–992. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Han HD, Mora EM, Roh JW, Nishimura M, Lee
SJ, Stone RL, Bar-Eli M, Lopez-Berestein G and Sood AK: Chitosan
hydrogel for localized gene silencing. Cancer Biol Ther.
11:839–845. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ma Z, Yang C, Song W, Wang Q, Kjems J and
Gao S: Chitosan hydrogel as siRNA vector for prolonged gene
silencing. J Nanobiotechnology. 12:232014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Andersen MØ, Le DQS, Chen M, Nygaard JV,
Moustapha K, Bünger C and Kjems J: Spatially controlled delivery of
siRNAs to stem cells in implants generated by multi-component
additive manufacturing. Adv Funct Mater. 23:5599–5607. 2013.
View Article : Google Scholar
|
|
15
|
Ahn SK, Jeon SY, Khalmuratov R, Kim DJ,
Kim JP, Park JJ and Hur DG: Rat model of staphylococcal enterotoxin
B-induced rhinosinusitis. Clin Exp Otorhinolaryngol. 1:24–28. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li SD, Chen YC, Hackett MJ and Huang L:
Tumor-targeted delivery of siRNA by self-assembled nanoparticles.
Mol Ther. 16:163–169. 2008. View Article : Google Scholar
|
|
17
|
Rimmer J, Fokkens W, Chong LY and Hopkins
C: Surgical versus medical interventions for chronic rhinosinusitis
with nasal polyps. Cochrane Database Syst Rev.
12:CD0069912014.PubMed/NCBI
|
|
18
|
Lee HS and Kim J: Constitutive expression
of vascular endothelial cell growth factor (VEGF) gene family
ligand and receptors on human upper and lower airway epithelial
cells. Int Forum Allergy Rhinol. 4:8–14. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsune S, Ohori J, Yoshifuku K and Kurono
Y: Effect of vascular endothelial growth factor on nasal vascular
permeability. Laryngoscope. 120:844–848. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Burdick JA: Injectable gels for
tissue/organ repair. Biomed Mater. 7:0202012012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Punnia-Moorthy A: Evaluation of pH changes
in inflammation of the subcutaneous air pouch lining in the rat,
induced by carrageenan, dextran and staphylococcus aureus. J Oral
Pathol. 16:36–44. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fernandes M, Gonçalves IC, Nardecchia S,
Amaral IF, Barbosa MA and Martins MC: Modulation of stability and
mucoadhesive properties of chitosan microspheres for therapeutic
gastric application. Int J Pharm. 454:116–124. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kinis V, Ozbay M, Akdag M, Alabalık U, Gul
A, Yılmaz B, Ozkan H and Topcu I: Effects of caffeic acid phenethyl
ester on wound healing of nasal mucosa in the rat: An experimental
study. Am J Otolaryngol. 35:482–486. 2014. View Article : Google Scholar : PubMed/NCBI
|