Activin receptor-like kinases (ALKs) belong to the
type I activin receptor family. The activin receptor was first
cloned in 1991, and subsequently named the type II activin receptor
(ActRII) (1,2). In 1992, the second activin receptor
was defined as the type I activin receptor (ActRI) and termed
activin receptor-like kinase (ALK) (3,4). To
date, seven ALKs, ALK1-7, have been identified in mammals. These
ALKs are transmembrane proteins, known as serine/threonine kinase
receptors belonging to the transforming growth factor-β (TGF-β)
superfamily. The ALKs harbor a transmembrane domain, an
extracellular binding domain and a glycine- and serine-rich
sequence (GS) domain. The GS domain is a kinase site activated by
the TGF-β superfamily type II receptor and can trigger downstream
signal transduction. The ALKs elicit various downstream effects of
activin/TGF-β, including cell differentiation, proliferation,
apoptosis, migration and adhesion as critical modulators of these
biological processes. ALKs are also involved in a variety of
diseases that include tumorigenesis, skeletal malfunctions,
hemorrhagic telangiectasia, renal and immune diseases (5–7).
This review briefly discusses the therapeutic prospects of small
molecule inhibitors of ALKs as drug targets in tumor and stem
cells.
In order to elucidate the biological actions of
small molecule inhibitors of ALKs, an understating of the basic
signal transduction of activin/TGF-β is important. The TGF-β
superfamily includes several subfamilies, such as TGF-β,
inhibin/activin, myostatin/GDF11 and bone morphogenetic protein
(BMP) (8–11). As a member of the TGF-β
superfamily, activin belongs to a group of multifunctional
cytokines that possess numerous biological functions, including
cell differentiation, proliferation and matrix formation (12–14).
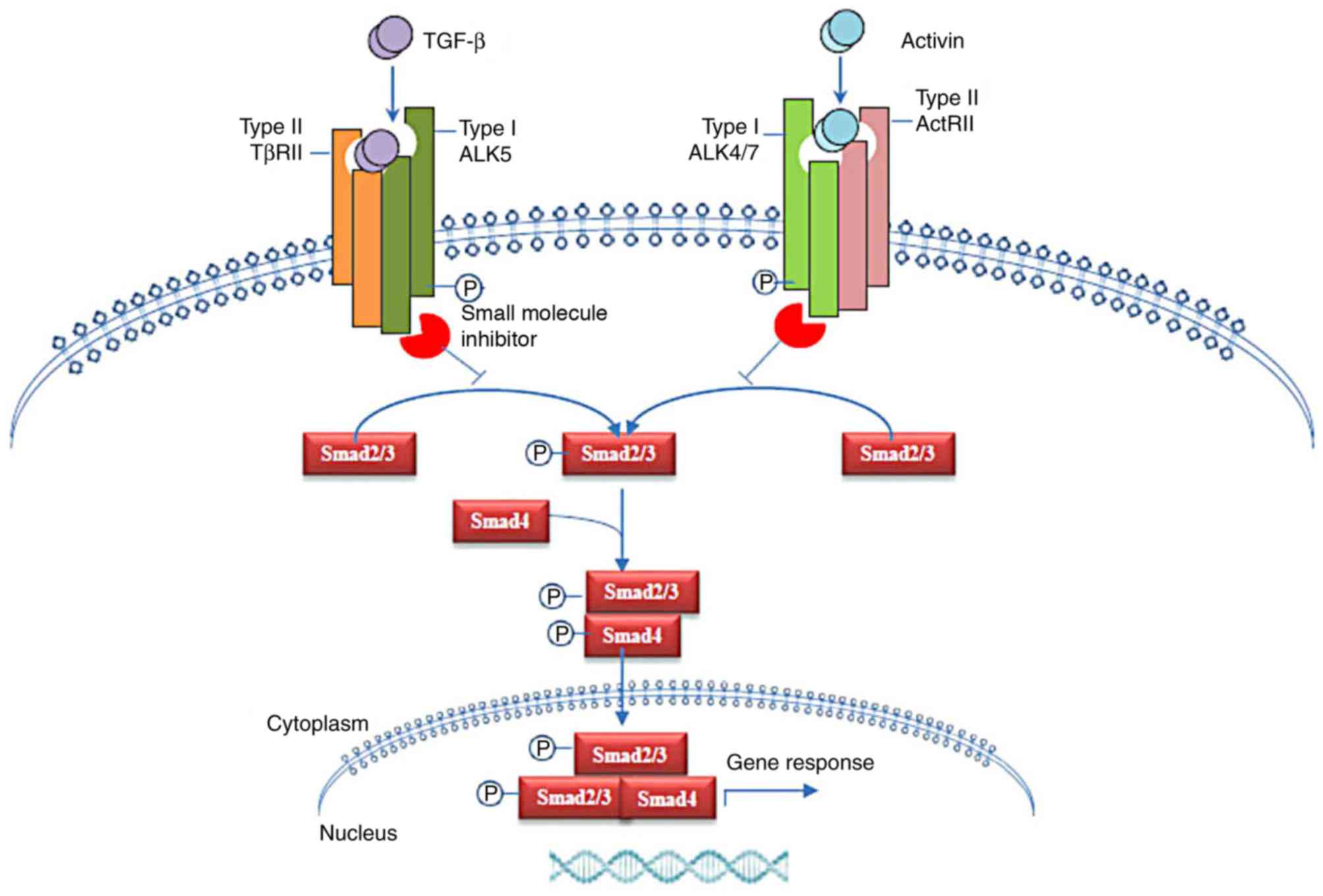
SMAD proteins, the Drosophila mothers against
decapentaplegic gene homologs in mammals, are shared by activin and
TGF-β in a classical signal transduction pathway (15–21).
Members of the TGF-β superfamily bind to type II receptors that are
subsequently stimulated by dimerization with their specific
phosphorylated type I receptor to activate shared canonical and
distinct non-canonical pathways (15–18).
A total of 7 ALKs are designated as type I receptors of the TGF-β
superfamily, ALK1-ALK7 (17,18).
Ligands can bind multiple ALKs, albeit with different affinities.
TGF-β interacts with ALK1 and ALK5 with high affinity. Activin
binds to ALK2 and ALK4 with high affinity and with moderate
affinity to ALK7. In addition, BMP interacts with ALK1, ALK3 and
ALK6 with high affinity and with moderate affinity to ALK2. The
activated ALKs phosphorylate and activate SMAD proteins and mediate
intracellular signal transduction (19).
The mammalian SMAD protein family is a family of 8
members that serve as intracellular signaling mediators of the
TGF-β superfamily (20,21). Smad2 and Smad3 mediate TGF-β and
activin/inhibin signaling, while BMP signaling is mediated by
Smad1, Smad5 and Smad8. On the other hand, Smad6 and Smad7 act as
intracellular antagonists in the signaling pathway of the TGF-β
superfamily. In the canonical pathway, the type I receptors (ALKs)
phosphorylate Smad2 and/or Smad3, facilitating the formation of a
protein complex with Smad4. The Smad2/3-Smad4 complex is
translocated to the nucleus where a substantial number of genes are
either transcriptionally activated or repressed. In addition,
mitogen-activated protein kinase (MAPK)/ERK, PI3K/AKT, WNT and
Notch are activated by the TGF-β superfamily, which in turn can
transduce the signaling of the independent SMAD proteins; this
cascade constitutes the non-canonical pathways (22–25).
Moreover, ALK4 mediates activin signaling transduction in a
SMAD-independent manner (26).
The recently identified activin receptor-interacting
proteins (ARIPs) are present in the cytoplasm (27). These proteins contain the PDZ
domain and mediate activin signaling in a SMAD-independent manner
(27,28). PDZ proteins play a critical role in
assembling the signaling molecules close to the sub-membranous
regions and membranous receptors (29). ARIP1 has multiple protein-protein
interacting domains that include 5 PDZ domains and 2 WW domains,
and bind to ActRII through the fifth PDZ domain at the C-terminal
(27,30). ARIP2 possesses only one PDZ domain
that can also interact with ActRII and Ral binding protein 1
(RalBP1). The ternary complex of ARIP2, ActRII and RalBP1 is
assembled near the sub-membranous regions (31). The overexpression of ARIP1 and
ARIP2 suppresses the gene transcription induced by activin in a
dose-dependent manner (27,31).
The subsequently identified isoforms of ARIP2, ARIP2b and 2c
(32), also harbor only one PDZ
domain that binds specifically to ActRII. However, overexpression
of ARIP2b and 2c enhances activin signaling transduction. Although
structural homology is observed between ARIP2b, ARIP2c and ARIP2,
the biological activities are different (31,32).
Furthermore, current studies have revealed that ARIPs are not only
functionally distinct but also exhibit differences in histological
distribution (32–35).
Activin shows pleiotropic functions in embryonic
development, erythropoiesis, wound healing, inflammation, arterial
pressure regulation, cancer initiation and progression (36–39).
Also, it promotes the production of the extracellular matrix, which
is the main factor causing liver, lung, heart and renal fibrosis
(36,37). Furthermore, activin regulates the
activities of macrophages, such as in promoting the activation of
resting macrophages and in the polarization of M2 macrophages,
while inhibiting the function of activated M1 macrophages in a
dual-directional manner (38,39).
Activin functions as a neuroprotective and neurotrophic factor in
the survival of cultured neurons and promotes the neurite outgrowth
of dorsal root ganglia neurons (40,41).
Nevertheless, these studies suggest that activin plays a major role
in the migration, proliferation and apoptosis of cancer cells
(10,42).
Activin not only promotes the genesis and
progression of certain tumors, but can also inhibit tumorigenesis,
depending on the tumor type and signaling pathways involved
(42,43). The overexpression of activin is
associated with colorectal cancer, metastatic prostate cancer, lung
cancer, hepatocellular carcinomas and pancreatic cancer (42–44),
with poor patient prognosis and positive lymph node status in oral
squamous cell carcinomas and lung adenocarcinoma. Additionally, a
recombinant activin A promoted the proliferation of lung cancer
cell lines SKLU1 and H460 and the invasion of ovarian cancer cell
lines OCC1 and SKOV-3 without affecting proliferation (45). Recent evidence has implicated
overactive activin signaling in breast cancer cell lines, including
MCF7 and MDA-MB231, and higher levels of p-Smad2, p-Smad3 and
activin A in advanced breast cancer (46,47).
Activin A also promotes invasion, angiogenesis,
epithelial-mesenchymal transition (EMT) and stemness in breast
cancer cells (46).
A high level of activin is an independent prognostic
factor for the survival of patients with cancer. In addition, it
also serves as a marker for the severity of the neoplastic disease
or the inflammatory process, and might be correlated with survival
by effectuating the loss of skeletal muscle mass and the
development of cachexia (43,48).
Some studies have utilized adeno-associated viral vectors to
increase the levels of circulating activin A, thereby inducing a
rapid and profound body weight loss (49). Similarly, in cachectic patients the
concentrations of activin A are higher than those in non-cachectic
patients and are positively associated with weight loss (50,51).
This phenomenon established a correlation between circulating
activin A levels and anorexia/cachexia syndrome in patients with
cancer.
Other studies have shown that activin also exerts a
protective effect on patients with cancer. The T47D breast cancer
cell model demonstrated that activin A treatment inhibits cell
proliferation and induces cell cycle arrest (52). Additionally, in thyroid papillary
carcinoma cells, activin exhibits an anti-proliferative mechanism,
thereby regulating thyroid tumorigenesis (53). Consistently, activin A is an
effective anti-angiogenic factor that inhibits the proliferation of
endothelial cells and tube formation by downregulating the
expression of cyclin D1 and retinoblastoma protein and enhancing
the production of the cell cycle inhibitor p21 (54).
Stem cells have the ability to self-renew and
generate differentiated cells that are retained in a specific
tissue, and are defined as different types of embryonic stem cells
(ESCs), somatic stem cells or induced pluripotent stem cells
(iPSCs) (60–62). Several studies have demonstrated
that activin A induces early embryonic development and plays a
critical role in the differentiation of erythroblasts, including
the generation and maturation of erythrocytes (63,64).
Recent studies have demonstrated that activin enhances eye field
formation from ESCs and promotes the generation of mature
photoreceptors in primary rodent retina cultures; however, it
inhibits the differentiation of pluripotent stem cells by
influencing the expression of key genes, including Nanog and Oct4,
in stem cells (65–68). During the embryonic development and
differentiation of ESCs, high-intensity signals of Nodal/activin
are required in pluripotent stem cell derivatives that give rise to
the definitive endoderm (DE), compared with the posterior
derivative that differentiates into the mesoderm (69,70).
Furthermore, the effect of the length of stimulation with activin A
plus Wnt3a on the development of hepatic and pancreatic progenitors
from the DE cells derived from human pluripotent stem cells has
also been investigated (71).
Another study reported that activin upregulates the expression of
developmental pluripotency associated 3 in early primordial germ
cells (PGCs) and the tyrosine kinase receptor cKIT genes in both
standard-derived and activin-derived human embryonic stem cells
(hESCs), suggesting that activin induces differentiation by priming
hESCs to become part of the PGC lineage (72). Interestingly, the treatment of
human and mouse ESCs with high concentrations of activin A triggers
stem cell differentiation via the activation of ALKs/Smads
(73–75).
Additionally, marked changes in BMP and
activin/Nodal signaling levels determine the specification of
cardiomyocytes and the cardiac mesoderm. Human iPSC and ESC
translational studies have indicated that the co-expression of
platelet derived growth factor receptor A and kinase insert domain
protein receptor directs the emergence of the cardiac mesoderm, and
that this is dependent on the optimal levels of BMP and
activin/Nodal signaling (70,76).
Accumulating evidence has demonstrated that some cancer stem cells
show stem cell properties, such as multipotency, self-renewal and
the expression of stem cell markers in the tumor. Such cells have
been identified in breast, brain and blood cancer (77–79).
As the seeding cells, cancer stem cells are capable of forming a
new tumor with the properties of the parental tumor. Activin/nodal
signaling can control tumor metastasis and progression by
influencing the differentiation and proliferation of cancer stem
cells via the activin-related signaling pathway similar to that in
somatic or embryonic stem cells, and activin signaling enhances the
self-renewal of colorectal cancer stem cells and promotes the
progression of colorectal cancer in vivo (80,81).
Several ALKs exert regulatory roles in cell
differentiation, proliferation, apoptosis, invasion and migration,
and mutation of ALKs in various human cancer types has also been
identified (5,82). The majority of tumors need a
functional vascular network to maintain an environment conducive to
tumor growth beyond local boundaries and to facilitate tumor
metastasis; thus, a promising approach to cancer therapy is
anti-angiogenic treatment. To date, a number of studies have
investigated the anti-angiogenic and anti-tumor growth functions of
ALK inhibitors with respect to anti-tumor therapy (5,83–85).
ALK1 has been found to exist widely in the tumor
blood vessels of lymphoma and cancer of the skin, kidney, prostate,
ovary, lung, thyroid, pancreas and liver (5). ALK1 has high affinity for BMP9 and is
mainly expressed in endothelial cells, wherein it regulates
angiogenesis (83). High ALK1
protein levels in blood vessels of tumor tissues may be a
prognostic marker of tumor metastasis in patients with breast
cancer. A total of two pharmacological inhibitors of ALK1,
PF-03446962, a human antibody against the extracellular domain of
ALK1 (84,85), and ACE-041/Dalantercept, a soluble
ALK1-Fc fusion protein (84,86),
have been used as anti-angiogenic drugs in clinical studies
(84–86). ALK1-Fc (Dalantercept) is a chimeric
protein consisting of the ligand-binding ALK1 extracellular domain
fused to the Fc region of the antibody (84). The ALK1 inhibitor PF-03446962 can
prevent the binding of TGF-β and BMP ligands to the extracellular
domain of ALK1 (85). The
inhibition of ALK1 results in a decrease in the phosphorylation of
p38, a decline in the expression of EMT markers, including matrix
metalloproteinase 1, vimentin, Slug and cadherin-2, and
downregulation of the expression of the DNA binding 1 (ID1) and ID2
proteins. Pharmacological inhibition of ALK1 also prevents lung
colonization and metastatic dissemination in endocrine pancreatic
and mammary carcinoma mouse models (87).
Recent studies have reported that BMP9 induces the
phosphorylation of Smad1/5 through ALK1 and ALK2, which contributes
to tumorigenesis by promoting the migration and proliferation of
cancer cells (88–90). Abnormal expression of ALK2 is
associated with a variety of diseases. Granulocyte-macrophage
colony-stimulating factor (GM-CSF) is required for the
proliferation of TF-1 cells; however, BMP9 also promotes the
proliferation of cultured TF-1 cells in the absence of GM-CSF. The
overexpression of ALK2 triggers the autophosphorylation of Smad1/5
in TF-1 cells, leading to proliferation of the cells (91,92).
KRC203 and KRC360, two specific ALK2 inhibitors, suppressed the
BMP9 and ALK2-induced migration and proliferation of cancer cells.
Compared to LDN193189, these two inhibitors were more specific and
effective in inhibiting ALK2 and were considered as promising drug
candidates for the treatment of cancers or diseases with abnormal
BMP9 or ALK2 signaling (93,94).
In adult tissues, ALK4 mediates the
anti-proliferative effect of activin in pituitary tumor cells. The
truncated form of ALK4 functions as a dominant negative inhibitor
of activin signaling and eliminates the growth suppression induced
by activin (95), while the
overexpression of wild-type ALK4 restores the anti-proliferative
activity of activin in human pituitary tumor cells (96). The expression of ALK4 was decreased
only slightly in breast cancer tissues when compared to normal
breast tissues (97). Based on the
abnormal activation of TGF-β signaling in hepatocellular carcinoma,
LY2157299, a small molecule inhibitor targeting the
serine/threonine kinases of TGF-βRI has been designed, which is
currently under clinical investigation. LY2157299 exerts anti-tumor
roles in patients with hepatocellular carcinoma and glioblastoma
(98). LY2157299 blocked the
migration and invasion of hepatocellular carcinoma cells, inhibited
the growth of hepatocellular carcinoma growth, blocked the
production of connective tissue growth factor and reduced stromal
reactions (99,100).
The role of ALK5 in tumorigenesis has been studied
extensively. In the prostate cancer cell line LNCaP, loss of the
tumor suppressive effects of TGF-β was attributed to the
rearrangement of the ALK5 gene; transfection with wild-type ALK5
restored the tumor suppressive effects of TGF-β (101). Furthermore, human prostate cancer
displays a decrease in the mRNA and protein levels of ALK5, and the
loss of ALK5 activity has been associated with an advanced tumor
stage and poor 4-year survival (102). The critical role of ALK5 in the
activity of TGF-β led to the development of drugs that target ALK5
for the inhibition of TGF-β signaling. Several ALK5 inhibitors have
been identified and shown to affect fibrosis and tumor progression
in animal models (103). CYLD
lysine 63 deubiquitinase (CYLD), a deubiquitinating enzyme, is
considered to be a potent tumor inhibitor. The knockdown of CYLD
stimulates TGF-β signaling by maintaining ALK5 stabilization in a
cell-autonomous fashion. Moreover, the ALK5 inhibitor TGF-βRI
kinase inhibitor II completely blocks the invasive phenotypes of
cancer cells induced by CYLD knockdown (104).
BMP signaling is also a critical mediator of
cartilage differentiation and endochondral ossification. The
mutation of arginine 206 to histidine results in the abnormal
activation of ALK2, and this mutation exists in 95% of patients
with fibrodysplasia ossificans progressiva (FOP) (107). FOP is a rare autosomal genetic
disease that results in the development of ectopic bone formation
in muscle. Activation of 5′AMP activated protein kinase catalytic
subunit α-2 promotes the expression of Smad6 and E3-ubiquitin
protein ligase Smurf1, leading to increased interactions and
inducing the proteasome-dependent degradation of ALK2 (108). Conversely, Smad6 or Smurf1
knockdown arrests metformin-induced ALK2 reduction. FOP fibroblasts
were transformed into iPSCs, followed by osteogenic differentiation
of iPSCs in vitro. Osteogenic differentiation of iPSCs was
blocked by metformin, a pharmacological AMPK activator (108). Therefore, ALK2 acts as a
potential therapeutic target during lesion-induced early
chondrogenic stages to avoid the heterotopic bone formation in FOP
and/or other pathological events (108,109).
3-(6-Methylpyridin-2-yl)-N-phenyl-4-(quinolin-4-yl)-1H-
pyrazole-1-carbothioamide, also known as A-83-01, is a selective
ALK inhibitor; for example, it is a strong inhibitor of ALK4
(IC50, 45 nM), ALK5 (IC50, 12 nM) and ALK7
(IC50, 7.5 nM), but only a weak inhibitor of ALK1, ALK2,
ALK3 and ALK6. A-83-01 is a TGF-β/ALK inhibitor that can block
TGF-β-induced EMT via the downregulation of Smad2 phosphorylation
levels (112). Moreover, A-83-01
can maintain the pluripotency of rat iPSCs, leading to long-term
and homogenous self-renewal and to the formation of ESC-like
colonies in vitro. It also can rapidly and uniformly alter
the fate of mouse embryonic stem cells from the pluripotent to
neuronal state (113,114).
Not applicable.
The present study was supported by the National
Basic Research Program of China (grant no. 2015CB943300), National
Natural Science Foundation of China (grant nos. 31871510 and
31500738), and Research Projects of Science and Health of Jilin
Province (grant nos. 608692, 2014Z066 and 20180414040GH).
Data sharing is not applicable to this review
article, as no datasets were generated or analyzed during the
current study.
XC, YQ and ZL conceptualized and designed the study.
XC, SS, XL and JZ collected, organized and drafted the information.
XC and ZL wrote the manuscript. YQ and ZL revised the manuscript
critically. All authors have read and approved the manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Mathews LS and Vale WW: Expression cloning
of an activin receptor, a predicted transmembrane serine kinase.
Cell. 65:973–982. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mathews LS, Vale WW and Kintner CR:
Cloning of a second type of activin receptor and functional
characterization in Xenopus embryos. Science. 255:1702–1705. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Attisano L, Wrana JL, Cheifetz S and
Massagué J: Novel activin receptors: Distinct genes and alternative
mRNA splicing generate a repertoire of serine/threonine kinase
receptors. Cell. 68:97–108. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tsuchida K, Mathews LS and Vale WW:
Cloning and characterization of a transmembrane serine kinase that
acts as an activin type I receptor. Proc Natl Acad Sci USA.
90:11242–11246. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu-Lowe DD, Chen E, Zhang L, Watson KD,
Mancuso P, Lappin P, Wickman G, Chen JH, Wang J, Jiang X, et al:
Targeting activin receptor-like kinase 1 inhibits angiogenesis and
tumorigenesis through a mechanism of action complementary to
anti-VEGF therapies. Cancer Res. 71:1362–1373. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Johnson DW, Berg JN, Baldwin MA, Gallione
CJ, Marondel I, Yoon SJ, Stenzel TT, Speer M, Pericak-Vance MA,
Diamond A, et al: Mutations in the activin receptor-like kinase 1
gene in hereditary haemorrhagic telangiectasia type 2. Nat Genet.
13:189–195. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muñoz-Félix JM, López-Novoa JM and
Martínez-Salgado C: Heterozygous disruption of activin
receptor-like kinase 1 is associated with increased renal fibrosis
in a mouse model of obstructive nephropathy. Kidney Int.
85:319–332. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Song T, Zhao J, Jiang T, Jin X, Li Y and
Liu X: Formononetin protects against balloon injury-induced
neointima formation in rats by regulating proliferation and
migration of vascular smooth muscle cells via the TGF β1/Smad3
signaling pathway. Int J Mol Med. 42:2155–2162. 2018.PubMed/NCBI
|
|
9
|
Liu H, Zhong L, Yuan T, Chen S, Zhou Y, An
L, Guo Y, Fan M, Li Y, Sun Y, et al: MicroRNA-155 inhibits the
osteogenic differentiation of mesenchymal stem cells induced by
BMP9 via downregulation of BMP signaling pathway. Int J Mol Med.
41:3379–3393. 2018.PubMed/NCBI
|
|
10
|
Takahashi S, Nakasatomi M, Takei Y,
Ikeuchi H, Sakairi T, Kaneko Y, Hiromura K, Nojima Y and Maeshima
A: Identification of urinary activin A as a novel biomarker
reflecting the severity of acute kidney injury. Sci Rep.
8:51762018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pirruccello-Straub M, Jackson J, Wawersik
S, Webster MT, Salta L, Long K, McConaughy W, Capili A, Boston C,
Carven GJ, et al: Blocking extracellular activation of myostatin as
a strategy for treating muscle wasting. Sci Rep. 8:22922018.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Donovan P, Dubey OA, Kallioinen S, Rogers
KW, Muehlethaler K, Müller P, Rimoldi D and Constam DB: Paracrine
activin-A signaling promotes melanoma growth and metastasis through
immune evasion. J Invest Dermatol. 137:2578–2587. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang Q, Yu Y, Zhang P, Chen Y, Li C, Chen
J, Wang Y and Li Y: The crucial role of activin A/ALK4 pathway in
the pathogenesis of Ang-II-induced atrial fibrosis and
vulnerability to atrial fibrillation. Basic Res Cardiol.
112:472017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xie D, Liu Z, Wu J, Feng W, Yang K, Deng
J, Tian G, Santos S, Cui X and Lin F: The effects of activin A on
the migration of human breast cancer cells and neutrophils and
their migratory interaction. Exp Cell Res. 357:107–115. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Heldin CH, Miyazono K and Ten Dijke P:
TGF-beta signaling from cell membrane to nucleus through SMAD
proteins. Nature. 390:465–471. 1997. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Massagué J and Gomis RR: The logic of
TGFbeta signaling. FEBS Lett. 580:2811–2820. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hawinkels LJ, Garcia de Vinuesa A and Ten
Dijke P: Activin receptor-like kinase 1 as a target for
anti-angiogenesis therapy. Expert Opin Investig Drugs.
22:1371–1383. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hinck AP, Mueller TD and Springer TA:
Structural biology and evolution of the TGF-β family. Cold Spring
Harb Perspect Biol. 8(pii): a0221032016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Niu L, Cui X, Qi Y, Xie D, Wu Q, Chen X,
Ge J and Liu Z: Involvement of TGF-β1/Smad3 signaling in carbon
tetrachloride-induced acute liver injury in mice. PLoS One.
11:e01560902016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Afrakhte M, Morén A, Jossan S, Itoh S,
Sampath K, Westermark B, Heldin CH, Heldin NE and Ten Dijke P:
Induction of inhibitory Smad6 and Smad7 mRNA by TGF-beta family
members. Biochem Biophys Res Commun. 249:505–511. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Qi Y, Ge J, Ma C, Wu N, Cui X and Liu Z:
Activin A regulates activation of mouse neutrophils by Smad3
signalling. Open Biol. 7(pii): 1603422017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Moustakas A and Heldin CH: Non-Smad
TGF-beta signals. J Cell Sci. 118:3573–3584. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang YE: Non-Smad pathways in TGF-beta
signaling. Cell Res. 19:128–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kua HY, Liu H, Leong WF, Li L, Jia D, Ma
G, Hu Y, Wang X, Chau JF, Chen YG, et al: c-Abl promotes osteoblast
expansion by differentially regulating canonical and non-canonical
BMP pathways and p16INK4a expression. Nat Cell Biol. 14:727–737.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li Z, Fei T, Zhang J, Zhu G, Wang L, Lu D,
Chi X, Teng Y, Hou N, Yang X, et al: BMP4 signaling acts via
dual-specificity phosphatase 9 to control ERK activity in mouse
embryonic stem cells. Cell Stem Cell. 10:171–182. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Suzuki K, Kobayashi T, Funatsu O, Morita A
and Ikekita M: Activin A induces neuronal differentiation and
survival via ALK4 in a SMAD-independent manner in a subpopulation
of human neuroblastomas. Biochem Biophys Res Commun. 394:639–645.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shoji H, Tsuchida K, Kishi H, Yamakawa N,
Matsuzaki T, Liu Z, Nakamura T and Sugino H: Identification and
characterization of a PDZ protein that interacts with activin types
II receptors. J Bol Chem. 275:5485–5492. 2000. View Article : Google Scholar
|
|
28
|
Kurisaki A, Inoue I, Kurisaki K, Yamakawa
N, Tsuchida K and Sugino H: Activin induces long-lasting
N-methyl-D-aspartate receptor activation via scaffolding PDZ
protein activin receptor interacting protein 1. Neuroscience.
151:1225–1235. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fanning AS and Anderson JM: PDZ domains:
Fundamental building blocks in the organization of protein
complexes at the plasma membrane. J Clin Invest. 103:767–772. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tsuchida K, Matsuzaki T, Yamakawa N, Liu
ZH and Sugino H: Intracellular and extracellular control of activin
function by novel regulatory molecules. Mol Cell Endocrinol.
180:25–31. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Matsuzaki T, Hanai S, Kishi H, Liu Z, Bao
Y, Kikuchi A, Tsuchida K and Sugino H: Regulation of endocytosisi
of activin type II receptors by a novel PDZ protein through
Ral/Ral-binding protein 1-dependent pathway. J Biol Chem.
277:19008–19018. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu ZH, Tsuchida K, Matsuzaki T, Bao YL,
Kurisaki A and Sugino H: Characterization of isoforms of activin
receptor-interacting protein 2 that augment activin signaling. J
Endocrinol. 189:409–421. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Liu HY, Chen FF, Ge JY, Wang YN, Zhang CH,
Cui XL, Yu F Tai GX and Liu ZH: Expression and localization of
activin receptor-interacting protein 2 in mouse tissues. Gen Comp
Endocrinol. 161:276–282. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Qi Y, Ge JY, Wang YN, Liu HY, Li YM, Liu
ZH and Cui XL: Co-expression of activin receptor-interacting
protein 1 and 2 in mouse nerve cells. Neurosci Lett. 542:53–58.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liu HY, Wang YN, Ge JY, Li N, Cui XL and
Liu ZH: Localization and role of activin receptor-interacting
protein 1 in mouse brain. J Neuroendocrinol. 25:87–95. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Manavski Y, Abel T, Hu J, Kleinlützum D,
Buchholz CJ, Belz C, Augustin HG, Boon RA and Dimmeler S:
Endothelial transcription factor KLF2 negatively regulates liver
regeneration via induction of activin A. Proc Natl Acad Sci USA.
114:3993–3998. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wei Q, Wang YN, Liu HY, Yang J, Yang CY,
Liu M, Liu YF, Yang P and Liu ZH: The expression and role of
activin A and follistatin in heart failure rats after myocardial
infarction. Int J Cardiol. 168:2994–2997. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ogawa K, Funaba M, Chen Y and Tsujimoto M:
Activin A functions as a Th2 cytokine in the promotion of the
alternative activation of macrophages. J Immunol. 177:6787–6794.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Li N, Cui X, Ge J, Li J, Niu L, Liu H, Qi
Y, Liu Z and Wang Y: Activin A inhibits activities of
lipopolysaccharide-activated macrophages via TLR4, not of TLR2.
Biochem Biophys Res Commun. 435:222–228. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Schubert D, Kimura H, LaCorbiere M,
Vaughan J, Karr D and Fische WH: Activin is a nerve cell survival
molecule. Nature. 344:868–870. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Fang L, Wang YN, Cui XL, Fang SY, Ge JY,
Sun Y and Liu ZH: The role and mechanism of action of activin A in
neurite outgrowth of chicken embryonic dorsal root ganglia. J Cell
Sci. 125:1500–1507. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ottley EC, Nicholson HD and Gold EJ:
Activin A regulates microRNAs and gene expression in LNCaP cells.
Prostate. 76:951–963. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Loomans HA and Andl CD: Intertwining of
activin A and TGFβ signaling: Dual roles in cancer progression and
cancer cell invasion. Cancers (Basel). 7:70–91. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wu S, Qi Y, Niu LM, Xie DX, Cui XL and Liu
ZH: Activin A as a novel biomarker for colorectal adenocarcinoma in
humans. Eur Rev Med Pharmacol Sci. 19:4371–4378. 2015.PubMed/NCBI
|
|
45
|
Steller MD, Shaw TJ, Vanderhyden BC and
Ethier JF: Inhibin resistance is associated with aggressive
tumorigenicity of ovarian cancer cells. Mol Cancer Res. 3:50–61.
2005.PubMed/NCBI
|
|
46
|
Bashir M, Damineni S, Mukherjee G and
Kondaiah P: Activin-A signaling promotes epithelial-mesenchymal
transition, invasion, and metastatic growth of breast cancer. NPJ
Breast Cancer. 1:150072015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kalli M, Mpekris F, Wong CK, Panagi M,
Ozturk S, Thiagalingam S, Stylianopoulos T and Papageorgis P:
Activin A signaling regulates IL13Rα2 expression to promote breast
cancer metastasis. Front Oncol. 9:322019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chang KP, Kao HK, Liang Y, Cheng MH, Chang
YL, Liu SC, Lin YC, Ko TY, Lee YS, Tsai CL, et al: Overexpression
of activin a in oral squamous cell carcinoma: Association with poor
prognosis and tumor progression. Ann Surg Oncol. 17:1945–1956.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chen JL, Walton KL, Qian H, Colgan TD,
Hagg A, WattM J, Harrison CA and Gregorevic P: Differential effects
of Il6 and activin a in the development of cancer-associated
cachexia. Cancer Res. 76:5372–5382. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Loumaye A, de Barsy M, Nachit M, Lause P,
van Maanen A, Trefois P, Gruson D and Thissen JP: Circulating
Activin A predicts survival in cancer patients. J Cachexia
Sarcopenia Muscle. 8:768–777. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Loumaye A, de Barsy M, Nachit M, Lause P,
Frateur L, van Maanen A, Trefois P, Gruson D and Thissen JP: Role
of activin a and myostatin in human cancer cachexia. J Clin
Endocrinol Metab. 100:2030–2038. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Burdette JE, Jeruss JS, Kurley SJ, Lee EJ
and Woodruff TK: Activin A mediates growth inhibition and cell
cycle arrest through Smads in human breast cancer cells. Cancer
Res. 65:7968–7975. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Matsuo SE, Leoni SG, Colquhoun A and
Kimura ET: Transforming growth factor-beta1 and activin A generate
antiproliferative signaling in thyroid cancer cells. J Endocrinol.
190:141–150. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Kaneda H, Arao T, Matsumoto K, De Velasco
MA, Tamura D, Aomatsu K, Kudo K, Sakai K, Nagai T, Fujita Y, et al:
Activin A inhibits vascular endothelial cell growth and suppresses
tumour angiogenesis in gastric cancer. Br J Cancer. 105:1210–1217.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Zonneville J, Safina A, Truskinovsky AM,
Arteaga CL and Bakin AV: TGF-β signaling promotes tumor vasculature
by enhancing the pericyte-endothelium association. BMC Cancer.
18:6702018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Furler RL, Nixon DF, Brantner CA,
Popratiloff A and Uittenbogaart CH: TGF-β sustains tumor
progression through biochemical and mechanical signal transduction.
Cancers (Basel). 10(pii): E1992018. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Miyazono K: Transforming growth
factor-beta signaling in epithelial-mesenchymal transition and
progression of cancer. Proc Jpn Acad Ser B Phys Biol Sci.
85:314–323. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Hu B, An HM, Yan X, Zheng JL, Huang XW and
Li M: Traditional Chinese medicine formulation Yanggan Jiedu Sanjie
inhibits TGF-β1-induced epithelial-mesenchymal transition and
metastatic potential in human hepatocarcinoma Bel-7402 cells. BMC
Complement Altern Med. 19:672019. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Yi EY, Park SY, Jung SY, Jang WJ and Kim
YJ: Mitochondrial dysfunction induces EMT through the
TGF-β/Smad/Snail signaling pathway in Hep3B hepatocellular
carcinoma cells. Int J Oncol. 47:1845–1853. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Zou G, Liu T, Guo L, Huang Y, Feng Y and
Duan T: MicroRNA-32 silences WWP2 expression to maintain the
pluripotency of human amniotic epithelial stem cells and β islet
like cell differentiation. Int J Mol Med. 41:1983–1991.
2018.PubMed/NCBI
|
|
61
|
Xu L, Long J, Shi C, Zhang N, Lv Y, Feng
J, Xuan A, He X, Li Q, Bai Y, et al: Effect of leukocyte inhibitory
factor on neuron differentiation from human induced pluripotent
stem cell-derived neural precursor cells. Int J Mol Med.
41:2037–2049. 2018.PubMed/NCBI
|
|
62
|
Murry CE and Keller G: Differentiation of
embryonic stem cells to clinically relevant populations: Iessons
from embryonic development. Cell. 132:661–680. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Thomsen G, Woolf T, Whitman M, Sokol S,
Vaughan J, Vale W and Melton DA: Activins are expressed early in
Xenopus embryogenesis and can induce axial mesoderm and anterior
structures. Cell. 63:485–493. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Murata M, Eto Y, Shibai H, Sakai M and
Muramatsu M: Erythroid differentiation factor is encoded by the
same mRNA as that of the inhibin beta A chain. Proc Natl Acad Sci
USA. 85:2434–2438. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bertacchi M, Lupo G, Pandolfini L,
Casarosa S, D'Onofrio M, Pedersen RA, Harris WA and Cremisi F:
Activin/Nodal signaling supports retinal progenitor specification
in a narrow time window during pluripotent stem cell neuralization.
Stem Cell Reports. 5:532–545. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Davis AA, Matzuk MM and Reh TA: Activin A
promotes progenitor differentiation into photoreceptors in rodent
retina. Mol Cell Neurosci. 15:11–21. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Vallier L, Mendjan S, Brown S, Chng Z, Teo
A, Smithers LE, Trotter MW, Cho CH, Martinez A, Rugg-Gunn P, et al:
Activin/Nodal signalling maintains pluripotency by controlling
Nanog expression. Development. 136:1339–1349. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Yang F, Wang N, Wang Y, Yu T and Wang H:
Activin-SMAD signaling is required for maintenance of porcine iPS
cell self-renewal through upregulation of NANOG and OCT4
expression. J Cell Physiol. 232:2253–2262. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Gadue P, Huber TL, Paddison PJ and Keller
GM: Wnt and TGF-beta signaling are required for the induction of an
in vitro model of primitive streak formation using embryonic stem
cells. Proc Natl Acad Sci USA. 103:16806–16811. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Kattman SJ, Witty AD, Gagliardi M, Dubois
NC, Niapour M, Hotta A, Ellis J and Keller G: Stage-specific
optimization of activin/nodal and BMP signaling promotes cardiac
differentiation of mouse and human pluripotent stem cell lines.
Cell Stem Cell. 8:228–240. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Toivonen S, Lundin K, Balboa D, Ustinov J,
Tamminen K, Palgi J, Trokovic R, Tuuri T and Otonkoski T: Activin A
and Wnt-dependent specification of human definitive endoderm cells.
Exp Cell Res. 319:2535–2544. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Duggal G, Heindryckx B, Warrier S, Taelman
J, Van der Jeught M, Deforce D, Chuva de Sousa Lopes S and De
Sutter P: Exogenous supplementation of Activin A enhances germ cell
differentiation of human embryonic stem cells. Mol Hum Reprod.
21:410–423. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Kubo A, Shinozaki K, Shannon JM, Kouskoff
V, Kennedy M, Woo S, Fehling HJ and Keller G: Development of
definitive endoderm from embryonic stem cells in culture.
Development. 131:1651–1662. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
D'Amour KA, Agulnick AD, Eliazer S, Kelly
OG, Kroon E and Baetge EE: Efficient differentiation of human
embryonic stem cells to definitive endoderm. Nat Biotechnol.
23:1534–1541. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Lu AQ, Popova EY and Barnstable CJ:
Activin signals through Smad2/3 to increase photoreceptor precursor
yield during embryonic stem cell differentiation. Stem Cell
Reports. 9:838–852. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Yang L, Soonpaa MH, Adler ED, Roepke TK,
Kattman SJ, Kennedy M, Henckaerts E, Bonham K, Abbott GW, Linden
RM, et al: Human cardiovascular progenitor cells develop from a
KDR+embryonic-stem-cell-derived population. Nature. 453:524–528.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Kim T, Echeagaray OH, Wang BJ, Casillas A,
Broughton KM, Kim BH and Sussman MA: In situ transcriptome
characteristics are lost following culture adaptation of adult
cardiac stem cells. Sci Rep. 8:120602018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Cao L, Yang Y, Ye Z, Lin B, Zeng J, Li C,
Liang T, Zhou K and Li J: Quercetin-3-methyl ether suppresses human
breast cancer stem cell formation by inhibiting the Notch1 and
PI3K/Akt signaling pathways. Int J Mol Med. 42:1625–1636.
2018.PubMed/NCBI
|
|
79
|
Singh SK, Hawkins C, Clarke ID, Squire JA,
Bayani J, Hide T, Henkelman RM, Cusimano MD and Dirks PB:
Identification of human brain tumour initiating cells. Nature.
432:396–401. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Spiller CM, Feng CW, Jackson A, Gillis AJ,
Rolland AD, Looijenga LH, Koopman P and Bowles J: Endogenous Nodal
signaling regulates germ cell potency during mammalian testis
development. Development. 139:4123–4132. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Ricci-Vitiani L, Lombardi DG, Pilozzi E,
Biffoni M, Todaro M, Peschle C and De Maria R: Identification and
expansion of human colon-cancer-initiating cells. Nature.
445:111–115. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Coffin CM, Hornick JL and Fletcher CD:
Inflammatory myofibroblastic tumor: Comparison of
clinicopathologic, histologic, and immunohistochemical features
including ALK expression in atypical and aggressive cases. Am J
Surg Pathol. 31:509–520. 2017. View Article : Google Scholar
|
|
83
|
David L, Mallet C, Mazerbourg S, Feige JJ
and Bailly S: Identification of BMP9 and BMP10 as functional
activators of the orphan activin receptor-like kinase 1 (ALK1) in
endothelial cells. Blood. 109:1953–1961. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
de Vinuesa AG, Bocci M, Pietras K and Ten
Dijke P: Targeting tumour vasculature by inhibiting activin
receptor-like kinase (ALK) 1 function. Biochem Soc Trans.
44:1142–1149. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Goff LW, Cohen RB, Berlin JD, de Braud FG,
Lyshchik A, Noberasco C, Bertolini F, Carpentieri M, Stampino CG,
Abbattista A, et al: A phase I study of the anti-activin
receptor-like kinase 1 (ALK-1) monoclonal antibody PF-03446962 in
patients with advanced solid tumors. Clin Cancer Res. 22:2146–2154.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Burger RA, Deng W, Makker V, Collins Y,
Gray H, Debernardo R, Martin LP and Aghajanian C: Phase II
evaluation of dalantercept in the treatment of persistent or
recurrent epithelial ovarian cancer: An NRG Oncology/Gynecologic
Oncology Group study. Gynecol Oncol. 150:466–470. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Cunha SI, Pardali E, Thorikay M, Anderberg
C, Hawinkels L, Goumans MJ, Seehra J, Heldin CH, Ten Dijke P and
Pietras K: Genetic and pharmacological targeting of activin
receptor-like kinase 1 impairs tumor growth and angiogenesis. J Exp
Med. 207:85–100. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Herrera B, Garcia-Álvaro M, Cruz S, Walsh
P, Fernández M, Roncero C, Fabregat I, Sánchez A and Inman GJ: BMP9
is a proliferative and survival factor for human hepatocellular
carcinoma cells. PLoS One. 8:e695352013. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Li Q, Gu X, Weng H, Ghafoory S, Liu Y,
Feng T, Dzieran J, Li L, Ilkavets I, Kruithof-de Julio M, et al:
Bone morphogenetic protein-9 induces epithelial to mesenchymal
transition in hepatocellular carcinoma cells. Cancer Sci.
104:398–408. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Suzuki Y, Ohga N, Morishita Y, Hida K,
Miyazono K and Watabe T: BMP-9 induces proliferation of multiple
typese of endothelial cells in vitro and in vivo. J Cell Sci.
123:1684–1692. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Machiya A, Tsukamoto S, Ohte S, Kuratani
M, Fujimoto M, Kumagai K, Osawa K, Suda N, Bullock AN and Katagiri
T: Effects of FKBP12 and type II BMP receptors on signal
transduction by ALK2 activating mutations associated with genetic
disorders. Bone. 111:101–108. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Macías-Silva M, Hoodless PA, Tang SJ,
Buchwald M and Wrana JL: Specific activation of Smad1 signaling
pathways by the BMP7 type I receptor, ALK2. J Biol Chem.
273:25628–25636. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Kim M, Choi O, Pyo S, Choi SU and Park CH:
Identification of novel ALK2 inhibitors and their effect on cancer
cells. Biochem Biophys Res Commun. 492:121–127. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zhang L, Wang H, Yu D, Chen J, Xing C, Li
J, Li J and Cai Y: The effects of mouse ovarian granulosa cell
function and related gene expression by suppressing BMP/Smad
signaling pathway. Anim Cells Syst (Seoul). 22:317–323. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Zhou Y, Sun H, Danila DC, Johnson SR,
Sigai DP, Zhang X and Klibanski A: Truncated activin type I
receptor Alk4 isoforms are dominant negative receptors inhibiting
activin signaling. Mol Endocrinol. 14:2066–2075. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Danila DC, Zhang X, Zhou Y, Haidar JN and
Klibanski A: Overexpression of wild-type activin receptor alk4-1
restores activin antiproliferative effects in human pituitary tumor
cells. J Clin Endocrinol Metab. 87:4741–4746. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Jeruss JS, Sturgis CD, Rademaker AW and
Woodruff TK: Down-regulation of activin, activin receptors, and
smads in high-grade breast cancer. Cancer Res. 63:3783–3790.
2003.PubMed/NCBI
|
|
98
|
Rodon J, Carducci MA, Sepulveda-Sánchez
JM, Azaro A, Calvo E, Seoane J, Braña I, Sicart E, Gueorguieva I,
Cleverly AL, et al: First-in-human dose study of the novel
transforming growth factor-β receptor I kinase inhibitor LY2157299
monohydrate in patients with advanced cancer and glioma. Clin
Cancer Res. 21:553–560. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Fransvea E, Angelotti U, Antonaci S and
Giannelli G: Blocking transforming growth factor-beta up-regulates
E-cadherin and reduces migration and invasion of hepatocellular
carcinoma cells. Hepatology. 47:1557–1566. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Mazzocca A, Fransvea E, Dituri F, Lupo L,
Antonaci S and Giannelli GL: Down-regulation of connective tissue
growth factor by inhibition of transforming growth factor beta
blocks the tumor-stroma cross-talk and tumor progression in
hepatocellular carcinoma. Hepatology. 51:523–534. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Kim IY, Ahn HJ, Zelner DJ, Shaw JW,
Sensibar JA, Kim JH, Kato M and Lee C: Genetic change in
transforming growth factor beta (TGF-beta) receptor type I gene
correlates with insensitivity to TGF-beta 1 in human prostate
cancer cells. Cancer Res. 56:44–48. 1996.PubMed/NCBI
|
|
102
|
Kim IY, Ahn HJ, Lang S, Oefelein MG, Oyasu
R, Kozlowski JM and Lee C: Loss of expression of transforming
growth factor-beta receptors is associated with poor prognosis in
prostate cancer patients. Clin Cancer Res. 4:1625–1630.
1998.PubMed/NCBI
|
|
103
|
Singh J, Ling LE, Sawyer JS, Lee WC, Zhang
F and Yingling JM: Transforming the TGFbeta pathway: Convergence of
distinct lead generation strategies on a novel kinase pharmacophore
for TbetaRI (ALK5). Curr Opin Drug Discov Devel. 7:437–445.
2004.PubMed/NCBI
|
|
104
|
Shinriki S, Jono H, Maeshiro M, Nakamura
T, Guo J, Li JD, Ueda M, Yoshida R, Shinohara M, Nakayama H, et al:
Loss of CYLD promotes cell invasion via ALK5 stabilization in oral
squamous cell carcinoma. J Pathol. 244:367–379. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Zeddou M, Relic B, Malaise O, Charlier E,
Desoroux A, Beguin Y, de Seny D and Malaise MG: Differential
signalling through ALK-1 and ALK-5 regulates leptin expression in
mesenchymal stem cells. Stem Cells Dev. 21:1948–1955. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
de Kroon LM, Narcisi R, Blaney Davidson
EN, Cleary MA, van Beuningen HM, Koevoet WJ, van Osch GJ and van
der Kraan PM: Activin receptor-like kinase receptors ALK5 and ALK1
are both required for TGFβ-induced chondrogenic differentiation of
human bone marrow-derived mesenchymal stem cells. PLoS One.
10:e01461242015. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Hatsell SJ, Idone V, Wolken DM, Huang L,
Kim HJ, Wang L, Wen X, Nannuru KC, Jimenez J, Xie L, et al:
ACVR1R206H receptor mutation causes fibrodysplasia ossificans
progressiva by imparting responsiveness to activin A. Sci Transl
Med. 7:303ra1372015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Lin H, Ying Y, Wang YY, Jiang SS, Huang D,
Luo L, Chen YG, Gerstenfeld LC and Luo Z: AMPK downregulates ALK2
via increasing the interaction between Smurf1 and Smad6, leading to
inhibition of osteogenic differentiation. Biochim Biophys Acta Mol
Cell Res. 1864:2369–2377. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Lin T, Ambasudhan R, Yuan X, Li W, Hilcove
S, Abujarour R, Lin X, Hahm HS, Hao E, Hayek A and Ding S: A
chemical platform for improved induction of human iPSCs. Nature
Methods. 6:805–808. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Laping NJ, Grygielko E, Mathur A, Butter
S, Bomberger J, Tweed C, Martin W, Fornwald J, Lehr R, Harling J,
et al: Inhibition of transforming growth factor (TGF)-beta1-induced
extracellular matrix with a novel inhibitor of the TGF-beta type I
receptor kinase activity: SB-431542. Mol Pharmacol. 62:58–64. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Inman GJ, Nicolás FJ, Callahan JF, Harling
JD, Gaster LM, Reith AD, Laping NJ and Hill CS: SB-431542 is a
potent and specific inhibitor of transforming growth factor-beta
superfamily type I activin receptor-like kinase (ALK) receptors
ALK4, ALK5, and ALK7. Mol Pharmacol. 62:65–74. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Tojo M, Hamashima Y, Hanyu A, Kajimoto T,
Saitoh M, Miyazono K, Node M and Imamura T: The ALK-5 inhibitor
A-83-01 inhibits Smad signaling and epithelial-to-mesenchymal
transition by transforming growth factor-beta. Cancer Sci.
96:791–800. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Li W, Wei W, Zhu S, Zhu J, Shi Y, Lin T,
Hao E, Hayek A, Deng H and Ding S: Generation of rat and human
induced pluripotent stem cells by combining genetic reprogramming
and chemical inhibitors. Cell Stem Cell. 4:16–19. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Klincumhom N, Tharasanit T,
Thongkittidilok C, Tiptanavattana N, Rungarunlert S, Dinnyés A and
Techakumphu M: Selective TGF-β1/ALK inhibitor improves neuronal
differentiation of mouse embryonic stem cells. Neurosci Lett.
578:1–6. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Halder SK, Beauchamp RD and Datta PK: A
specific inhibitor of TGF-beta receptor kinase, SB-431542, as a
potent antitumor agent for human cancers. Neoplasia. 7:509–521.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Matsuyama S, Iwadate M, Kondo M, Saitoh M,
Hanyu A, Shimizu K, Aburatani H, Mishima HK, Imamura T, Miyazono K
and Miyazawa K: SB-431542 and Gleevec inhibit transforming growth
factor-beta-induced proliferation of human osteosarcoma cells.
Cancer Res. 63:7791–7798. 2003.PubMed/NCBI
|
|
117
|
Sato M, Matsubara T, Adachi J, Hashimoto
Y, Fukamizu K, Kishida M, Yang YA, Wakefield LM and Tomonaga T:
Differential proteome analysis identifies TGF-β-related
pro-metastatic proteins in a 4T1 murine breast cancer model. PLoS
One. 10:e01264832015. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Kim BH, Guardia Clausi M, Frondelli M,
Nnah IC, Saqcena C, Dobrowolski R and Levison SW: Age-dependent
effects of ALK5 inhibition and mechanism of neuroprotection in
neonatal hypoxic-ischemic brain injury. Dev Neurosci. 39:338–351.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Wang XB, Zhu H, Song W and Su JH: Gremlin
regulates podocyte apoptosis via transforming growth factor-β
(TGF-β) pathway in diabetic nephropathy. Med Sci Monit. 24:183–189.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Grygielko ET, Martin WM, Tweed C, Thornton
P, Harling J, Brooks DP and Laping NJ: Inhibition of gene markers
of fibrosis with a novel inhibitor of transforming growth
factor-beta type I receptor kinase in puromycin-induced nephritis.
J Pharmacol Exp Ther. 313:943–951. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Xu H, Yang F, Sun Y, Yuan Y, Cheng H, Wei
Z, Li S, Cheng T, Brann D and Wang R: A new antifibrotic target of
Ac-SDKP: Inhibition of myofibroblast differentiation in rat lung
with silicosis. PLoS One. 7:e403012012. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Gauger KJ, Chenausky KL, Murray ME and
Schneider SS: SFRP1 reduction results in an increased sensitivity
to TGF-β signaling. BMC Cancer. 11:592011. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Kimura-Kuroda J, Teng X, Komuta Y,
Yoshioka N, Sango K, Kawamura K, Raisman G and Kawano H: An in
vitro model of the inhibition of axon growth in the lesion scar
formed after central nervous system injury. Mol Cell Neurosci.
43:177–187. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Giannelli G, Villa E and Lahn M:
Transforming growth factor-β as a therapeutic target in
hepatocellular carcinoma. Cancer Res. 74:1890–1894. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Bueno L, de Alwis DP, Pitou C, Yingling J,
Lahn M, Glatt S and Trocóniz IF: Semi-mechanistic modelling of the
tumour growth inhibitory effects of LY2157299, a new type I
receptor TGF-beta kinase antagonist, in mice. Eur J Cancer.
44:142–150. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
de Gouville AC, Boullay V, Krysa G, Pilot
J, Brusq JM, Loriolle F, Gauthier JM, Papworth SA, Laroze A,
Gellibert F and Huet S: Inhibition of TGF-beta signaling by an ALK5
inhibitor protects rats from dimethylnitrosamine-induced liver
fibrosis. Br J Pharmacol. 145:166–177. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Leung SY, Niimi A, Noble A, Oates T,
Williams AS, Medicherla S, Protter AA and Chung KF: Effect of
transforming growth factor-beta receptor I kinase inhibitor
2,4-disubstituted pteridine (SD-208) in chronic allergic airway
inflammation and remodeling. J Pharmacol Exp Ther. 319:586–594.
2006. View Article : Google Scholar : PubMed/NCBI
|