Introduction
Osteochondromas, also termed osteocartilaginous
exostoses, comprise the majority of bone tumours in the human
skeleton. These tumours are benign osseous growths that are capped
with hyaline cartilage (1). Solitary
osteochondromas develop in a single bone and are not hereditary. By
contrast, multiple osteochondromas, also known as hereditary
multiple osteochondromas (HMO), result from an autosomal dominant
disorder characterised by the abundant proliferation of exostoses
(2). Genetic studies have identified
an association between HMO and three loci: i) Exostosin-1 (EXT1)
(3), which maps to chromosome 8q24.1;
ii) EXT2 (4), which maps to
chromosome 11p13; and iii) EXT3 (5),
which is located on the short arm of chromosome 19 (the exact
position has yet to be mapped). It has been estimated that half of
all patients with HMO have EXT1 mutations, while one-third have
EXT2 mutations (6).
Multiple osteochondromas typically increase in size
and number during childhood and adolescence. Although these tumours
primarily develop at the juxta-epiphyseal region of the long bones,
they can occur on nearly every bone of the skeleton, including
short bones, flat bones and irregular bones (7). Patients with HMO are generally
asymptomatic, unless the osteochondroma exerts pressure on adjacent
muscles, tendons, nerves or blood vessels (8). The clinical presentation is commonly
associated with this effect, and includes pain, angular
deformities, short stature, restricted joint motion, fractures of
the lesion itself, inflammatory changes of the bursa exostotica
covering the cartilage cap and malignant transformation (9).
Osteochondromas typically occur around the growth
plate of long bones in childhood and then move toward the diaphysis
as growth occurs (10). Therefore,
osteochondromas are generally located extra-articularly.
Intra-articular osteochondromas are rare, but do occur, and may
cause pain and discomfort, as well as range-of-motion
restrictions.
The present study investigated the clinical,
imaging, histological and genetic aspects of a 27-year-old male
patient with typical HMO who presented with intra-articular
osteochondromas, manifesting as bony loose bodies within the knee
joint. To the best of our knowledge, the present case is the first
reported incidence of intra-articular osteochondromas manifesting
as >1 loose body in the joint of a patient with HMO. In
addition, the current study performed genetic analysis of the
patient and the patient's family members with the aim of
identifying the underlying mutation causing HMO in this family.
Case report
A 27-year-old male patient of short stature,
presented to Zhejiang Provincial People's Hospital (Hangzhou,
China) on May 5th, 2013, with multiple elevated bony prominences
and a limited ability to bend the right knee, which had been
ongoing for 10 years. No history of trauma was reported by the
patient. The bony prominences and surface anomalies were
asymptomatic, and initially arose when the patient was 6 years old;
the bony prominences had progressively increased in size and number
since, with pain initially experienced 10 years previously, on
maximal flexion of the knee. The patient progressively experienced
limitation in squatting ability. He was also was uncomfortable with
the appearance of the multiple osteochondromas.
The patient had a family history of HMO on the
maternal side. The patient's mother was also of short stature and
had multiple elevated exostoses in various locations, although no
limitations in joint mobility. The patient's maternal grandmother
and uncle had also been diagnosed with HMO. However, these two
family members had succumbed to unknown causes a number of years
previously.
Physical examination revealed multiple bony
prominences around the knees and no significant symptoms at rest.
However, there was significant pain in the right knee joint during
loaded flexion. Although the patient was capable of full extension,
maximum flexion was 85°. The collateral and cruciate ligaments were
stable, and the medial joint line and medial femoral condyle were
tender to palpation. The function of his left knee was normal.
Plain radiographs demonstrated an intra-articular, mineralised mass
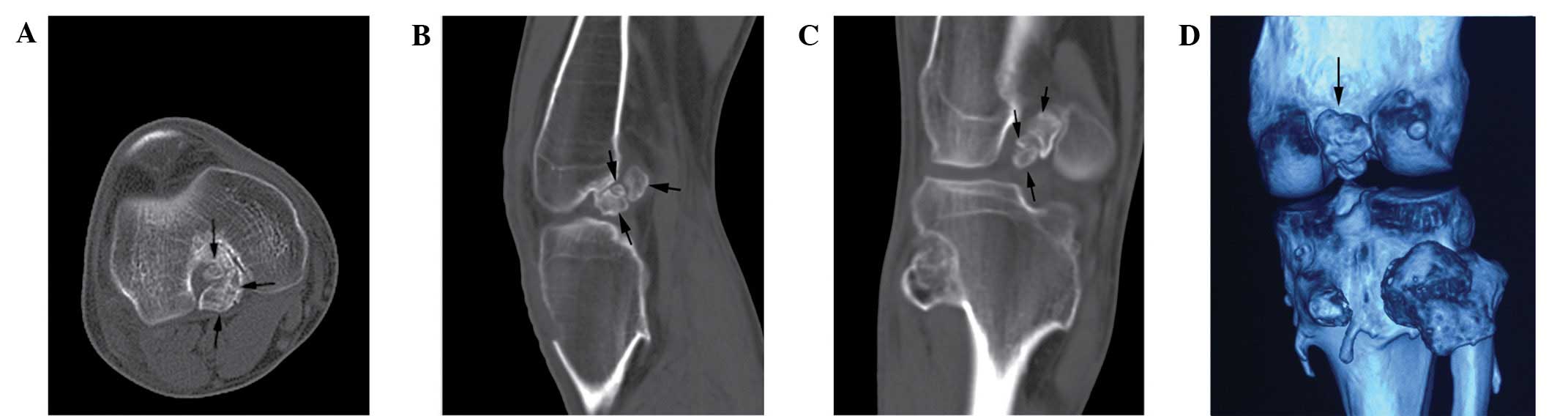
at the intercondylar fossa (Fig. 1).
Computed tomography (CT) and three-dimensional CT reconstruction of
the right knee revealed three mineralised masses manifesting as
loose bodies at the intercondylar fossa and no abnormalities in
other intra-articular structures (Fig.
2). In addition, magnetic resonance imaging (MRI) revealed that
the anterior mass was located in close proximity to the posterior
cruciate ligament (PCL; Fig. 3).
Due to the pain and limited range of motion
experienced by the patient, as well as limited knowledge of the
exact nature of the lesion, an arthroscopic excision was performed.
The knee was passively flexed under general anaesthesia. A
decreased range of flexion with maximum flexion of 85°, was
observed. Arthroscopic standard portals were created and the
intercondylar view revealed an oval mass with a cartilaginous
surface between the concave condyles. The mass was located
posterior to the anterior cruciate ligament (ACL) and adjacent to
the PCL. The mass filled the majority of the intercondylar fossa
space and mild synovial joint hyperplasia was observed. The
ligaments, cartilage and menisci were intact, and patellar tracking
was normal. A probe demonstrated that the mass had limited
mobility, indicating that the mass was a loose body (Fig. 4A). The lesions was then removed, and a
further small mass was observed, just posterior to the first
(Fig. 4B). This small mass was also
removed and a third large mass was observed posterior to the PCL
(Fig. 4C). The two posterior masses
also appeared to be loose bodies. The third mass was removed and
the intercondylar fossa was free of bony tissue (Fig. 4D). The knee was bent again and a
dramatic improvement in flexion was observed (maximum flexion,
110°), demonstrating that the intra-articular masses had been
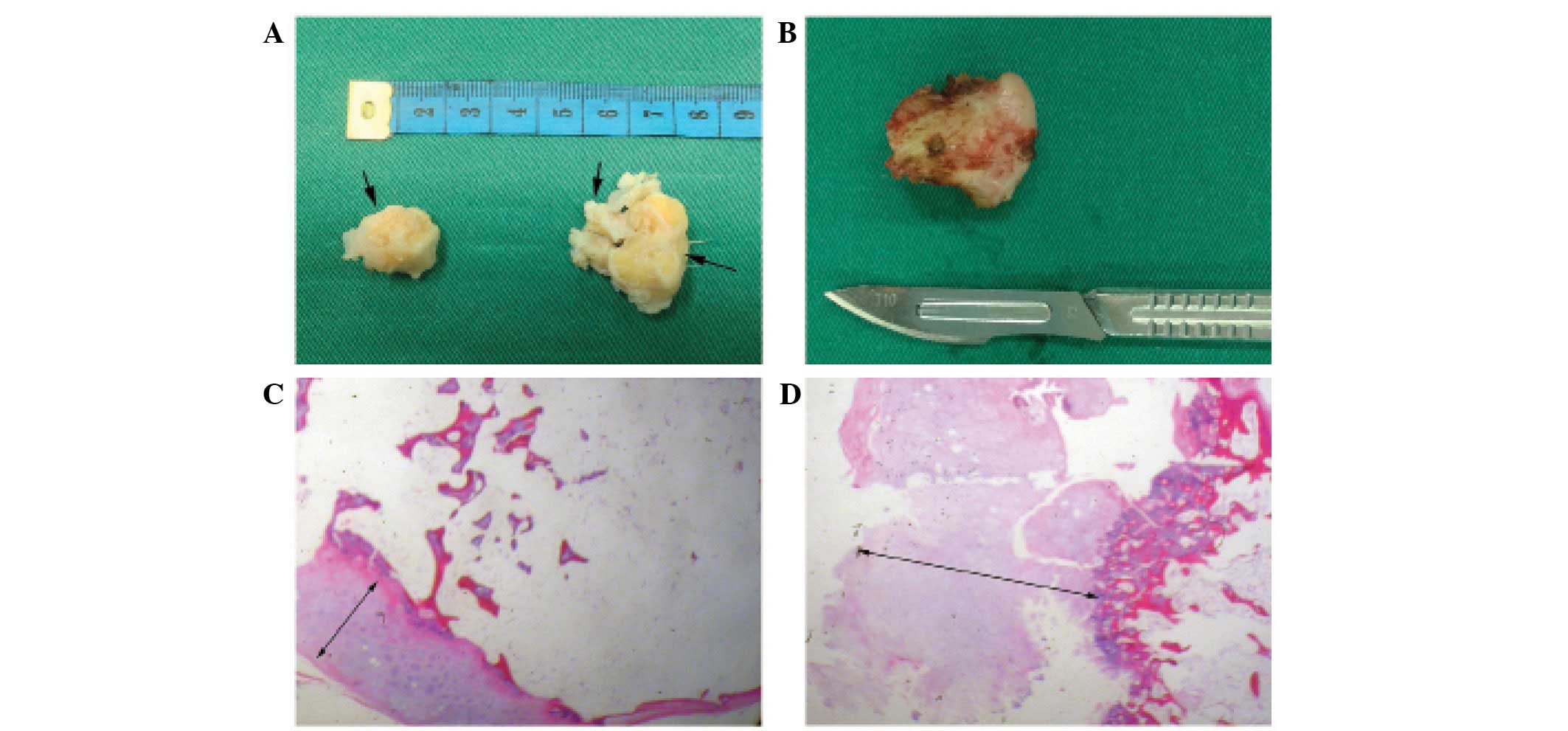
preventing the right knee from fully flexing. Macroscopically, the
three excised masses measured 2.0×1.5×1.5 cm, 1.0×1.0×0.5 cm and
3.0×3.0×2.0 cm, respectively (Fig.
5A). For aesthetic reasons, the protuberant extra-articular
osteochondromas in the tibia and femur around the right knee were
also resected with small incisions. Pathological analysis under the
microscope (BX50; Olympus Corporation, Tokyo, Japan) demonstrated
that the extra-articular masses were typical osteochondromas, which
were composed of three layers (fibrous perichondrium, cartilage cap
and bone; Fig. 5D). However, in
contrast to the extra-articular osteochondromas, pathological
examination of the intra-articular osteochondromas revealed thinner
layers of fibrous perichondrium and cartilage cap, and a thicker
layer of bone (3.6 vs. 2.0-mm thick cartilage; Fig. 5C). Following arthroscopy, the pain
previously experienced during loaded flexion in the right knee
disappeared and the range of motion recovered to 120° degrees.
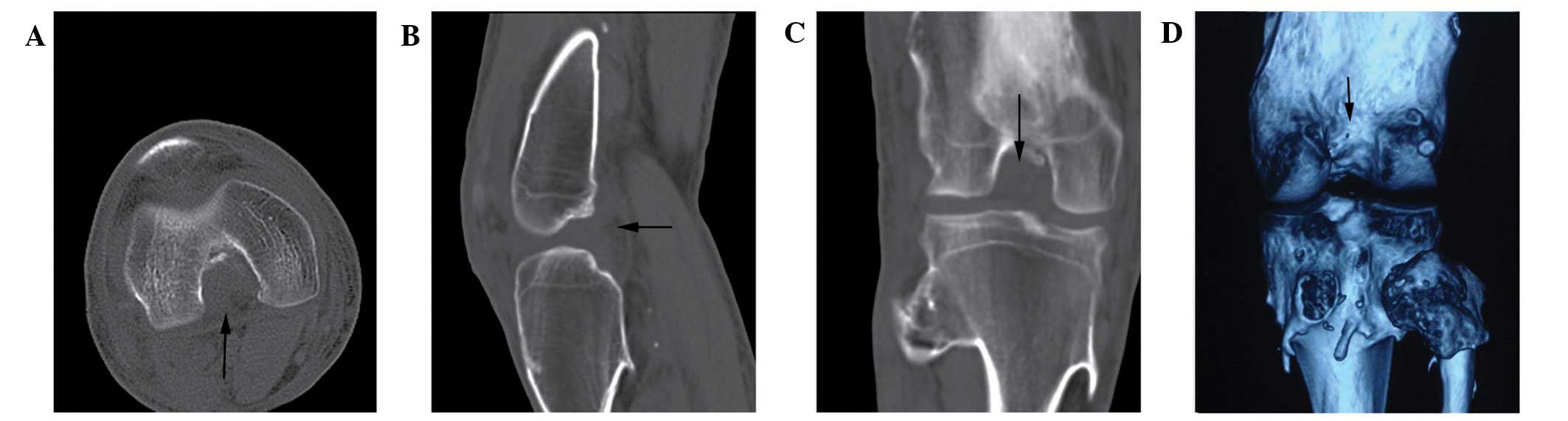
Imaging confirmed that the three masses had been removed (Fig. 6). One year after removal, the patient
was asymptomatic with respect to his knee, with no signs of
recurrence evident on radiographic analysis.
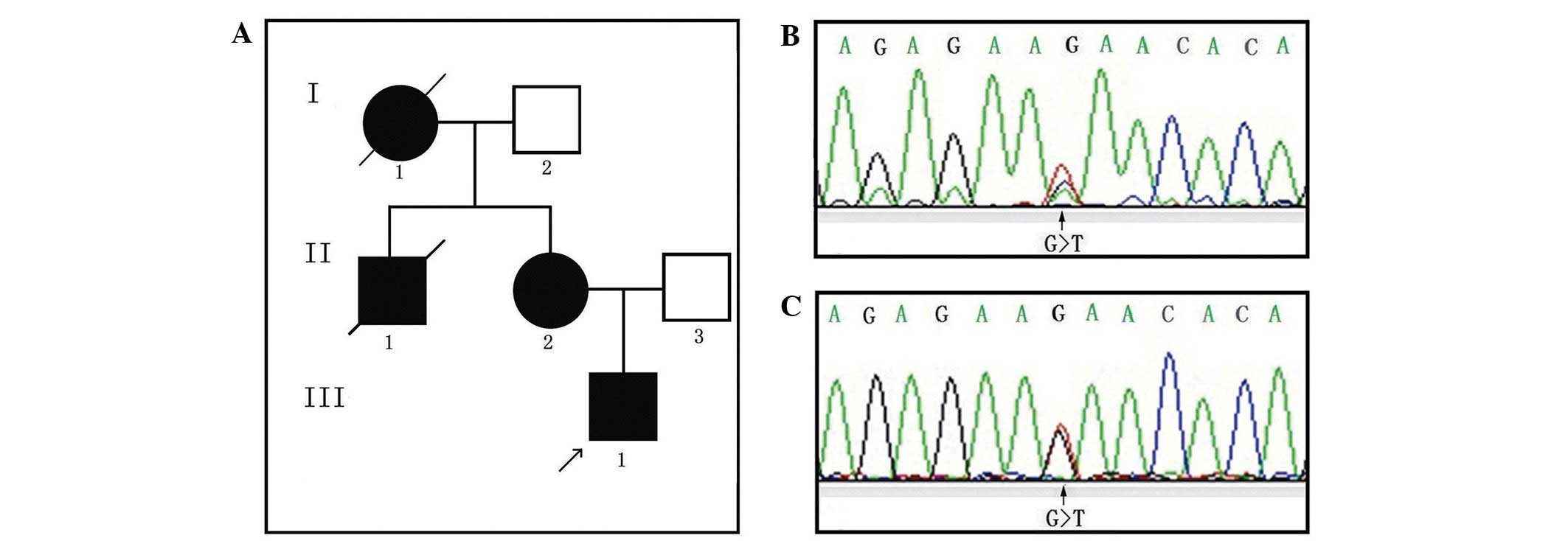
In order to determine the genetic cause of HMO in
this case, the patient and his mother underwent genetic analysis.
The pedigree of this Chinese family is shown in Fig. 7A. All study procedures were approved
by the Ethics Review Committee of the Zhejiang Provincial People's
Hospital (Hangzhou, China) and were conducted following receipt of
written informed consent from the patient and the patient's family.
Genomic DNA was purified from peripheral blood leukocytes using an
Axygen® AxyPrep Nucleic Acid Purification kit (Corning Life
Sciences, Union City, CA, USA), according to the manufacturer's
instructions. The Sanger method of direct DNA sequencing was
performed on the EXT1 and EXT2 coding regions, including the 100-bp
flanking intron-exon junctions. This was achieved by performing
polymerase chain reactions of genomic DNA followed by sequencing
reactions with Sanger sequencing chemistry, using the BigDye®
Terminator v3.1 Cycle Sequencing kit on a 3730XL automated
sequencer (Applied Biosystems Inc., Foster City, CA, USA). The
primer sequences used are those previously cited by Cao et
al (11). Sequencing data were
analyzed by Sequencer Demo 3.0 and Mutation Surveyor® Demo software
(version 4.0; SoftGenetics, LLC, State College, PA, USA) using
reference sequences from the National Center for Biotechnology
Information (NM_000127.2 for EXT1; NM_001178083.1 for EXT2).
A heterozygous mutation was identified in the
genomic DNA of the patient. A substitution in exon 1 of the EXT1
gene (c.115G>T) changed a leucine codon into a stop codon
(p.E39X) in the EXT1 protein (Fig. 7B and
C; Table I). The patient was also
heterozygous for the synonymous mutation in exon 9 of the EXT1 gene
(Table I). The same heterozygous exon
1 (c.115G>T; p.E39X) nonsense mutation and the synonymous
mutation were detected in the patient's mother. c.115G>T; p.E39X
has previously been reported as a disease-causing mutation
(12). However, to the best of our
knowledge, the current study is the first report this mutation in a
Chinese individual.
 | Table I.EXT1 gene changes detected by
polymerase chain reaction and direct sequencing. |
Table I.
EXT1 gene changes detected by
polymerase chain reaction and direct sequencing.
| ID | Gene name | Location | Nucleotide
change | Amino acid
change | Mutation type | Category |
|---|
| II2a, III1b | EXT1 | Exon 1 |
115G>T(het) |
39E>X | Nonsense | SNV |
| II2, III1 | EXT1 | Exon 9 | 1761C>T(het) | 587E>E | Synonymous | SNV |
Discussion
Intra-articular osteochondromas are rare in patients
with HMO and have, thus far, only been described as case reports in
the literature. Patients with HMO exhibit osteochondromas in the
intra-articular region of the hip and ankle joints, causing
functional joint defects in certain cases (13–15). It is
theoretically feasible that an osteochondroma could remain located
intra-articularly within the hip and ankle joints, as the neck of
the femur and the talus are located in these joints. The knee is
also a common location for intra-articular osteochondromas due to
the large size of the joint capsule. However, in the context of
HMO, intra-articular osteochondromas of the knee joint have rarely
been described. To the best of our knowledge, only two cases of
intra-articular osteochondromas in patients with HMO have been
described in the literature. Takahashi et al (8) reported the first case of a patient
exhibiting HMO with an osteochondroma in the knee joint. The mass
was located in the anterolateral site of the distal femur,
impinging upon the lateral edge of the lateral facets of the
patella and inducing an inflammatory response in the lateral
capsule of the patellofemoral joint. The second case of an
osteochondroma within the knee joint was reported by Matsumoto
et al (16). In this case, the
osteochondroma was small and manifested as a loose body measuring
~1×1×2 cm. The lesions was located posterior to the PCL, causing
pain and limited joint function. However, the present case was
distinct in a number of ways from the previous two cases. Firstly,
the current study reported a greater number of intra-articular
osteochondromas that were also larger in size. Secondly, the
intra-articular and extra-articular osteochondromas were resected
and pathologically compared. Thirdly, HMO was clinically diagnosed
in the current patient, and was also genetically diagnosed via the
identification of a nonsense mutation in the EXT1 gene.
Intra-articular osteochondromas are difficult to
visualize and are only detectable through imaging or arthroscopic
exploration. In certain cases, even the use of plain radiographs
cannot provide a definitive diagnosis. CT scans provide a clear
image of the bony structure of the joint, as well as the outline of
bony masses within it. Furthermore, MRI imaging aids in determining
the nature of the mass and clearly delineates adjacent tissues,
including ligaments and tendons. Symptoms of intra-articular
osteochondromas may result from exostotic impingement on adjacent
intra-articular structures. In the current case study, plain
radiographs identified the lesion at the intercondylar fossa. In
addition, a CT scan revealed three intra-articular masses, and MRI
was utilised to further characterise the nature of the masses and
to visualise the adjacent soft structures. The first mass was
located adjacent to the PCL; exerting pressure on the ligament
(Fig. 3). Furthermore, the area where
the three bony, loose bodies were located impacted the posterior
contour of the medial condyle of the tibia upon flexion (Fig. 2D). Therefore, the patient experienced
pain during loaded flexion, as well as a significant decrease in
bending range.
Surgical excision is the only reliable treatment
strategy for symptomatic intra-articular osteochondromas. It is
performed in order to treat the patient and as a means of making a
definitive diagnosis. Surgical excision may be performed using an
open technique or arthroscopically. Arthroscopy is minimally
invasive, does not cause significant trauma to the musculature, and
is useful for treating meniscal tears and synovitis, as well as
removing loose bodies from the joint. The treatment of
intra-articular osteochondroma with precise extension using
arthroscopic techniques has recently been reviewed in a number of
studies and has demonstrated good overall results (8,16,17). The advantages of arthroscopic
resection of osteochondromas include a cosmetically pleasing
result, a potentially less painful procedure, tailored resection of
the lesion and a low complication rate. This technique also results
in rapid recovery (17).
The origin and pathogenesis of the intra-articular
loose osteochondromas presented in the current study are
controversial. In specific cases of extraskeletal osteochondromas,
the origin of intra-articular osteochondromas have been shown to be
soft tissues (18,19). Jaffe (20) initially introduced the concept of
para-articular osteochondromas in 1958, using the synonymous terms
para-articular chondromas and intracapsular chondromas to describe
osteochondral metaplasia occurring in the fibrous joint capsule or
soft tissue adjacent to the joint. Subsequently, Milgram and Dunn
(19) used the term para-articular
osteochondroma to differentiate between intra-articular
osteochondroma and synovial osteochondromatosis. Synovial
osteochondromatosis typically includes multiple osteochondrous
synovium nodules with loose bodies in the joint (21); the multiple lobules of proliferative
cartilage originate in the synovial joint tissue. By contrast,
para-articular osteochondromas originate from a cartilaginous
metaplasia of the articular and para-articular connective tissues
(22). They are typically composed of
a single large calcified mass of multiple osteochondral nodules,
with no histological evidence of a synovial origin (23). The two aforementioned osteochondromas
originate from intra-articular soft tissues and are therefore not
true osteochondromas, which originate in the growth plates of long
bones.
However, the patient in the present case may not
represent either of these types of osteochondromas. The current
patient was clinically and genetically diagnosed with HMO, and
histological analysis of the intra-articular osteochondroma did not
reveal any evidence of synovial or other soft tissue origin.
Additionally, histological analysis demonstrated that the
intra-articular osteochondroma appeared to have a thinner cartilage
cap. This indicates that the osteochrondroma may have stopped
growing for a long time period, as the thickness of the cartilage
cap is positively correlated with the growth activity of the
osteochondroma and growth rate decreases with age (24). Once osteochondromas stop growing, the
cartilage cap shrinks due to compression by adjacent structures.
Therefore, it is proposed that the osteochondroma in the case
described, originated at the posterior end-plate of the femur or
tibia a number of years prior to presentation and grew towards the
articular cavity of the knee. The pedicle may subsequently have
torn, allowing the osteochondroma to become loose in the knee
joint. At that point, growth of the osteochondroma may have
stopped. As the mass remained in the intercondylar fossa of the
knee and was compressed by the bony structure of the intercondylar
fossa, the cartilage cap may have begun to degenerate. Exposure to
the synovial fluid and movement of the knee over time may have
caused a single loose osteochondroma to divide into three distinct
masses. However, the aetiology of the intra-articular
osteochondromas described in the present study, as well as the
histological differences between intra-articular and
extra-articular osteochondromas in the context of HMO, remains
unknown and requires further investigation.
Acknowledgements
The authors would like to thank the patient and his
family members for their interest and cooperation. The present
study was supported by a grant, awarded to Professor Qing Bi, by
the Natural Science Foundation of Zhejiang Province (grant no.
Y2100731) and the Medical Science and Technology Project in
Zhejiang Province (grant no. Y201024964).
References
|
1
|
Stieber JR and Dormans JP: Manifestations
of hereditary multiple exostoses. J Am Acad Orthop Surg.
13:110–120. 2005.PubMed/NCBI
|
|
2
|
Solomon L: Hereditary Multiple Exostosis.
Am J Hum Genet. 16:351–363. 1964.PubMed/NCBI
|
|
3
|
Cook A, Raskind W, Blanton SH, Pauli RM,
Gregg RG, Francomano CA, Puffenberger E, Conrad EU, Schmale G,
Schellenberg G, et al: Genetic heterogeneity in families with
hereditary multiple exostoses. Am J Hum Genet. 53:71–79.
1993.PubMed/NCBI
|
|
4
|
Wu YQ, Heutink P, de Vries BB, Sandkuijl
LA, van den Ouweland AM, Niermeijer MF, Galjaard H, Reyniers E,
Willems PJ and Halley DJ: Assignment of a second locus for multiple
exostoses to the pericentromeric region of chromosome 11. Hum Mol
Genet. 3:167–171. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Le Merrer M, Legeai-Mallet L, Jeannin PM,
Horsthemke B, Schinzel A, Plauchu H, Toutain A, Achard F, Munnich A
and Maroteaux P: A gene for hereditary multiple exostoses maps to
chromosome 19p. Hum Mol Genet. 3:717–722. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Porter DE, Lonie L, Fraser M, Dobson-Stone
C, Porter JR, Monaco AP and Simpson AH: Severity of disease and
risk of malignant change in hereditary multiple exostoses. A
genotype-phenotype study. J Bone Joint Surg Br. 86:1041–1046. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cao L, Liu F, Kong M, Fang Y, Gu H, Chen
Y, Zhao C, Zhang S and Bi Q: Novel EXT1 mutation identified in a
pedigree with hereditary multiple exostoses. Oncol Rep. 31:713–718.
2014.PubMed/NCBI
|
|
8
|
Takahashi M, Nishihara A, Ohishi T, Shiga
K, Yamamoto K and Nagano A: Arthroscopic resection of an
intra-articular osteochondroma of the knee in the patient with
multiple osteochondromatosis. Arthroscopy. 20 (Suppl 2):28–31.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vanhoenacker FM, Van Hul W, Wuyts W,
Willems PJ and De Schepper AM: Hereditary multiple exostoses: From
genetics to clinical syndrome and complications. Eur J Radiol.
40:208–217. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wicklund CL, Pauli RM, Johnston D and
Hecht JT: Natural history study of hereditary multiple exostoses.
Am J Med Genet. 55:43–46. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cao L, Liu F, Kong M, Fang Y, Gu H, Chen
Y, Zhao C, Zhang S and Bi Q: Novel EXT1 mutation identified in a
pedigree with hereditary multiple exostoses. Oncol Rep. 31:713–718.
2014.PubMed/NCBI
|
|
12
|
Alvarez CM, De Vera MA, Heslip TR and
Casey B: Evaluation of the anatomic burden of patients with
hereditary multiple exostoses. Clin Orthop Relat Res. 462:73–79.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bonnomet F, Clavert P, Abidine FZ, Gicquel
P, Clavert JM and Kempf JF: Hip arthroscopy in hereditary multiple
exostoses: A new perspective of treatment. Arthroscopy. 17:E402001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
El-Fiky TA, Chow W, Li YH and To M:
Hereditary multiple exostoses of the hip. J Orthop Surg (Hong
Kong). 17:161–165. 2009.PubMed/NCBI
|
|
15
|
Rook FR: Intra-articular osteochondroma of
the astragalus. Am J Surg. 85:807–810. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Matsumoto Y, Matsuda S, Matono K, Oda Y,
Tsuneyoshi M and Iwamoto Y: Intra-articular osteochondroma of the
knee joint in a patient with hereditary multiple
osteochondromatosis. Fukuoka Igaku Zasshi. 98:425–430.
2007.PubMed/NCBI
|
|
17
|
Schmoyer S and Ciullo JV: Arthroscopic
resection of an osteochondroma of the knee. Arthroscopy.
17:765–767. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Das AK and Mukherjee DR: Giant
osteochondral loose body of the knee joint. A case report. J Bone
Joint Surg Am. 60:559–560. 1978.PubMed/NCBI
|
|
19
|
Milgram JW and Dunn EJ: Para-articular
chondromas and osteochondromas: A report of three cases. Clin
Orthop Relat Res. 148:147–151. 1980.PubMed/NCBI
|
|
20
|
Jaffe HL: Tumors and tumorous conditions
of the bones and joints. Acad Med. 34:721959. View Article : Google Scholar
|
|
21
|
Schofield TD, Pitcher JD and Youngberg R:
Synovial chondromatosis simulating neoplastic degeneration of
osteochondroma: Findings on MRI and CT. Skeletal Radiol. 23:99–102.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rizzello G, Franceschi F, Meloni MC,
Cristi E, Barnaba SA, Rabitti C and Denaro V: Para-articular
osteochondroma of the knee. Arthroscopy. 23:910.e1–910.e4. 2007.
View Article : Google Scholar
|
|
23
|
Karlin CA, De Smet AA, Neff J, Lin F,
Horton W and Wertzberger JJ: The variable manifestations of
extraarticular synovial chondromatosis. AJR Am J Roentgenol.
137:731–735. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hudson TM, Springfield DS, Spanier SS,
Enneking WF and Hamlin DJ: Benign exostoses and exostotic
chondrosarcomas: Evaluation of cartilage thickness by CT.
Radiology. 152:595–599. 1984. View Article : Google Scholar : PubMed/NCBI
|