Introduction
Paraneoplastic neurological syndromes are usually
attributed to autoimmune processes directed against onconeural
antigens (1), which are common to
cancer cells and the nervous system. Lambert-Eaton myasthenic
syndrome (LEMS) is the most common neurological paraneoplastic
syndrome (2). LEMS is a neuromuscular
junction disorder characterized by fluctuating proximal limb muscle
weakness, decreased deep tendon reflexes and various autonomic
symptoms. The etiology of LEMS is reduced exocytosis of
acetylcholine from nerve endings caused by antibodies directed
against voltage-gated calcium channels (VGCCs), increases in the
titers of which are observed in >90% of patients with LEMS
(3).
LEMS is most frequently associated with small-cell
lung cancer (SCLC) (4). The estimated
annual incidence of LEMS is ~10 times lower compared with that of
myasthenia gravis (MG), and its frequency in patients with SCLC is
~3% (2). In cases of patients with
SCLC and LEMS, a primary diagnosis of LEMS may lead to the
identification of early-stage SCLC and a better prognosis compared
with that of patients with SCLC alone. However, there is currently
no clinical manifestation specific to LEMS or a conclusive test for
its diagnosis. The most commonly reported symptom by patients with
LEMS is proximal muscle weakness, which is a non-specific symptom
that may associated with a number of other diseases (5).
The present case emphasizes that clinicians must
remain alert for recognising LEMS, particularly in patients
presenting with muscle weakness. This study was approved by the
Ethics Committee of the People's Liberation Army General Hospital
of Shenyang Military Region (Shenyang, China). The patient signed a
written informed consent regarding publication of his medical
information.
Case report
A 68-year-old male patient was admitted to the
Department of Neurology of the People's Liberation Army General
Hospital of Shenyang Military Region with xerostomia and
progressive limb muscle weakness. The weakness was initially
noticed in the proximal lower limb musculature, followed by the
upper limbs. The patient stated that his proximal limbs were so
weak that he could not stand unaided, and that he had lost the
ability to live independently. The patient did not report any
diurnal variation of weakness and had never experienced persistent
cough or hemoptysis. The patient had smoked one pack of cigarettes
a day for 50 years. The family history was unremarkable.
A neurological examination revealed proximal muscle
weakness and absence of deep tendon reflexes. The cranial nerve,
cerebellar and sensory functions were all normal. The laboratory
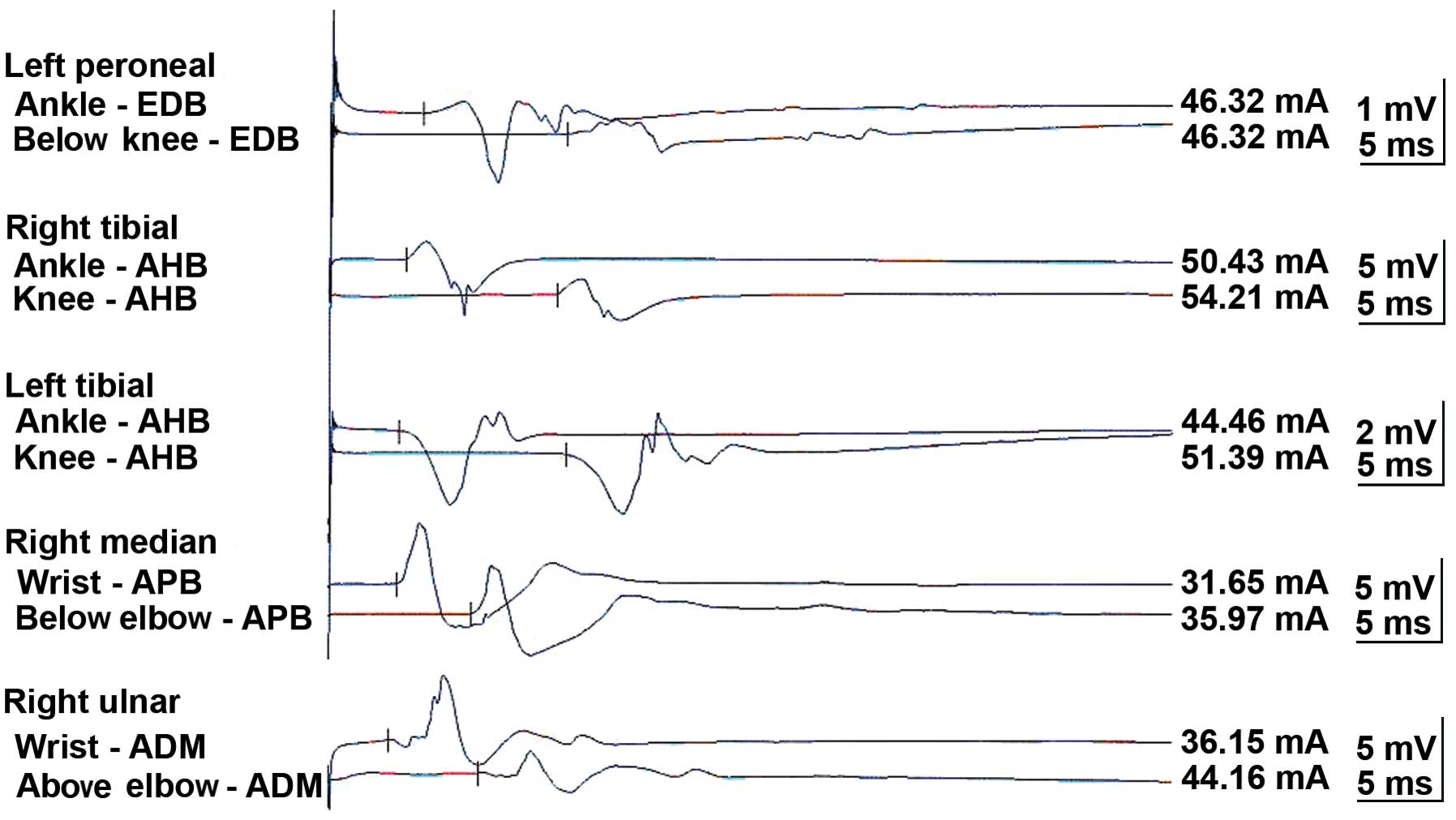
tests revealed hyponatremia and hypochloremia. The electromyogram
suggested neurogenic damage (Bilateral abductor muscle and peroneus
longus, potential loss of the median nerve, the common peroneal
nerve, and mild slowing of the motor conduction velocity of the
tibial nerve). A repetitive nerve stimulation test performed on the
right median nerve revealed a decremental response to the
electrical stimulation. An experiment with neostigmine supported
the presence of postsynaptic membrane lesions. Repeated nerve
stimulation of 7 Hz lead to an increased response, whereas repeated
nerve stimulation of 15 Hz was associated with decreased response
(Fig. 1). The findings of magnetic
resonance imaging scans of the brain and lumbar vertebra were
normal. The preliminary diagnosis of the patient's condition was
MG. However, treatment with hypertonic saline and fluid
restriction, as well as low-dose corticosteroid therapy for MG, did
not improve the symptoms. After referring to several studies in the
literature (6–8), LEMS was taken into consideration. The
levels of tumor markers, including carcinoembryonic antigen and
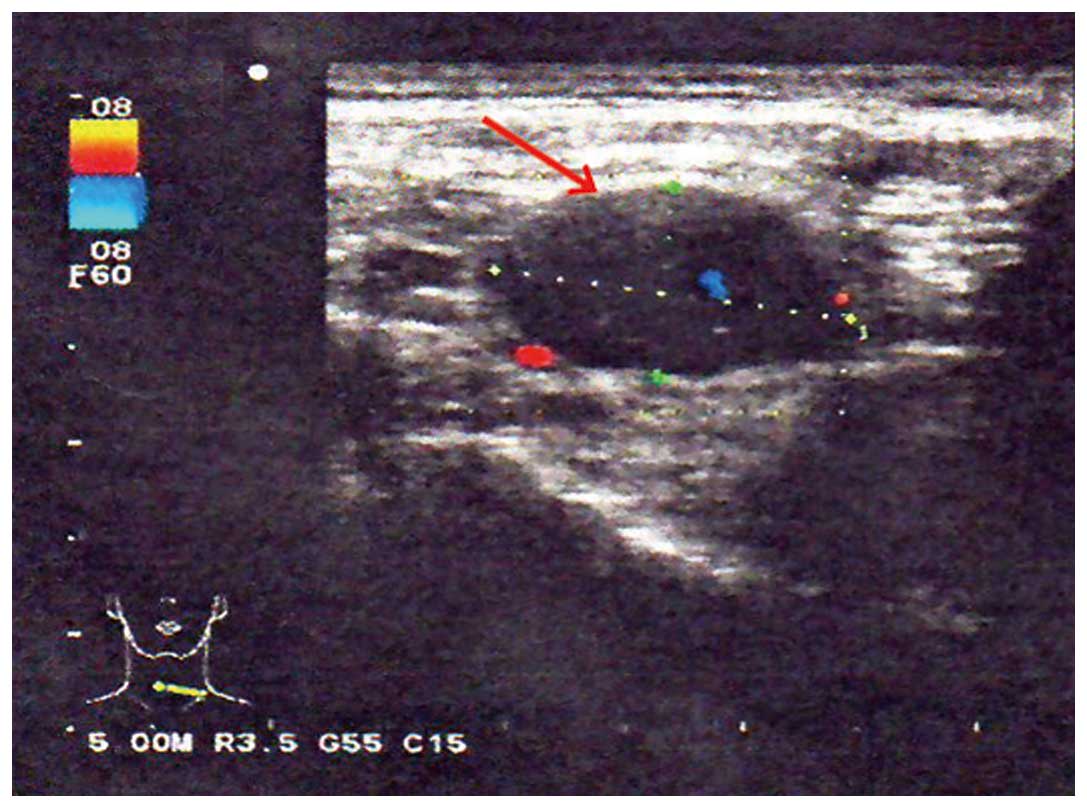
neuron-specific enolase, were found to be abnormal. An ultrasound
of the superficial lymph nodes identified an enlarged lymph node in
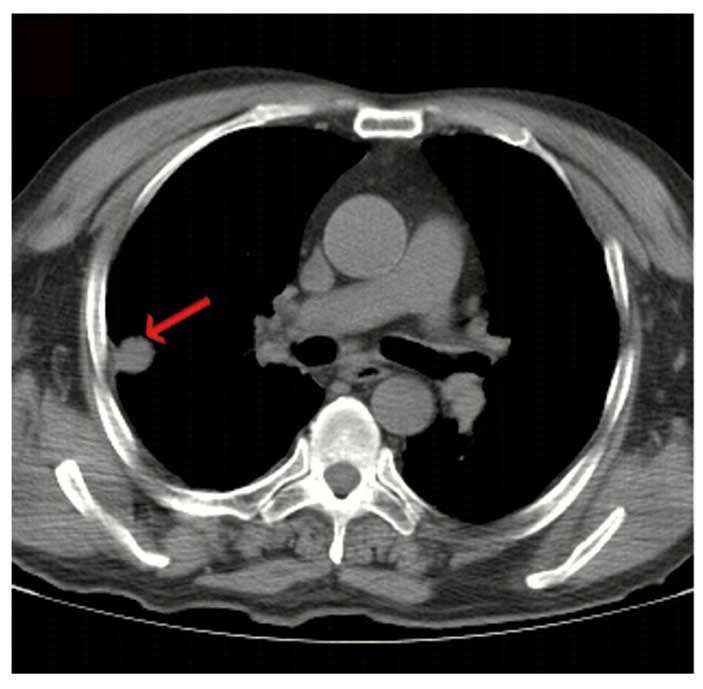
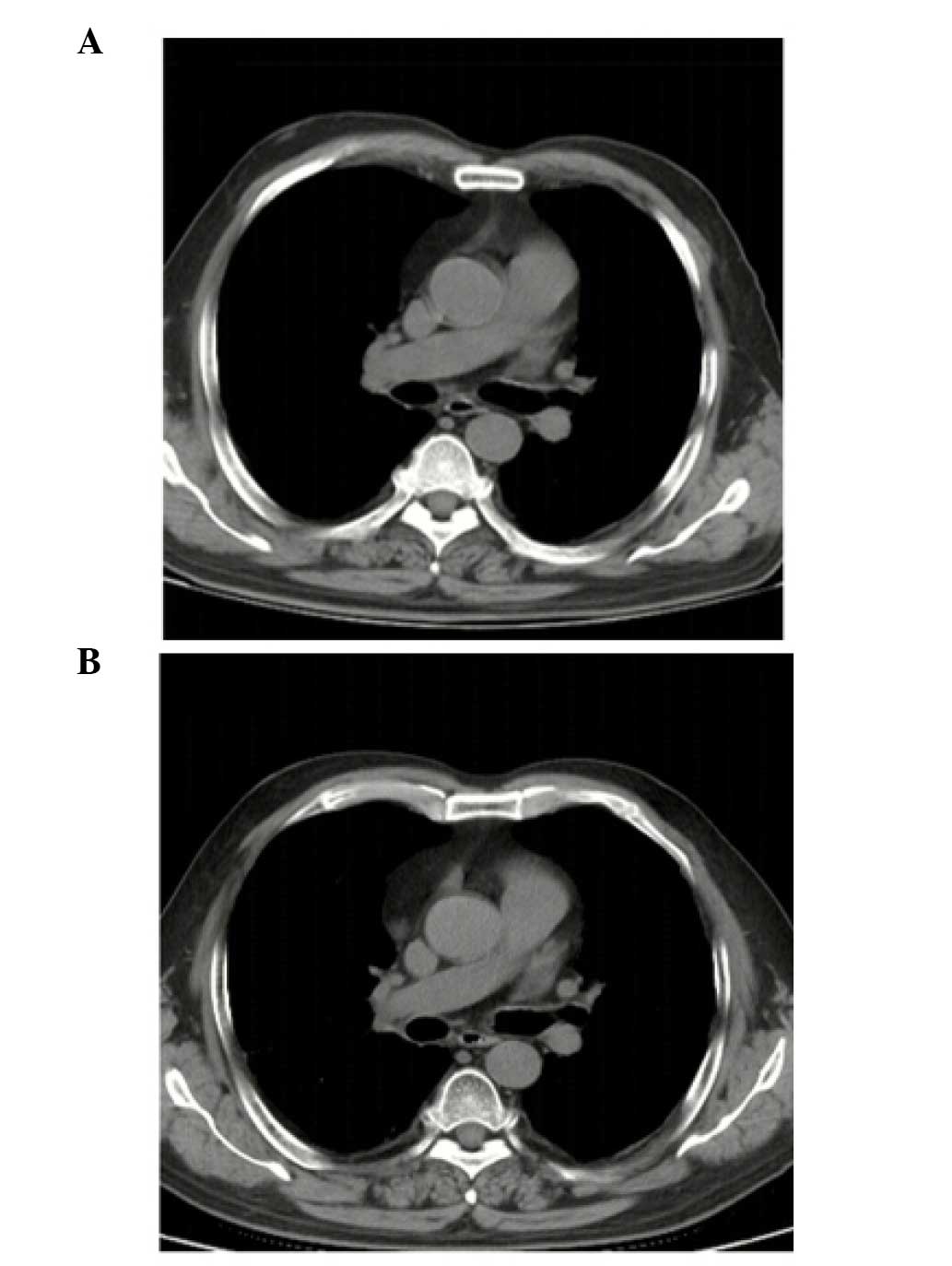
the right cervical region, sized 1.5×0.9 cm (Fig. 2). Chest computed tomography (CT)
images revealed a 1.6-cm mass in the superior lobe of the right
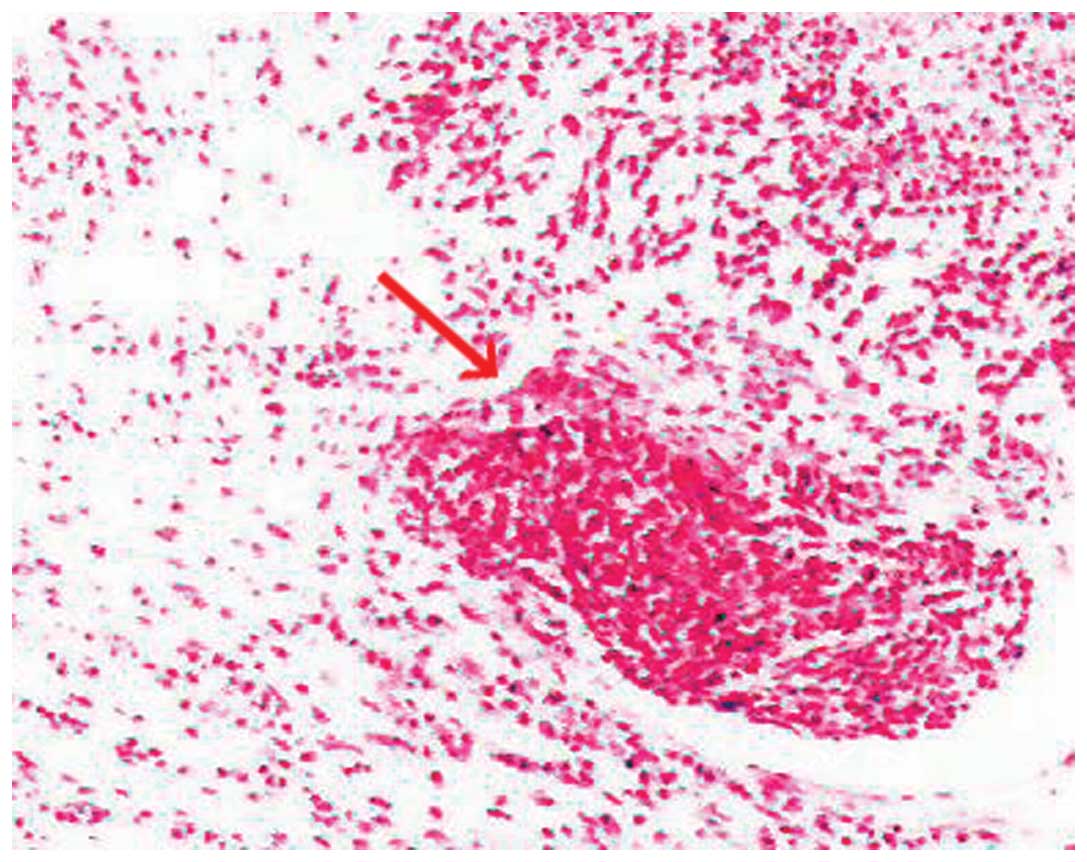
lung, associated with a small amount of pleural effusion (Fig. 3). A right cervical lymph node biopsy
was conducted; on pathological immunohistochemical examination, the
lesion was found to be positive for epithelial membrane antigen
(+), CD56 (+), thyroid transcription factor-1 (+), creatine
phosphokinase (+) and Ki67 (+++) and negative for synaptophysin and
leukocyte common antigen. Combined with the findings of the
histopathological analysis (hematoxylin and eosin staining;
Fig. 4), the diagnosis was eventually
confirmed as SCLC combined with LEMS.
In accordance with the National Comprehensive Cancer
Network guidelines, the patient was administered etoposide and
cisplatin (EP) chemotherapy. After two cycles of EP, the patient
exhibited a noticeable improvement in muscular strength (Fig. 5A), was able to walk without
assistance, and his ability to live independently was restored.
After six cycles of chemotherapy, the primary malignancy
disappeared (Fig. 5B) and the sodium
and chloride levels returned to normal. The response was evaluated
as complete, according to the Response Evaluation Criteria in Solid
Tumors 1.0. The patient is currently followed up and remains
recurrence- and metastasis-free.
Discussion
In the present case, the main symptom of the patient
was the progressive weakness of the limbs, particularly of the
proximal muscles. No evident aggravating factors were associated
with the onset of the weakness. Thus, when muscle weakness is
present, LEMS should be taken into consideration.
Whether the syndrome of inappropriate antidiuretic
hormone secretion (SIADH) existed in the present case remains
unknown. Since SCLC also causes SIADH (9) and the laboratory tests revealed the
presence of hyponatremia and hypochloremia, the muscle weakness may
have also been associated with SIADH, as well as LEMS. However,
laboratory evidence is required to determine whether the symptoms
should be attributed to SIADH rather than LEMS.
The median survival of SCLC patients is 7–8 months.
Although the efficiency of first-line chemotherapy is 60%, nearly
all the patients recur within 1 year (10). Our patient remains alive for 3 years,
without evidence of recurrence or metastasis. Thus, in patients
with LEMS, the presence of a paraneoplastic syndrome should be
considered. LEMS may be a favorable factor for the prognosis of
SCLC (11,12). VGCCs are usually blocked in patients
with LEMS. Antibodies against P/Q type VGCCs inhibit acetylcholine
release from the motor nerve terminals, resulting in muscle
weakness (13). Anti-VGCC antibodies
may play a role in controlling tumor growth, or alternatively, SCLC
may cause LEMS to develop slowly (11). However, these possible explanations
require further confirmation by a large clinical sample.
In conclusion, a diagnosis of LEMS may lead to the
early detection of SCLC, as the clinical symptoms of LEMS usually
precede cancer detection (14).
Although SCLC is a highly malignant disease with poor prognosis
(15), early detection and treatment
through diagnosing a paraneoplastic syndrome may significantly
improve patient survival.
Acknowledgements
This study was funded by a grant from the National
Research Key Project of the Twelfth Five-Year Plan of P.R. China
(no. 2012ZX09303016-002).
References
|
1
|
Kida E, Barcikowska M, Michalska T, et al:
Peripheral nervous system alterations in small cell lung cancer.
Clinico-pathological study. Neuropatol Pol. 30:43–56.
1992.PubMed/NCBI
|
|
2
|
Sanders DB and Juel VC: The Lambert-Eaton
myasthenic syndrome. Handb Clin Neurol. 91:273–283. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee JH, Shin HY, Kim SM and Sunwoo IN: A
case of Lambert-Eaton myasthenic syndrome with small-cell lung
cancer and transient increase in
anti-acetylcholine-receptor-binding antibody titer. J Clin Neurol.
8:305–307. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Struthers CS: Lambert-Eaton myasthenic
syndrome in small cell lung cancer: nursing implications. Oncol
Nurs Forum. 21:677–683; quiz 684–685. 1994.PubMed/NCBI
|
|
5
|
Vincent A, Clover L, Buckley C, et al:
Evidence of underdiagnosis of myasthenia gravis in older people. J
Neurol Neurosurg Psychiatry. 74:1105–1108. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sabater L, Höftberger R, Boronat A, Saiz
A, Dalmau J and Graus F: Antibody repertoire in paraneoplastic
cerebellar degeneration and small cell lung cancer. PLoS One.
8:e604382013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Portaro S, Parisi MD, Polizzi A, Ruggieri
M, Andreetta F, Bernasconi P, Toscano A and Rodolico C: Long-term
follow-up in infantile-onset lambert-eaton myasthenic syndrome. J
Child Neurol. 29:58–61. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arai H, Inui K, Hashimoto K, et al: Lung
adenocarcinoma with Lambert-Eaton myasthenic syndrome indicated by
voltage-gated calcium channel: A case report. J Med Case Rep.
6:2812012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fernandez-Torron R, Arcocha J,
López-Picazo JM, et al: Isolated dysphagia due to paraneoplastic
myasthenic syndrome with anti-P/Q-type voltage-gated
calcium-channel and anti-acetylcholine receptor antibodies.
Neuromuscul Disord. 21:126–128. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kuo YH, Lin ZZ, Yang YY, et al: Survival
of patients with small cell lung carcinoma in Taiwan. Oncology.
82:19–24. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ray S, Sonthalia N, Kundu S, et al:
Lambert-Eaton myasthenic syndrome and solitary cerebellar
metastasis in a patient with occult small-cell lung cancer: a rare
experience. BMJ Case Rep 2012:2012.
|
|
12
|
Titulaer MJ, Wirtz PW, Willems LN, et al:
Screening for small-cell lung cancer: a follow-up study of patients
with Lambert-Eaton myasthenic syndrome. J Clin Oncol. 26:4276–4281.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim YI and Neher E: IgG from patients with
Lambert-Eaton syndrome blocks voltage-dependent calcium channels.
Science. 239:405–408. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nixdorf DR, Peters E and Lung KE: Clinical
presentation and differential diagnosis of nasolabial cyst. J Can
Dent Assoc. 69:146–149. 2003.PubMed/NCBI
|
|
15
|
Siegel R, Ward E, Brawley O and Jemal A:
Cancer statistics, 2011: the impact of eliminating socioeconomic
and racial disparities on premature cancer deaths. CA Cancer J
Clin. 61:212–236. 2011. View Article : Google Scholar : PubMed/NCBI
|