Introduction
Extranodal marginal zone B-cell lymphoma (MZL) of
mucosa-associated lymphoid tissue (MALT), and splenic and nodal MZL
are the three subtypes of MZL recognized by the World Health
Organization (WHO) classification (1). Overall, MZLs share morphological and
immunophenotypical features that are similar to those of the
hypothesized common cell of origin, the marginal zone B-cell in
secondary B-follicles.
Extranodal MZL, also termed MALT lymphoma, is a
distinct subgroup of non-Hodgkin's lymphoma (NHL) that accounts for
~5% of all NHLs (1,2). Despite the stomach being the most
frequently involved organ in extranodal MZL, the lung is one of the
most common non-gastrointestinal sites of occurrence (3,4).
Extranodal MZL accounts for <0.5% of all primary lung neoplasms,
but more than two-thirds of primary pulmonary NHLs are extranodal
MZLs (5–7). Pulmonary MALT-MZL exhibits no clear
symptoms and thus, the disease is usually identified during routine
chest X-ray examinations (8).
Pulmonary MALT-MZL is diagnosed by imaging examination and biopsy
(9,10)
and the main treatment modalities for MALT-MZL include surgery,
radiotherapy and chemotherapy (11,12).
Pulmonary MALT-MZL exhibits a good prognosis, with a five-year
survival rate of 93.6% (8,13).
Due to the non-specific clinical manifestations of
pulmonary MALT-MZL, misdiagnosis is frequently observed in clinical
practice. The present study describes the presentation and
diagnosis of one patient with pulmonary MALT-MZL, and aims to
provide evidence for the accurate diagnosis of pulmonary MALT-MZL.
Written informed consent was obtained from the patient.
Case report
A 49-year-old male was referred to The First
Affiliated Hospital of Xi'an JiaoTong University (Xi'an, Shaanxi,
China) with a pulmonary lesion in the right upper lung observed on
a chest radiograph that was performed during a routine health
checkup at a local hospital. The patient had smoked for >20
years and reported no history of respiratory illness, such as
tuberculosis. The vital signs of the patient were normal, and a
physical examination revealed no abnormalities.
The laboratory data were within the normal ranges,
with the exception of a tumor marker, carcinoembryonic antigen
(CEA), which possessed a level of 5.24 ng/ml (normal range, 0–3.4
ng/ml). Pulmonary function testing revealed no ventilatory defects.
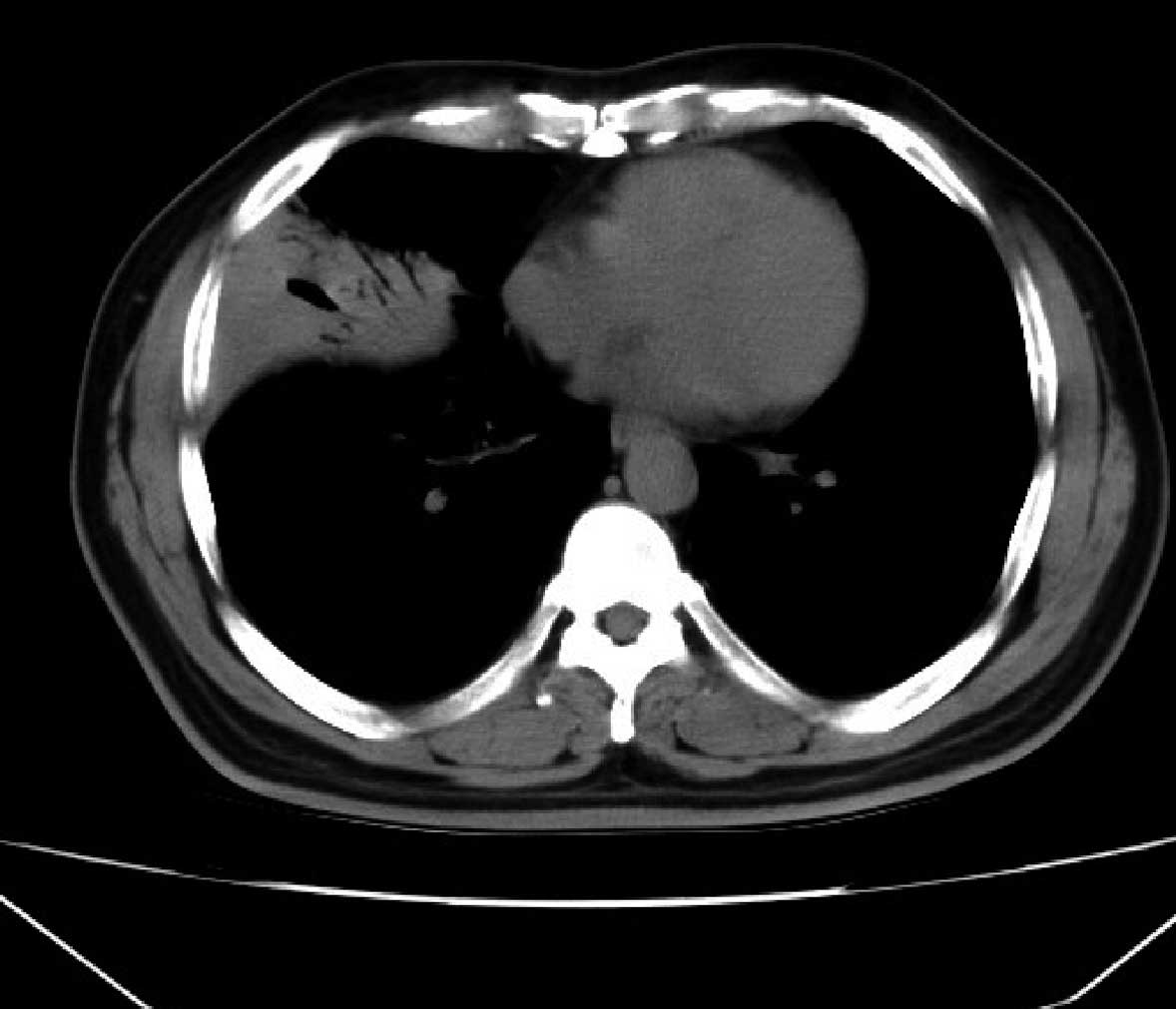
A chest radiograph revealed a nodule in the right upper lung
(Fig. 1). A chest computed tomography
(CT) scan revealed signs of inflammation accompanied by mediastinal
lymphadenopathy in the anterior segment of the right upper lobe
(Fig. 2). Additionally, flexible
bronchoscopy was performed to identify the endobronchial lesion. At
bronchoscopy, mucosal edema and slight stenosis were observed in
the right main bronchus (Fig. 3).
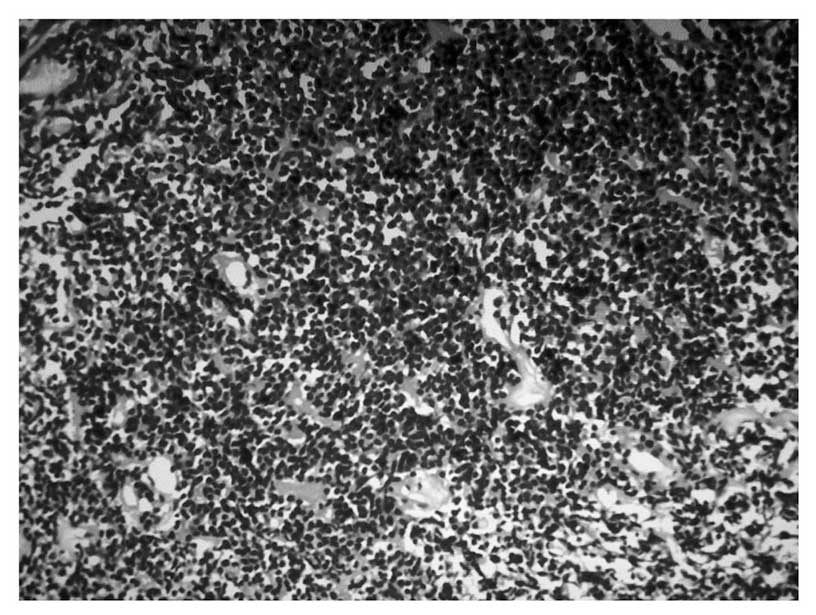
Immunohistochemical staining revealed diffuse strong positive
staining for cluster of differentiation (CD)20, B-cell lymphoma-2
and CD79a, and the samples were negative for CD3, CD5, cyclin D1
and κ-light chain expression (Fig.
4). Considering the clinical outcomes, the pulmonary lesion was
diagnosed as extranodal MALT-MZL. No evident absorption of the
lesion was identified on CT scan following combined treatment with
mezlocillin and sulbactam (3.75 g every 8 h) for 1 week.
Bronchoscopic examination and pathological analysis revealed no
evidence of bleeding or lumps, which confirmed the diagnosis of
extranodal MALT-MZL. Subsequently, the patient was transferred to
the Hematology Department, but refused further treatment. No
follow-up examinations were performed.
Discussion
In 1983, Isaacson and Wright (14) reported two cases of MALT lymphoma
arising from the gastrointestinal tract for the first time.
Subsequently, a variety of studies identified additional MALT
lymphoma cases worldwide (3,14,15). MALT
lymphoma has been classified in the WHO and revised
European-American classifications of lymphoid neoplasms as
extranodal MALT-MZL (1,4,7). This
extranodal lymphoma with low-grade features infiltrates the
marginal zone of reactive B-cell follicles and arises most commonly
from the MALT of the stomach, but also from the lungs, salivary
glands and thyroid gland (4).
Pulmonary extranodal MZL is a rare entity that
accounts for <0.5% of primary pulmonary malignancies and <1%
of all lymphomas (5–7). The incidence of lung adenocarcinoma,
which usually arises from peripheral small bronchi or alveolar
epithelial cells, is increasing worldwide. The etiology of
pulmonary extranodal MZL has yet to be elucidated (7), but chronic immune stimulation resulting
from infection or autoimmune disorder may be associated with the
pathogenesis of extranodal MZL. In addition, previous studies have
identified the strong association between Helicobacter
pylori infection and gastric extranodal MZL (2,4).
It has been indicated that approximately half of
patients are asymptomatic at presentation, with abnormal
radiological findings being identified by chest radiography. For
the initial staging and follow-up in patients with malignant
lymphoma, 18Fluoro-2-deoxyglucose-positron emission
tomography (18FDG-PET) has been widely used (16). Although a previous study (17) indicated that there is a limited role
for PET in extranodal MALT lymphoma patients due to the lack of FDG
avidity, a later study by Elstrom et al (16) indicated that the issue is
controversial, in particular, the accuracy of 18FDG
avidity in MZL. In the study by Elstrom et al, at least one
site of involvement was detected by PET-FDG in only 67% of MZL
patients (16). Increased FDG uptake
was detected in the majority of a small cohort of nodal MZL
patients, but not in patients with extranodal disease, suggesting
that the FDG-avidity depends on the tumor location or the MZL
subtype (18).
In addition, symptomatic patients present with
non-specific pulmonary symptoms, including cough, dyspnea, chest
pain and hemoptysis. The B symptoms are uncommon and are observed
in only a minor proportion of patients (4,7,19,20).
In the current study, the patient with pulmonary
extranodal MZL was asymptomatic and the pulmonary lesions were
incidentally found during physical examinations at a local
hospital. The major radiographic patterns of pulmonary extranodal
MZL have been reported as nodules, consolidation, ground-glass
opacity and centrilobular nodules with linear branching opacities,
also termed a tree-in-bud sign (4,7,15,20). In a
previous study on the CT findings of MZL, single or multiple
nodules or areas of consolidation were the main patterns, while
none exhibited involvement of the main bronchus (15). In a later study, only two of the 61
enrolled patients were found to possess masses of various sizes in
the main bronchus (19). Therefore,
the characteristics of the present patient are observed extremely
rarely in clinical settings as the patient presented with
endobronchial edema and inflammatory symptoms, without lung
parenchymal lesions being observed during bronchoscopy, which
highly enhanced the difficulty of diagnosis and delayed the
administration of the corresponding therapies.
Extranodal MZL can be clinically diagnosed by
bronchoscopic, transbronchial or percutaneous needle biopsies, with
a surgical lung biopsy being required in numerous cases (4,15,19). An infiltrate of small to medium-sized
lymphocytes with irregular nuclei and abundant cytoplasm is
characteristic of extranodal MZL, with reactive follicles also
usually observed. Lymphoepithelial lesions, in which tumor cells
infiltrate the bronchial, bronchiolar and alveolar epithelium, are
characteristic of MZL, but not pathognomonic (2,4,7). Immunophenotyping studies aid in the
confirmation of diagnosis, particularly when performed on small
biopsy specimens, and aid in the differentiation of extranodal MZL
from diffuse large B-cell, small lymphocytic, mantle cell and
follicular lymphomas (2,4,7,19). Pulmonary extranodal MZL is an indolent
disease and exhibits a favorable prognosis, with a five-year
survival rate of ~90% (4,7,20), but
extra-pulmonary lesions and lymph node involvement are poor
prognostic factors (20).
In the present study, since the male patient was
asymptomatic, which significantly increased the difficulty of the
clinical diagnosis, the male patient was required to undergo a
series of clinical examinations, comprising chest radiography,
chest CT, bronchoscopic examinations, immunohistochemical staining
and transbronchial lung biopsy. Combining these clinical results
and subsequent analysis outcomes, an accurate diagnosis of
pulmonary extranodal MALT-MZL was finally confirmed.
References
|
1
|
Harris NL, Jaffe ES, Stein H, et al: A
revised European-American classification of lymphoid neoplasms: a
proposal from the International Lymphoma Study Group. Blood.
84:1361–1392. 1994.PubMed/NCBI
|
|
2
|
Armitage JO and Weisenburger DD: New
approach to classifying non-Hodgkin's lymphomas: clinical features
of the major histologic subtypes. Non-Hodgkin's Lymphoma
Classification Project. J Clin Oncol. 16:2780–2795. 1998.PubMed/NCBI
|
|
3
|
Zucca E, Conconi A, Pedrinis E, et al:
Nongastric marginal zone B-cell lymphoma of mucosa-associated
lymphoid tissue. Blood. 101:2489–2495. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jaffe ES, Harris NL, Stein H and Vardiman
JW: World Health Organization Classification of TumoursPathology
and Genetics of Tumours of Haematopoietic and Lymphoid Tissues.
IARC Press; Lyon: pp. 171–181. 2001
|
|
5
|
Ahmed S, Siddiqui AK and Rai KR: Low-grade
B-cell bronchial associated lymphoid tissue (BALT) lymphoma. Cancer
Invest. 20:1059–1068. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Koss MN: Malignant and benign lymphoid
lesions of the lung. Ann Diagn Pathol. 8:167–187. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Travis WD, Brambilla E, Müller-Hermelink
HK and Harris CC: World Health Organization Classification of
TumoursPathology and Genetics of Tumours of the Lung, Pleura,
Thymus and Heart. 3rd. IARC Press; Lyon: pp. 95–98. 2004
|
|
8
|
Cordier JF, Chailleux E, Lauque D, et al:
Primary pulmonary lymphomas. A clinical study of 70 cases in
nonimmunocompromised patients. Chest. 103:201–208. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wislez M, Cadranel J, Antoine M, Milleron
B, Bazot M, Mayaud C and Carette MF: Lymphoma of pulmonary
mucosa-associated lymphoid tissue: CT scan findings and
pathological correlations. Eur Respir J. 14:423–429. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cadranel J, Wislez M and Antoine M:
Primary pulmonary lymphoma. Eur Respir J. 20:750–762. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang LB, Sun YE, Yu CH and Liu Y:
Clinical diagnosis and surgical treatment of primary pulmonary
lymphoma. Zhonghua Wai Ke Za Zhi. 44:97–99. 2006.(In Chinese).
PubMed/NCBI
|
|
12
|
Vanden Eynden F, Fadel E, de Perrot M, et
al: Role of surgery in the treatment of primary pulmonary B-cell
lymphoma. Ann Thorac Surg. 83:236–240. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li G, Hansmann ML, Zwingers T and Lennert
K: Primary lymphomas of the lung: morphological,
immunohistochemical and clinical features. Histopathology.
16:519–531. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Isaacson P and Wright DH: Malignant
lymphoma of mucosa-associated lymphoid tissue. A distinctive type
of B-cell lymphoma. Cancer. 52:1410–1416. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bae YA, Lee KS, Han J, et al: Marginal
zone B-cell lymphoma of bronchus-associated lymphoid tissue:
imaging findings in 21 patients. Chest. 133:433–440. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Elstrom R, Guan L, Baker G, et al: Utility
of FDG-PET scanning in lymphoma by WHO classification. Blood.
101:3875–3876. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Perry C, Herishanu Y, Metzer U, et al:
Diagnostic accuracy of PET/CT in patients with extranodal marginal
zone MALT lymphoma. Eur J Haematol. 79:205–209. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hoffmann M, Kletter K, Becherer A, et al:
18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET)
for staging and follow-up of marginal zone B-cell lymphoma.
Oncology. 64:336–340. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Oh SY, Kim WS, Kim JS, et al: Pulmonary
marginal zone B-cell lymphoma of MALT type-what is a prognostic
factor and which is the optimal treatment, operation, or
chemotherapy?: Consortium for Improving Survival of Lymphoma (CISL)
study. Ann Hematol. 89:563–568. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ahmed S, Kussick SJ, Siddiqui AK, et al:
Bronchial-associated lymphoid tissue lymphoma: a clinical study of
a rare disease. Eur J Cancer. 40:1320–1326. 2004. View Article : Google Scholar : PubMed/NCBI
|