Introduction
Primary cardiac tumors, which can occur at any age,
are extremely rare in children, with an incidence varying between
0.0017 and 0.28%, with >90% of these cases being benign
(1). Primary cardiac tumors in
children may arise in any region of the myocardium, endocardium or
pericardium (1). The most common
cardiac tumor is rhabdomyoma (67%), usually associated with
tuberous sclerosis, followed by fibroma (17%) and fibroelastoma
(8%). Clinical presentation is dependent on the age of the patient,
as well as the size and location of the cardiac tumor (2). Children with cardiac tumors can be
asymptomatic or may present with symptoms such as, murmur,
arrhythmia, heart failure, or sudden death (2–4). Biopsy is
the diagnostic gold standard (1).
Treatment modalities include conservative management, surgical
resection and transplantation, and treatment choice varies
according to the diagnosis and the patient's symptoms (2). Surgery is the main approach for patients
with symptomatic primary cardiac tumors (3,4). Due to
the rarity of theprimary cardiac tumors, literature regarding the
management and outcome remains limited (5). However, low coverage is a major problem
with the current social security and medical insurance in China. In
the present study, a retrospective analysis was performed on the
medical records of patients with a diagnosis of primary cardiac
tumor (with the exception of myxoma) who were treated between 2004
and 2013. A total of 11 patients were identified. This study
describes the experience of a single institute with regard to these
cases of primary cardiac tumors in infants and children.
Patients and methods
Clinical data
Between May 2004 and March 2013, 11 children (9
males and 2 females) diagnosed with primary cardiac tumors
underwent a tumor resection at the Second Xiangya Hospital of
Central South University (Changsha, Hunan, China). Patient age
ranged between 13 days and 4 years (mean, 23 months), with a mean
weight of 13±5.7 kg. The most common clinical symptom was a cardiac
murmur, followed by intolerance to feeding, palpitations and
dyspnea. Chest X-ray showed mild to moderate cardiac enlargement
(10 cases) and pulmonary oligemia (4 cases). Echocardiography
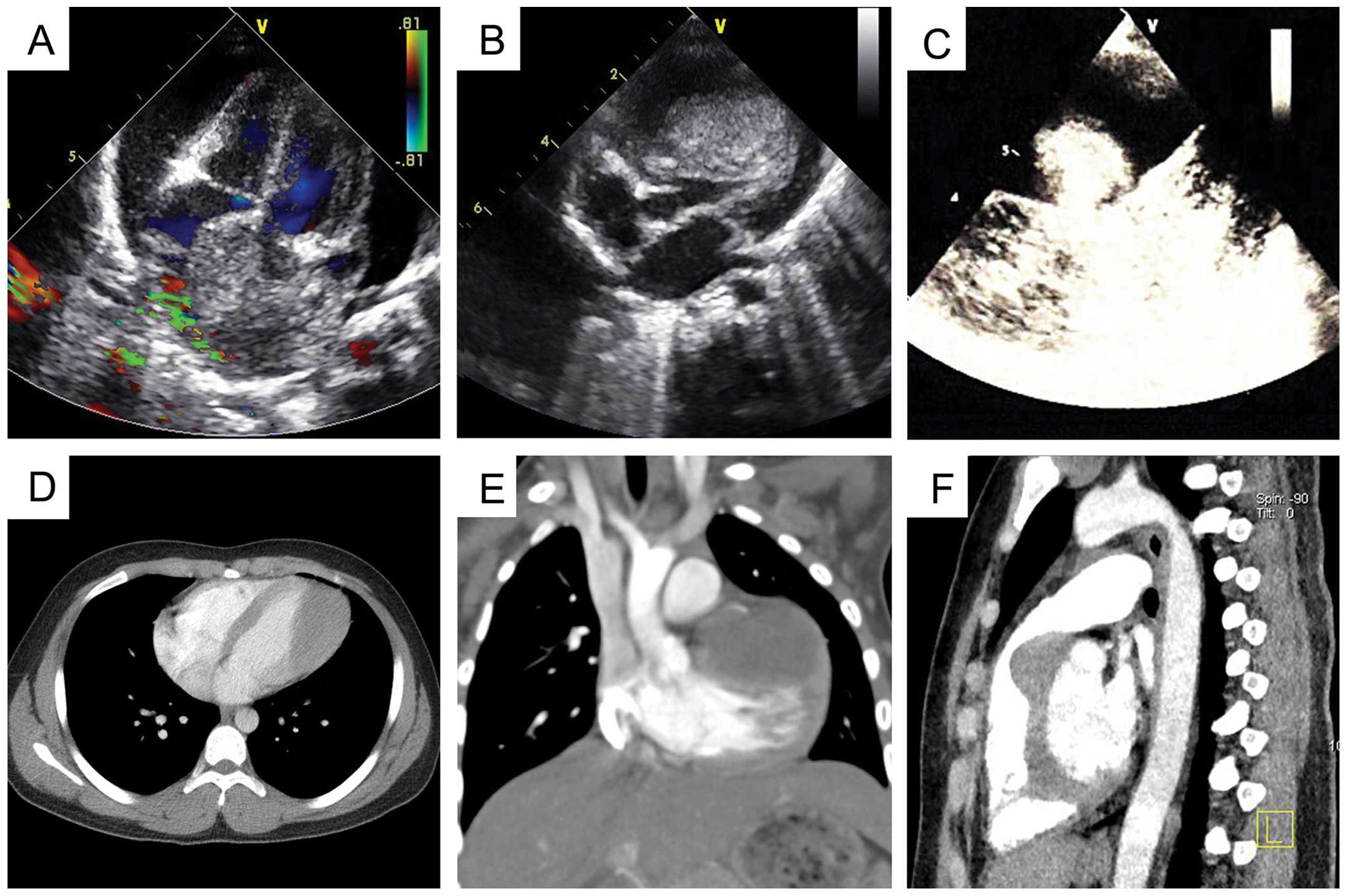
revealed masses inside two cardiac chambers (Fig. 1A), a mass inside the right ventricle
(Fig. 1B) and an intrapericardial
mass (Fig. 1C). Examination by
cardiac computed tomography also revealed cardiac masses (Fig. 1D-F). Written informed consent was
obtained from the patients' families prior to publication of the
data.
Surgical procedure
All surgeries in this study were performed via a
median sternotomy. Patients with intrapericardial masses underwent
excision off-pump, while the remaining patients were placed on
cardiopulmonary bypass (CPB). In 1 patient, a tumor was found
involving the aortic root, superior vena cava (SVC) and sinus node
after opening the pericardium, thus, a total tumor resection with
aortic root replacement, SVC patch repair and implantation of a
permanent cardiac pacemaker was indicated. However, following
communication with the patient's parents, the surgery was refused
and a partial tumor resection was requested due to insufficient
financial support. Thus, a partial resection and pathological
biopsy were performed. All other patients underwent a total tumor
resection successfully. The associated cardiac deformities were
also corrected at the same time. A patient with a ventricular
septal defect (VSD), in whom the diagnosis of a primary cardiac
tumor was missed pre-operatively, was treated, and a mass was found
behind the left ventricular free wall during surgery. VSD patch
repair and a total resection of the tumor were subsequently
performed.
Results
Rhabdomyoma (Fig. 2A),
fibroma (Fig. 2B), angiofibroma
(Fig. 2C) and fibrosarcoma (Fig. 2D) were histologically diagnosed in 5,
3, 2 and 1 patient, respectively. The tumor involving the aortic
root, SVC and sinus node was found to be an infiltrating
angiofibroma. The patients were discharged on post-operative days
7–10 without any complications, including pericardial effusion,
arrhythmia and pulmonary embolism. Echocardiography at 1 week
post-surgery showed normal blood flow velocities in the
atrioventricular and aortic valve orifices. At the 6-month
follow-up, the patient who underwent a partial resection of a
diffuse infiltrating angiofibroma was diagnosed with a residual
tumor, 32 mm in diameter, which infiltrated the aortic root and SVC
upon three-dimensional echocardiography. Further surgery was
refused and the patient succumbed to the disease 2 years after the
initial surgery. For the patient in whom cardiac tamponade was
initially identified, a pericardial fibrosarcoma was diagnosed
following a total resection performed as an emergency procedure.
Echocardiography shown tumor recurrence 1 year after the resection.
However, the patient's custodian refused a repeat surgical
procedure and the patient succumbed 1 year after the initial
surgery. The remaining 9 patients who underwent complete tumor
resections are alive and well at 2–9 years of follow-up, and show
no signs of tumor relapse.
Discussion
Primary cardiac tumors may be malignant or benign,
and may arise in any region of the myocardium, endocardium or
pericardium (1). The clinical
symptoms are based on the tumor location, number, size and shape,
as well as the nature of the tumor. The tumors vary from being
completely asymptomatic to presenting with arrhythmia, tumor
embolism, severe angina or sudden mortality (2–4). Timely
surgical removal of the tumor is necessary when the patient shows
associated symptoms. Myxoma, as with thrombosis, was excluded from
the present study owing to its higher incidence and its relatively
fixed surgical options.
Surgery is recommended for patients with symptomatic
primary cardiac tumors. Thus, once diagnosed, a total tumor
resection should be performed to avoid the increasing surgical risk
with tumor progression. Once the tumor has progressed to a
non-resectable life-threatening stage, one remaining treatment
option is a cardiac transplant (6).
Rhabdomyoma is the most common primary cardiac tumor in children.
Rhabdomyomas tend to regress spontaneously, and close observation
must be ensured in patients without symptoms (7). Surgery is required in cases with severe
symptoms, such as obstruction in the ventricular output tracts
(3). Cardiac fibromas are associated
with high mortality rates, and spontaneous regression rarely
occurs. Surgical resection is normally recommended in infants due
to the high risk of lethal arrhythmias, right ventricular outflow
tract obstruction or heart failure (4). Angiofibroma tends to involve the cardiac
valves, and these tumors should be removed in a timely manner
(8). A previous study with one of the
largest patient groups studied by autopsy recorded an incidence
rate of 0.0022% for primary pericardial tumors (9). Primary pericardial fibrosarcoma in
children is extremely rare, and surgery is required when the
diagnosis has been confirmed.
Primary cardiac tumors, with the exception of
certain regions of pericardial tumors, should be removed with the
affected patients on CPB. One surgical principle is that the
preservation of remaining heart function should be the first
priority, with total resection as the second. If a resection of the
tumor is not achievable in severely symptomatic patients, such as
those with a large tumors affecting the left side of the heart or
in the case of a malignant tumor, cardiac transplantation may be
considered. To date, there have been no evidence-based studies on
whether post-operative radiotherapy and/or chemotherapy is
necessary for the treatment of primary pericardial sarcomas
(10).
In the present study, all patients underwent
surgical removal of the tumor. Two patients succumbed during the
follow-up period. Not everyone in the Chinese population is covered
by health insurance schemes, particularly with regard to medical
insurance for serious illnesses, and with the tense doctor-patient
relationship in China, this results in surgeons having to undertake
more secure and economical procedures, rather than the most optimal
treatment. Healthcare must be pushed step by step, and it is also
important to improve the morale and working environment of health
professionals (11). The main goal
should be for every single Chinese patient to obtain the most
optimal treatment in the near future.
In conclusion, individualized treatment should be
introduced for children with primary cardiac tumors. Surgery is
required in symptomatic cases, and has good early and long-term
outcomes. For those Chinese parents who would prefer to procreate
again rather than pay for the treatment of such affected patients,
more education and comprehensive Social Security and Medicare may
require consideration.
Acknowledgements
The authors would like to thank the Committee of the
Provincial Science Study Foundation of Hunan (grant no. 2014SK2014)
for providing funding.
References
|
1
|
Paramés F, Freitas I, Martins JD, Trigo C
and Pinto MF: Cardiac tumors: The 17-year experience of pediatric
cardiology department. Rev Port Cardiol. 28:929–940. 2009.(In
Portuguese). PubMed/NCBI
|
|
2
|
Tao TY, Yahyavi-Firouz-Abadi N, Singh GK
and Bhalla S: Pediatric cardiac tumors: Clinical and imaging
features. Radiographics. 34:1031–1046. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gazit AZ, Singh GK, Shumway J, Johnson MC
and Ludomirsky A: Fetal cardiac rhabdomyoma: A sheep or a wolf? J
Matern Fetal Neonatal Med. 20:343–348. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bielefeld KJ and Moller JH: Cardiac tumors
in infants and children: Study of 120 operated patients. Pediatr
Cardiol. 34:125–128. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Habertheuer A, Laufer G, Wiedemann D,
Andreas M, Ehrlich M, Rath C and Kocher A: Primary cardiac tumors
on the verge of oblivion: A European experience over 15 years. J
Cardiothorac Surg. 10:562015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Elbardissi AW, Dearani JA, Daly RC,
Mullany CJ, Orszulak TA, Puga FJ and Schaff HV: Survival after
resection of primary cardiac tumors: A 48-year experience.
Circulation. 118 (Suppl 14):S7–S15. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bakaeen FG, Reardon MJ, Coselli JS, Miller
CC, Howell JF, Lawrie GM, Espada R, Ramchandani MK, Noon GP,
Weilbaecher DG and DeBakey ME: Surgical outcome in 85 patients with
primary cardiac tumors. Am J Surg. 186:641–647. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Issa OM, Reyna J, Santana O, DeBeer S,
LaPietra A and Lamelas J: Cardiac angiofibroma: A rare primary
cardiac tumor. J Card Surg. 28:404–405. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lagrotteria DD, Tsang B, Elavathil LJ and
Tomlinson CW: A case of primary malignant pericardial mesothelioma.
Can J Cardiol. 21:185–187. 2005.PubMed/NCBI
|
|
10
|
NeragiMiandoab S, Kim J and Vlahakes GJ:
Malignant tumours of the heart: A review of tumour type, diagnosis
and therapy. Clin Oncol (R Coll Radiol). 19:748–756. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang HH: China's new health department:
Progress and priorities. Lancet. 384:733–734. 2014. View Article : Google Scholar : PubMed/NCBI
|