Introduction
At present, the global incidence of colorectal
cancer is increasing, which is considered to be a result of
westernization of the diet and obesity (1–4). The main
symptoms are rectal bleeding with or without progressive anemia and
weight loss. The recommended treatment for stage I colorectal
cancer is surgical resection combined with lymph node dissection
(5). The 5-year survival rate of
patients following resection of stage I colorectal cancer is
90–95%, with postoperative distant metastasis/recurrence occuring
in 5–10% of patients (5). The
incidence of postoperative local recurrence in the pelvic cavity is
low (5–7). However, it is not uncommon for colon
cancer to cause an abscess in a distant organ (8–16).
Regarding the pathogenesis of systemic abscesses associated with
colorectal cancer, small abscesses may form around the tumor or
bacterial invasion may occur secondary to damage to the intestinal
wall, which is followed by hematogenous spread (13). The development of abscesses may be
promoted by the impaired immunity of tumor-bearing patients and
associated diseases, such as diabetes, may also affect immunity
(12,13). In the literature, five cases of
colorectal cancer in which liver abscesses were the chief complaint
have been reported. Of these five cases, 1 early cancer patient
(8) and 3 advanced cancer patients
exhibited liver abscesses alone (9,10,13) and 1 advanced cancer patient exhibited
multiple systemic abscesses (12).
Fever was the main symptom in all cases, with weight loss, malaise
and nausea/vomiting also observed (8–10,12,13). In
addition, the case of an advanced colorectal cancer patient
exhibiting multiple systemic abscesses without any liver abscesses
has also been reported (16).
However, to the best of our knowledge there have been no reports of
multiple systemic abscesses associated with early rectal cancer.
The present case study describes the management of a patient with
multiple systemic abscesses due to early rectal cancer.
Case report
The study was approved by the ethics committee of
Tokai University Hachioji Hospital (Tokyo, Japan) and all patients
provided written, informed consent in accordance with the
institutional review board of Tokai University Hachioji Hospital.
The patient was a 70-year-old man who presented with cough, fever
and numbness of the upper extremities. The patient was diabetic,
however that was controlled. In early February 2008, the patient
developed a cough and pyrexia. The patient was admitted to Uenohara
Municipal Hospital (Yamanasi, Japan) where the patient had been
treated for diabetes, but his symptoms did not improve.
Computerized tomography (CT) scanning was performed in late
February 2008, revealing an abscess in the liver and multiple
nodules in the lungs, which were also considered likely to be
abscesses. The patient then developed numbness of the upper
extremities and neck pain, and was subsequently transferred to
Tokai University Hachioji Hospital (Tokyo, Japan). Physical
examination indicated that the patient was 161 cm tall and weighed
64 kg; blood pressure was 136/80 mmHg; pulse rate was 92/min
(regular); and body temperature was 38.5°C. The patient did not
have conjunctival pallor or jaundice, and the abdomen was soft and
flat. Laboratory blood tests demonstrated a slight increase in the
white blood cell count to 9,500/µl and a high C-reactive protein
level of 20.6 mg/dl. In addition, the patient demonstrated elevated
levels of aspartate aminotransferase (GOT/AST), alanine
aminotransferase (GPT/ALT), alkaline phosphatase (ALP) and
γ-glutamyl transpeptidase (γ-GTP) to 69, 53, 650 and 129 IU/l,
respectively. The blood glucose level was high at 210 mg/dl,
however the glycated hemoglobin (HbA1c) levels were only slightly
elevated to 6.4%, indicating that until recently the patient's
diabetes was well controlled. CT scans demonstrated multiple
nodular lesions in the lungs, which were considered to be multiple
lung abscesses. In addition, there was a multilocular cystic lesion
in segments 4, 7 and 8 of the liver, which was considered to be a
liver abscess (Fig. 1). Abdominal
ultrasonography also demonstrated a multilocular cystic lesion in
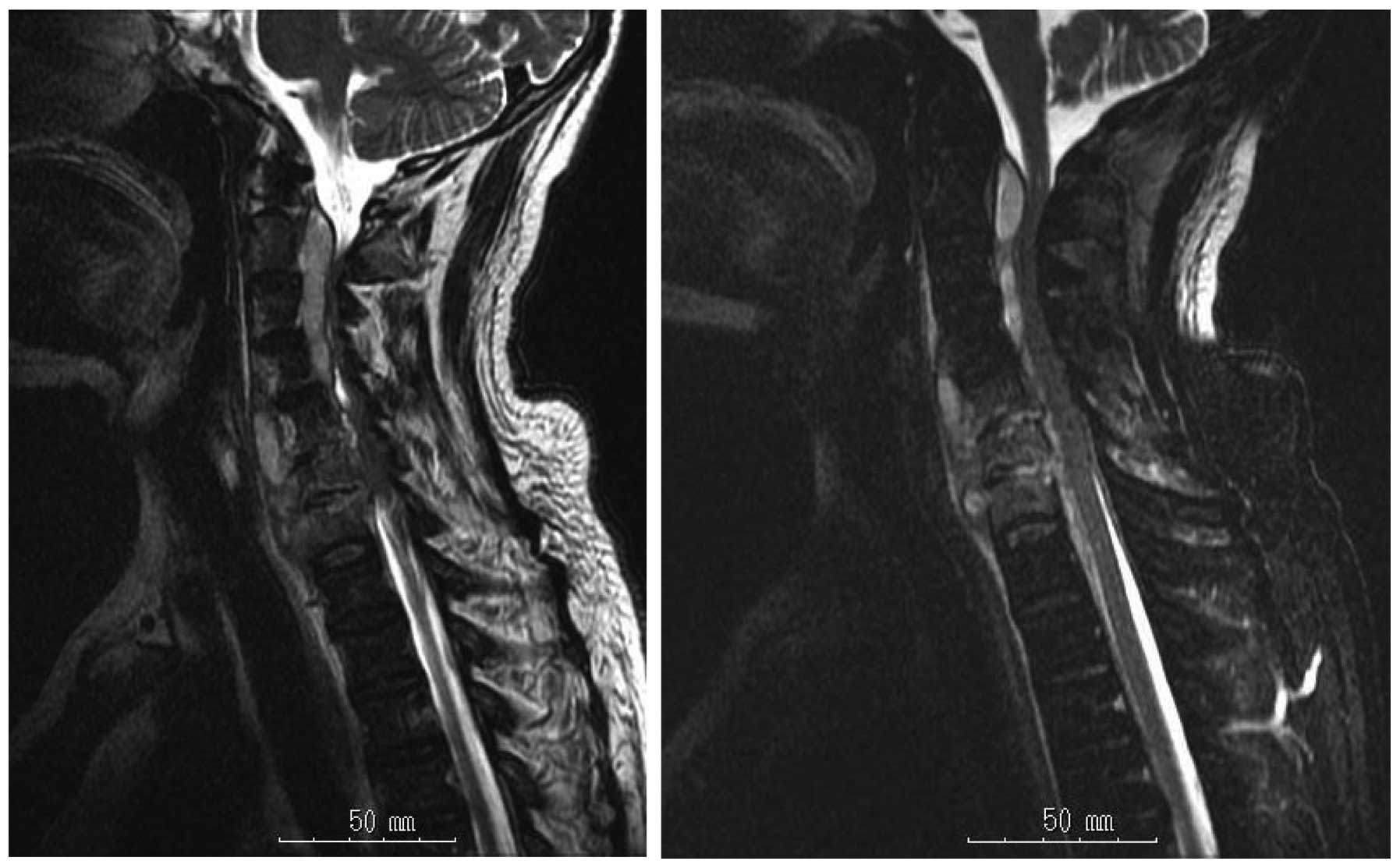
segments 4, 7 and 8 of the liver. Magnetic resonance imaging of the
cervical region revealed an epidural abscess that extended from C2
to C7, originating from a site of vertebral destruction due to
spondylitis at C5/6. Accordingly, osteomyelitis of the upper
cervical spine was diagnosed (Fig. 2)
combined with liver abscess and multiple lung abscesses.
Percutaneous transhepatic drainage (PTD) of the liver abscess was
immediately performed and ≥100 ml of yellowish-white pus was
removed. There was no connection between the abscess and the
intrahepatic bile ducts. Systemic administration of antibiotics was
initiated (17,18). Since the patient also experienced
numbness of the upper extremities, drainage of the neck abscess,
iliac bone grafting and anterior cervical spinal fusion were
promptly performed. Following these procedures, a thorough
examination of the gastrointestinal tract was performed, while
continuing antibiotic treatment and rehabilitation. A barium enema
revealed a protruding lesion with an irregular border in the rectum
(Ra; above the peritoneal reflection) (Fig. 3). Colonoscopy detected a protruding
lesion with an irregular border on a rectal fold. Biopsy of the
lesion demonstrated that it was a moderately differentiated
adenocarcinoma (Fig. 4). The nodular
lesions in the lungs of the patient were no longer detected when CT
scanning was performed again once the inflammation had subsided,
which indicates that these were multiple lung abscesses.
Consequently, the final diagnosis was early rectal cancer that
presented with multiple systemic abscesses. Radical resection of
the rectal lesion was performed ~1 month following the initiation
of treatment for the abscesses.
Midline laparotomy was performed in the lower
abdomen and the peritoneal cavity was investigated but there was no
peritoneal dissemination or liver metastasis. The rectal cancer was
removed by lower anterior resection. Multiple blocks were taken and
routinely processed in paraffin. The sections were stained with
hematoxylin and eosin. The pathological diagnosis was made using
microscopic examination using a BX51 light microscope with a
U-TV0.5XC-3 adaptor, and images were captured using a DP-21 camera
(Olympus Corporation, Tokyo, Japan). Examination of the resected
specimen indicated an Isp type (subpedunculated) tumor with a
diameter of 2×1 cm in the rectum (Ra; above the peritoneal
reflection) (Fig. 5A). The
histopathological diagnosis was a moderately differentiated
adenocarcinoma, which was Ra, pT1b (early cancer with the deepest
level of invasion being 1,500 µm), ly0, v0, N0 and M0, and the
tumor was classified as stage l (Fig. 5B
and C), as in accordance with the General Rules for Clinical
and Pathological Studies on Cancer of the Colon, Rectum and Anus
(19). The patient's postoperative
course was uneventful and there has been no evidence of metastasis
or recurrence in the 7 years following the surgery.
Discussion
It is uncommon for colorectal cancer to present with
liver abscess and this is reported to occur in ≤5% of patients
(20,21). The incidence of abscess formation due
to colorectal cancer is highest in the liver, followed by the
lungs, and cases of endocarditis and meningitis have also been
reported (8–16). However, to the best of our knowledge
there has only been 1 reported case of early colorectal cancer
associated with a liver abscess (1),
in addition to 2 cases of multiple abscesses due to colorectal
cancer (12,16); therefore, the patient in the present
case report is the first to be reported with multiple abscesses
caused by early rectal cancer. The majority of the bacteria
isolated from abscesses associated with colorectal cancer are gram
negative rods such as Klebsiella (50.0%) or
Fusobacterium (6.90%) species (14,15).
Klebsiella with the same antibiotic sensitivity profile was
isolated from the liver and neck abscesses from the patient in the
current study. The potential mechanisms of abscess formation
include bacteremia as a result of a hematogenous spread from the
tumor, direct extension of the intraperitoneal infection along the
portal vein or a secondary infection of metastases. Since the
patient in the present report was elderly and diabetic, impairment
of the immune system may have been associated with the formation of
multiple abscesses in addition to the colon cancer (13,22,23).
Lonardo et al (13) considered
that micro-abscesses may occasionally develop surrounding colon
cancer, and lead to bacterial infection in multiple organs by
spreading the infection through the portal vein if the defense
mechanism of the intestinal tract wall against infection is
disrupted. However, the patient in the present study received
antibiotic treatment for the liver and cervical abscesses and no
micro-abscesses or extensive necrosis were observed in the resected
specimen. Nevertheless, the tumor depth had invaded into the
submucosal layer (1,500 µm), so the possibility of bacterial
infection may not be ruled out. Initially, the liver and cervical
abscesses were observed in the patient, while the multiple lung
nodules disappeared during antibiotic therapy, indicating that
these nodules were lung abscesses. It is important to note that
multiple abscess formation can be one manifestation of colorectal
cancer. Cohen et al (24) and
Huang et al (15) reported
that it is necessary to investigate the gastrointestinal tract in
patients who develop an abscess of unknown etiology.
For management of colorectal cancer associated with
an abscess, it is common to initially treat the abscess
conservatively with antibiotics and drainage and then perform
definitive surgery for the cancer once the abscess has resolved.
Since the patient in the present study was experiencing numbness of
the upper extremities when transferred to Tokai University Hachioji
Hospital, drainage of the cervical spine abscess and iliac bone
grafting was performed and immediately followed by anterior
cervical spinal fusion. Subsequent to these procedures, systemic
antibiotic treatment and rehabilitation was promptly initiated. In
considering antibiotic therapy for the patient, the de-escalation
method was decided upon as the most effective, and thus, antibiotic
agents with a wider antibacterial spectrum were administered
initially and then substituted to other agents with a narrower
spectrum. Although the optimum timing for radical resection of
rectal cancer in these patients has not yet been defined clearly,
surgery was performed 4 weeks following transfer of the patient to
Tokai University Hachioji Hospital since the patient's general
condition had improved. As the patient's postoperative course was
uneventful, the timing of the surgery was considered to be
appropriate. It is occasionally difficult to differentiate between
abscesses and metastasis, but in the present case the multiple lung
nodules disappeared following antibiotic treatment, indicating that
these lesions were abscesses. However, patients who developed
metastases to the lung or liver following surgery have been
reported (12), so care should be
taken when making a diagnosis. Considering the possibility that an
abscess may be caused by secondary infection of a metastasis, it is
important to pay close attention to patients who may have
metastatic cancer.
In conclusion, the present case emphasizes that it
is necessary to perform thorough investigation for possible
colorectal cancer (including early cancer) when treating a patient
who has multiple abscesses involving organs such as the liver. It
is also important to follow the patient carefully following surgery
due to the risk of metastasis.
Abbreviations:
|
PTD
|
percutaneous transhepatic drainage
|
|
Ra
|
above peritoneal reflection
|
References
|
1
|
Larsson SC and Wolk A: Obesity and colon
and rectal cancer risk: A meta-analysis of prospective studies. Am
J Clin Nutr. 86:556–565. 2007.PubMed/NCBI
|
|
2
|
Moghaddam AA, Woodward M and Huxley R:
Obesity and risk of colorectal cancer: aAmeta-analysis of 31
studies with 70,000 events. Cancer Epidemiol Biomarkers Prev.
16:2533–2547. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
No authors listed: Obesity: Preventing and
managing the global epidemic. Report of a WHO consultation. World
Health Organ Tech Rep Ser. 894:1–253. 2000.
|
|
4
|
Endo H, Higurashi T, Takahashi H and
Nakajima A: Obesity, life style-related diseases and colorectal
cancer. Gastro Endosc. 55:3735–3744. 2013.(In Japanese).
|
|
5
|
Watanabe T, Itabashi M, Shimada Y, et al:
Japanese Society for Cancer of the Colon and Rectum: Japanese
Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014
for treatment of colorectal cancer. Int J Clin Oncol. 20:207–239.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Journal of Health and Welfare Statistics.
Health and Welfare Statistics Association; Tokyo: 61. pp. 63–67.
2014/2015
|
|
7
|
Multi-Institutional Registry of Large
Bowel Cancer in JapanCases treated in 1994. Japanese Society for
Cancer of the Colon and Rectum; Tokyo: 23. 2002
|
|
8
|
Tanizaki H, Kawano N, Watanabe H, Tsutsumi
O, Hatate K and Sugai T: A case of a solitary liver abscess
complicated by early sigmoid colon cancer. J Jpn Surg Assoc.
63:449–453. 2002.(In Japanese). View Article : Google Scholar
|
|
9
|
Ritchie JD: Portal pyaemia secondary to
carcinoma of the rectum. Aust NZJ Surg. 45:284–285. 1975.
View Article : Google Scholar
|
|
10
|
Panwalker AP: Unusual infections
associated with colorectal cancer. Rev Infect Dis. 10:347–364.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Legier JF: Streptococcus salivarius
meningitis and colonic carcinoma. South Med J. 84:1058–1059. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hiratsuka H, Yasui N and Maeda K: A case
of cancer of the rectum accompanied with multiple systemic
abscesses. JJSC. 65:453–457. 2012.(In Japanese).
|
|
13
|
Lonardo A, Grisendi A, Pulvirenti M, et
al: Right colon adenocarcinoma presenting as Bacteroides fragilis
liver abscesses. J Clin Gastroenterol. 14:335–338. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Qu K, Liu C, Wang ZX, Tian F, et al:
Pyogenic liver abscesses associated with nonmetastatic colorectal
cancers: an increasing problem in Eastern Asia. World J
Gastroenterol. 18:2948–2955. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang WK, Chang JW, See LC, et al: Higher
rate of colorectal cancer among patients with pyogenic liver
abscess with Klebsiella pneumoniae than those without: an 11-year
follow-up study. Colorectal Dis. 14:e794–e801. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Isohata N, Watanabe O, Domoto K, et al: A
case of rectal cancer developed bacterial meningitis. JJCS.
32:783–786. 2007.(In Japanese). View Article : Google Scholar
|
|
17
|
Andersson R, Forsberg L, Hederstrom E,
Hochbergs P and Bengmark S: Percutaneous management of pyogenic
hepatic abscesses. HPB Surg. 2:185–188. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nosher JL, Giudici M, Needell GS and
Brolin RE: Elective one-stage abdominal operations after
percutaneous catheter drainage of pyogenic liver abscess. Am Surg.
59:658–663. 1993.PubMed/NCBI
|
|
19
|
Japanese Society for Cancer of the Colon
and Rectum (JSCCR): General Rules for Clinical and Pathological
Studies on Cancer of the ColonRectum and Anus. 7th. revised
version. Kanehara Shuppan; Tokyo, Japan: 2009
|
|
20
|
McDonald AP and Howard RJ: Pyogenic liver
abscess. World J Surg. 4:369–380. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
McDonald MI, Corey GR, Gallis HA and
Durack DT: Single and multiple pyogenic liver abscesses. Natural
history, diagnosis and treatment, with emphasis on percutaneous
drainage. Medicine (Baltimore). 63:291–302. 1984.PubMed/NCBI
|
|
22
|
Teitz S, GuidettiSharon A, Manor H and
Halevy A: Pyogenic liver abscess: warning indicator of silent
colonic cancer. Report of a case and review of the literature. Dis
Colon Rectum. 38:1220–1223. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nosher JL, Giudici M, Needell GS and
Brolin RE: Elective one-stage abdominal operations after
percutaneous catheter drainage of pyogenic liver abscess. Am Surg.
59:658–663. 1993.PubMed/NCBI
|
|
24
|
Cohen JL, Martin M, Rossi RL and Schoetz
DJ: Liver abscess. The need for complete gastrointestinal
evaluation. Arch Surg. 124:561–564. 1989. View Article : Google Scholar : PubMed/NCBI
|