Introduction
Exposure to ultraviolet radiation (UV) from the sun
has negative effects on human health due to its carcinogenic
effects on the skin (1). However, low
skin exposure to UVB radiation (wavelength, 290–320 nm) from the
sun due to environmental factors or the specific behavior an
individual may also have negative outcomes (1). Vitamin D synthesis predominantly depends
on the level of UVB sun radiation that the skin receives, with a
lack of vitamin D in the body resulting in negative effects on
overall health, muscle function and bone strength (2). In addition, vitamin D is associated with
preventing type 1 diabetes and heart-associated diseases (2). Therefore, it is important to quantify
the required time to synthesize adequate vitamin D levels from UVB
radiation penetrating the skin (2,3).
It is possible to determine the time required to
synthesize adequate vitamin D levels in an organism depending on
skin type by using experimental solar UV index (UVI) measurements
(3). Sufficient levels of vitamin D
are associated with multiple benefits in humans, including
providing protection against different types of cancer, including
colon (4), prostatic (5) and stomach cancer. Evidence of these
associations has been provided by epidemiological studies performed
in Northern hemisphere populations (6,7). In
addition, it has been identified that vitamin D has a positive
effect on controlling high blood pressure (8); in humans, blood pressure decreases when
vitamin D levels are at a suitable level. Furthermore, an adequate
level of vitamin D is a reduction factor for autoimmune diseases,
including multiple sclerosis, type 1 diabetes, rheumatoid
arthritis, autoimmune disease of the thyroid and inflammatory bowel
disease (9).
Humans depend on vitamin D synthesized from sunlight
radiation to maintain calcified skeletons; however, a small
quantity of vitamin D remains in the skin (10–13). This
vitamin D is activated by interaction with the vitamin D receptor
to control cell proliferation using a variety of strategies, such
as interacting with long non-coding RNAs to reduce the risk of
photocarcinogenesis (11,12). In addition, vitamin D has a clearly
defined role in phosphorus, calcium and bone metabolism (13–16). UV
radiation has been demonstrated to be carcinogenic and responsible
for the onset of the majority of types of skin cancer (13–15).
Therefore, the population should be warned about misleading
advertising from the tanning industry. The aim of the present study
was to determine the required time to induce solar erythema
(TEry) for skin type IV and the required time to produce
1,000 international units (IU) of vitamin D (TVitD).
Materials and methods
Location of the study
Arica is a city located in a subtropical area in the
northernmost region of Chile. Arica has a microclimate with fairly
stable meteorological conditions throughout the year, including a
lack of rainfall (<5 mm a decade), predictable winds and a high
percentage of sunny days per year (15,16). In
addition, Arica is a desert area with vast sand and sea surfaces as
well as scarce vegetation; therefore, Arica has high ground
reflectivity (14,15). The city is located at sea level and
due to the good climate conditions, the population perform numerous
outdoor recreational activities. (16,17).
Measuring UVB sunlight radiation
A UVB sun device, which has been in used at the UV
Sunlight Radiation Laboratory of Tarapacá University (Arica, Chile)
since September 2006, was used in the present study. It is located
25 m above sea level, at a latitude of 18° 49′S and longitude of
70° 19′W on the uppermost part of the building with no elements
blocking incoming sunlight radiation. Erythemal UV irradiance
(UVEry) was measured using a calibrated high-range
YES-UVB-1 biometer (serial no. 090710, Yankee Environmental
Systems, Inc., Turners Falls, MA, USA) through an agreement between
Tarapacá University and the Chilean Meteorological Department (CMD,
Santiago, Chile). Measurements obtained from the device were
incorporated in real-time using a UVB device network installed by
the CMD. Thus, the device was connected to the UVB sun-measuring
network of Chile, covering an area between Arica and the Antarctic
territory in the South of Chile. All devices used in the present
study complied with the World Meteorological Organization
calibration specifications (18).
Calculation of UV index and related
calculations
The solar UVI (W/m2) was calculated from
the collected UVEry biometer data by multiplying
UVEry by 40 (11).
Subsequently, the TEry [1 minimal erythemal dose (MED)]
was calculated using the following equation: TEry =
(4,000/60) × [(MED × sun protection factor)/UVI)], where MEDF
depends on the Fitzpatrick classification of skin types (19,20). In
the present study, the cohort included individuals with MED skin
type IV (0.40–0.60 kJ/m2/day). The cohort used in this
study has been further described previously (15).
UVEry is expressed as the standard
erythemal dose (SED) required to induce erythema, where 1 SED=100
Jm−2 UVEry. From the UVEry
biometer measurement, vitamin D UV irradiation (UVVitD)
was estimated using a tropospheric UV model (21). Ozone layer data were obtained from
NASA/TOMS measurements by using the User's Guide from National
Aeronautics and Space Administration (NASA) (22). The subsequent calculation for TVitD
was obtained from Mckenzie et al (3). The most common skin types in chilean
teenagers of low social economical strata that have been analyzed
in previous studies (14–16) were used in the present study. In this
study, the cohort included 98 patients treated at the Pathology
Department of Dr Juan Noé Crevani Hospital (Arica, Chile) between
January 1989 and December 1993 (14).
Furthermore, when ozone layer and solar zenith angle (SZA) data
were known, the TVitD was calculated using the following
formula: TVitD= 20/(UVI × R), where R is a quotient of
UVVitD/UVEry. The ratio function of
UVVitD and UVEry was adjusted using the
following equation: UVVitD/UVEry =
(2.00524–1.48303) × exp (−UVI/2.73854). In addition, the skin
cancer rates (SCR) per 100,000 individuals between 2001 and 2011
(14,23) were adjusted using the following linear
fit equation: SCR = (−918.24 + 1.46) × number of years.
The study was approved by the ethics committee of
Servicio de Dermatología, Dr Juan Noé Crevani Hospital (Arica,
Chile). The data analyzed in the study were obtained from public
databases of Servicio de Dermatología, Dr Juan Noé Crevani
Hospital.
Results
UV light and UV quotient
The present study investigated the association
between the risk of skin cancer and mild exposure to UV light in
Arica, Chile. The TEry and TVitD were
calculated to explain the possible effects of insufficient vitamin
D in individuals living at a latitude of 18° 18′S, a longitude of
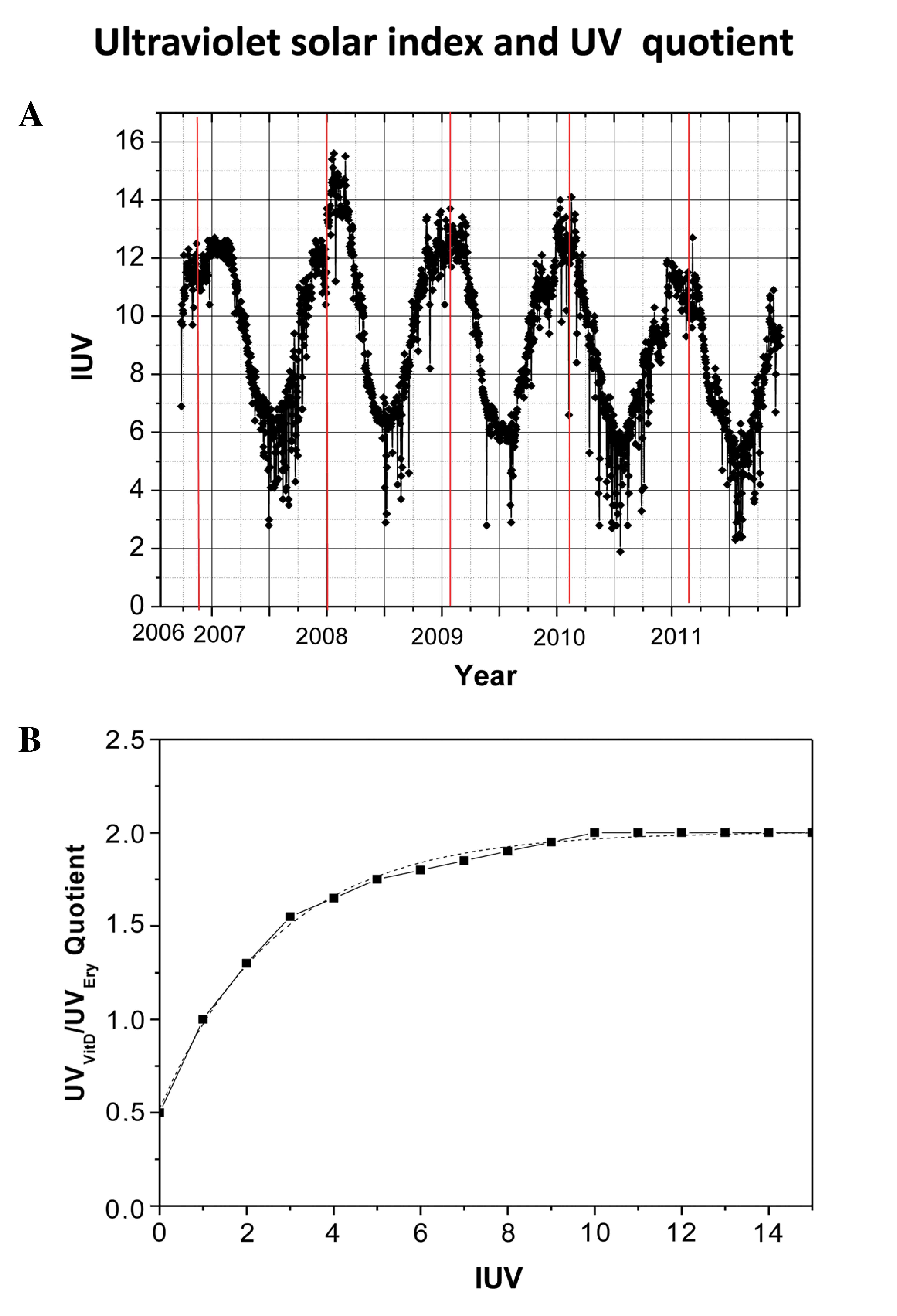
70°, 26′W and a height of 23 m. Fig.
1A displays the highest daily levels of solar UVI versus Julian
day (in one year Julian days take the values 1–365), the second
scale indicate the years. Solar UVI values were obtained in Arica
between September 20, 2006 and November 24, 2011, with the solar
UVI fluctuating between 2 and 15.5 W/m2. Fig. 1B indicates the quotients of
UVVitD/UVEry as a function of UVI and
demonstrates that the quotient varied between 0.5 and 2.0 for UVI
values between 0 and 15 W/m2.
Exposure time of UV radiation and
vitamin D synthesis
Fig. 2A reveals the
results obtained from calculating the TEry in the four
different seasons of the year between 2007 and 2013. It was
observed that the TEry varied between 12 min in the
summer and 34 min in the winter for skin type IV. Fig. 2B displays the mean value
TVitD per person during the four seasons of the year
when only hands and face were directly exposed to UV sunlight (10%
of the surface area of the body). These calculations were obtained
between 2007 and 2013, and varied from 8 min in the summer to 24
min in the winter.
Vitamin D and skin cancer rate
Fig. 3A indicates the
average monthly TVitD required for individuals that only
exposed their hands and face to direct sunlight. These calculations
were made at midday each month between 2006 and 2009. It was
observed that the exposure times varied between 8 min in summer
(January-February) and 24 min in winter (June-July). In addition,
the calculated TVitD data was similar each year.
Fig. 3B shows the SCR per 100,000
individuals between 2001 and 2006 (23), and 2007 and 2011 (14). A steady increase was observed,
increasing from 6.9 in 2001 to 23.8 in 2011, with the highest rate
reaching 30.8 in 2009.
UV index and solar zenith angle
The quotient of UVVitD/UVEry
as a function of the SZA is displayed in Fig. 4A. This calculation was performed using
UVI data obtained in 2007, which behaved similarly to previous
years, using an ozone layer thickness of 250 Dobson units (DU). The
highest value for this quotient (2.06–2.07) was obtained at a SZA
of <10°, whereas the lowest value for this quotient (1.83) was
obtained at a SZA of >50°. The quotient of
UVVitD/UVEry as a function of UVI data from
2007, with an ozone layer thickness of 250 DU is indicated in
Fig. 4B. The highest value for this
quotient (2.06–2.07) had a UVI value of >10 W/m2 and
the lowest value for this quotient (1.83) had a UVI of 5
W/m2. Fig. 4C demonstrates
solar UVI as a function of SZA between January and July 2007. The
highest UVI value was 12.7 W/m2 for a SZA that
fluctuated between 5 and 20°, with a maximum and minimum value of 5
and 40°, respectively. Table I
presents the skin cancer rate and time to synthesize 1000 UI of
vitamin D (TVID) during the four seasons of the year between 2007
and 2011 in Arica, Chile. The mean SCR between 2007 and 2011 was
calculated as 26.9 per 100,000 individuals.
 | Table I.Skin cancer rate and
TVitDduring the four seasons of the year between 2007
and 2011 in Arica, Chile. |
Table I.
Skin cancer rate and
TVitDduring the four seasons of the year between 2007
and 2011 in Arica, Chile.
|
|
| TVitD,
min |
|---|
|
|
|
|
|---|
| Year | Skin cancer
rate/100,000 individuals | Winter | Fall | Spring | Summer |
|---|
| 2007 | 30.2 | 19.1 | 11.0 | 10.1 | 8.5 |
| 2008 | 25.4 | 18.5 | 9.9 | 9.3 | 8.1 |
| 2009 | 30.8 | 19.9 | 10.2 | 10.3 | 8.6 |
| 2010 | 24.3 | 22.5 | 11.9 | 11.5 | 9.1 |
| 2011 | 23.8 | 23.8 | 12.6 | 12.7 | 9.9 |
Discussion
Arica is located in the northern region of Chile,
close to the equator, and is surrounded by desert and ocean
(14). Therefore, the quotient
calculated from the level of reflective solar UV radiation and the
incidence of solar UV radiation is generally high (14). Furthermore, the ground surfaces are
poorly vegetated, dusty and covered by extended areas of water
surface that induce high reflectivity, resulting in high diffuse
radiation (14). In addition to
receiving high doses of UV solar radiation, the stratospheric ozone
layer in this location is lower in comparison with other cities in
Chile below the equator, as Arica has a minimum ozone value of 230
DU in the summer and the maximum of 290 DU in September (14). The observed destruction of the ozone
layer has intensified research regarding the levels of solar UV
irradiance received on the surface of the earth (24). These factors allow incremental
increases in solar UV radiation to be measured at different
latitudes, which enables the evaluation of potential health
consequences for individuals in the population. In addition, these
factors have been accompanied by public campaigns to alert the
population of the dangers of overexposure to UV (14). However, this issue has sensitized a
large number of people to take extreme measures, such as completely
avoiding exposure to the sun. Numerous studies have demonstrated
the association between poor sun exposure and vitamin D synthesis
(9–12). Such insufficiency is associated with
various diseases, including melanoma skin cancer, type 1 diabetes,
multiple sclerosis, rheumatoid arthritis and inflammatory bowel
disease (25).
Incidence rates of skin cancer have significantly
increased at equatorial latitudes between 2001 and 2011
(6.9–23.8%), according to statistics obtained from Arica (24,26). This
significant increase is becoming a health issue for those living in
this area. A possible reason for this increase in the rate of skin
cancer may be due to inadequate levels of vitamin D in the blood
plasma. Vitamin D has immune stimulatory and immunosuppressive
effects relevant to human and mycobacterium responses (2). It has been reported that low vitamin D
levels induce immunomodulation and may affect the association
between vitamin D and tuberculosis (25). The results of the present study
demonstrated that at midday, TVitD varies between 8 and
24 min according to the season. Taking these factors into account,
the aforementioned exposure times are considered to be ideal
condition. However, if exposure occurs at a time other than midday
or on a cloudy day, the exposure time should be increased.
Therefore, despite high UV levels in this region, a certain
proportion of the population appear to be receiving insufficient
sunlight exposure to synthesize appropriate vitamin D levels.
Furthermore, in high UV sun radiation regions, individuals may work
under artificial light or with little exposure to UV radiation.
Therefore, the aim of the present study was to compare
TEry and TVitD. It was proposed that these
calculations should be determined in different latitudes and UV
exposure regions, where the time to vitamin D absorption and
synthesis are higher. In addition, special care is recommended
regarding the potential harm of inappropriate vitamin D
supplementation, as excess vitamin D is associated with immune
stimulatory and immune suppressive effects relevant to human
antimicrobial responses. Furthermore, vitamin D trials in patients
with active tuberculosis should be performed in well-selected
populations using adequate vitamin D doses (10). Our previous study reported that skin
cancer risk is influenced by UV irradiation in different latitudes
(18–20). To the best of our knowledge, there are
no previous studies linking vitamin D synthesis and exposure to UV
solar radiation in this latitude. The present study indicated that
despite being in an area of high exposure to UV solar radiation,
increased rates of skin cancer may also be due to vitamin D
deficiency in high risk groups such as post-menopausal women.
Acknowledgements
The present study was supported by grants from the
University of Tarapacá, Arica, Chile (grant no. UTA-4720, 2015, to
Professors Miguel Rivas and Elisa Rojas) and FONDECYT (grant no.
1120006; Dr Gloria M. Calaf). The authors would like to thank Mr.
Leodan A. Crispin and Mr. Richard Ponce-Cusi for their assistance
in the present study.
References
|
1
|
Elwood JM and Jopson J: Melanoma and sun
exposure: An overview of published studies. Int J Cancer.
73:198–203. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Holick MF: Vitamin D: Importance in the
prevention of cancers, type I diabetes, heart disease and
osteoporosis. Am J Clin Nutr. 79:362–371. 2004.PubMed/NCBI
|
|
3
|
Mckenzie L, Liley JB and Bjorn LO: UV
Radiation: Balancing Risk and Benefits. Photochem Photobiol.
85:88–98. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Garland CF, Comstock GW, Garland FC,
Helsing KJ, Shaw EK and Gorham ED: Serum 25-hydroxyvitamin D and
colon cancer: Eight year prospective study. Lancet. 2:1176–1178.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Banwell CM, Singh R, Stewart PM, Uskokovic
MR and Campbell MJ: Antiproliferative signalling by 1,25(OH)2D3 in
prostate and breast cancer is suppressed by a mechanism involving
histone deacetylation. Recent Results Cancer Res. 164:83–98. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grant WB: An ecologic study of dietary and
solar ultraviolet-B links to breast carcinoma mortality rates.
Cancer. 94:272–281. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Grant WB: An estimate of premature cancer
mortality in the U.S. due to inadequate doses of solar
ultraviolet-B radiation. Cancer. 94:1867–1875. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zittermann A, Schleithoff SS, Tenderich H,
Berthold HK, Körfer R and Stehle P: Low vitamin D status: A
contributing factor in the pathogenesis of congestive heart
failure? J Am Coll Cardiol. 41:105–112. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Holick MF: Shedding new light on the role
of the sunshine vitamin D for skin health: The lncRNA-skin cancer
connection. Exp Dermatol. 23:391–392. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Matkovic V: Calcium metabolism and calcium
requirements during skeletal modeling and consolidation of bone
mass. Am J Clin Nutr. 54:245S–260S. 1991.PubMed/NCBI
|
|
11
|
Leccia MT: Skin, sun exposure and vitamin
D: Facts and controversies. Ann Dermatol Venereol. 140:176–182.
2013.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ralph AP, Lucas RM and Norval M: Vitamin D
and solar ultraviolet radiation in the risk and treatment of
tuberculosis. Lancet Infect Dis. 13:77–88. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ooms ME, Roos JC, Bezemer PD, van der Vijh
WJ, Bouter LM and Lips P: Prevention of bone lost by vitamin D
supplementation in elderly women: A randomized double blindtrial. J
Clin Endoc & Metab. 80:1052–1085. 1995. View Article : Google Scholar
|
|
14
|
Rivas M, Araya MC, Caba F, Rojas E and
Calaf GM: Ultraviolet light exposure influences skin cancer in
association with latitude. Oncol Rep. 25:1153–1159. 2011.PubMed/NCBI
|
|
15
|
Rivas M, Rojas E and Calaf GM: Prediction
of skin cancer ocurrence by ultraviolet solar index. Oncol Lett.
3:893–896. 2012.PubMed/NCBI
|
|
16
|
Rivas M, Rojas E and Calaf GM: Skin cancer
risk influenced by ultraviolet solar irradiance. Oncol Lett.
7:483–486. 2014.PubMed/NCBI
|
|
17
|
Rivas M, Leiva C and Rojas E: Estudio de
series temporales de energía solar UVB de 305 nm y espesor de la
capa de ozono estratosférico en Arica, norte de Chile. Ingeniare.
19:168–173. 2011.(In Spanish).
|
|
18
|
World Meteorological Organization (WMO), .
Report of the WMO Meeting of Experts on UV-B Measurements, Data
Quality and Standardization Of UV IndicesLes Diablerets. WHO;
Geneva, Switzerland: pp. 361994, (WMO TD no. 625).
|
|
19
|
Fitzpatrick TB: The validity and
practicality of sun-reactive skin types I through VI. Arch
Dermatol. 124:869–871. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sachdeva S: Fitzpatrick skin typing.
Applications in dermatology. Indian J Dermatol Venereol Leprol.
75:93–96. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Madronich S, McKenzie RL, Björn LO and
Caldwell MM: Changes in biologically active ultraviolet radiation
reaching the Earth's surface. J Photochem Photobiol B. 46:5–19.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Peters RD, Krueger AJ, Bhartia PK and
Herman JR: Earth probe total ozone mapping spectrometer (TOMS) Data
Products User's GuideNASA Reference Publication 1998-206895.
National Aeronautics and Space Administration; Washington, DC:
1998
|
|
23
|
Rivas M, Araya MC, Durán V, Rojas E,
Cortes J and Calaf GM: Ultraviolet light exposure and skin cancer
in the city of Arica, Chile. Mol Med Rep. 2:567–572.
2009.PubMed/NCBI
|
|
24
|
Bojkov R and Fioletov V: Estimating the
global ozone characteristics during the last 30 years. J Geoph Res.
100:16537–16551. 1995. View Article : Google Scholar
|
|
25
|
Schwalfenberg GK: Solar radiation and
vitamin D: Mitigating environmental factors in autoimmune disease.
J Environ Public Health 2012. Article ID. : 2012. View Article : Google Scholar
|
|
26
|
Moan J, Porojnicu AC, Dahlback A and
Setlow RB: Addressing the health benefits and risks, involving
vitamin D or skin cancer of increased sun exposure. Proc Natl Acad
Sci USA. 105:668–673. 2008. View Article : Google Scholar : PubMed/NCBI
|