Introduction
Lung cancer is one of the most prevalent health
problems, accounting for >1.6 million new cancer cases and 1.4
million cancer-related fatalities each year worldwide (1). The survival of lung cancer patients,
particularly for non-small cell lung cancer (NSCLC), which
constitutes ~80% of all lung cases diagnosed, mostly relies on
early detection. Surgery is the most critical treatment option to
improve the survival of NSCLC patients, however, only those
patients with early-stage disease and those who are physically able
can undergo surgical procedures. Hemophilia is an inherited blood
coagulation disorder caused by a genetic deficiency of blood
coagulation factors. Hemophilia often causes life-threatening
bleeding (2). The complication of
hemophilia often presents with deep internal bleeding, hemophilic
arthropathy and transfusion-transmitted infection (3). Patients with hemophilia are often not
suitable for any surgery, which may cause iatrogenic bleeding and
be life-threatening. The present study report the unusual case of a
lung cancer patient with hemophilia A who underwent surgery
successfully. The patient's diagnosis, treatment options for
hemophilia A and lung cancer, such as indications for thoracoscopic
lobectomy, pre-operative preparations and post-operative cares, and
other treatment options are discussed. Written informed consent was
obtained from the patient. The literature is also reviewed for the
treatment and management of such patients.
Case report
Admission to hospital
In June 2013, a 53-year-old male patient seeking
medical attention due to a cough with sputum that had persisted for
two month presented to the First Hospital of Jilin University
(Changchun, Jilin, China). The patient underwent a computed
tomography (CT) scan, which showed a 3.0×2.0-cm mass in the right
lower lobe of the lung and was subsequently admitted. A physical
examination showed stable vital signs, stained body skin, stained
conjunctival and oral mucosa, swollen joints, and darker old scars
on the forehead. The patient could not walk independently.
Moreover, the bilateral thoracic size was symmetrical, bilateral
breathing was smooth and bilateral fremitus was normal.
Auscultation of the lungs revealed slightly weaker breathing sounds
in the right lower lung. The systemic lymph nodes were normal.
Auxiliary lung CT showed a 3.0×2.0-cm mass in the right lower lobe
with irregular edges and burrs, but there was no significant
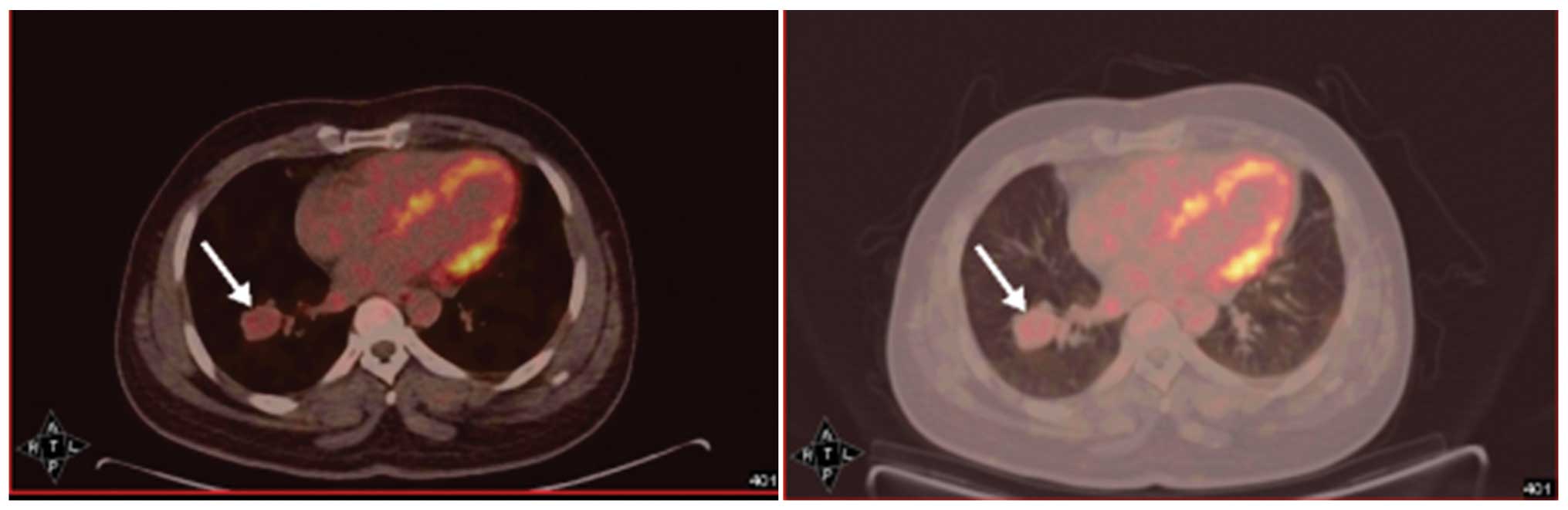
mediastinal lymph node enlargement. Positron emission
tomography-computed tomography (Fig.
1) in the right lower lobe lung revealed a high metabolic mass
with possible large lumps, 3.0×2.0 cm in size. Cardiac function was
rated with a fractional shortening value of 32% (normal range,
25–35%) and an ejection fraction value of 68% (normal range,
>50%), while lung function was recorded with a 2.86 l/sec forced
expiratory volume in one second (FEV1; normal range, 80–120 l/sec).
There was no significant mediastinal lymph node metastasis.
Laboratory tests showed an activated partial thromboplastin time
(APTT) of 66.5 sec (normal range, 20–40 sec), a prothrombin time of
16.3 sec (normal range, 9–13 sec), a fibrinogen (Fbg) level of 6.34
g/l (normal range, 2–4 g/l), a platelet level of
323×109/l (normal range, 125–250×109/l), an
alanine aminotransferase level of 23 U/l (normal range, 10–60 U/l)
and 0.80% blood coagulation factor VIII (normal range, 50–150%). It
was noted that 40 years ago, the patient had suffered excessive
bleeding after a minor trauma and was subsequently diagnosed with
influenza with severe hereditary hemophilia and underwent a
long-term treatment with factor VIII (monthly infusion of ~250 mg),
and that the bleeding symptoms were controlled well.
Pre-surgical preparations and
surgery
The patient underwent a routine health examination,
which revealed a normal electrocardiogram, normal echocardiography
and 90% FEV1/forced vital capacity. The family members and patient
refused a bronchoscopy. The patient was subjected to dynamic
monitoring of clotting factor VIII levels, with timely infusion of
clotting factor VIII (Bai Keqi, Bayer HealthCare AG, Beijing,
China) according to the formula: Required factor VIII units (IU) /
Ci = 0.5 × patient body weight (kg) × required elevated levels of
factor VIII activity (% of normal). This resulted in administration
of ~3,400 IU daily, and 1 day prior to surgery, the levels of
factor VIII had reached 87%. During surgery, the patient was
infused with 10 units of red blood cell suspension and 1,000 ml
plasma. Surgical anesthesia was used for the thoracoscopic right
lower lobe resection and lymph node dissection. During and after
the surgery, the patient did not experience any significant
bleeding (~400 ml), and was subsequently infused with two units of
red blood cells and 400 ml plasma.
Post-surgical care
Following the successful surgical removal of the
lung cancer lesion, the patient continued to receive factor VIII
infusion therapy and dynamic monitoring (Table I).
 | Table I.Dynamic monitoring of the patient for
continued factor VIII infusion therapy. |
Table I.
Dynamic monitoring of the patient for
continued factor VIII infusion therapy.
| Days
post-surgery | Dose of factor VIII,
IU | Blood levels of
factor VIII, % | Chest fluid volume
and color trait |
|---|
| 1 | 3500 | 120.00 | 600 ml of dark red
bloody fluid |
| 2 | 3500 | 128.10 | 250 ml of dark red
bloody fluid |
| 3 | 3500 | 133.50 | 150 ml of pinkish
transparent liquid |
| 4 | 3500 | 207.50 | 140 ml of pinkish
transparent liquid |
| 5 | 3500 | 160.20 | 100 ml of pinkish
transparent liquid |
| 6 | 3500 | 140.20 | Pleural drainage tube
removed |
| 7 | 2000 |
61.00 | – |
| 9 | 2000 | 111.00 | – |
| 11 | 1000 |
57.00 | – |
| 13 | 500 |
22.00 | – |
| 15 |
0 | – | Discharged from
hospital |
The patient also underwent conventional
post-operative treatment with ambroxol (60 mg, twice daily for 7
days), omeprazole (40 mg, twice daily for 2 days) and cefoxitin
sodium (2,000 mg, twice daily for 5 days). At 24 h post-surgery,
the patient was generally in good condition, exhibiting stable
vital signs and weak breathing sounds on lung auscultation. The
number and percentage of white blood cells gradually reached normal
levels. Routine coagulation tests showed an APTT of 44.4 sec and an
Fbg level of 4.82 g/l. Post-operative thoracic drainage gradually
decreased, the coloration changing from dark red bloody fluid into
pink transparent liquid. The patient had generally recovered 4 days
later, with stable vital signs and lung CT showing post-operative
changes in lung compliance, with good lung re-expansion, although
there was still a small liquid shadow in the right lower lobe.
Blood and liver functions were normal. On post-operative day 6, the
chest tube was removed and the patient showed no evident
discomfort. On pathological examination, a 2.3×3.1×2.2 cm tumor was
identified in the right lower lobe. The tumor was unencaspulated,
grey and yellow in colour, and composed of poorly differentiated
cells with unclear cytoplasmic boundaries and round nuclei. A
pathological diagnosis of a right lower lobe low-grade
neuroendocrine tumor (formerly carcinoid tumor) [TNM stage, T2aN0M0
(4)] without lymph node metastasis
was made. On post-operative day 15, the patient was discharged.
Discussion
The lifespan of patients with severe hemophilia who
do not receive an adequate modern treatment regimen is markedly
reduced. Indeed, these patients often do not reach maturity. By
contrast, patients with hemophilia who receive appropriate therapy
go on to live 50–60 years (5). Such
patients, however, may suffer from other diseases, including lung
cancer. As surgery may cause uncontrolled bleeding in these
patients, they are often not suitable for surgery.
In the present case study, the case of a hemophilia
patient with lung cancer who underwent surgical removal of a tumor
lesion is presented. Indeed, to date, there have been few studies
describing minor surgical procedures in hemophilia patients
(6–8),
however, no cases of lobectomy use for the removal of a lung tumor
have been reported. As these patients lack the hemophilia clotting
factor due to a genetic defect, such surgical procedures are
believed to be extremely risky. Thus, extensive pre-operative
preparations and post-operative care are of utmost importance for
these patients. Through the course of the diagnosis and treatment
in the present case, the maintenance of factor VIII levels was
found to be critical, since the biological half-life of factor VIII
is between 6 and 14 h. As such, regular monitoring of blood
clotting factor levels during treatment adjustment of infusion
doses and intervals is crucial (3).
Bai Keqi factor VIII is a recombinant preparation for the treatment
of hemophilia factor, with better efficacy and safety profiles when
compared with plasma or cryoprecipitate direct input treatment,
which are considered the conventional preoperative treatments for
patients with hemophilia. However, recombinant factor VIII
preparation for Chinese patients has not yet been reported.
Therefore, the selection and use of Bai Keqi clotting factor drug
was a better choice and following such treatment, patients have
exhibited no symptoms of factor VIII-specific antibody generation,
which is a specific neutralization reaction against such treatment
in the host (9). The present patient
responded well to treatment, and 5 days after surgery, the
post-operative drainage tubes were removed and the drug dose was
reduced to half and a normal blood factor VIII level (>80%) was
maintained, although blood factor VIII levels in the patient
declined. Specifically, the patient did not show any evident signs
of discomfort or adverse symptoms, the drainage liquid color
gradually cleared from dark red to yellow and transparent, and the
post-operative thoracic drainage was gradually reduced. Thus, the
treatment was considered successful.
Lung cancer surgery or thoracoscopic thoracic
surgery could be an important option for such patients, if they are
carefully treated. The present study indicates that the treatment
course, and drug choice and amount are crucial factors for
successfully managing these patients prior to, during and following
surgical procedures. In the present study, the choice of surgery
was a minimally invasive thoracoscopic technique. For
post-operative care, the coagulation factor, and pleural drainage
volume and color were dynamically monitored, which was consistent
with and supported by other studies (10,11).
In the current study, the case of a lung cancer
patient with hemophilia who underwent successful surgical resection
of a tumor lesion was presented. Hemophilia can lead to spontaneous
hemorrhage and coagulopathy and thus, hemophilia patients exhibit a
high risk when undergoing surgery. However, minimally invasive
surgical techniques and genetically engineered drug treatments have
been developed which decrease this risk. The patient in the present
study underwent a thoracoscopic lobectomy following the
administration of a pre-operative preparation and the procedure was
successful. Future studies of such patients will improve knowledge
with regard to the clinical management of hemophilia patients that
require surgery for the treatment of other conditions.
References
|
1
|
Rakovich G and Tremblay L: Tailored
therapy in lung cancer. Can Respir J. 20:367–368. 2013.PubMed/NCBI
|
|
2
|
Chen HZ: Practical Internal Medicine
(10th). Beijing: People's Medical Publishing House. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siboni SM, Biguzzi E, Solimeno LP, Pasta
G, Mistretta C, Mannucci PM and Peyvandi F: Orthopaedic surgery in
patients with von Willebrand disease. Haemophilia. 20:133–140.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ettinger DS, Wood DE, Akerley W, et al:
Non-small cell lung cancer, version 1.2015. J Natl Compr Canc Netw.
12:1738–1761. 2014.PubMed/NCBI
|
|
5
|
Chorba TL, Holman RC, Strine TW, Clarke MJ
and Evatt BL: Changes in longevity and causes of death among
persons with hemophilia A. Am J Hematol. 45:112–121. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Washino S, Hirai M, Kobayashi Y, Saito K
and Miyagawa T: Heavy hematuria requiring cystectomy in a patient
with hemophilia A: A case report and literature review. BMC Urol.
15:842015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ingram GI: Haemophilia and the forbidden
abdomen. Haemophilia. 6:719–722. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lavery HJ, Senaratne P, Gainsburg DM and
Samadi DB: Robotic prostatectomy in a patient with hemophilia.
JSLS. 14:439–441. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Beutler E, Lichtman MA, Coller BS, Kipps
TJ and Seligsohn U: Williams Hematology (6th). New York:
McGraw-Hill Professional. 2001.
|
|
10
|
Demmy TL and Nwogu C: Is video-assisted
thoracic surgery lobectomy better? Quality of life considerations.
Ann Thorac Surg. 85:S719–S728. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Craig SR, Leaver HA, Yap PL, Pugh GC and
Walker WS: Acute phase responses following minimal access and
conventional thoracic surgery. Eur J Cardiothorac Surg. 20:455–463.
2001. View Article : Google Scholar : PubMed/NCBI
|