Introduction
Approximately 4% of metastases in the lung evolve
into cavity lesions, two-thirds of which are from squamous cell
primary tumors. Spontaneous cavitation of metastases from the
bladder (1), kidney (2) and synovial sarcoma (3) have been reported, however, few studies
have reported the cavitation of metastases following systematic
treatment (4). Post-therapy
cavitation from gland cell primary tumors is particularly rare, and
we hypothesize that the cavitation process following therapy
involves a completely different mechanism and morphology compared
with the necrotic tumor process.
Currently, the incidence of non-squamous
non-small-cell lung cancer (NSCLC) is increasing and the disease is
frequently associated with the activation of genetic alterations
that become innovative therapeutic targets (5). This case report describes the cavitation
of multiple solid lung metastases in targeted monotherapy in a
39-year-old male, and follows the changes for three years. The
patient provided informed consent for the publication of this
study.
Case report
Case presentation and treatment
A 39-year-old male presented at The People's
Hospital of Jingjiang (Jingjiang, China) in December 2007 with the
complaint of a cough with left-side chest pain for four years and
sputum with blood for a week. He was a non-smoker, but had smoked
passively for five years. Chest computed tomography (CT) was
normal. In 2011, the constant stuffy pain had gradually increased
without cause and the patient spitted sputum with blood streaks
after playing badminton. Local hospital chest radiography revealed
a lesion occupying the left lung, and the patient was admitted to
the Respiratory Department of the First Affiliated Hospital of
Nanjing Medical University (Nanjing, China), for further
investigation. Abnormal tumor markers revealed a carcinoembryonic
antigen level of 13.69 ng/l and a neuron-specific enolase level of
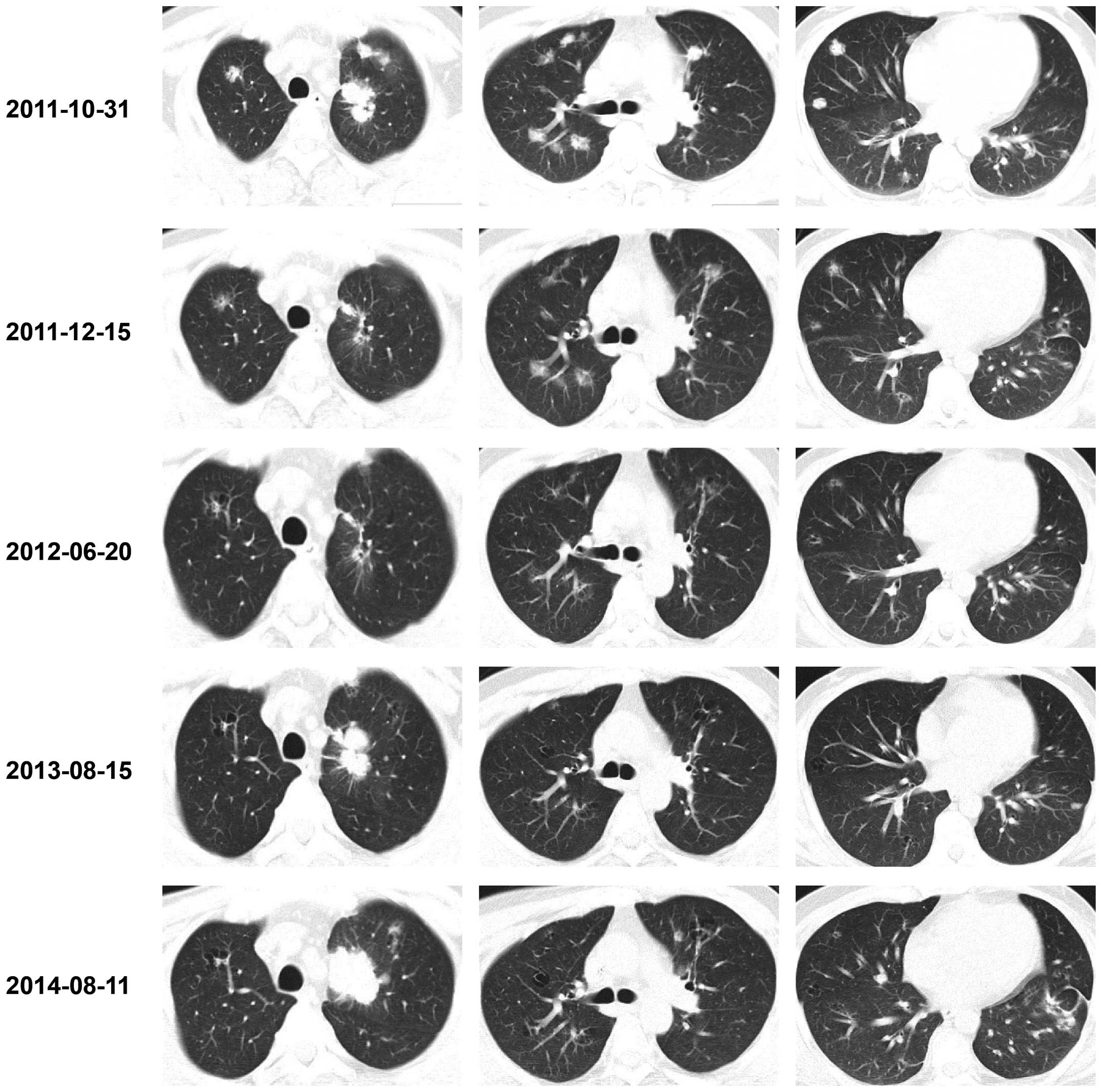
18.29 ng/l. In October 2011, chest CT revealed a left upper lobe
stiff spiculated mass with multiple intrapulmonary nodules
(Fig. 1). A left lower pulmonary
wedge resection was conducted following consultation with the
Cardial Surgery Department, and the pathological result was
adenocarcinoma (T2aN3M1a-IV). Further gene mutation detection
presented epidermal growth factor receptor (EGFR) gene mutation
with exon 21 T/G hybrid positivity, which prompted the clinical use
of EGFR gene-targeting drugs. The patient's Karnofsky score was 90,
and Tarceva was administered orally on a daily basis. During the
process, regular chest CT and tumor markers were monitored.
3-year follow-up
In December 2011, a chest CT scan revealed the
primary tumor together with multiple metastases appearing to be
decreased in size and of a relatively lower density. Certain
metastatic nodules were round with a small hole in the center.
In June 2012, chest CT revealed further improvement
of the primary tumor and metastases. Multiple irregular cavities
with thickened septum appeared to have replaced the original tumor
node metastases. The patient's carcinoembryonic antigen level was
7.04 ng/l.
In August 2013, chest CT demonstrated larger and
clearer cavities resembling pulmonary bullous, while the primary
cancer increased in size. In the period that followed, the
patient's tumor markers and chest CTs were monitored every two
months until April 2014. The patient's carcinoembryonic antigen
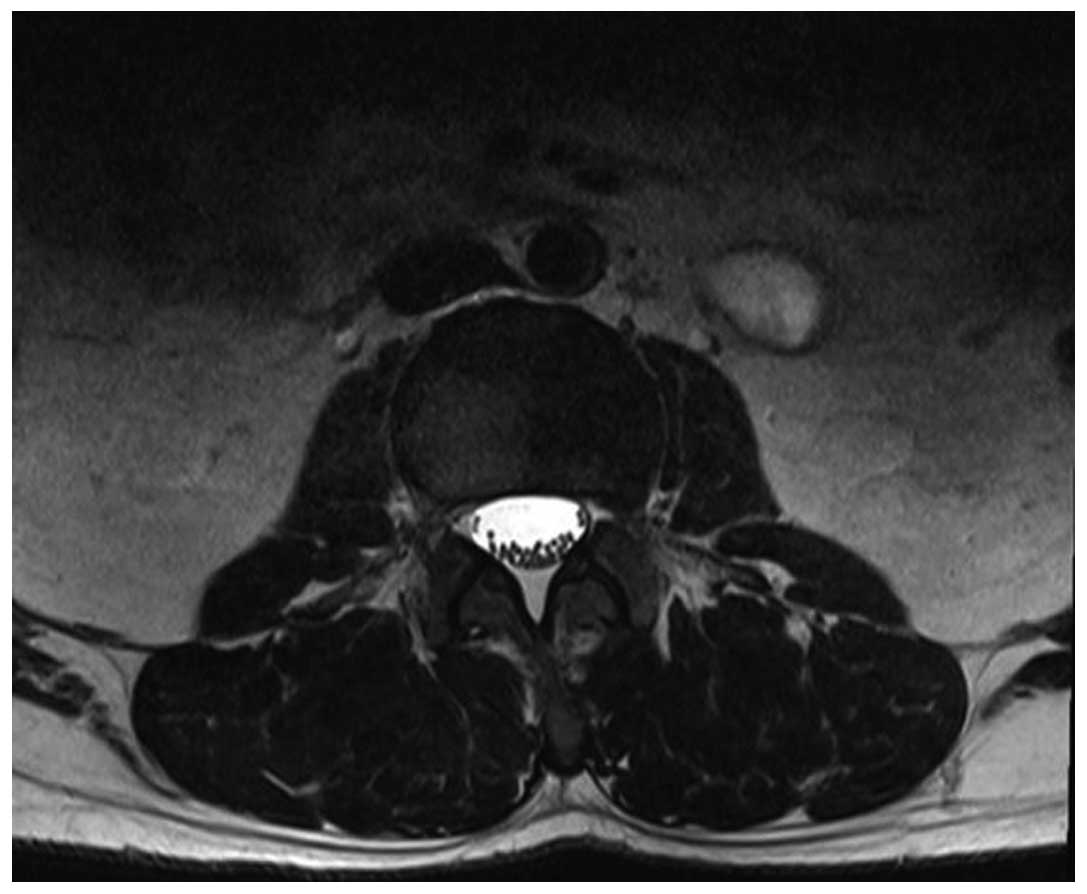
level increased to 9.9 ng/l and he experienced waist pain. Lumbar
magnetic resonance imaging revealed a hyperintense nodule in the
third lumbar vertebrae on the T2-weighted image (Fig. 2). The pathological result following
surgery confirmed the suspicion of bone metastasis. The patient
started a chemotherapy regimen of pemetrexed disodium (0.9 g) plus
carboplatin (600 mg) once a month.
In August 2014, during the fourth month of
chemotherapy, the patient had a carcinoembryonic antigen level of
9.7 ng/l, a cytokeratin 19 fragment level of 0.7 ng/l and a
neuron-specific enolase level of 14.4 ng/ml. Chest CT revealed the
growth of the original tumor with several new metastases and slight
pleural effusion on the left side, without any notable changes to
the existing cavities.
Pathological analysis
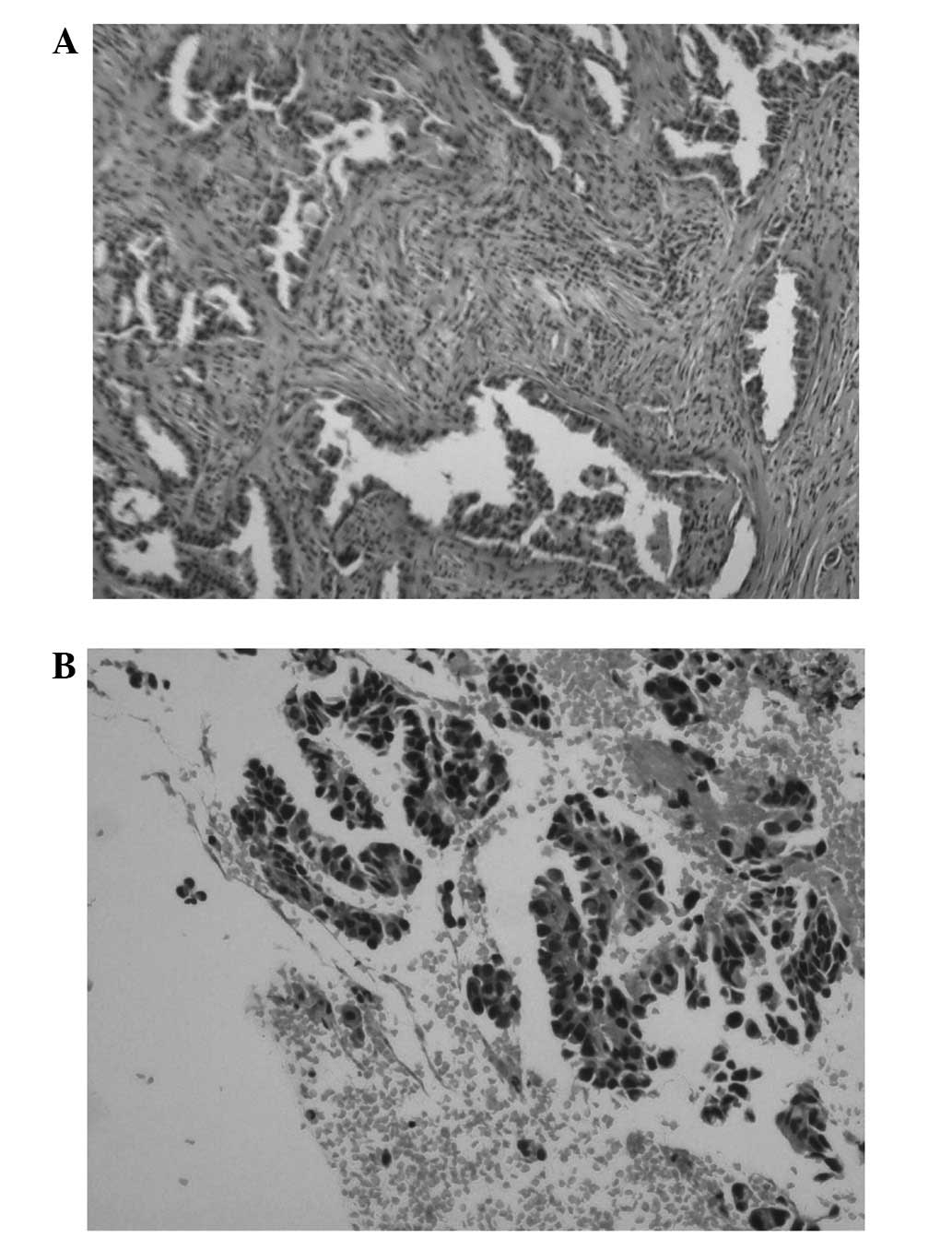
The pathological results of the surgical specimen
revealed dysplastic cells arranged in a gland-like formation among
the intercellular matrix, which presented a microscopic
manifestation typical of adenocarcinoma (Fig. 3). Papillary arrangements of broken
atypical epithelial cells were noted among the bone tissue and
blood cells on the vertebral pathological analysis (Fig. 4).
Discussion
Outcomes for locally advanced NSCLC remain
suboptimal, with a median overall survival duration of ~20 months
(6). The identification of somatic
mutations of EGFR brought about a paradigm shift in therapeutic
strategy (7). Extensive research
focused on the survival outcome of patients with EGFR-mutant
advanced NSCLC depending on the different combined modality therapy
employed or whole-body extent of metastasis (8,9). In the
present study, we presented a rare case of cavitation transition of
lung metastasis owing to effective targeted therapy. Although in
the later stage of the disease process, the primary tumor turned to
a growth momentum and new metastases appeared, the already formed
smooth cavities did not demonstrate notable changes and never
filled with fluid or necrotic debris.
Cavitation usually forms as a result of necrosis
from insufficient blood supply to the tumor or invasion of vessels
by tumor cells, which always raises the likelihood of disease
progress. Kurian et al (10)
reported a case of urothelial bladder cancer with cavitary lung
metastases, which exhibited a large irregular cavity surrounded by
a wall of uneven thickness. This type of cavity is formed by
central ischemic necrosis with the progression of the tumor. Unlike
common cavities with irregular lumen and wall nodules, this type of
thin-walled and smooth morphology may reflect a completely
different mechanism and to a certain extent supports the improved
treatment effect. Mermershtain et al (4) reported the only case of massive
cavitation of solid pulmonary metastatic lesions in a breast cancer
patient following adjuvant chemotherapy and radiation therapy. The
regular and sharply defined cavities resemble those of our case and
may specifically appear following effective therapy.
For the present case, this type of regular
cavitation resulted from inhibited tumor angiogenesis and provided
clinical reference value for treatment effectiveness.
References
|
1
|
Koh KB, Rogawski K and Smith PH:
Cavitating pulmonary metastases from superficial transitional cell
carcinoma of urinary bladder. Case report. Scand J Urol Nephrol.
28:201–202. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Essadki O, Chartrand-Lefèbvre C, Finet JF
and Grenier P: Cystic pulmonary metastasis simulating a diagnosis
of histiocytosis X. J Radiol. 79:886–888. 1998.(In French).
PubMed/NCBI
|
|
3
|
Cohen MC and Drut R: Persistent
interstitial pulmonary emphysema-like cyst associated with
metastatic synovial sarcoma. Pediatr Dev Pathol. 3:391–393. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mermershtain W, Schulman H, Hertzanu Y and
Cohen Y: Massive cavitation of solid pulmonary metastatic lesions
in a breast cancer patient: A case report. Ann Oncol. 13:173–174.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wu M, Zhao J, Song SW, Zhuo M, Wang X, Bai
H, Wang S, Yang L, An T, Zhang Y, et al: EGFR mutations are
associated with prognosis but not with the response to front-line
chemotherapy in the Chinese patients with advanced non-small cell
lung cancer. Lung Cancer. 67:343–347. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hanna N, Neubauer M, Yiannoutsos C,
McGarry R, Arseneau J, Ansari R, Reynolds C, Govindan R, Melnyk A,
Fisher W, et al: Hoosier Oncology Group; US Oncology: Phase III
study of cisplatin, etoposide, and concurrent chest radiation with
or without consolidation docetaxel in patients with inoperable
stage III non-small-cell lung cancer: the Hoosier Oncology Group
and U.S. Oncology. J Clin Oncol. 26:5755–5760. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Azzoli CG, Baker S Jr, Temin S, Pao W,
Aliff T, Brahmer J, Johnson DH, Laskin JL, Masters G, Milton D, et
al: American Society of Clinical Oncology: American Society of
Clinical Oncology Clinical Practice Guideline update on
chemotherapy for stage IV non-small-cell lung cancer. J Clin Oncol.
27:6251–6266. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee DS, Kang JH, Lee CG, Kim SJ, Choi YJ,
Lee KY and Kim YS: Predicting Survival in Patients with Advanced
Non-squamous Non-small Cell Lung Cancer: Validating the Extent of
Metastasis. Cancer Res Treat. 45:95–102. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mak RH, Doran E, Muzikansky A, Kang J,
Neal JW, Baldini EH, Choi NC, Willers H, Jackman DM and Sequist LV:
Outcomes after combined modality therapy for EGFR-mutant and
wild-type locally advanced NSCLC. Oncologist. 16:886–895. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kurian A, Lee J and Born A: Urothelial
bladder cancer with cavitary lung metastases. Can Respir J.
18:e46–e47. 2011.PubMed/NCBI
|