Introduction
Cerebrovascular disease is the one of the most
frequent cancer complication of the central nervous system, second
to brain metastasis (1). The
largest study thus far, found that 14.6% of 3,426 cancer patients
had cerebrovascular disease based on pathological autopsy results,
and ~50% of them were symptomatic (1). Cerebrovascular complications often
affect the prognosis of cancer; thus, diagnosis and treatment of
these associated pathologies is important. Cerebral venous sinus
thrombosis (CVST) is a rare disease of the cerebrovascular system,
and there have been few reports of cancer patients with CVST
(2). A rare case of leptomeningeal
carcinomatosis (LC) is presented, which may be an underlying cause
for CVST in patients with lung cancer.
Case report
A 64-year-old female was referred to the Japanese
Red Cross Okayama Hospital (Okayama, Japan) with complaints of
experiencing dizziness for two weeks. The patient was not
prescribed any medications and had no specific family history. She
had smoked one packet of cigarettes a day for 40 years. A
neurological examination revealed a mild cognitive impairment
(mini-mental state examination, 21/30), left-side fixation
nystagmus, and an ataxic gait. Chest computed tomography (CT)
revealed an ~3-cm peripheral nodule in the left upper lobe, and
brain magnetic resonance imaging (MRI) demonstrated the presence of
multiple brain masses in the bilateral cerebrum, cerebellum and
pons. Hematological, coagulation, biochemical, and serological
findings were normal, except for elevated carcinoembryonic antigen
(CEA) and sialylated SSEA-1 antigen levels of 115.8 ng/ml and 32.5
U/ml, respectively. Whole-brain radiotherapy was conducted (30 Gray
total) in 10 fractions for two weeks with intravenous dexamethasone
and concentrated glycerin, based on a tentative diagnosis of lung
cancer with multiple brain metastases.
The diagnosis was later confirmed as a lung
adenocarcinoma by an endobronchial biopsy, with a mutated (exon 19
deletion) epidermal growth factor receptor (EGFR). The patient also
had multiple pulmonary, bone, and left adrenal metastases, and was
therefore designated T4N3M1b, stage IV, by the clinical TNM
classification system. There was temporary improvement of symptoms
until the development of a severe headache on the 31st day of
hospitalization, which became exacerbated with neck stiffness for a
few days. On the 33rd day of hospitalization, brain CT revealed a
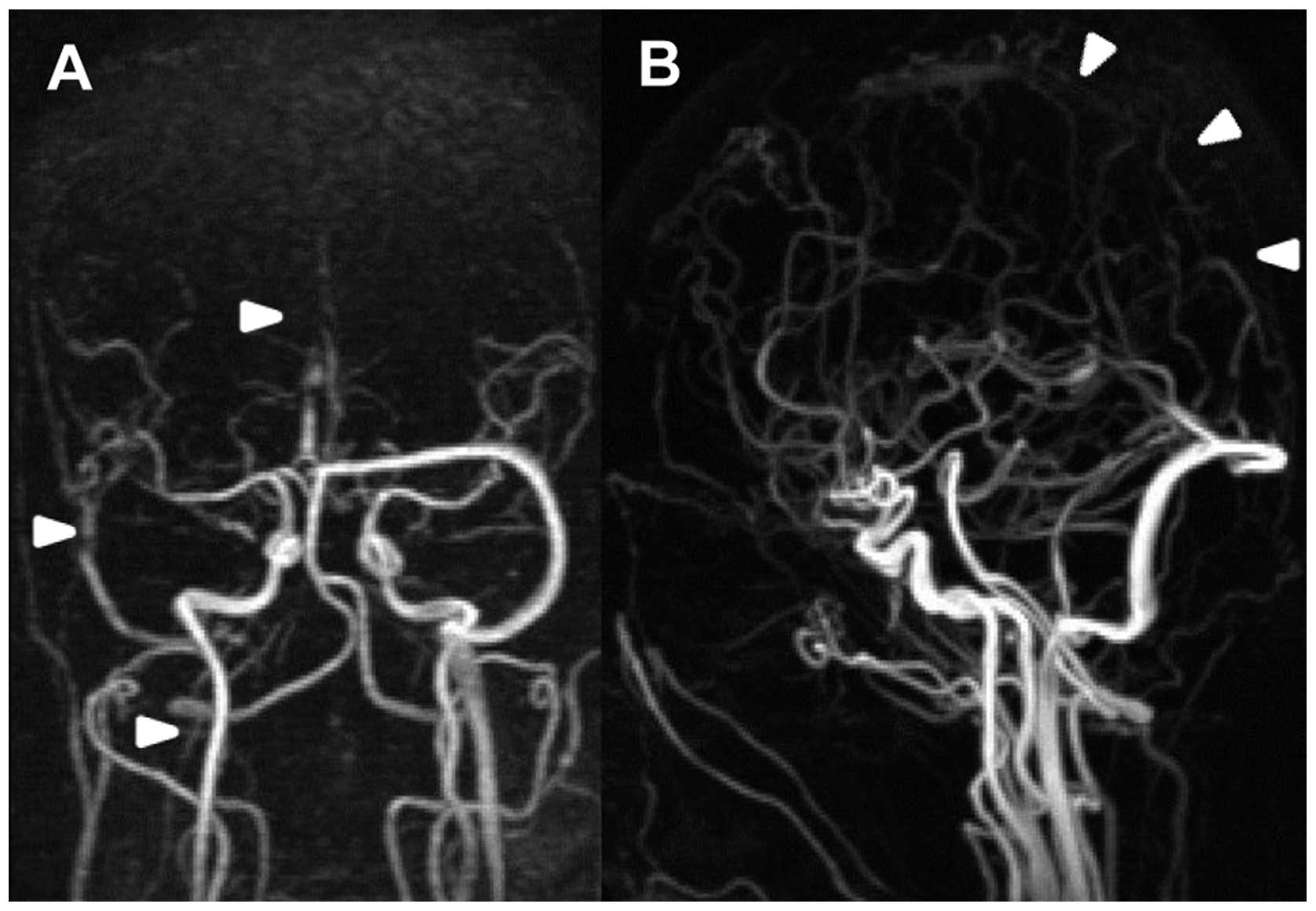
hyperdense area at the right transverse venous sinus (Fig. 1). Magnetic resonance venography
(MRV) revealed defects in the superior sagittal, right sigmoid, and
right transverse venous sinuses, as well as the right internal
jugular vein (Fig. 2). D-dimer
levels were elevated from 0.2 to 1.3 μg/ml. The blood cell count,
prothrombin time, activated partial thromboplastin time,
fibrinogen, antithrombin III, protein C, protein S, and
homocysteine levels were all within the normal limits, and lupus
anticoagulant and anticardiolipin antibodies were negative. A neck
echography did not detect lymph node metastases compressing the
jugular vein. Anticoagulation therapy using unfractionated heparin
was immediately administered following confirmation of the
diagnosis of CVST. Brain MRI also demonstrated leptomeningeal
gadolinium enhancement in the front of the pons and medulla
(Fig. 3). The cerebrospinal fluid
cell count, protein and CEA results increased to 12 cells/μl, 797
mg/dl and 4650 ng/ml, repsectively, whereas glucose results
decreased to 11 mg/dl. Positive cerebrospinal fluid tumor cytology
confirmed the diagnosis of LC. Following four weeks of
anticoagulation therapy, complete thrombolysis was confirmed by MRV
(Fig. 4). Anticoagulation therapy
using warfarin was subsequently continued. The patient became
drowsy due to secondary hydrocephalus; however, she returned to
consciousness following insertion of a lumboperitoneal shunt.
Effective treatment with gefitinib (250 mg daily) was administered,
and the patient survived for 10 months following the diagnosis of
CVST and LC.
Discussion
CVST is a rare cerebrovascular disease with an
estimated five people per million being affected each year,
accounting for 0.5–1% of all cerebrovascular diseases. Causes of
the disease are divided into acquired and genetic factors. Acquired
factors include infection, surgery, trauma, pregnancy, puerperium,
anti-phospholipid antibody syndrome, malignant tumor, and the use
of hormone preparations. Genetic factors include a congenital
clotting abnormality (3).
Approximately 7.4% CVST cases are associated with malignant tumors.
The underlying mechanisms of malignant tumor-induced CVST include
direct pressure on the sinus venosus by the tumor (dural/cranial
metastasis), direct tumor extension into the sinus venosus,
thrombophilia, and side effects of anti-cancer agents such as
tamoxifen and L-asparaginase (3).
Sigsbee et al (4) reported
seven malignant tumor patients with complications of superior
sagittal venous sinus thrombosis. It was shown that thrombophilia
due to the malignant tumor led to sinus thrombosis. Raizer et
al (5) reported 20 malignant
tumor patients with complications of CVST. According to their
report, 9/20 patients had hematological malignancies, of whom five
were administered L-asparaginase, two exhibited disseminated
intravascular coagulation, and one had leukocytosis. In addition,
11/20 patients had solid tumors, six of which were dural/cranial
metastases, three were administered antiestrogen agents, two had
LC, one had low partial thromboplastin time, and one had
thrombocytosis (5). The patient
described in the present study exhibited a normal blood count at
the time of onset and a slightly elevated D-dimer level of 1.3
ng/ml in the coagulation test. It was therefore unclear whether the
patient had thrombophilia. Furthermore, there was no dural/cranial
metastasis that would directly result in pressure on the sinus
venosus.
Although the adverse effects of whole-brain
radiotherapy are known, there have been no reports thus far on CVST
complications caused by radiation exposure. At the time of
hospitalization, the patient did not present with symptoms
suggestive of LC, such as headache or neck stiffness, and there
were no images to support a diagnosis of LC. The disease became
evident during the progression of the patient, which was consistent
with the onset of CVST. It is proposed that in this case, LC
contributed to the onset of CVST. Previous case reports suggesting
an association between LC and CVST include that of Li et al
(6), who proposed that it was an
extremely rare complication unique to patients with ovarian cancer.
However, the underlying mechanism responsible for the disease was
unclear and as with the present case study, pathology was not
performed. Cerebrospinal fluid is produced in the choroid plexuses,
circulated through the subarachnoid space, and absorbed in the
sinus venosus through the arachnoid granulations protruding into
the sinus venosus (7). Given this
physiological circulatory route, it was inferred that thrombosis
may occur due to direct extension into the sinus venosus of the
tumor cells present in the cerebrospinal fluid, or the spread of
inflammation into the vascular endothelium of the sinus
venosus.
Approximately 90% of patients exhibit headache as a
symptom of CVST, reflecting an increase in intracranial pressure.
Pain throughout the whole head typically worsens over several days
or weeks, although some patients develop sudden headaches
suggestive of a subarachnoid hemorrhage, as was evident in the
present case study. Neurological focal symptoms are not often
present unless there are complications of cerebral infarction or
cerebral hemorrhage (3). Abnormal
findings indicating CVST using plain CT have a low detection rate
of ~30%, therefore the current technique used for diagnosis is
brain MRI (in particular a T2* MRI) combined with MRV (8). For treatment, anticoagulation therapy
using unfractionated heparin or low-molecular-weight heparin is
initially administered and thereafter is changed to vitamin K
antagonists (3). According to a
previous report by Ferro et al (9) on 624 patients, most of whom received
anticoagulation therapy, 79% achieved complete neurologic recovery
and 8.3% succummbed to the disease. Although cerebral infarction
and cerebral hemorrhage may lead to poor prognosis, numerous
patients receiving proper diagnosis and early treatment, can
improve without experiencing any neurological sequelae.
Similar to hematological malignancies and breast
cancer, lung cancer is often complicated by LC, with an incidence
rate of 1–6%. LC is treated by a combination of systemic and
intrathecal chemotherapy, and spinal cord radiation. The benefits
of this treatment, however, are limited and even when administered,
the prognosis is extremely poor with a median survival of 8–16
weeks (10). It has been reported
that in EGFR mutation-positive (exon 19 deletion) patients with
non-small cell lung cancer complicated by LC, a survival rate of 11
months can be achieved with targeted treatment using EGFR-tyrosine
kinase inhibitors (TKI) such as gefitinib (11). Following the administration of
gefitinib to the presented patient, a survival period from LC onset
of ~10 months was achieved. Recent developments in the genetic
diagnosis and targeted molecular therapy have significantly
improved the prognosis of patients with non-small cell lung cancer.
It has therefore become more viable to manage complications
associated with lung cancer.
Based on a review of the literature, this is the
first case report, to the best of our knowledge, of CVST
concomitant with LC due to lung cancer. Adequate early diagnosis
and treatment of CVST enabled an improved survival time, despite LC
in this case. Development of headaches in patients with lung cancer
should be considered for CVST. Furthermore, following diagnosis of
CVST, LC should be investigated as an underlying cause.
References
|
1
|
Graus F, Rogers LR and Posner JB:
Cerebrovascular complications in patients with cancer. Medicine
(Baltimore). 64:16–35. 1985.
|
|
2
|
Rogers LR: Cerebrovascular complications
in patients with cancer. Semin Neurol. 24:453–460. 2004.
|
|
3
|
Saposnik G, Barinagarrementeria F, Brown
RD Jr, et al; American Heart Association Stroke Council and the
Council on Epidemiology and Prevention. Diagnosis and management of
cerebral venous thrombosis: a statement for healthcare
professionals from the American Heart Association/American Stroke
Association. Stroke. 42:1158–1192. 2011.
|
|
4
|
Sigsbee B, Deck MD and Posner JB:
Nonmetastatic superior sagittal sinus thrombosis complicating
systemic cancer. Neurology. 29:139–146. 1979.
|
|
5
|
Raizer JJ and DeAngelis LM: Cerebral sinus
thrombosis diagnosed by MRI and MR venography in cancer patients.
Neurology. 54:1222–1226. 2000.
|
|
6
|
Li HK, Harding V, Williamson R, et al:
Cerebral sinus thrombosis and leptomeningeal carcinomatosis in a
patient with ovarian cancer. J Clin Oncol. 30:e19–e20. 2012.
|
|
7
|
Sakka L, Coll G and Chazal J: Anatomy and
physiology of cerebrospinal fluid. Eur Ann Otorhinolaryngol Head
Neck Dis. 128:309–316. 2011.
|
|
8
|
Bousser MG and Ferro JM: Cerebral venous
thrombosis: an update. Lancet Neurol. 6:162–170. 2007.
|
|
9
|
Ferro JM, Canhão P, Stam J, et al:
Prognosis of cerebral vein and dural sinus thrombosis: results of
the International Study on Cerebral Vein and Dural Sinus Thrombosis
(ISCVT). Stroke. 35:664–670. 2004.
|
|
10
|
Beauchesne P: Intrathecal chemocherapy for
treatment of leptomeningeal dissemination of metastatic tumors.
Lancet Oncol. 11:871–879. 2010.
|
|
11
|
Umemura S, Tsubouchi K, Yoshioka H, et al:
Clinical outcome in patients with leptomeningeal metastasis from
non-small cell lung cancer: okayama lung cancer study group. Lung
Cancer. 77:134–139. 2012.
|