Introduction
Schwannomas are rare tumors histologically derived
from Schwann cells that form the neural sheath. The tumors occur
most frequently in the head, neck, arms and limbs. Primary
schwannomas of the colon and rectum that are not associated with
von Recklinghausen’s disease are extremely rare (2–6% of all
stromal tumors of digestive tract); only ~50 cases are reported in
the literature worldwide (1).
Schwannomas are mostly asymptomatic, but can present with
non-specific symptoms, including pain, fatigue and fever.
Occasionally, rectal bleeding and signs of colonic obstruction may
also occur (2). The majority of
primary schwannomas are benign and asymptomatic; nevertheless, the
possibility of malignant degeneration exists and is directly
associated with the tumor dimensions. Radical excision with margins
free of disease is the treatment of choice, since the response to
chemotherapy and radiotherapy remains uncertain (3). Despite aggressive surgical management,
these tumors may appear with a high rate of local recurrence and
malignant degeneration. In such cases, there are few treatment
options and the prognosis is poor (3).
Case report
A 65-year-old male underwent colonoscopy due to the
presence of occult blood in the feces. The procedure revealed an
oval-shaped mass of roughly 2.5 cm in diameter covered by ulcerated
mucosa, located 22 cm from the anal verge. Endoscopic
ultrasonography revealed an hypo-oechogenic, homogeneous lesion,
with well-defined margins, originating from the submucosa. A
standard biopsy examination indicated a gelatinous carcinoma. A
total body computed tomography scan excluded metastasis, therefore
the patient underwent a laparoscopic resection of the left
colon.
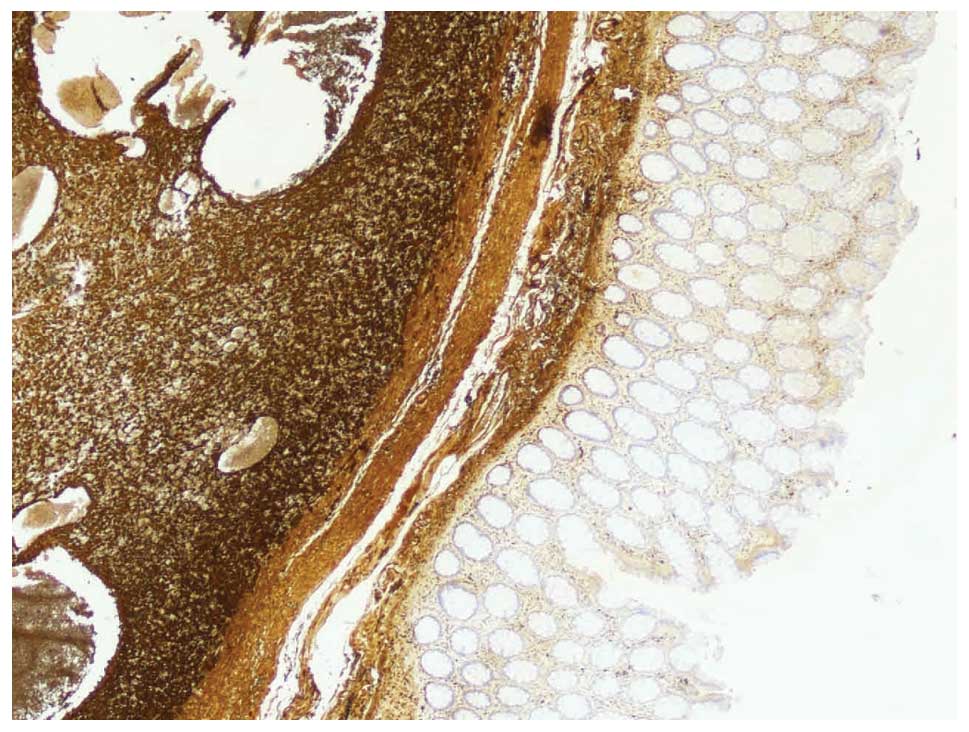
A histological examination revealed a schwannoma
covered by an ulcerated mucosa. Immunohistochemistry showed that
the tumor was positive for S100 and vimentin, but negative for
cluster of differentiation (CD)117, cytokeratin (CK)7, CK20,
chromogranin, actin and synaptophysin, with a Ki-67 proliferative
index of 3% (Fig. 1). The lymph
nodes were not involved. The patient did not undergo any adjuvant
therapy. A total-body computed tomography scan was performed every
six months and a colonscopy was performed yearly. No local or
distal recurrence of the lesion was identified following two years
of follow-up. Written informed consent was obtained from the
patient for publication of this study.
Discussion
Schwannomas are rare tumors of ectodermic origin
growing from the neural sheath (2).
In the digestive tract they arise from the autonomous nervous
system; more frequently from Auerbach’s plexus, and less frequently
from Meissner’s plexus. The tumors are usually benign,
slowly-growing neoplasms, although in extremely rare cases they can
present with malignant degeneration if not surgically removed
(1–3). The incidence rate is the identical for
males and females, and increases between the sixth and seventh
decades of life. The stomach and the small bowel are the most
frequently involved sections of the digestive tract (83 and 12%,
respectively) (1).
Macroscopically, schwannomas are lobulated and
well-delimited tumors, often with a cystic pattern.
Neoplasms originating from Auerbach’s plexus
protrude into the intestinal lumen and are characterized by a
non-pedunculated oval-shaped mass, whereas those arising from
Meissner’s plexus are often similar to pedunculated polyps
(4).
Schwannomas are histologically characterized by
Verocay corpuscles, a lymphoid cuff and a spiral-like form
consisting of densely arrayed spindle-shaped cells, palisade
arrangements and loose reticular networks of cells. Two
histological growth patterns have been described: Antoni A (dense
growth of fusiform cells compactly arranged in palisades to form
Verocay bodies) and Antoni B (the fusiform cells are more loosely
distributed with rounded or elongated nuclei, with a great quantity
of myxoid stroma and xanthomatous histiocytes) (1,4).
Schwann cells covering a basal membrane are not generally
identified, however, there may be undifferentiated mesenchymal
cells, smooth muscle cells and cells with neural characteristics or
with mixed differentiation of the neural/muscle type (1).
Although certain studies consider schwannomas to be
a subtype of gastrointestinal stromal tumor (GIST) belonging to the
gastrointestinal autonomic nerve tumors (GANT), there are
significant histopathological and immunohistochemical differences
(2,3). In contrast to GISTs, schwannomas are
consistently negative for CD117 (KIT) and usually negative for
CD34, CKs, smooth muscle actin and desmin, but strongly positive
for S100 protein and vimentin. (1,4,5).
Moreover a lymphoid cuff, diffuse lymphoid infiltration, an
impression of cellular heterogeneity, focal nuclear atypia and a
microtrabecular pattern are not features of GISTs (6).
The precise biological behavior of schwannomas is
not fully understood, mostly due to their rarity. Although they are
considered benign neoplasms, possible malignant behavior must not
be ignored. In fact, Das Gupta and Brasfield reported that in 2% of
cases, distant metastasis may be observed (7). A correct histological diagnosis
requires investigation of the Ki-67 proliferative index (MIB-1), as
its positivity (≥5%) is strictly correlated with greater tumor
aggressiveness. A mitotic activity rate of more than five mitoses
per field at high magnification and a tumor size >5 cm tend to
be associated with a high risk of metastasis and recurrence. A low
rate of mitosis and the absence of atypical mitotic figures and
nuclear hyperpigmentation characterize a benign lesion (1).
Pre-operative biopsy examinations may be difficult,
and immunohistochemistry is necessary for the correct diagnosis of
a schwannoma. Currently, the gold standard treatment for
schwannomas is complete surgical resection with oncological radical
intent. Our experience leads us to suggest that, even if the lymph
nodes are not involved, radical surgery is the best treatment.
Abbreviations:
|
GIST
|
gastrointestinal stromal tumor
|
|
GANT
|
gastrointestinal autonomic nerve
tumor
|
References
|
1
|
Nonose R, Lahan AY, Santos Valenciano J
and Martinez CA: Schwannoma of the colon. Case Rep Gastroenterol.
3:293–299. 2009.
|
|
2
|
Zippi M, Pica R, Scialpi R, Cassieri C,
Avallone EV and Occhigrossi G: Schwannoma of the rectum: A case
report and literature review. World J Clin Cases. 1:49–51.
2013.
|
|
3
|
Fotiadis CI, Kouerinis IA, Papandreou I,
Zografos GC and Agapitos G: Sigmoid schwannoma: a rare case. World
J Gastroenterol. 11:5079–5081. 2005.
|
|
4
|
Tsunoda C, Kato H, Sakamoto T, Yamada R,
Mitsumaru A, et al: A case of benign schwannoma of the transverse
colon with granulation tissue. Case Rep Gastroenterol. 3:116–120.
2009.
|
|
5
|
Braumann C, Guenther N, Menenakos C and
Junghans T: Schwannoma of the colon mimicking carcinoma: a case
report and literature review. Int J Colorectal Dis. 22:1547–8.
2007.
|
|
6
|
Miettinen M, Shekitka KM and Sobin LH:
Schwannomas in the colon and rectum: a clinicopathologic and
immunohistochemical study of 20 cases. Am J Surg Pathol. 25:846–55.
2001.
|
|
7
|
Das Gupta TK and Brasfield RD: Tumors of
peripheral nerve origin: benign and malignant solitary schwannomas.
CA Cancer J Clin. 20:228–233. 1970.
|