Introduction
Leiomyoma is a rare ovarian tumors, which accounts
for 0.5–1% of all benign ovarian tumors (1). They are usually bilateral if they
occur in young patients, however, no bilateral ovarian leiomyoma
has been reported in patients >35 years old. A total of 78% of
ovarian leiomyoma cases are concomitantly observed with uterine
leiomyoma and as hormone stimulation is a cause of uterine
leiomyoma, it was hypothesized that hormone stimulation may also be
a cause of ovarian leiomyoma (2).
It is estimated that ~3% of gravid females present with an adnexal
mass on ultrasound according to data obtained from 6636 pregnant
females from the Department of Obstetrics and Gynecology in Italy
between January 1996 and December 1999 (3). Surgery must be considered when the
patient develops symptoms, such as abdominal pain or an ovarian
cyst, or if the ovarian cyst is >6 cm in diameter, as this
presents a risk to the continuing pregnancy (4). Few adnexal masses during pregnancy
exhibit rapid growth with the progression of pregnancy. The current
study presents the case of a 28-year-old female with an ovarian
mass, which showed rapid growth during early pregnancy. The mass
was excised by laparoscopy during the 12th week of gestation,
without complications, when the mass had reached ~18×16×10 cm. The
final postoperative histopathological examination confirmed primary
ovarian leiomyoma. To the best of our knowledge, the management of
large primary ovarian leiomyoma by laparoscopy during pregnancy has
not been reported to date. Written informed consent was obtained
from the patient.
Case report
Patient presentation
In October 2012, a 28-year-old female was referred
to the local hospital due to two missed menstrual periods one month
previously. Abdominal ultrasonography revealed a single normal
fetus in the uterus and a right adnexal hypoechoic solid mass of
4.1×3.2 cm in size. The mass had been identified three years
previously with a diameter of 2.5 cm during a routine gynecological
check up and was followed-up by an ultrasound scan every six months
for three years, which showed that the size of mass had remained
stable. No further measurements were recorded due to the stability
of the mass for a long period of time, without related symptoms.
However, 16 days following the initial visit, the patient presented
to the local hospital once again with a complaint of acute right
lower abdominal pain following activity. An emergency ultrasound
examination revealed that the adnexal mass had increased to 7×6.5
cm in size, without characteristics of torsion or rupture. The pain
was significantly alleviated 1 h later without any therapy. Due to
the increasing size of mass and the presence of pain, the patient
was referred to Zhejiang Provincial People’s Hospital (Hangzhou,
China) for surgical intervention.
During the following days, mild intermittent
abdominal pain was experienced, without fever, vomiting, vaginal
bleeding or uterine contractions. Approximately one week later the
patient was admitted to Zhejiang Provincial People’s Hospital
(Hangzhou, China) with slight abdominal pain on the right side.
Physical examination revealed a tender mass of ~11×10 cm in size,
located in the right upper abdominal quadrant region. The mass was
palpable and movable, with clear edges. During the pelvic
examination, the cervix was normal and no amniotic fluid or bloody
discharge was observed. The uterus was movable with no tenderness,
and was of the size corresponding to the gestational age.
Ultrasound revealed a single live fetus and a
partial cystic adnexal mass of 10.4×10×6.6 cm in size (Fig. 1).
Treatment
Surgery was scheduled to remove the mass one week
later. The patient underwent laparoscopic ovarian tumorectomy under
endotracheal intubation and general anesthesia. During the surgery,
basic vital signs, including oxygen saturation and the end-tidal
carbon dioxide level of the patient, were monitored continuously by
the anesthetist. The laparoscope revealed an enlarged uterus of the
size corresponding to that expected for a three-month pregnant
uterus, normal bilateral fallopian tubes and a normal left ovary. A
mass arising from the right ovary was ~18×16×10 cm in size and
grossly appeared solid, with smooth/shiny surfaces and marked
superficial vascularity. No adhesion or infiltration was observed
in the pelvis. The ovary was preserved and the mass was excised.
Following the completion of tumor enucleation, the ovarian defect
was sutured with 2–0 absorbable VICRYL suture (Johnson &
Johnson Medical Ltd., New Brunswick, NJ, USA) in a continuous
manner, while bipolar electrocoagulation was used to secure
hemostasis. The samples were removed using the bag-retrieval
technique, where a 35×25 cm bag was used to remove the mass through
the extended left trocar incision, and were subsequently sent to
the Department of Pathology (Zhejiang Provincial People’s Hospital)
for histological testing. The examination of frozen sections
reported a benign spindle cell tumor with focal ischemic
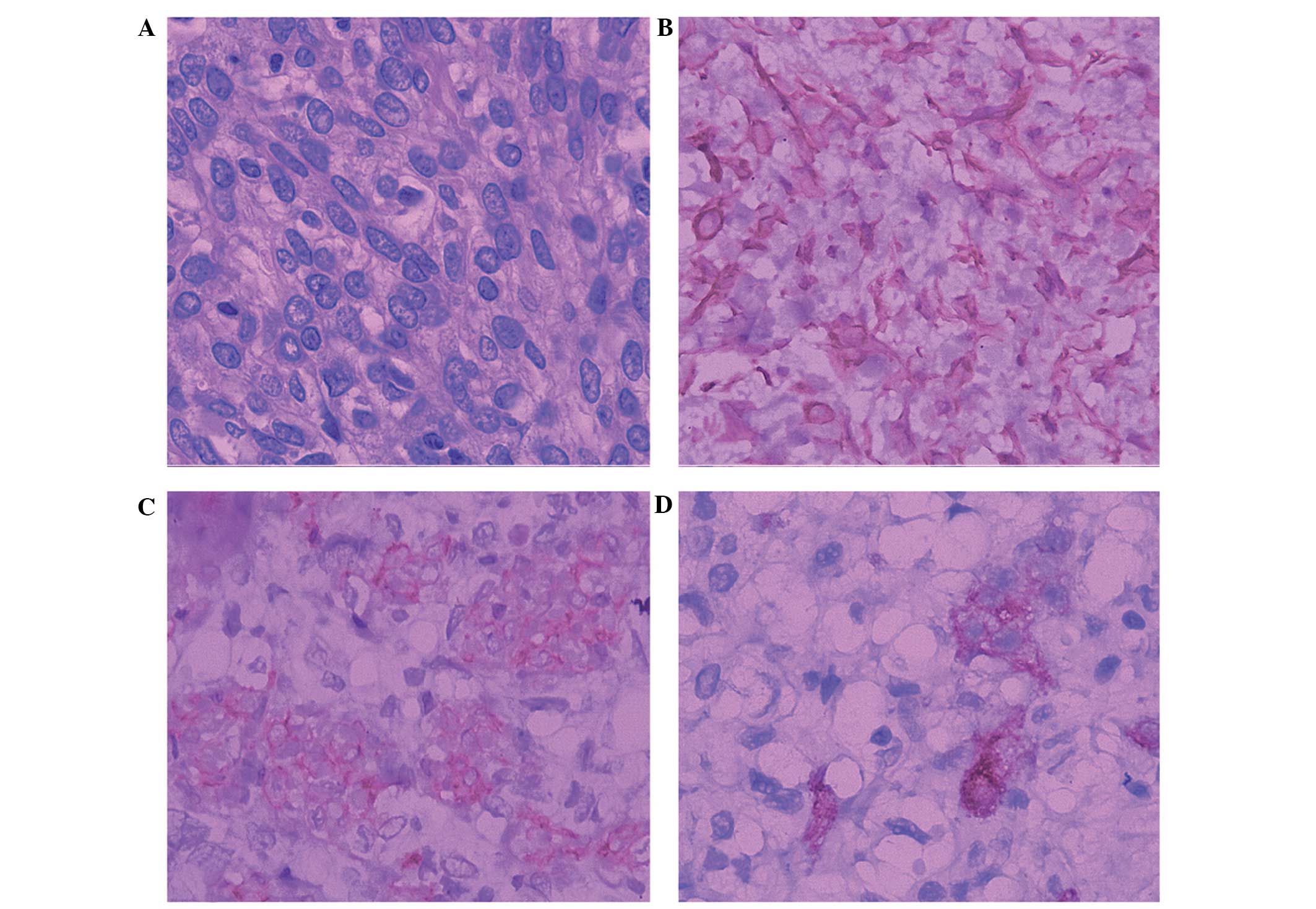
infarction. Pathological examination of the paraffin section
following surgery demonstrated that the mass was comprised of
typical smooth muscle cells, which formed strands and bundles
arranged in a whorled interlacing pattern. Microscopically,
ischemic infarction focus of the mass was observed, while
significant nuclear atypia or pleomorphism was absent.
Immunohistochemical staining with antibodies against vimentin,
inhibin, α-smooth muscle actin and the α-helical rod domain of
desmin was performed to confirm the diagnosis of this rare tumor.
The tumor cells stained positively for vimentin, inhibin and
α-smooth muscle actin, but not for the α-helical rod domain of
desmin, which aided in confirming the diagnosis of ovarian
leiomyoma (Fig. 2).
Follow up
Fetal surveillance monitoring via ultrasound prior
to and following surgery indicated that the surgery had been
successful. Prophylactic antibiotics and progesterone at a dose of
20 mg twice daily for four days were prescribed following surgery
to prevent miscarriage. The surgery time, defined as the period
between the skin incision and the closure of the skin, was 118
minutes and the estimated blood loss was 800 ml. The patient
experienced an uneventful postoperative recovery. Routine follow-up
after discharge was conducted every six months for three years and
no complications were observed. A 3.4-kg healthy baby was delivered
spontaneously at full term.
Discussion
Due to the widespread use of routine ultrasound in
maternity examinations, it has been reported that the incidence of
adnexal masses in pregnant females is ~3%, of which 55% may
spontaneously resolve completely or significantly decrease in size
(5). It is difficult to determine
the treatment of adnexal masses in pregnancy, as surgery may pose a
risk to the mother and fetus (6),
but conservative management may result in severe complications,
including torsion or rupture of the ovarian masses. However, there
is no controversy with surgical intervention for pregnant females
with symptoms of acute abdominal pain or adnexal mass larger than 6
cm in diameter (4).
The first case of a primary ovarian fibroid was
described in 1862 (7,8), <100 cases of this rare tumor have
since been reported (7,8). Clinically, few patients present with
symptoms, and the majority of tumors are identified incidentally
and are only a few millimeters in diameter (2,7).
However, various characteristics of these benign neoplasms have
been reported, including a variety of clinical presentations, such
as abdominal pain, a palpable mass, marginal elevation in tumor
marker levels and the complication of Meigs syndrome (8,9,10), as
well as a wide range of tumor sizes. Lim and Jeon (8) described a case of large bilateral
ovarian leiomyoma in a 17-year-old female in 2004, where the left
ovary measured 17×10×7 cm and the right ovary measured 14×11×9 cm
at their greatest dimensions. Similarly, Safaei et al
(11) reported the case of a
54-year-old postmenopausal multipara female with an ovarian
leiomyoma measuring 16×13×10 cm in size, in 2011. Furthermore, a
study investigating uterine leiomyoma revealed that 15–30% of
leiomyomas tend to grow under the influence of estrogens during
pregnancy (12). Wei et al
(8) suggested that estrogens may be
a significant factor in the development of these ovarian neoplasms.
A number of ovarian leiomyomas in pregnant females have been noted.
Zorlu et al (13) presented
the case of an adnexal mass complicating pregnancy, which was
diagnosed as ovarian leiomyoma following surgery. The patient
underwent surgery following spontaneous delivery, as there were no
prior complaints with regard to the mass. In the case reported by
Hsiao et al (14), the
patient received an emergency cesarean section and oophorectomy due
to an ovarian leiomyoma. The authors also drew the conclusion that
increased concentrations of the progesterone and estrogen hormones
during pregnancy may have been a factor in stimulating the growth
of these tumors. Kohno et al (15) reported the case of a 32-year-old
female who had a large pelvic mass, with rapid growth noted at the
16th week of gestation. An adnexal tumorectomy was performed on the
patient by laparotomy at the 20th week of gestation, and the
patient gave birth to a female infant at the 40th week of
gestation. However, no recent studies have discussed the excision
of an ovarian leiomyoma by laparoscopy during pregnancy. The case
presented in the current study is of interest due to the rarity of
this disease and the successful laparoscopic approach to remove the
enlarged mass of the ovary during pregnancy.
We hypothesize that surgery is not to be considered
for adnexal tumors of <3 cm in diameter during pregnancy. In the
case presented in the current study, an adnexal tumor was observed
in the patient, which had remained at ~2.5 cm in diameter for three
years prior to gestation. However, the patient presented with
symptoms of abdominal pain and rapid tumor growth during pregnancy,
which suggested that surgical intervention prior to the birth
should be considered for solid tumors identified before or during
gestation, even for those <3 cm in diameter, in order to avoid
complications during pregnancy.
Numerous studies have reported that a laparoscopic
approach to the removal of ovarian masses provides benefits,
including an improved view of the surgical site, reduced blood
loss, fewer adhesions, decreased postoperative pain, shorter
hospitalization and smaller scars, compared with transabdominal
surgery. These advantages are particularly significant for gravid
females. A laparoscopic approach for the management of benign
ovarian tumors in pregnant females has become the preferred
approach by surgeons, due to its efficacy and safety (16). Potential concerns with regard to
laparoscopic surgery in pregnancy include a limited surgical field,
trauma to the gravid uterus due to trocar penetration, and the
negative effect on the fetus of CO2 gas pneumoperitoneum
(17). The patient discussed in the
current study was in the early second trimester of pregnancy, at
which stage the uterus may not be of as much concern when placing
the laparoscopic ports. Additionally, the correlation between
CO2 abdominal insufflation and increased intraoperative
complications during pregnancy has not been investigated to date.
This case supports the previously observed safety and feasibility
of laparoscopic approach in pregnancy.
The predominant challenges of laparoscopic
tumorectomy of solid large ovary tumors during pregnancy are
enucleation of the tumor and removal of the mass from the abdominal
cavity, particularly when the mass exists in marked vascularity.
During the surgical enucleation of large tumors with marked
vascularity, bipolar and monopolar cautery, as well as ultrasonic
scalpel devices were used to control bleeding, all of which were
deemed entirely profitless exercises for the patient in the present
case. Therefore, in this case, the tumor was enucleated and the
residual ovary tissue was sutured rapidly for hemostasis, based on
a skillful laparoscopic technique. However, ~800 ml of operative
blood loss was observed. Temporary ligation of the ovarian pedicle,
the proper ligament and the suspensory ligament may be promising in
reducing operative blood loss; however, this approach was
considered in this surgery. An additional challenge is the integral
extraction of the solid tumor. Although the morcellation technique
is prevalent in laparoscopic surgery for solid tumors, an endobag
remains a necessity when removing the tumor, in order to minimize
the probability of the diffusion and implantation of the tumor
cells. During the surgery in the current case, the entire sample
was enveloped in a 30×35-cm medical endobag, and removed via the
trocar incision at the left anterior axillary line, which was
extended to 3 cm following the initial scalpel incision.
In conclusion, to the best of our knowledge, no
studies have investigated the laparoscopic management of primary
ovarian leiomyomas during pregnancy. The case presented in the
current study demonstrates that symptomatic ovarian leiomyoma may
be successfully managed without complications by laparoscopic
surgery, even when large in size and during pregnancy. By contrast,
when considering solid progestational tumors, operative therapy
prior to gestation is advised, even for tumors <3 cm in
diameter, due to the probability of rapid growth of the tumor
during pregnancy.
References
|
1
|
Tomas D, Lenicek T, Tuckar N, et al:
Primary ovarian leiomyoma associated with endometriotic cyst
presenting with symptoms of acute appendicitis: a case report.
Diagn Pathol. 4:252009.
|
|
2
|
Lim SC and Jeon HJ: Bilateral primary
ovarian leiomyoma in a young woman: case report and literature
review. Gynecol Oncol. 95:733–735. 2004.
|
|
3
|
Nelson MJ, Cavalieri R, Graham D and
Sanders RC: Cysts in pregnancy discovered by sonography. J Clin
Ultrasound. 14:509–512. 1986.
|
|
4
|
Roberts JA: Management of gynecologic
tumors during pregnancy. Clin Perinatol. 10:369–382. 1983.
|
|
5
|
Zanetta G, Mariani E, Lissoni A, Ceruti P,
Trio D, Strobelt N and Mariani S: A prospective study of the role
of ultrasound in the management of adnexal masses in pregnancy.
BJOG. 110:578–583. 2003.
|
|
6
|
Shnider SM and Webster GM: Maternal and
fetal hazards of surgery during pregnancy. Am J Obstet Gynecol.
92:891–900. 1965.
|
|
7
|
Kobayashi Y, Murakami R, Sugizaki K, et
al: Primary leiomyoma of the ovary: a case report. Eur Radiol.
8:1444–1446. 1998.
|
|
8
|
Wei C, Lilic N, Shorter N and Garrow E:
Primary ovarian leiomyoma: a rare cause of ovarian tumor in
adolescence. J Pediatr Adolesc Gynecol. 21:33–36. 2008.
|
|
9
|
Khaffaf N, Khaffaf H and Wuketich S: Giant
ovarian leiomyoma as a rare cause of acute abdomen and
hydronephrosis. Obstet Gynecol. 87:872–873. 1996.
|
|
10
|
Vierhout ME, Pijpers L, Tham MN and
Chadha-Ajwani S: Leiomyoma of the ovary. Acta Obstet Gynecol Scand.
69:445–447. 1990.
|
|
11
|
Safaei A, Khanlari M, Azarpira N and
Monabati A: Large ovarian leiomyoma in a postmenopausal woman.
Indian J Pathol Microbiol. 54:413–414. 2011.
|
|
12
|
Stewart EA: Uterine fibroids. Lancet.
357:293–298. 2001.
|
|
13
|
Zorlu CG, Cengiz S and Harmanlí HO:
Primary ovarian leiomyoma. A case report. Gynecol Obstet Invest.
36:191–192. 1993.
|
|
14
|
Hsiao CH, Wang HC and Chang SL: Ovarian
leiomyoma in a pregnant woman. Taiwan J Obstet Gynecol. 46:311–313.
2007.
|
|
15
|
Kohno A, Yoshikawa W, Yunoki M, Yanagida T
and Fukunaga S: MR findings in degenerated ovarian leiomyoma. Br J
Radiol. 72:1213–1215. 1999.
|
|
16
|
Balthazar U, Steiner AZ, Boggess JF and
Gehrig PA: Management of a persistent adnexal mass in pregnancy:
what is the ideal surgical approach? J Minim Invasive Gynecol.
18:720–725. 2011.
|
|
17
|
Soriano D, Yefet Y, Seidman DS, Goldenberg
M, Mashiach S and Oelsner G: Laparoscopy versus laparotomy in the
management of adnexal masses during pregnancy. Fertil Steril.
71:955–960. 1999.
|