Introduction
Non-Hodgkin lymphomas (NHLs) are a large group of
cancers of lymphocytes. NHL can occur at any age and is often
marked by lymph nodes that are larger than normal, fever and weight
loss (1). Primary involvement of
the larynx in NHL is rare, accounting for <1% of all laryngeal
tumors, worldwide (2). To the best
of our knowledge, <100 cases of primary laryngeal NHL have been
reported, worldwide. In these cases, the most common site of
involvement was the supraglottic region. Involvement of the glottis
and subglottic region were rarely reported and cases with diffuse
involvement of the whole larynx were extremely rare (2). The standard first-line chemotherapy
regimens for the majority of cases of aggressive NHL include
cyclophosphamide, doxorubicin, vincristine and prednisolone.
Although the majority of NHL patients are responsive to the initial
chemotherapy, 40–60% of patients do not achieve a complete response
following first-line chemotherapy (3).
In the present study, the case of a 52 year-old male
with hoarseness due to diffuse T-cell lymphoma as the first
manifestation of precursor T-cell acute lymphoblastic leukemia
(T-ALL) is presented. Written informed consent was obtained from
the patient.
Case report
In August 2010, a 52-year-old male was admitted to
Huashan Hospital, Fudan University (Shanghai, China) due to
progressive hoarseness subsequent to overuse of the larynx ten
months previously. Laryngoscopy had been performed at another
hospital in December 2009, which revealed chronic swollen
congestive vocal cords with a smooth surface. Computed tomography
(CT) scan and blood tests revealed normal results. The patient was
subsequently diagnosed with laryngitis. However, anti-inflammatory
therapy did not improve the patient’s symptoms. Two months later,
the patient underwent an additional laryngoscopy and biopsy. The
laryngoscopy revealed swollen laryngeal ventricles and false vocal
cords. The pathology of the laryngeal ventricles demonstrated
chronic mucositis with diffuse infiltration of lymphoid tissue. The
patient was diagnosed with chronic laryngitis, however, subsequent
treatment with antibiotics did not alleviate the patient’s
symptoms. In June 2010, routine blood tests revealed a red blood
cell (RBC) count of 4.19×1012/l (normal range,
4.32–5.72×1012/l), a hemoglobin (Hb) level of 122 g/l
(normal range, 135–175 g/l), a white blood cell (WBC) count of
11.6×109/l (normal range, 4–10×109/l) and a
platelet (PLT) count of 119×109/l (normal range,
100–300×109/l). Additionally, the neutrophil granulocyte
and lymphocyte percentages were identified to be abnormally low
(20%) and abnormally high (78%), respectively, indicating
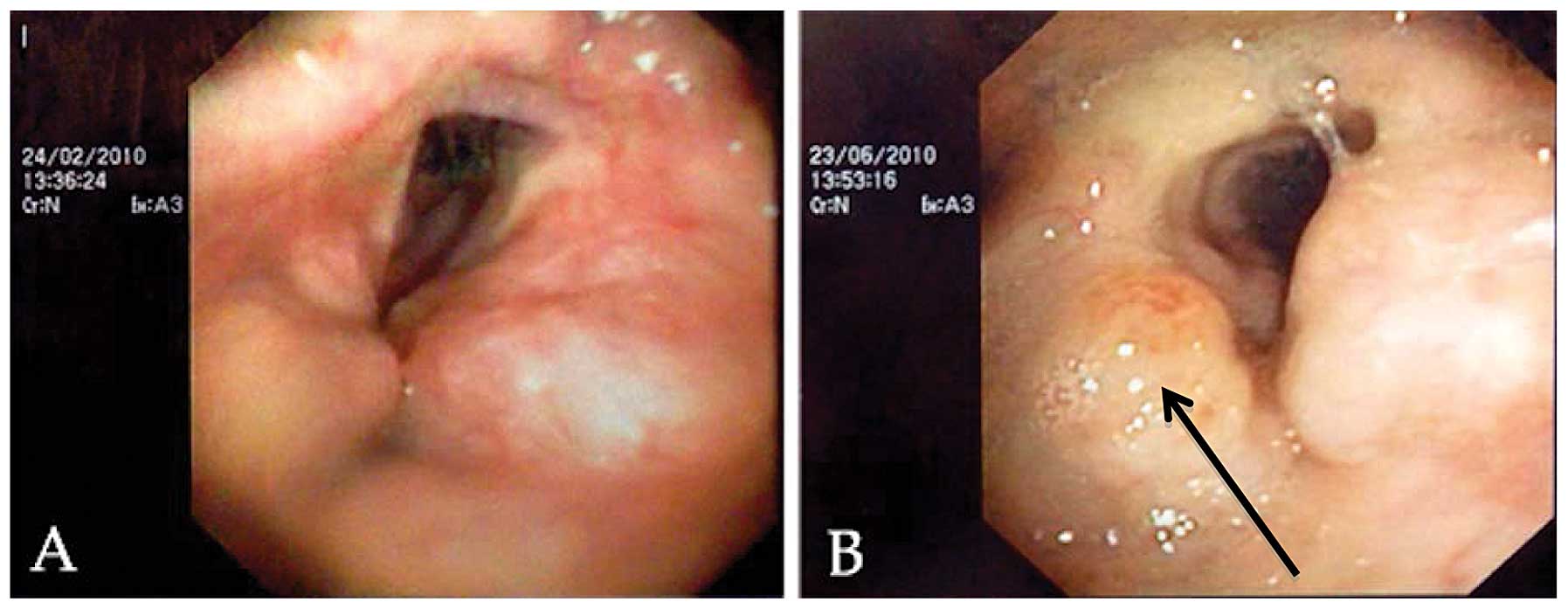
hematologic abnormality. The hoarseness worsened and thus,
endoscopy was performed, which revealed neoplasms in the two
ventricles of the larynx (Fig. 1).
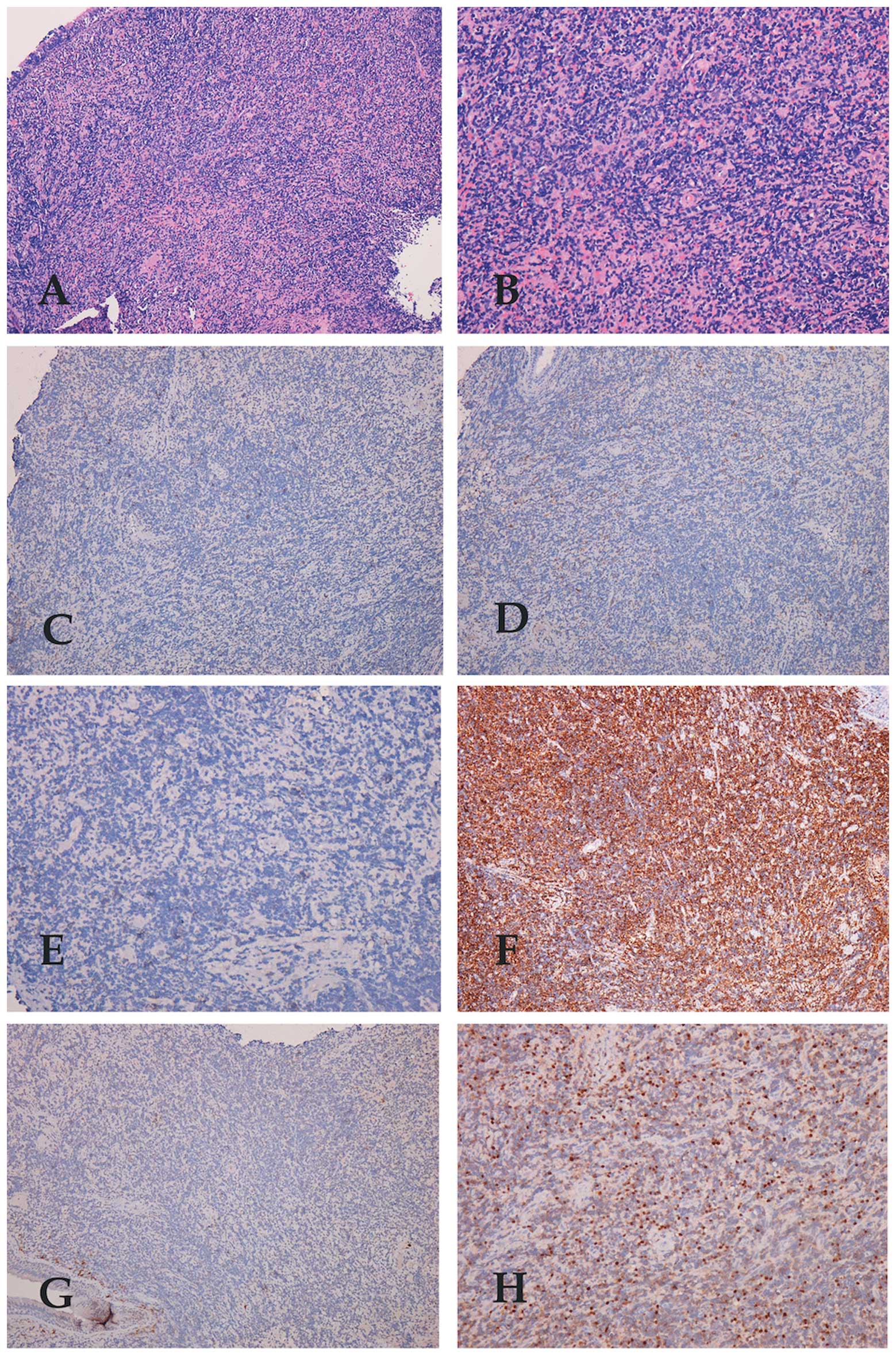
Pathology of biopsy specimens obtained from the ventricular bands
revealed neoplastic transformation of the lymphoid tissue.
Immunohistochemistry revealed the cells to be positive for
leukocyte common antigen, lysosome-associated glycoprotein cluster
of differentiation (CD)68, CD3, terminal deoxynucleotidyl
transferase and CD43 and negative for L26, CD79, CD56, granzyme B,
perforin, latent membrane protein-1, Vimentin, CD5, CD10, CD23 and
cytokeratin (Fig. 2). A CT scan of
the neck revealed hyperplasia of the soft tissues in the
supraglottic, glottis and subglottic regions. Three groups of lymph
nodes in the submaxillary region were also involved.
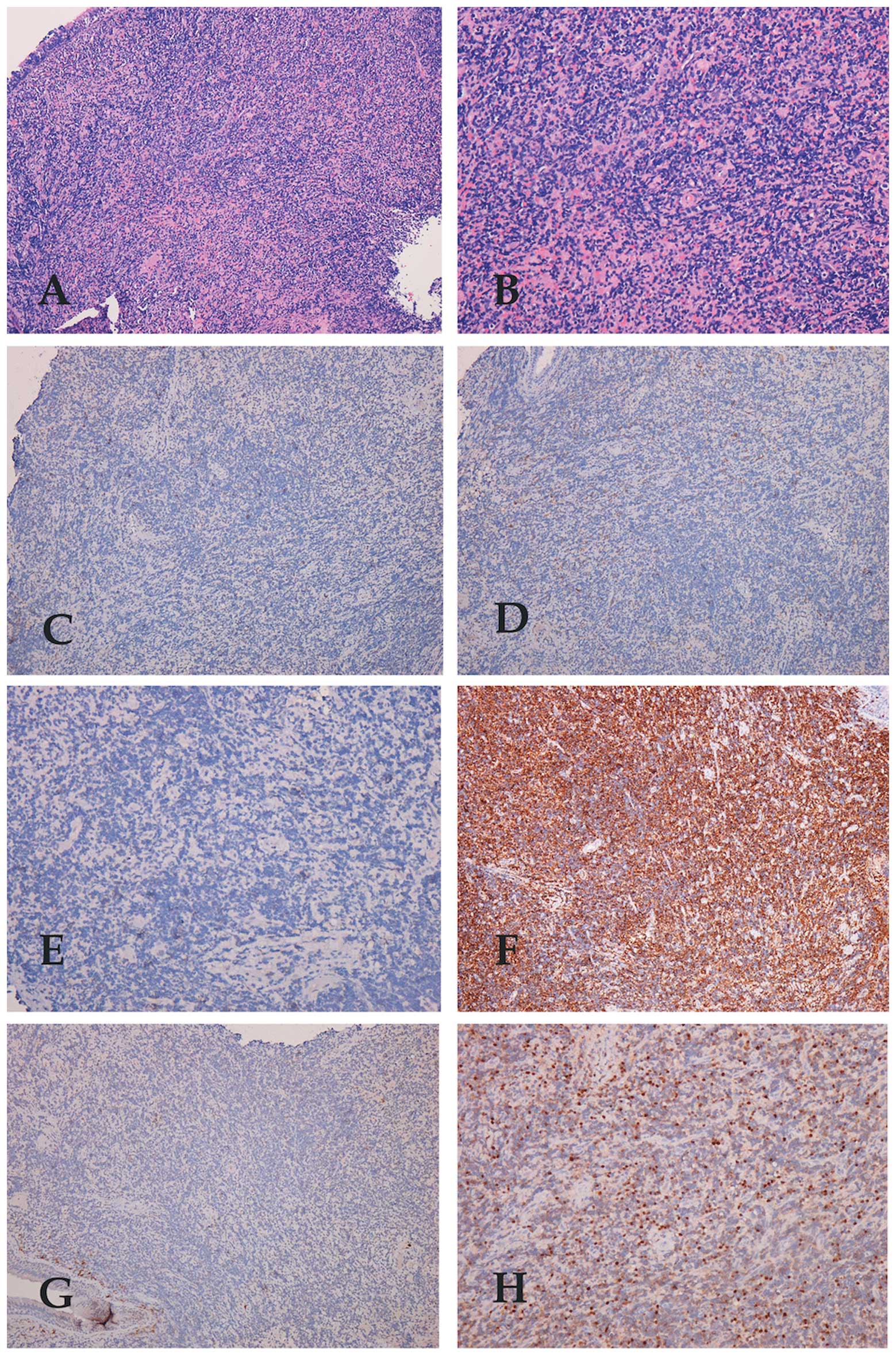 | Figure 2Immunohistochemical staining revealed
(A) laryngeal mucosa with diffuse lymphocytic infiltration (stain,
HE; magnification, ×40), and (B) lymphoepithelial lesions (stain,
HE; magnification, ×100). Neoplastic lymphoid cells were negative
for (C) CD5 (stain, HE; magnification, ×40), (D) CD10 (stain, HE;
magnification, ×40) and (E) CD23 (stain, HE; magnification, ×100),
positive for (F) CD43 (stain, HE; magnification, ×40), negative for
(G) CD79 (stain, HE; magnification, ×40) and positive for (H)
terminal deoxynucleotidyl transferase (stain, HE; magnification,
×100). HE, hematoxylin and eosin. |
In August 2010, the patient presented to the
Department of Hematology, Huashan Hospital, Fudan University.
Physical examination revealed lymphadenopathy and splenomegaly.
Furthermore, blood tests revealed a RBC count of
3.55×1012/l, Hb level of 107 g/l, WBC count of
27.85×109/l and PLT level of 110×109/l, as
well as an abnormally low percentage (13%) of neutrophil
granulocytes and an abnormally high percentage (84%) of
lymphocytes, indicating hematologic abnormality. A number of basket
cells were also observed under the microscope (CX31-P; Olympus,
Tokyo, Japan). In addition, a CT scan of the chest, abdomen and
pelvis demonstrated superior mediastinum lymph node involvement. A
bone marrow smear and biopsy indicated acute lymphoblastic
leukemia, with 83.5% blasts. Immunophenotype analysis, which was
determined by flow cytometry, revealed that precursor T cells
accounted for 92% of the bone marrow total cell count and 85% of
the peripheral blood cell count, indicating a definitive diagnosis
of precursor T-cell ALL. The patient was administered with the VDCP
chemotherapy regimen (2 mg vincristine, days 1,8,15 and 22; 60 mg
daunorubicin, days 1–3 and 15–17; 1.0 g cyclophosphamide, days 1
and 15; 50 mg prednisolone, days 1–14). The patient experienced
tachycardia after three days. Considering daunorubicin can
interfere with the pumping action of the heart, epirubicin was
administered instead of daunorubicin. Remission was not achieved
after the first cycle of chemotherapy. The second chemotherapeutic
regimen administered was EA (150 mg etoposide, days 1–4; 150 mg
cytosine arabinoside, days 1–7). Three cycles of EA chemotherapy
resulted in 17.5% blasts in the bone marrow. L-asparaginase was
administered in the fourth EA regimen, which resulted in remission
with blasts comprising 3% of the bone marrow. Laryngoscopy and CT
scan were performed. No tumor tissue was identified in the larynx
and the mediastinum involvement was also resolved. The patient then
received six courses of consolidation therapy, including the EA +
L-asparaginase (10,000 units L-asparginase, days 3 and 4) regimen
and a high dose of methotrexate (3 g, day 1). At present, the
patient remains disease free at the tumor site and lymph nodes.
Discussion
Primary NHL of the larynx is rare. The age of onset
for laryngeal lymphoma varies between four and 81 years, and
previous studies have reported a male predominance (4). Patients with laryngeal NHLs usually
present with progressive hoarseness, cough, stridor, dysphagia, a
feeling of a foreign body and dyspnea. Early symptoms are
nonspecific and thus, it is difficult to confirm the diagnosis. The
main mass of the tumor is predominantly located in the supraglottic
region, which contains lymphoid tissue in the lamina propria and
ventricles. In certain cases, lymphoma may affect the glottis,
however, the majority of cases occur in the subglottic or
transglottic regions (2). The
majority of tumors appear as a localized polyploidy sub-mucosal and
nonulcerated swelling on endoscopy. CT scan or magnetic resonance
imaging may aid assessment. Pathological and immunohistochemical
analysis revealed plasmacytoma, mucosa-associated lymphoid
tissue-lymphoma and diffuse large B-cell lymphoma to be the most
common subtypes of NHL involving the larynx (5). T-cell laryngeal lymphoma is much less
common than B-cell lymphoma (6).
However, at the time of diagnosis, the majority of
patients already exhibit bone marrow or peripheral blood
involvement, as well as mediastinal masses, lymphadenopathy and
organomegaly. Uyttebroeck et al (7) reported that T-ALL and T-lymphoblastic
lymphoma (T-LBL) represent precursor T-cell malignancies that
reflect the various stages of T-cell development. A percentage of
blasts >25% of total cells in the bone marrow differentiates
acute lymphoblastic leukemia from lymphoblastic lymphoma (6). In the present case, precursor T cells
accounted for 92% of the bone marrow of the patient and thus, T-ALL
was diagnosed. T-ALL in adults is rare, accounting for ~25% of all
adult ALL cases and it is more common in males than females. In the
present study, the tumor cells were positive for CD3 and thus,
according to the World Health Organization (WHO) classification of
lymphoid neoplasms guidelines (8),
the immunological subtype was diagnosed as T-IV (positive for
surface CD3 and negative for CD1a, irrespective of other
markers).
Treatments for T-ALL and T-LBL are different. It has
been suggested that laryngeal T-LBL should be managed as a rare
presentation of NHL. Radiotherapy and chemotherapy are the most
common therapeutic strategies used for the treatment of primary
laryngeal lymphomas. Surgery may be essential as the first line
treatment if laryngeal obstruction or massive hemorrhage is
identified (4). Kovac et al
(6) reported a female patient with
subglottic T-cell lymphoma as the only manifestation of precursor
T-cell acute lymphoblastic leukemia. The patient underwent one
cycle of chemotherapy with cyclophosphamide, doxorubicin,
vincristine and prednisone, however, remission was not achieved.
High doses of cytarabine (3 g) and mitoxantrone (15 mg) resulted in
remission. The patient succumbed to an infection prior to auto
transplantation surgery. In the present case, the patient did not
respond to the first cycle of VDCP chemotherapy and thus, the
regimen was changed. Following three cycles of the EA regimen and
one cycle of the EA+L-asp regimen, precursor T cells accounted for
3% of the bone marrow of the patient. Laryngoscopy revealed
complete remission of the tumor. Six consolidation therapy courses
were performed subsequently. At present, the patient remains
disease free, which indicates that the EA+L-asp regimen and
treatment with a high dose of methotrexate are appropriate
treatments for T-ALL.
To the best of our knowledge, this is the first
report of a case of precursor T-cell lymphoblastic leukemia
manifesting as diffuse involvement of the whole larynx. In summary,
the symptoms during the early stage of the disease are subtle and
non-specific and thus, diagnosis is difficult to establish. A
number of deep biopsies, bone marrow biopsies and flow cytometry
analysis are required to distinguish the tumor from inflammatory
cells.
Primary involvement of the larynx in NHL is rare,
accounting for <1% of all laryngeal tumors. The symptoms in the
early stage are subtle and nonspecific and thus, diagnosis is
difficult to establish. In the present study, a male patient with
hoarseness due to diffuse T-cell lymphoma as the first
manifestation of precursor T-ALL was reported. Following three
cycles of the EA regimen and one cycle of the EA+L-asp regimen, the
patient achieved complete remission. A series of consolidation
therapy cycles were performed subsequently. At present, the patient
remains disease-free, indicating that this treatment was
effective.
In conclusion, clinical features are important in
diagnosis. However, similar onset manifestations may be caused by
different diseases. In this report, the onset clinical
manifestation was hoarseness, which is often observed in patients
with laryngeal tumors. In this case, based on the results of bone
marrow biopsy and immunophenotype analysis, which revealed abnormal
high percentages of precursor T cells, the diagnosis was precursor
T-cell acute lymphoblastic leukemia, according to the 2008 WHO
classification of lymphoid neoplasms (8).
Acknowledgements
This study was supported by grants from the China
National Natural Science foundation (grant no. 81070404 and
81100340) and the Ministry of Education fundation (grant no.
20110071120068).
References
|
1
|
Laurini JA, Perry AM, Boilesen E, et al:
Classification of non-Hodgkin lymphoma in Central and South
America: a review of 1028 cases. Blood. 120:4795–4801. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
King AD, Yuen EH, Lei KI, Ahuja AT and Van
Hasselt A: Non-Hodgkin Lymphoma of the larynx: CT and MR imaging
findings. AJNR Am J Neuroadiol. 25:12–15. 2004.
|
|
3
|
Lin X, Shi X, Zeng W, Zheng M and Huang L:
Salvage therapy with mitoxantrone, etoposide, bleomycin and
dexamethasone for refractory or relapsed aggressive non-Hodgkin’s
lymphoma patients with a poor performance status or comorbidity.
Oncol Lett. 8:2012–2016. 2014.PubMed/NCBI
|
|
4
|
Markou K, Goudakos J, Constantinidis J, et
al: Primary laryngeal lymphoma: report of 3 cases and review of the
literature. Head Neck. 32:541–549. 2010.
|
|
5
|
Vega F, Lin P and Medeiros LJ: Extranodal
lymphomas of the head and neck. Ann Diagn Pathol. 9:340–350. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kovac L, Bilić M, Bumber B and Topić I:
Primary laryngeal manifestation in precursor T-cell acute
lymphoblastic leukemia. Otolaryngol Head Neck Surg. 139:474–475.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Uyttebroeck A, Vanhentenrijk V, Hagemeijer
A, et al: Is there a difference in childhood T-cell acute
lymphoblastic leukaemia and T-cell lymphoblastic lymphoma? Leuk
Lymphoma. 48:1745–1754. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Campo E, Swerdlow SH, Harris NL, Pileri S,
Stein H and Jaffe ES: The 2008 WHO classification of lymphoid
neoplasms and beyond: evolving concepts and practical applications.
Blood. 117:5019–5032. 2011. View Article : Google Scholar : PubMed/NCBI
|