Introduction
Primary malignant lymphomas of the prostate are
rare, and the majority are reported as single cases. The tumors
account for 0.09% of all prostate neoplasms and 0.1% of all
non-Hodgkin’s lymphomas (NHLs) (1).
Non-Hodgkin’s lymphoma is the major histological subtype of primary
Hodgkin’s lymphoma (PHL) and diffuse large B-cell lymphoma (DLBCL)
is the most common type of NHL. As primary lymphoma of the prostate
is rare, at present there is no consensus regarding its optimal
management, however, current treatment modalities include
chemotherapy, radiotherapy and radical prostatectomy. Advanced
pelvic urological malignancies are the most common cause of
intractable haematuria (2–4). Blood loss as a result of intractable
haematuria is often severe and the condition of the patient is
generally poor and thus, to avoid the additional risk associated
with surgical intervention, selective transarterial embolization of
the internal iliac arteries has been found to be safe and highly
effective for patients with severe bladder and prostatic
haemorrhage (2,4). The current study presents the case of
a 75-year-old male with prostatic DLBCL and intractable hematuria,
which was successfully controlled by a low dose of rituximab
combined with cyclophosphamide, doxorubicin, vincristine and
prednisone (R-CHOP), and bilateral selective iliac arterial
chemoembolization. Written informed consent was obtained from the
patient.
Case report
A 75-year-old male was admitted to the Department of
Urology in the Second Xiangya Hospital (Central South University,
Changsha, Hunan, China) due to difficulty in urinating, with a
one-year history of urinary obstruction and a 10-day history of
gross hematuria. A physical examination revealed hypertrophy of the
prostate, and disappearance of the median sulcus. There was no
palpable enlargement of the superficial lymph nodes and no
hepatosplenomegaly.
Laboratory findings, including blood count, and
liver and renal function, were all normal. Chest X-rays revealed no
abnormalities. Computed tomography (CT) showed no evidence of
distant metastasis to the lungs or abdomen. The concentrations of
tumor markers, including α-fetoprotein, carcinoembryonic antigen
and prostate-specific antigen (PSA), were within normal limits. The
level of serum lactate dehydrogenase (LDH) was elevated to 375.4
U/l (normal range, 104.0–245.0 U/l) and the concentration of
β2-microglobulin was 3.89 mg/l (normal range, 0.80–2.40 mg/l).
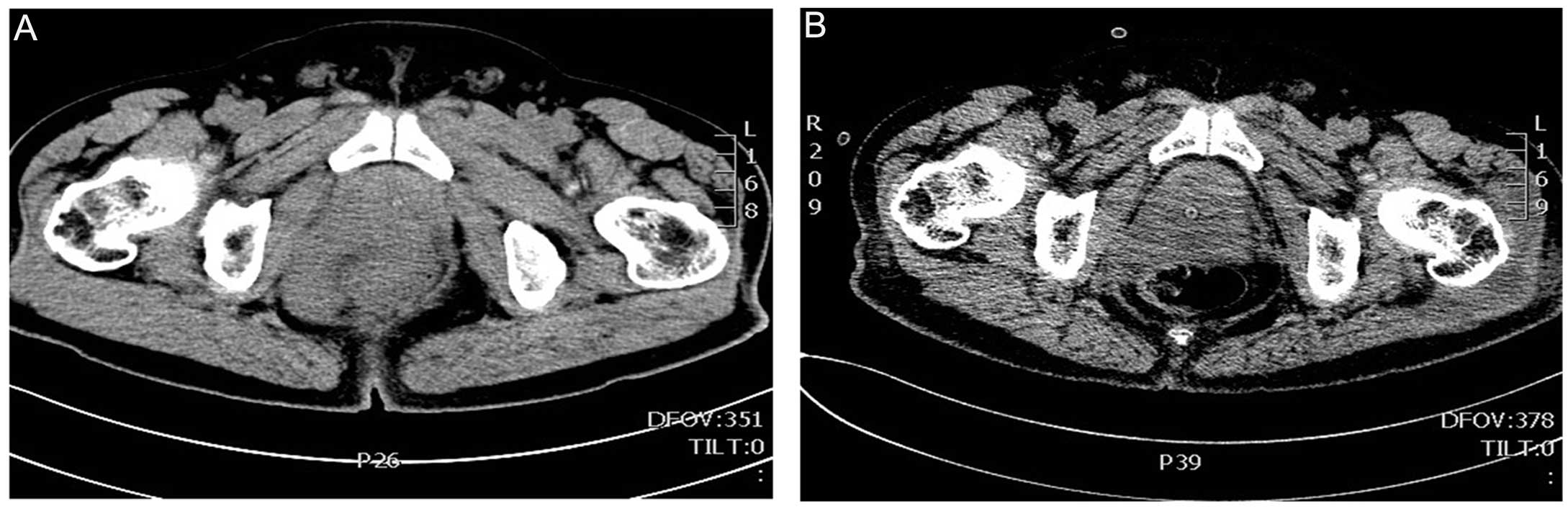
Ultrasound (US) of the prostate revealed large
masses measuring 93×79 mm. A pelvic CT scan (Fig. 1A) showed multiple low-density
masses, with unclear boundaries with the bladder, prostate and
rectum. Three enlarged lymph nodes were observed on the right side
of the pelvis, with diameters of 3.5 cm each. The findings met the
diagnostic criteria of lymphoma. A bone marrow biopsy showed no
abnormalities. Due to significant bleeding, a Foley catheter was
inserted and continuous bladder irrigation was commenced. The use
of antibiotics and a blood transfusion yielded unsatisfactory
results. Due to the rapid loss of blood, the blood pressure
decreased resulting in shock and the hemoglobin level decreased to
55 g/l. A bilateral iliac arteriography and chemoembolization (40
mg pirarubicin and 2 mg vincristine) were performed as emergency
procedures under local anesthesia (Fig.
2). The duration of surgery was 45 min and the bleeding was
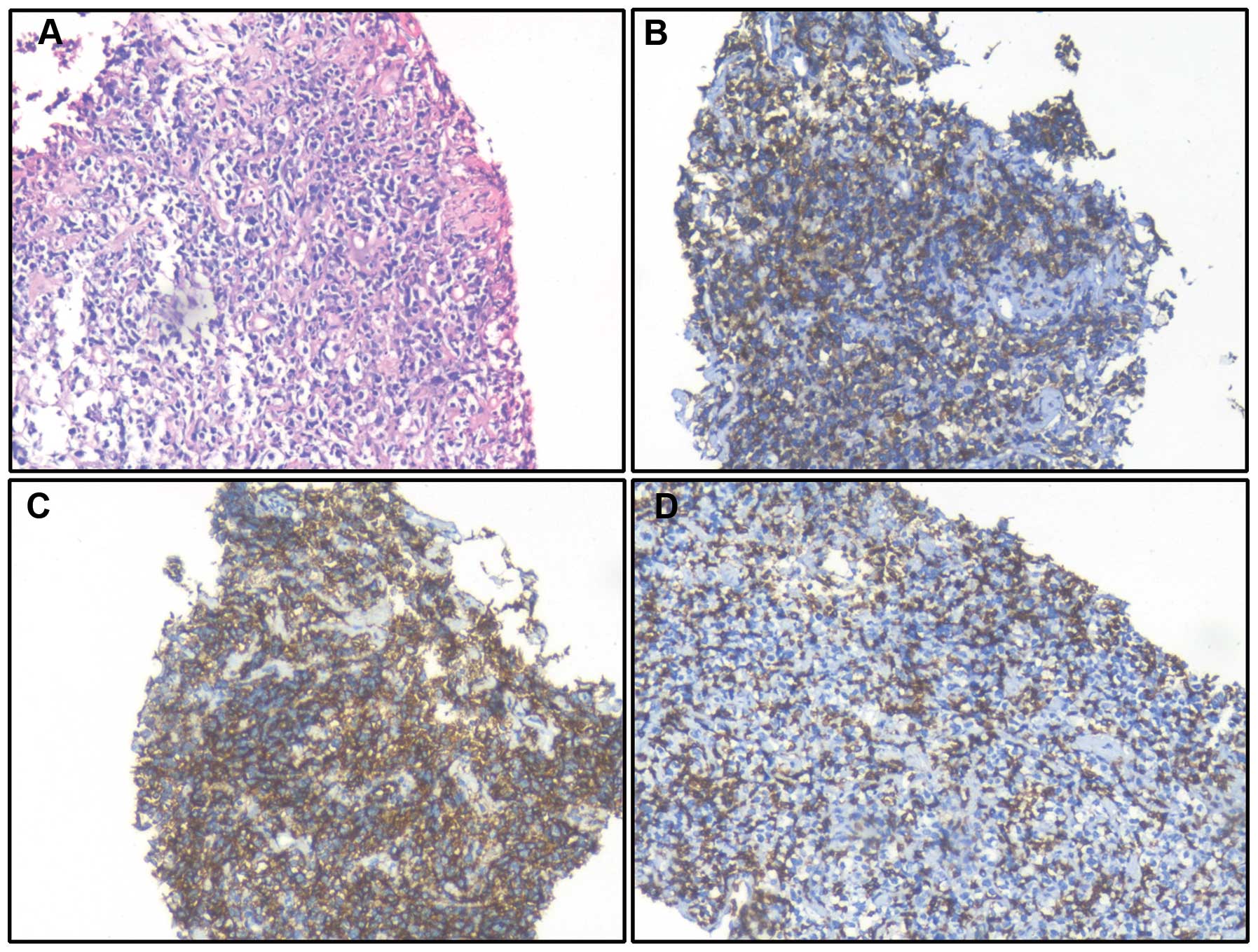
stopped 15 min after the surgery. Immunohistochemical examination
of a mass demonstrated the following results: Positivity for
cluster of differentiation (CD)20(++), CD3(+), leukocyte common
antigen(+++), B-cell lymphoma (BCL)-2(+), BCL-6(+), MUM-1(+),
vimentin(+) and S-100(+), with a Ki-67 of 80%; and negativity for
PSA, human melanoma black 45, P504S, 34βE12, p63, cytokeratin (CK),
CK20, villin, caudal-type homeobox-2, smooth muscle actin,
myogenin, CD30 and CD10 (Fig. 3).
Immunohistochemistry was assessed using the Intensity Reactivity
Score (IRS), which evaluates both the staining intensity and the
percentage of positive cells. Two pathologists at the Second
Xiangya hospital evaluated scores independently. The staining
intensity (SI) of the dye color was graded as either : 0, no color;
1, light yellow; 2, light brown; or 3, brown. The reactivity was
determined according to the percentage of positive cells (PP) in
the total number of cells where there were no negative specimens:
1–10%, 1; 11–30%, 2; 31–50%, 3; 51–80%, 4; and >80%, 5. The IRS
was calculated by multiplying the SI with the PP resulting in a
minimum score of 0 and a maximum score of 15. Subsequently, the
specimens were assigned one of four different levels: 0, (−); 1–4,
(+); 5–9, (++); and 10–15, (+++). Combined morphological and
immunophenotyping examinations confirmed the diagnosis of a DLBCL
of non-germinal center B-cell origin. Subsequent to pathological
confirmation of the diagnosis, the patient received intravenous
chemotherapy consisting of three courses of a low-dose R-CHOP
chemotherapy regimen. This was composed of 375 mg/m2
rituximab, 500 mg/m2 cyclophosphamide, 20
mg/m2 doxorubicin and 1 mg/m2 vincristine on
day 1 and 50 mg/m2 prednisone from days 1–5.
Following one course of chemotherapy, the patient
achieved partial remission, and the CT examination showed that the
size of the tumor had been reduced significantly (Fig. 1B). Subsequent to three courses of
chemotherapy, the patient achieved complete remission. The patient
was followed up for eight months, and is currently in a stable
condition, with no sign of recurrence of the hematuria.
Discussion
Primary malignant lymphoma of the prostate,
accounting for <0.1% of all non-Hodgkin’s lymphomas, are
globally rare. Clinical misdiagnosis of this condition has been
common, particularly in the elderly, due to the high similarity
with benign prostatic hyperplasia (BPH) or prostate cancer with
regard to the symptoms exhibited, including increased urinary
frequency, urinary urgency, hematuria and acute urinary retention
(5,6). The criteria for a diagnosis of primary
prostatic lymphoma are as follows: A tumor only located at the
prostate; no lymphoid node or tissue involvement, including the
blood vessels; and a lymphoma free period of at least one month
after diagnosis (6,7). In the present study, no other lymphoid
nodes or tissue involvement was observed in the patient, as
confirmed by systemic examination, in accordance to the diagnostic
criteria.
Imaging examinations, including CT, transrectal US
(TRUS) and positron emission tomography (PET)/CT, are useful in
assisting a diagnosis of the primary prostatic lymphoma. Early
fluorodeoxyglucose-PET is predictive of prognosis in patients with
aggressive NHL, and is useful for selecting patients who could
benefit from alternative treatments (6,8,9). The
final diagnosis can be established by pathological and
immunohistochemical examinations of samples obtained by surgery or
transrectal prostate biopsy. In the present study, the CT revealed
features that were similar to the published cases of NHL, such as
enlargement of the prostate, with low density lesions in the
presence or absence of abdominal and pelvic enlargement of the
lymph nodes (6,10), which were subsequently confirmed by
pathological and immunohistochemical examination.
Due to its rarity, there is no consensus on the
preferred treatment for prostatic lymphoma at present. Previous
studies demonstrated that R-CHOP chemotherapy was superior to CHOP,
a previous standard treatment for NHL (11). The studies suggested that it was the
optimal choice for curative intent, and that this combination
should become the standard treatment for DLBCL (12–14).
Rituxan, a chimeric monoclonal antibody of CD20, a cell-surface
protein that is present as one of the typical characteristics of
DLBCL, could specifically target the CD20 antigen of B-cell
lymphoma. Thus, Rituxan could enhance the cytotoxic sensitivity of
lymphoma cells, and synergize with chemotherapy without a
clinically significant increase in toxicity (15). In the present study, due to the poor
general condition and low hemoglobin levels of the patient, a
low-dose R-CHOP chemotherapy regimen was adopted. Following three
courses of chemotherapy, the patient achieved complete remission,
which suggested that the chemotherapy regimen had exhibited a
positive effect. The advantage of low-dose R-CHOP for this patient
was that it could minimize the side-effects of chemotherapy, while
simultaneously achieving the maximum associated benefits.
The clinical strategies for the treatment of
hematuria of prostatic origin consist of medical, surgical and
minimally invasive approaches. Conservative means to stop hematuria
include the use of 5α-reductase inhibitors and placement of a Foley
catheter with continuous bladder irrigation. However, in the case
of inoperable patients with acute or hyperacute hematuria,
interventional radiology appears to be a suitable alternative
option (3). Hald and Mygind
(16) first reported unilateral
hypogastric artery embolization for the treatment of severe bladder
hemorrhage in 1974. Selective arterial prostatic embolization has
subsequently been demonstrated to be useful in treating refractory
hematuria secondary to prostate cancer or BPH (4). The cessation of bleeding occurs
quickly after this procedure and can be subsequently maintained
without anesthesia (3). Recently,
arterial chemoembolization via various drug carrier systems has
become a suitable treatment for localized tumors (17). Combining chemotherapy with
embolization may maximize the curative effects. Firstly,
embolization could reduce the blood supply of a tumor, thus slowing
down the growth of the tumor. Secondly, it could also slow down the
local blood circulation, so that chemotherapy drugs can stay longer
in the lesions, thus significantly improving their effectiveness
(18). In the present study, the
patient developed a prostate tumor complicated by an acute massive
hemorrhage; conservative treatments, such as placement of a Foley
catheter with continuous bladder irrigation and a blood
transfusion, were unsuccessful. Considering that the patient’s
blood pressure decreased to 80/50 mmHg (normal range, 90/60–140/90
mmHg) and heart rate increased to 100 beats per min from 85 beats
per min (normal range, 60–100 beats per min) indicating that the
patient was in a state of shock and that they were not suitable for
a transurethral resection of the prostate under general anesthesia,
bilateral iliac arterial infusion chemotherapy and embolization
were chosen, both of which could impair the tumor and quickly stop
the bleeding. Surgery effectively stopped the bleeding under local
anesthesia and the duration of the procedure was short.
Post-operatively, the patient only developed mild hip pain and low
thermal discomfort, without serious complications such as a
recto-urethral fistula. Therefore, we propose that bilateral iliac
arterial infusion chemotherapy and embolization could be a safe and
effective method to treat prostate tumor with intractable
hemorrhage.
Due to the rarity of primary prostatic lymphoma, its
prognosis is unclear. In a retrospective review of 62 patients,
Bostwick et al (7)
demonstrated that the specific five-year survival rate was only
33%, and 73% of patients with primary prostatic lymphoma developed
metastasis one to 59 months after diagnosis. However, another
review of 23 cases showed that patients responded well to
chemotherapy and could possibly be cured if the primary prostatic
lymphoma was confined to the prostatic region (19). Serum LDH has proven to be an
important prognostic factor for non-Hodgkin’s lymphoma, with an
inverse correlation detected between levels of LDH and the survival
rate (20). Increased serum LDH
levels suggest a poor prognosis. In the present case, the patient
was >60 years old with a high LDH, which suggested a poor
prognosis. However, in cooperation with the Department of
Intervention and Hematology (Second Xiangya Hospital), R-CHOP was
administered and interventional embolization was performed on the
patient, which achieved a favorable effect. Following three courses
of chemotherapy, the patient was followed up for eight months, and
currently remains in a stable condition. Further observation is
required to obtain long-term results.
References
|
1
|
Sarris A, Dimopoulos M, Pugh W and
Cabanillas F: Primary lymphoma of the prostate: good outcome with
doxorubicin-based combination chemotherapy. J Urol. 153:1852–1854.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liguori G, Amodeo A, Mucelli FP, et al:
Intractable haematuria: long-term results after selective
embolization of the internal iliac arteries. BJU Int. 106:500–503.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abt D, Bywater M, Engeler DS and Schmid
HP: Therapeutic options for intractable hematuria in advanced
bladder cancer. Int J Urol. 20:651–660. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rastinehad AR, Caplin DM, Ost MC, et al:
Selective arterial prostatic embolization (SAPE) for refractory
hematuria of prostatic origin. Urology. 71:181–184. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zuazu JR, Iglesias R, Costa DR, et al:
Prostatic lymphoma and review of the literature. Actas Urol Esp.
33:686–690. 2009.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pan B, Han JK, Wang SC and Xu A: Positron
emission tomography/computerized tomography in the evaluation of
primary non-Hodgkin’s lymphoma of prostate. World J Gastroenterol.
19:6699–6702. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bostwick DG, Iczkowski KA, Amin MB,
Discigil G and Osborne B: Malignant lymphoma involving the
prostate: Report of 62 cases. Cancer. 83:732–738. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mikhaeel NG, Hutchings M, Fields PA,
O’Doherty MJ and Timothy AR: FDG-PET after two to three cycles of
chemotherapy predicts progression-free and overall survival in
high-grade non-Hodgkin lymphoma. Ann Oncol. 16:1514–1523. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhao J, Qiao W, Wang C, Wang T and Xing Y:
Therapeutic evaluation and prognostic value of interim hybrid
PET/CT with (18)F-FDG after three to four cycles of chemotherapy in
non-Hodgkin’s lymphoma. Hematol. 12:423–430. 2007. View Article : Google Scholar
|
|
10
|
Jhavar S, Agarwal JP, Naresh KN,
Shrivastava SK, Borges AM and Dinshaw KA: Primary extranodal mucosa
associated lymphoid tissue (MALT) lymphoma of the prostate. Leuk
Lymphoma. 41:445–449. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fisher RI, Gaynor ER, Dahlberg S, et al:
Comparison of a standard regimen (CHOP) with three intensive
chemotherapy regimens for advanced non-Hodgkin’s lymphoma. N Engl J
Med. 328:1002–1006. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Csomor J, Kaszás I, Kollár B, et al:
Prolonged survival using anti-CD20 combined chemotherapy in primary
prostatic intravascular large B-cell lymphoma. Pathol Oncol Res.
14:281–284. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Feugier P, Van Hoof A, Sebban C, et al:
Long-term results of the R-CHOP study in the treatment of elderly
patients with diffuse large B-cell lymphoma: a study by the Groupe
d’Etude des Lymphomes de l’Adulte. J Clin Oncol. 23:4117–4126.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lupu A, Radu P, Pană B and Kalfas C:
R-CHOP vs. CHOP: A cost-effectiveness analysis on aggressive
non-Hodgkin’s lymphoma (NHL). Management in Health. 13:18–21. 2009.
View Article : Google Scholar
|
|
15
|
Coiffier B, Lepage E, Briere J, et al:
CHOP chemotherapy plus rituximab compared with CHOP alone in
elderly patients with diffuse large-B-cell lymphoma. N Engl J Med.
346:235–242. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hald T and Mygind T: Control of
life-threatening vesical hemorrhage by unilateral hypogastric
artery muscle embolization. J Urol. 112:60–63. 1974.PubMed/NCBI
|
|
17
|
Kato T, Sato K, Sasaki R, Kakinuma H and
Moriyama M: Targeted cancer chemotherapy with arterial microcapsule
chemoembolization: review of 1013 patients. Cancer Chemother
Pharmacol. 37:289–296. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ozono S, Kim S, Takashima K, et al:
Intra-arterial chemotherapy for invasive bladder cancer. Hinyokika
Kiyo. 45:133–137. 1999.(In Japanese). PubMed/NCBI
|
|
19
|
Fukutani K, Koyama Y, Fujimori M and
Ishida T: Primary malignant lymphoma of the prostate: report of a
case achieving complete response to combination chemotherapy and
review of 22 Japanese cases. Nihon Hinyokika Gakkai Zasshi.
94:621–625. 2003.(In Japanese). PubMed/NCBI
|
|
20
|
Ferraris AM, Giuntini P and Gaetani GF:
Serum lactic dehydrogenase as a prognostic tool for non-Hodgkin
lymphomas. Blood. 54:928–932. 1979.PubMed/NCBI
|