Introduction
Pulmonary artery leiomyosarcoma (PAL) is an
extremely rare primary sarcoma of the pulmonary artery with an
incidence rate of ~0.001–0.03% (1,2). Due
to its low incidence, PAL is often undetected and frequently
misdiagnosed as chronic pulmonary embolism (3,4).
However, the majority of PAL tumors are highly malignant,
highlighting the requirement for improved methods of detecting and
treating these tumors (2). Early
detection and surgical resection of the primary PAL lesion have
been demonstrated to improve patient survival; the median survival
time of all patients was 1.5 months, but this was prolonged to 10
months with surgery such as pneumonectomy or mere excision of the
tumor from the vascular bed (5).
However recurrence of PAL often occurs following surgical resection
(6). The benefits of adjuvant
therapy for PAL tumors have not been clearly defined, particularly
in the case of recurrent tumors. A previous report showed that a
patient with primary leiomyosarcoma, who was receiving adjuvant
therapy, survived for as long as 20 months (7). The current study presents the case of
a patient with recurrent PAL. Written informed consent was obtained
from the patient.
Case report
A 42-year-old male presented to The First Affiliated
Hospital of Anhui Medical University (Hefei, China) with repeated
and progressive dizziness and chest pain for the previous five
months, and with one occurrence of syncope in this period. The
patient was admitted to the Department of Cardiac Surgery on 25th
October 2012. Upon physical examination the patient’s blood
pressure was 100/70 mmHg (normal range, 100–140/60–90 mmHg; 1
mmHg=0.133 kPa) and his heart rate was 78 beats/minute. No cyanosis
was detectable when the patient was in a supine position. The
patient’s jugular vein filling time was normal, and a slightly
enlarged left heart border was observed. A grade III systolic
murmur was identified between the second and third left intercostal
space. Cardiac exam indicated that the patient’s pulmonary valve
closing (P2) was normal, with no signs of hyperactivity. The liver
was not accessible for examination. Blood tests revealed no
abnormalities in the patient’s blood cell counts or blood
chemistry. Echocardiography (ECG) indicated that the right atrium
and right ventricle had significantly increased in size. ECG also
revealed abnormal Q waves of and ST-T changes in the II, III and
aVF leads. The pulmonary trunk and left distal pulmonary artery
were filled by light reflection. The patient experienced severe
tricuspid regurgitation, with estimated pulmonary artery pressure
of 126 mmHg (normal range, 12–18 mmHg).
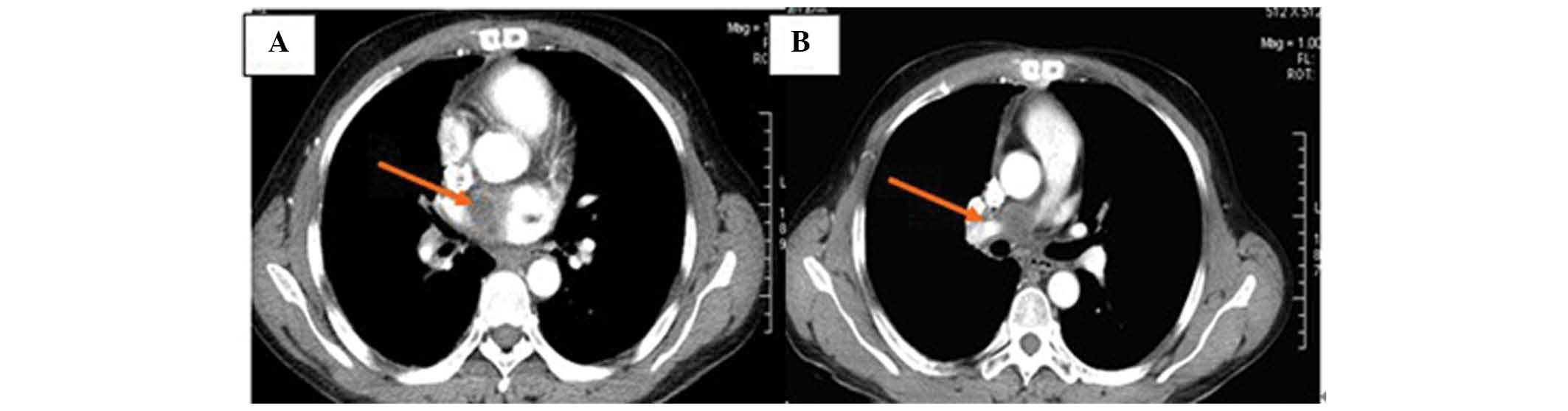
Based on these symptoms, an initial diagnosis of
pulmonary thromboembolism with severe pulmonary hypertension and a
minor pericardial effusion was determined. A computed tomography
(CT) angiogram revealed thrombosis of the pulmonary artery, left
pulmonary artery, and the right pulmonary artery branch. The
diameters of ascending aortic and descending aortic were 28.9×30.9
mm and 23.5×23.4 mm, respectively (normal diameters, <35×35 mm)
(Figs. 1A and 2A). A vascular ultrasound indicated that
the portal vein, splenic vein, inferior vena cava, and bilateral
iliac vein of the patient were all normal.
Based on the initial diagnosis of pulmonary
thromboembolism, the patient was scheduled to undergo a pulmonary
embolectomy in combination with tricuspid valvuloplasty under
extracorporeal circulation. However, during surgery, a mass
predominantly involving the right pulmonary artery and its branches
was observed. No similar mass was identified in the left pulmonary
artery. Tissue samples of the mass were extracted from the patient
and frozen for subsequent analysis. Analysis of the frozen tissue
section indicated that the mass was a malignant emboli of unknown
origin. Therefore, tumor cystectomy and tricuspid valvuloplasty was
performed.
Upon postoperative pathological analysis, the mass
was identified as a spindle cell sarcoma, indicating that the mass
was a PAL tumor (Fig. 1B).
Immunohistochemical analysis showed that the cells of the mass were
positive for CD117 and negative for cytokeratin (CK) 7, CK20,
Villln, CD34, DOG-1, CK10 and CD10. Proliferation analysis by Ki-67
staining indicated that 40% of the cells were actively
proliferating in the tumor. Following the removal of the tumor, the
patient’s dizziness and chest pain were eliminated and no abnormal
lesions were detected in the right pulmonary artery under enhanced
CT examination on 30th November 2012 (Fig. 2B). Following surgery, the patient
received three cycles of chemotherapy with 100 mg epirubicin and 20
mg cisplatin under a d1-5 regimen on 11th December 2012, 12th
January 2013, and 19th February 2013, respectively.
On 20th March 2013, the patient returned to the
hospital presenting with dizziness and congestion. Enhanced chest
CT examination revealed a soft tissue mass of 3.5×3.4×3.6 cm in
size in the right pulmonary artery (Fig. 3A). The mass was diagnosed as a
recurrent PAL tumor. The patient’s Karnofsky Performance Score
(KPS) was 60, indicating that the quality of life was compromised
(8). The patient was subsequently
treated with intensity modulated conformal radiotherapy
(diffusion-tensor; 32 Gy/16 f) at the right pulmonary artery
between 28th March and 16th April 2013. Following therapy, the
patient reported relief of dizziness and congestion. Enhanced chest
CT examination revealed that the tumor mass had reduced in size to
3.1×3.2×3.3 cm (Fig. 3B). The
patient received additional radiotherapy (30 sessions) with a
dosage each time of 2 Gy administered five times a week for six
weeks until May 2, 2013 (Fig. 5).
During the course of radiotherapy, the patient reported chest pain
when swallowing food, which was due to radiation esophagitis; this
was relieved following symptomatic treatment (160,000 units
gentamicin, three times a day, orally). The patient did not receive
any additional chemotherapy after radiotherapy. By 27th May 2013,
enhanced chest CT examination indicated that the mass had further
reduced in size to 3.0×3.2×2.7 cm (Fig.
4A). Following this course of radiotherapy, the patient
reported relatively good health with minor tightness of the chest
after climbing stairs quickly, and had regained the ability to
perform mild to moderate physical labor. Enhanced chest CT
examination on 8th August 2013 showed further reduction of the PAL
mass to a size of 2.5×2.2×2.4 cm (Fig.
4B). Bronchial ultrasound examination of the patient’s abdomen
revealed no further abnormalities. The patient was followed up four
times over a period of eight months. The tumor appeared to be
stable for the first three sessions. However, at the fourth
follow-up tumor growth was observed. At this time, the patient’s
quality of life was substantially improved, with a KPS of 90.
Discussion
Primary leiomyosarcoma of the pulmonary artery is an
extremely rare tumor, and the majority of PAL patients present with
non-specific symptoms including dyspnea, chest pain, coughing and
hemoptysis (5,9). As a result, many PAL patients are
initially misdiagnosed with pulmonary thromboembolism (10–13),
as demonstrated in the present case. However, as PAL is an
extremely aggressive tumor, more thorough diagnoses must be
considered when patients present with such symptoms, so as to
minimize the risk of misdiagnosing a malignant PAL lesion. In
particular, the diagnosis of a tumor must be considered in the
absence of predisposing factors for thromboembolism, in cases were
the patient’s symptoms persist or recur despite adequate
anticoagulation, and also in cases with a unilateral distribution
of a massive perfusion defect (14).
In the current study, PAL was diagnosed incidentally
during surgery and the tumor was subsequently resected, which
potentially contributed to the favorable prognosis of this patient,
as early detection and surgical resection has been shown to improve
PAL survival rates (6). Patients
typically develop PAL between the ages of 40 and 60 years. Thus
patients within this age range should be subjected to a thorough
clinical examination, and diagnoses including PAL, thromboembolism
and lung cancer must be considered. For maximal benefit, definitive
diagnostic methods must be employed to differentiate between these
possibilities, and immediate surgical intervention must be
performed in cases of cancer.
The diagnosis of PAL is frequently delayed due to
the nonspecific symptoms, therefore, these neoplasms are often well
developed before they are clinically diagnosed (2,9,15,16).
If the tumor is detected early and can be completely resected,
surgery offers the best opportunity to eliminate PAL without
residual disease. However, despite aggressive surgical
intervention, the mean patient survival time of 1.5 months has been
shown to improve by only a few months, to 10 months, due to the
aggressive nature of advanced PAL lesions (5,17).
Another study showed that the median survival time of all patients
was 1.5 months, but this was prolonged to 10 months following
surgery such as pneumonectomy or mere excision of the tumor from
the vascular bed (5). This is also
shown in the current study, as the PAL recurred within four months
of surgical resection, indicating that the patient’s disease had
already reached an aggressive state at the time of diagnosis.
To date, little evidence is available indicating
that adjuvant therapies, such as chemotherapy or radiotherapy, are
beneficial for patients with recurrent PAL (6,18–20).
Furthermore, only a few reports have demonstrated the successful
treatment of recurrent PAL, primarily through surgery or stenting
(6,19,20).
Notably, in the current study, radiotherapy was found to
effectively inhibit and control the development of PAL in the
patient. This case suggests that radiotherapy may benefit PAL
patients, including those who have failed to respond to surgery
and/or chemotherapy. However, why radiotherapy was effective in
this case, but ineffective in previous reports, remains unclear. A
more extensive analysis of the factors that influenced the present
patient’s response to radiotherapy may aid in informing future
treatment strategies for recurrent PAL.
Chemotherapy and radiotherapy are two major adjuvant
therapeutic methods for the treatment of malignancies (21,22).
The therapeutic efficacy of these two methods varies depending on
the specific tumor. In the present case, the patient did not
respond well to chemotherapy, however, did respond to radiotherapy.
This is in contrast to the majority of reports describing PAL, in
which adjuvant therapies had been largely ineffective, as PAL is
considered not sensitive to radiotherapy and chemotherapy.
Therefore, there is insufficient evidence to conclude that
radiotherapy is more efficient than chemotherapy in treating
recurrent PAL. Nonetheless, the clinical results presented in this
case report indicate that the use of radiotherapy to treat PAL
warrants further investigation to better assess the efficacy of
this therapeutic strategy.
References
|
1
|
Hoffmeier A, Semik M, Fallenberg EM and
Scheld HH: Leiomyosarcoma of the pulmonary artery - a diagnostic
chameleon. Eur J Cardiothorac Surg. 20:1049–1051. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dumont P, Diot P, Aupart MR and Toumieux
B: Leiomyosarcoma of the pulmonary artery. Ann Thorac Surg.
66:2089–2091. 1998. View Article : Google Scholar
|
|
3
|
Adeli SH, Nemati B, Jandaghi M, Riahi MM,
Hosseinzadeh F and Salarvand F: Pulmonary Hypertension due to a
Pulmonary Artery Leiomyosarcoma: A Case Report. Case Rep Pulmonol.
2013:1606192013.PubMed/NCBI
|
|
4
|
Widera E and Sulica R: Pulmonary artery
sarcoma misdiagnosed as chronic thromboembolic pulmonary
hypertension. Mt Sinai J Med. 72:360–364. 2005.PubMed/NCBI
|
|
5
|
Krüger I, Borowski A, Horst M, de Vivie
ER, Theissen P and Gross-Fengels W: Symptoms, diagnosis, and
therapy of primary sarcomas of the pulmonary artery. Thorac
Cardiovasc Surg. 38:91–95. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Okada K, Okada M, Yamamoto S, et al:
Successful resection of a recurrent leiomyosarcoma of the pulmonary
trunk. Ann Thorac Surg. 55:1009–1012. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kashima K1, Yamashita E, Mataki H,
Yotsumoto G, Nomoto M, Sonoda M and Hanada S: Primary
leiomyosarcoma of the pulmonary artery: a case of a 20-month
survivor after incomplete surgical resection. Intern Med. 51:75–78.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Milstein JM, Cohen ME and Sinks LF: The
influence and reliability of neurologic assessment and Karnofsky
performance score on prognosis. Cancer. 56(7 Suppl): 1834–1836.
1985. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mayer E, Kriegsmann J, Gaumann A, et al:
Surgical treatment of pulmonary artery sarcoma. J Thorac Cardiovasc
Surg. 121:77–82. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Allen S, Todd J, Copley S and Al-Nahhas A:
F-18 FDG uptake in bilateral pulmonary artery leiomyosarcomata, one
mimicking a pulmonary embolus. Clin Nucl Med. 30:418–419. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Minakata K, Konishi Y, Matsumoto M, Aota
M, Nonaka M and Yamada N: Primary leiomyosarcoma of the pulmonary
artery mimicking massive pulmonary thromboembolism. Jpn Circ J.
64:783–784. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mazzucco A, Luciani GB, Bertolini P,
Faggian G, Morando G and Ghimenton C: Primary leiomyosarcoma of the
pulmonary artery: diagnostic and surgical implications. Ann Thorac
Surg. 57:222–225. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Myerson PJ, Myerson DA, Katz R and Lawson
JP: Gallium imaging in pulmonary artery sarcoma mimicking pulmonary
embolism: case report. J Nucl Med. 17:893–895. 1976.PubMed/NCBI
|
|
14
|
Eng J and Murday AJ: Leiomyosarcoma of the
pulmonary artery. Ann Thorac Surg. 53:905–906. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Babatasi G, Massetti M, Galateau F and
Khayat A: Leiomyosarcoma of the pulmonary veins extending into the
left atrium or left atrial leiomyosarcoma: multimodality therapy. J
Thorac Cardiovasc Surg. 116:665–667. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rafal RB, Nichols JN and Markisz JA:
Pulmonary artery sarcoma: diagnosis and postoperative follow-up
with gadolinium-diethylenetriamine pentaacetic acid-enhanced
magnetic resonance imaging. Mayo Clin Proc. 70:173–176. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tanaka I, Masuda R, Inoue M, et al:
Primary pulmonary-artery sarcoma. Report of a case with complete
resection and graft replacement and review of 47 surgically treated
cases reported in the literature. Thorac Cardiovasc Surg. 42:64–68.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yamada N, Kamei S, Yasuda F, Isaka N, Yada
I and Nakano T: Primary leiomyosarcoma of the pulmonary artery
confirmed by catheter suction biopsy. Chest. 113:555–556. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Omura A, Tobe S, Yoshida K and Yamaguchi
M: Surgical treatment for recurrent pulmonary artery sarcoma. Gen
Thorac Cardiovasc Surg. 56:28–31. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Meckel S, Buitrago-Téllez C, Herrmann R
and Jacob AL: Stenting for pulmonary artery stenosis due to a
recurrent primary leiomyosarcoma. J Endovasc Ther. 10:141–146.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zaric B, Stojsic V, Tepavac A, et al:
Adjuvant chemotherapy and radiotherapy in the treatment of
non-small cell lung cancer (NSCLC). J Thorac Dis. 5(Suppl 4):
S371–S377. 2013.PubMed/NCBI
|
|
22
|
Chaulagain CP, Ng J, Goodman MD and Saif
MW: Adjuvant therapy of pancreatic cancer. JOP. 14:119–122.
2013.PubMed/NCBI
|