Introduction
Primary and secondary ectopic meningiomas are rare
lesions (1). In addition, primary
ectopic meningiomas that develop in the nasal sinus or nasal cavity
possess an unknown etiology (2).
Meningiomas account for 10–15% of all intracranial
tumors (3), but primary and
secondary meningiomas outside the central nervous system are
uncommon. The most common sites of extracranial meningiomas are the
skull, scalp, nose, orbit, paranasal sinuses, middle ear, neck and
skin (4).
Extracranial meningiomas of the sinonasal tract are
rare tumors that are frequently misdiagnosed, resulting in
inappropriate clinical management. Primary extracranial meningiomas
are likely to arise from the transformation of embryonic arachnoid
cell remnants of ectopic meningocytes, which are derived from
pluripotent mesenchymal cells. The diagnosis of extracranial
primary meningiomas requires confirmation by computed tomography
(CT) to exclude the presence of an intracranial mass or any
underlying bony erosion of the skull base (5). Treatment usually involves tumor
resectioning, and additional treatment with radiotherapy and
chemotherapy. Fine-needle aspiration cytology of the lesion can be
inaccurate, and a final diagnosis is usually made on the basis of a
histological examination of the excised mass (6). The present study reports the diagnosis
and treatment of a nasal meningioma and reviews the recent
literature. Written informed consent was obtained from the
patient.
Case report
A 60-year-old female presented to the Otolaryngology
Department of the Shanghai Pudong New Area Gongli Hospital
(Shanghai, China) with hyposmia that had been present for a
six-month period, without rhinorrhea or epistaxis. Clinical
examination did not identify a nasal obstruction, and the patient
did not possess a history of headaches or visual problems.
Endoscopy identified the presence of a neoplasm in the bilateral
olfactory cleft, with the nasal polyp morphology necessitating a
radiological examination.
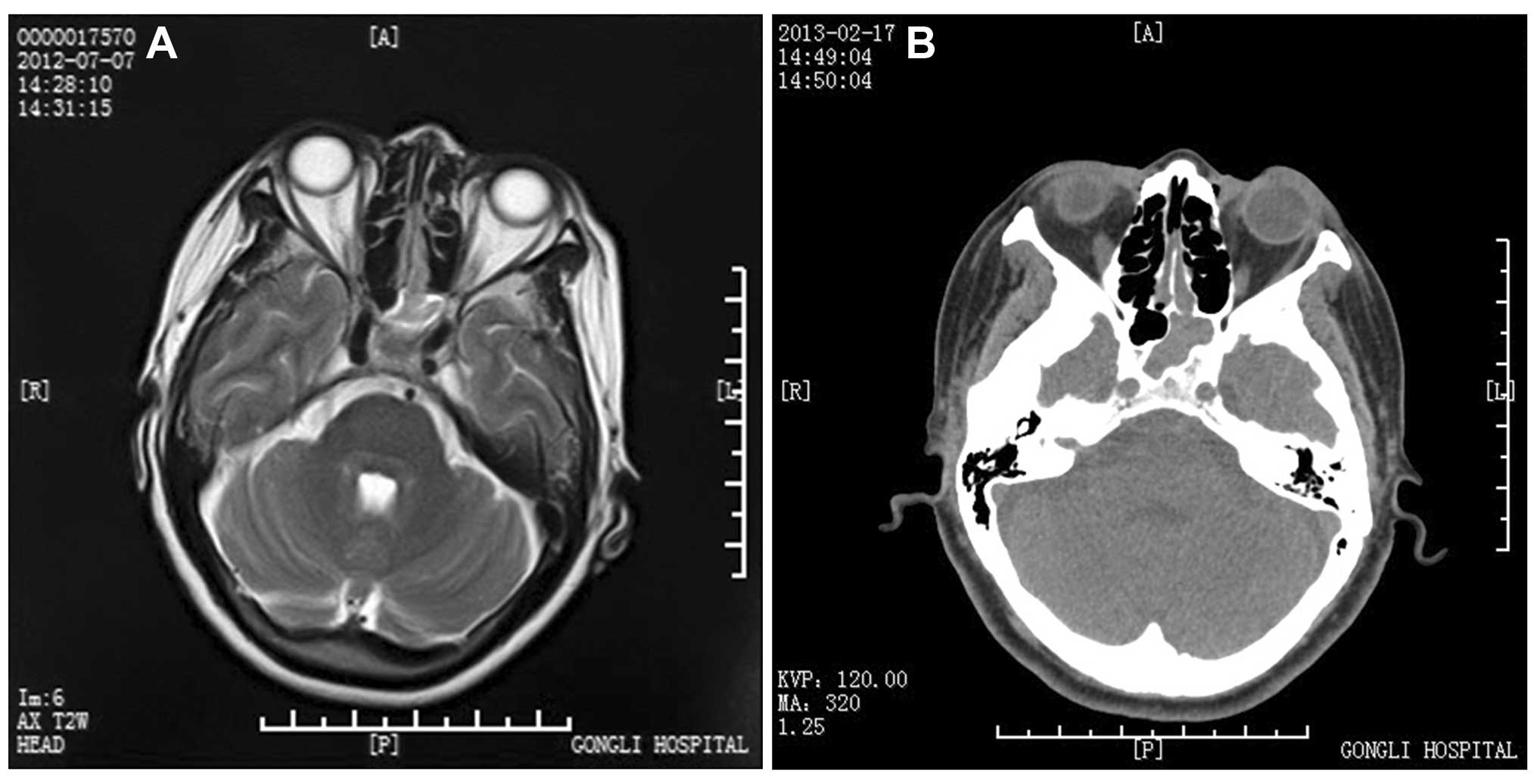
A magnetic resonance imaging (MRI) examination in
the Radiology Department of Shanghai Pudong New Area Gongli
Hospital revealed sphenoid sinusitis on the left side of the
olfactory cleft and a high-density shadow in the bilateral
olfactory cleft five months prior to presenting at the
Otolaryngology Department, where a CT scan of the paranasal sinus
was conducted. Radiological examination of the nasal cavity prior
to surgery identified the presence of soft tissue shadows in the
bilateral olfactory cleft area and sinusitis in the left side of
the sphenoid. MRI and CT scans of the orbit and nasal cavity
revealed that the soft tissue mass was situated exclusively in the
bilateral olfactory cleft region and did not invade other sinuses
or the orbit (Fig. 1A and B).
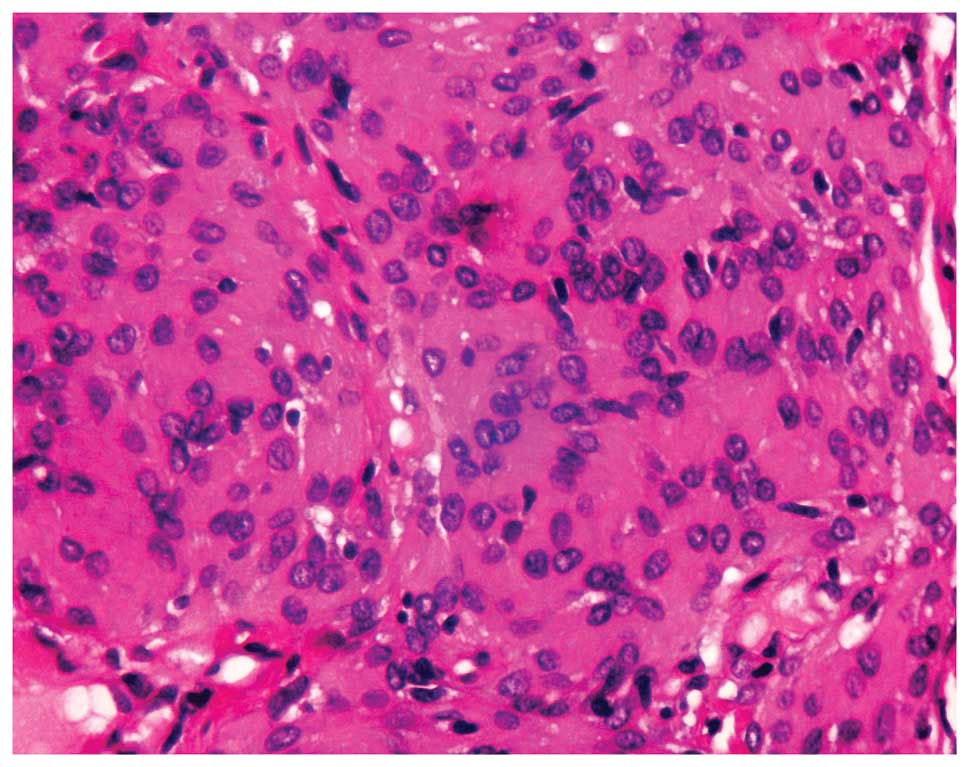
The histopathological appearance of the lesion was
meningothelial, a common tumor type in which the cells present in a
lobulated arrangement and are spaced along collagen fibers. The
tumor cells also varied in size. They demonstrated a high
nucleocytoplasmic ratio and a marginal oval nucleus, with nucleoli
discernable in each cell. Fibroblasts were arranged in a matrix
rich in collagen and crosslinking reticular fibers. Spiral
structures were visible and did not contain psammoma bodies.
Mitosis was inconspicuous, and no necrosis was observed (Figs. 2 and 3).
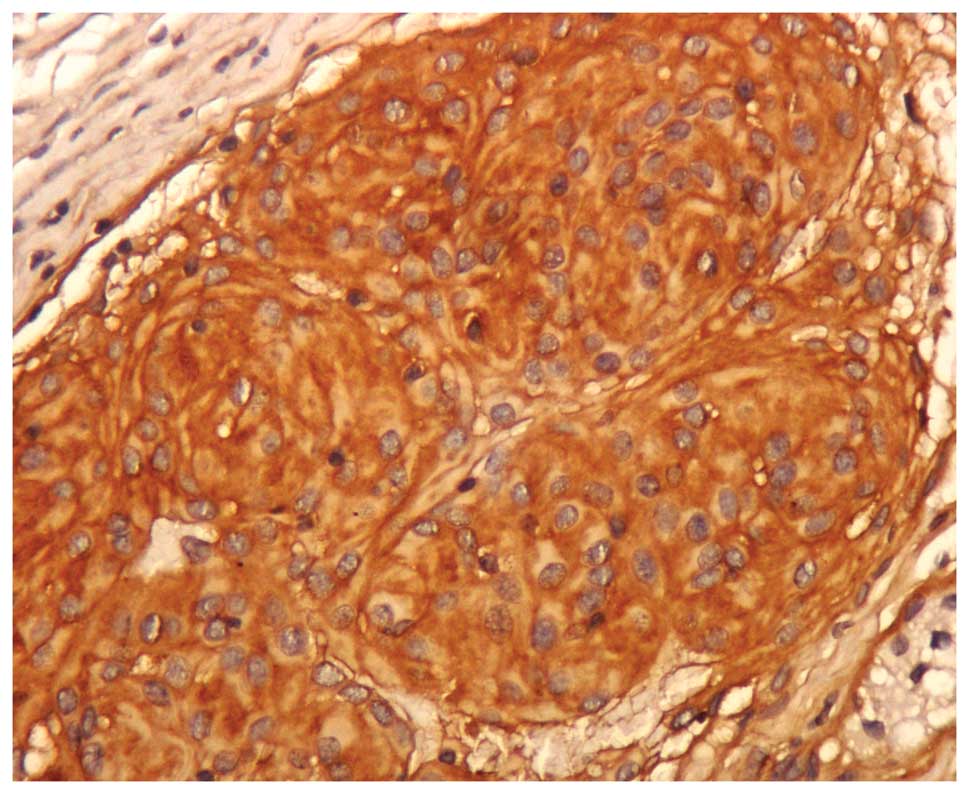
Immunohistochemical examination identified the
presence of the epithelial membrane antigen expression. However,
the immunoreactivity was focal and generally weak, identifying only
a small number of positive cells in the sample examined. Other
epithelial markers were also identified, including the S-100
protein in the nucleus and the cytoplasm. Isolated tumor cells were
stained for the expression of Ki-67 in the nucleus.
The tumor was excised from the sinus by functional
endoscopy surgery. The patient continues to experience disease-free
survival seven months subsequent to surgery. Post-operative nasal
endoscopic examination revealed no residual mass. Follow-up visits
were scheduled every three months, with no evidence of recurrence
to date. The patient’s olfactory recovery and nasal ventilation
were normal subsequent to surgery.
Discussion
The present patient presented with a benign primary
ectopic meningioma. Meningiomas of the nasal cavity, particularly
in the olfactory cleft, are rare. Primary ectopic meningiomas are
challenging to diagnose, partly due to the infrequency of their
presentation and often being confused with nasal polyps. However,
primary ectopic meningiomas tend to be aggressive. Definitive
diagnosis requires histological examination. Anosmia is among the
first symptoms associated with ectopic meningioma, although
patients also present with headaches or visual problems (7). Endoscopic surgery to remove the growth
is an accepted therapy for this condition and is associated with a
good survival rate (2).
Primary extracranial meningiomas of the head and
neck are rare, with the majority presenting at secondary locations
relative to the primary intracranial tumor. Primary extracranial
meningiomas account for 1–2% of all meningiomas and are generally
associated with a favorable prognosis. Subsequent to the diagnosis
of a meningioma, it is necessary to exclude meningioma of the
neuraxis or a primary central meningioma (9).
The most frequent extracranial sites reported for
primary meningioma are the nasal cavity, paranasal sinuses, cranial
bones, middle ear, scalp and soft tissues of the face and neck, and
the parotid gland (10). The
largest study that reported extracranial head and neck meningiomas
consisted of 146 cases (8), among
which the majority of meningiomas were of the skin and scalp
(n=59), middle ear (n=26), nasal cavity (n=17), temporal bone
(n=2), or the parotid gland (n=1). Other similar studies included
patients with meningioma of the sinonasal tract (n=30) (11), ear and temporal bone.
The etiopathogenesis of extracranial meningiomas
involves the migration of arachnoid cells derived from the neural
crest. However, additional mechanisms have been proposed. For
example, extracranial meningiomas may potentially originate from:
i) Arachnoid cells of nerve sheaths emerging from the skull
foramina; ii) pacchionian bodies that have been displaced or
entrapped in an extracranial location during embryological
development; iii) arachnoid islets that have been displaced due to
trauma or cerebral hypertension; and iv) undifferentiated
mesenchymal cells (12).
The classification system utilized by Hoye et
al (13) encompasses the major
etiologies suggested in the development of extracranial
meningiomas: i) Extracranial extensions of a meningioma with an
intracranial origin (secondary); ii) extracranial extensions of a
meningioma arising in a neural foramina (primary); iii) ectopic,
without any connection to intracranial structures (primary); and
iv) extracranial metastasis from an intracranial meningioma
(secondary).
The meningioma described in the present study was
derived from the third group of the aforementioned classification
system. The presentation of hyposmia in the current patient
facilitated the diagnosis of meningioma prior to the invasion of
the tumor into other sinuses or the orbit.
The current World Health Organization classification
distinguishes between three grades of meningioma: Typical or benign
(Grade I); atypical with frequent mitosis (Grade II); and
anaplastic with invasion (Grade III). However, Zulch (14) suggested that the completeness of
extirpation is more important than histological grading for
classifying meningioma. Although meningiomas are classified as
benign, since they do not metastasize, they demonstrate a
predilection for invading crevices and foramina, and necrosis may
be spread between one cavity and another (15). In the present study, the benign
nature of the tumor was evident from its slow growth and
non-involvement with the orbit or any cranial nerves. Radiological
examination provided precise information regarding the extent of
tumor invasion, which is key to diagnosis. However, confirmation of
the radiological diagnosis by histological and immunohistochemical
examinations was required.
Rushing et al (8) reported in 2009 that 76% of
extracranial meningiomas were progesterone receptor-positive, 96%
were somatostatin receptor-positive, 89% were epidermal growth
factor receptor-positive, and 19% were estrogen receptor-positive
(Table I) (8). Accordingly, Tamoxifen and RU-486, an
antiprogesterone, are being investigated for potential as
treatments for certain meningiomas. Monosomy 22 is a characteristic
and frequent chromosomal aberration associated with meningioma and
its prognosis (16).
 | Table IImmunohistochemical profile of
extracranial meningiomas. |
Table I
Immunohistochemical profile of
extracranial meningiomas.
| Antigen | Total number of
observations, n | Number of positive
reactions, n (%) |
|---|
| Vimentin | 78 | 78 (100.0) |
| Epithelial membrane
antigena | 80 | 61 (76.3) |
| Cytokeratinb | 75 | 18 (24.0) |
| CK7 | 55 | 12 (21.8) |
| S-100 protein | 78 | 15 (19.2) |
| CAM 5.2 | 54 | 3 (5.6) |
| Synaptophysin | 75 | 3 (4.0) |
| CK20 | 52 | 1 (1.9) |
| GFAP | 69 | 1 (1.4) |
| Chromogranin | 72 | 0 (0.0) |
| Synuclein | 18 | 0 (0.0) |
| Ki-67 index
>1% | 78 | 21 (26.9) |
Radical surgical resection has been associated with
a good prognosis in patients with meningioma, but the benefit of
adjunctive post-operative radiotherapy has not yet been established
(3). Radiotherapy is suggested as
the treatment of choice for unresectable malignant meningiomas and
for recurrent meningiomas in patients with a late onset or other
conditions that do not permit surgery to be conducted, including
poor general condition and coagulation disorders.
Novel techniques available for meningioma management
include proton irradiation and stereotactic radiosurgery using a
gamma knife. Incomplete tumor removal, atypical or malignant
tumors, nucleolar prominence, more than two visible mitotic events
per 10 high-power fields and a heterogeneous contrast enhancement
on CT are associated with increased rates of recurrence (17).
Meningiomas are infrequently occurring tumors with
unpredictable clinical behavior. A clear understanding of the
etiology and the appropriate principles for the diagnosis and
management of these lesions may aid in overcoming the difficulty of
treating primary extracranial meningiomas. The present case
revealed that CT and immunohistochemical examination are important
for the diagnosis of ectopic meningioma of the nasal cavity and
that tumor resection presents the optimum treatment for
meningiomas.
Acknowledgements
The authors would like to thank Medjaden Bioscience
Limited for assisting in the preparation of the present manuscript.
This study was supported, in part, by the the Shanghai Pudong New
Area Science and Technology Development Foundation (grant no’s.
PKJ2014-Y22 and PKJ2012-Y27) and the Key Disciplines Group
Construction Project of Shanghai Pudong Health Bureau (grant no.
PWZxq2014-09).
References
|
1
|
Sanei MH, Berjis N, Mahzouni P and Naimi
A: A case of neck ectopic meningioma. Neuropathology. 28:157–159.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhou X, Li J and Peng T: Report of 4 cases
ectopic meningioma of maxillary sinus in children and the review of
relative literatures. Lin Chuang Er Bi Yan Hou Ke Za Zhi.
19:490–491. 2005.(In Chinese). PubMed/NCBI
|
|
3
|
Kurt AJ, Cohen ME and Duffner PK:
Neurology in clinical practise. 3rd ed. pp. 1273
|
|
4
|
Kjeldsberg CR and Minckler J: Meningiomas
presenting as Nasal Polyps. Cancer. 29:153–156. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Qutub MF, Haider A, Jawad HA and Khalbuss
WE: Fine needle aspiration cytology of ectopic meningioma
presenting as a neck mass: a case report and a review of the
literature. Cytopathology. 23:61–64. 2012. View Article : Google Scholar
|
|
6
|
Kolte SS and Lanjewar RA: Ectopic
meningioma diagnosed on fine needle aspiration cytology. Acta
Cytol. 54:1075–1076. 2010.PubMed/NCBI
|
|
7
|
Fu JY, Gao XG, Li SY, et al: Ectopic
meningioma in oral and maxillofacial region: report of 23 cases.
Shanghai Kou Qiang Yi Xue. 19:23–27. 2010.(In Chinese). PubMed/NCBI
|
|
8
|
Rushing EJ, Bouffard JP, McCall S, et al:
Primary extracranial meningiomas: an analysis of 146 cases. Head
Neck Pathol. 3:116–130. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hameed A, Gokden M and Hanna EY:
Fine-needle aspiration cytology of a primary ectopic meningioma.
Diagn Cytopathol. 26:297–300. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sanei MH, Rabiei S, Eftekhari M and Jafari
HR: Ectopic meningioma (hamartoma) of the middle ear: a challenging
case in frozen section. Otol Neurotol. 35:e231–e232. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Thompson LD and Gyure KA: Extracranial
sinonasal tract meningiomas: a clinicopathologic study of 30 cases
with a review of the literature. Am J Surg Pathol. 24:640–650.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Serry P, Rombaux PH, Ledeghen S, et al:
Extracranial sinosal tract meningioma: a case report. Acta
Otorhinolaryngol Belg. 58:151–155. 2004.
|
|
13
|
Hoye SJ, Hoar CS Jr and Murray JE:
Extracranial meningioma presenting as a tumour of the neck. Am J
Surg. 100:486–489. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zülch KJ: Histological typing of tumours
of the central nervous system. World Health Organization; Geneva:
pp. 57–58. 1979
|
|
15
|
Friedmann I and Osborn DA: Pathology of
granulations and neoplasms of the nose and paranasal sinus.
Churchill Livinstone; London: pp. 193–197. 1982
|
|
16
|
Ketter R, Henn W, Feiden W, et al:
Nasoethmoidal meningioma with cytogenetic features of
tumouraggressiveness. Paediatr Neurosurg. 39:190–194. 2003.
View Article : Google Scholar
|
|
17
|
Sharma JK, Pippal SK and Sethi Y: A rare
case of primary nasoethmoidal meningioma. Indian J Otolaryngol Head
Neck Surg. 58:101–103. 2006.PubMed/NCBI
|