Introduction
Acute myeloid leukemia (AML) is a type of
hematologic malignancy. The peak age of onset is >60 years old
(1). AML is frequently accompanied by
specific cytogenetic aberrations. t(16;21) (p11;q22) is a rare and
non-random chromosomal translocation that causes the rearrangement
of erythroblast transformation specific-related gene (ERG) on
chromosome 21 and translocated in sarcoma/fused in sarcoma
(TLS/FUS) on chromosome 16, forming the TLS/FUS-ERG fusion gene.
t(16;21) (p11;q22) occurs with an incidence of 1% in AML (2). The morphology, immunology and clinical
manifestation of this translocation are distinct from other
subtypes of AML. Literature associated with t(16;21) (p11;q22) AML
is scarce. The present study reports three patients with AML and
t(16;21)(p11;q22) who exhibited unique characteristics compared
with other subtypes of AML. Written infomred consent was obtained
from the family of the patient.
Case report
Patient 1
Patient 1 was a 17-year-old male. Three weeks prior
to presentation, the patient exhibited a fever of unknown origin
with a peak temperature of 38.5°C. The patient did not exhibit
chest tightness, chest pain or a cough. He was administered
antibiotics and dexamethasone in a local hospital, and his body
temperature returned to normal. The patient was then transferred to
the Shandong Provincial Hospital (Jinan, China) for further
diagnosis and treatment. Peripheral blood count results showed a
hemoglobin level of 77 g/l, a platelet (PLT) count of
14×109/l, and a white blood cell (WBC) count of
46.82×109/l (10.5% segmented neutrophils, 12%
lymphocytes and 77.5% leukemic blast cells). A physical examination
revealed an anemic appearance, no skin or mucosal bleeding, no pain
at the bottom of the sternum, normal heart and lung exams and no
hepatosplenomegaly.
Bone marrow aspirate was stained by Wright-Giemsa
stain (Sigma-Aldrich, St. Louis, MO, USA), and showed a
hypercellular marrow with 77.5% leukemic blast cells.
Hemophagocytosis and vacuolation were observed in the leukemic
cells (Fig. 1). Phagocytosed blood
cells included WBCs, red blood cells and PLTs. Cytochemical
staining of leukemic blast cells included peroxidase, naphthol AS-D
chloroacetate esterase and periodic acid-schiff reaction staining
(all obtained from Zhuhai Baso Biological Technology Co., Ltd.,
Zhuhai, China). Morphology and cytochemical staining of leukemic
cells are shown in Table I. Blasts
were detected using flow cytometry (BD Biosciences, San Jose, CA,
USA) for the antigens shown in Table
II, including cluster of differentiation (CD)117, CD13, CD34,
CD56, CD38, CD33, CD15, myeloperoxidase (MPO) and human leukocyte
antigen-DR (HLA-DR) (all purchased from BD Biosciences). Antigens
CD19, CD10, CD20, CD7, CD11b, CD64, CD3 and CD138 were all negative
(data not shown). Under the French-American-British (FAB)
classification system, patient 1 was AML-M4. Bone marrow cells were
incubated with RPMI 1640 medium (Biosource International, Inc.,
Camarillo, CA, USA) containing 10% heat-inactivated fetal bovine
serum for 24 h and chromosomes were analyzed using the
Wright-Giemsa stain. VideoTesT-Karyo3.1 Chromosome Analysis system
(Video TesT, Petersburg, Russia) was used to analyze the karyogram.
The karyotypes were described according to the International System
for Human Cytogenetic Nomenclature 2009 (3). Patient 1 was
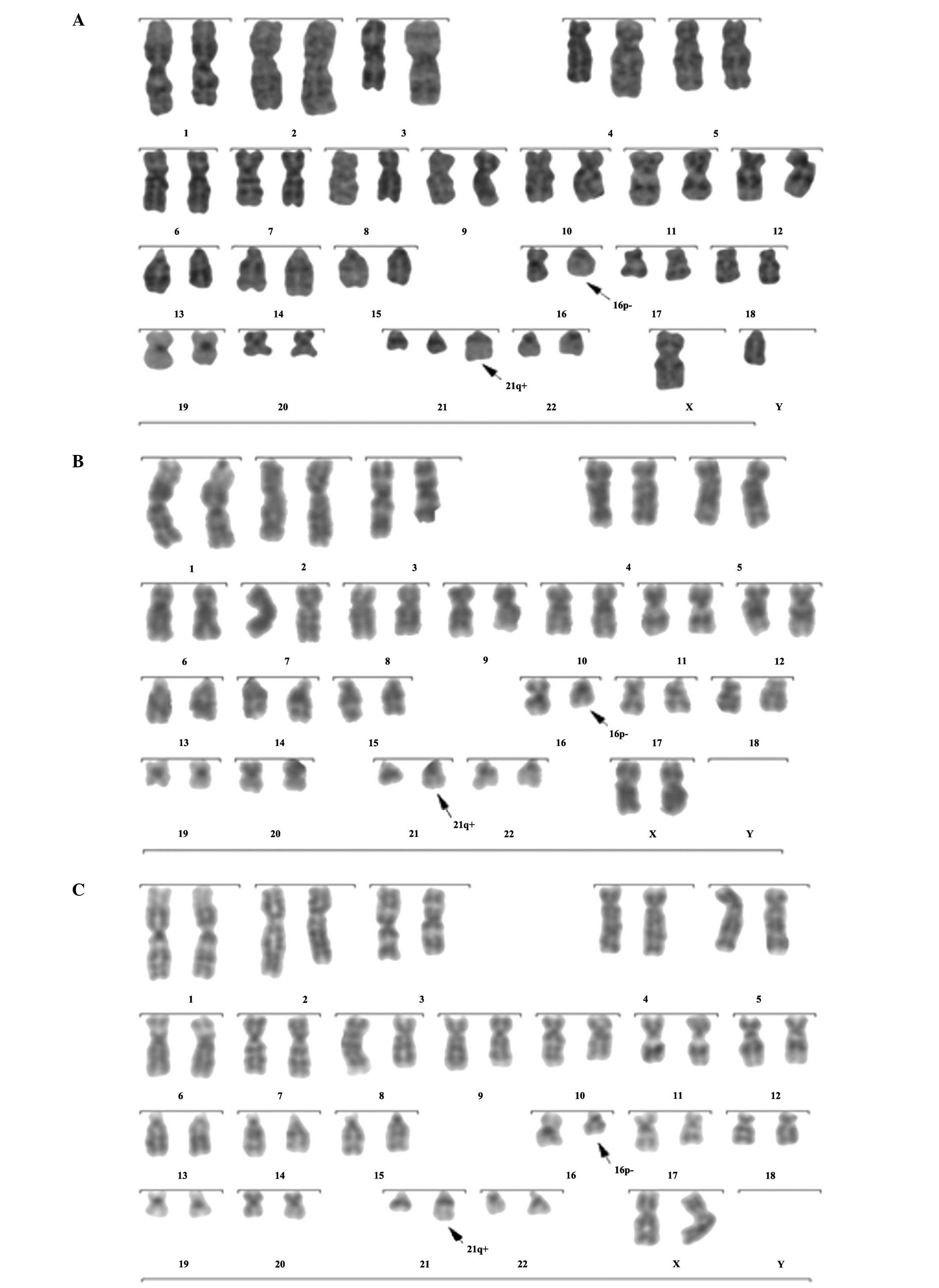
46,XY,t(16;21)(p11;q22)(16)/47,idem,+21(4) (Fig. 2A). Bio-Rad CFX96 fluorescent
quantitative polymerase chain reaction (PCR) system (Bio-Rad
Laboratories, Hercules, CA, USA) and reverse-transcription PCR kit
[Tiangen Biotech (Beijing) Co., Ltd., Beijing, China] were used for
detection. The patient was negative for the following fusion genes:
AML1-Eight-Twenty-One, promyelocytic leukemia-retinoic acid
receptor α (long, short, variant), core binding factor β-myosin
11A, E2A-pre-B-cell leukemia homeobox 1, breakpoint cluster
region-Abelson murine leukemia viral oncogene homolog 1 (P210,
P190), translocation ets-like gene-AML1, SCL interrupting
locus-transcription-activator-like 1, and mixed lineage
leukemia-AF4. The TLS/FUS-ERG fusion gene was positive.
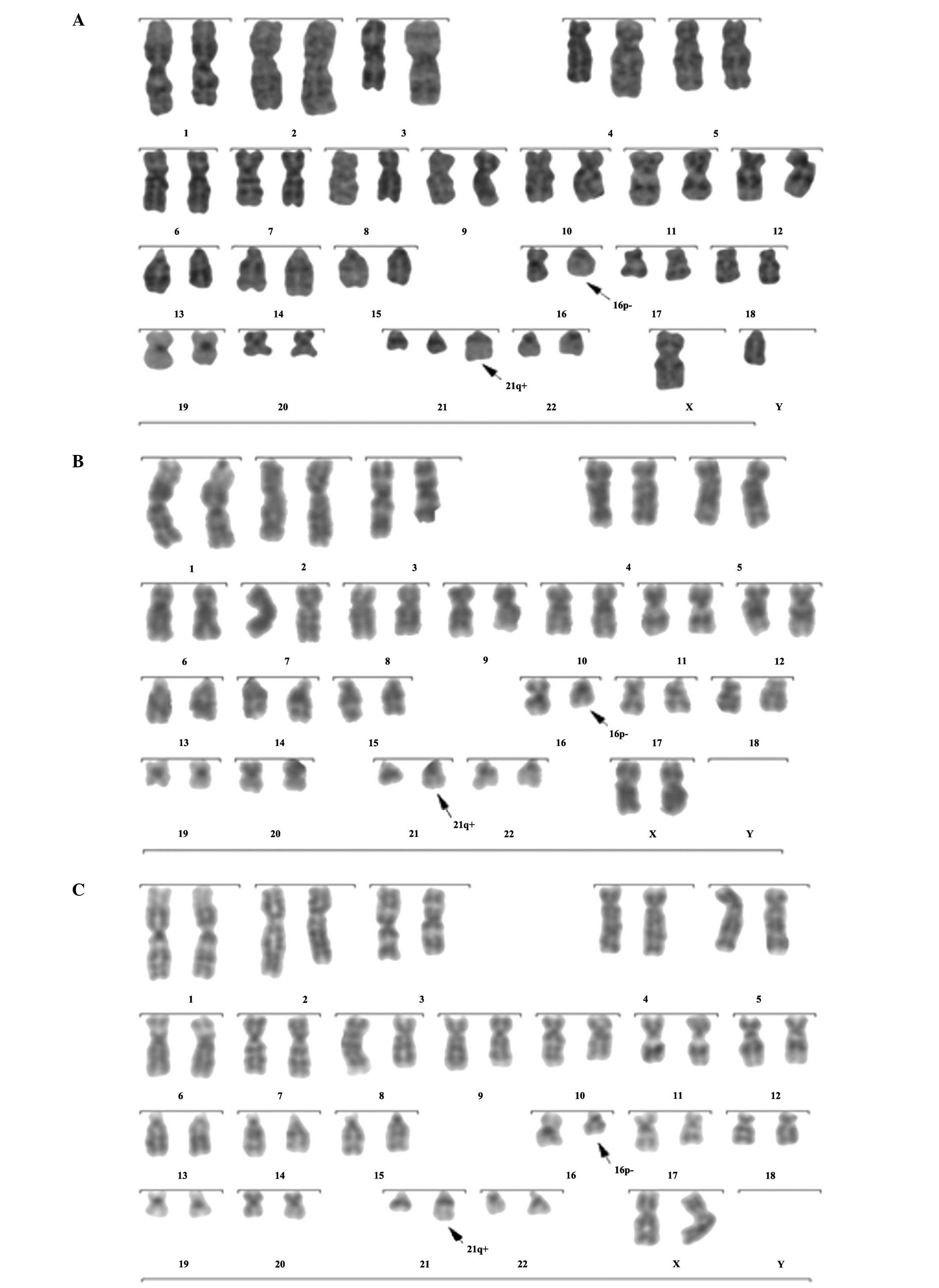 | Figure 2.Karyograms of patients using Giemsa
banding (stain, Wright-Giemsa). (A) Patient 1:
46,XY,t(16;21)(p11;q22)(16)/47,XY,t(16;21)(p11;q22),+21(4). (B)
Patient 2: 46,XX,t(16;21)(p11;q22)(20). (C) Patient 3:
46,XX,t(16;21)(p11;q22)(20). |
 | Table I.Morphology and cytochemical staining
of the leukemic blast cells of the three patients at diagnosis. |
Table I.
Morphology and cytochemical staining
of the leukemic blast cells of the three patients at diagnosis.
| Patient | Bone marrow
hyperplasia degree | Leukemi blast ccells
(%) | Auer rods or
bodies | Cytophagocytosis | POXa | AS-DCEa | PASa |
|---|
| 1 | Active | 77.5 | Not observed | Yes | Positive | Negative | Negative |
| 2 | Active | 93.5 | Not observed | Yes | Positive | Negative | Partial positive |
| 3 | Active | 62.0 | Not observed | Yes | Positive | Negative | Positive |
 | Table II.Percentage of blasts with antigen
positive cells. |
Table II.
Percentage of blasts with antigen
positive cells.
| Patient | CD117 (%) | CD13 (%) | CD34 (%) | CD56 (%) | CD38 (%) | CD33 (%) | CD15 (%) | MPO (%) | HLA-DR (%) |
|---|
| 1 | 85.49 | 65.95 | 89.80 | 79.30 | 26.83 | - | - | 79.69 | 62.91 |
| 2 | 66.68 | 98.67 | 99.50 | 93.41 | 38.45 | 99.65 | 48.58 | - | - |
| 3 | 61.75 | 52.11 | 91.97 | 71.60 | 75.40 | 94.18 | 55.54 | - | 39.50 |
Patient 1 was treated with DA (administration of 40
mg daunorubicin once a day between days 1 and 3 and 150 mg
cytarabine once a day between days 1 and 7) for the first treatment
cycle. The next two treatment cycles were administration of HA (3
mg homoharringtonine once a day between days 1 and 3 and 150 mg
cytarabine once a day between days 1 and 7). The fourth treatment
cycle was administration of 30 mg pirarubicin once a day between
days 1 and 3 and 150 mg cytarabine once a day between days 1 and 7.
The fifth and sixth treatment cycles were HA, subsequent to which
the patient achieved complete remission. The seventh treatment
cycle was administration of 100 mg etoposide VP16 once a day
between days 1 and 5 and 150 mg cytarabine once a day between days
1 and 7. The eighth treatment cycle was medium cytarabine
(administration of 1.0 g twice a day between days 1 and 7). The
ninth treatment cycle occurred following admission to the hospital.
Bone marrow aspirate showed 30.5% leukemic blast cells. The patient
was considered to exhibit a recurrence and was treated with
administration of 10 mg idarubicin hydrochloride once a day between
days 1 and 3 and 150 mg cytarabine once a day between days 1 and
5). The patient received nine courses of chemotherapy and did not
achieve complete molecular and hematological remission. The patient
succumbed after 2 years.
Patient 2
Patient 2 was a 10-year-old female who presented
with a recurrent fever that lasted >2 weeks and leg pain that
lasted 10 days. Two weeks previously, the patient appeared pale and
exhibited a fever and a non-productive cough with no evident cause.
She did not exhibit nausea, vomiting, abdominal pain or diarrhea.
The fever was resolved following drug treatment at a local clinic.
A physical examination revealed an anemic appearance, diffuse
petechiae and no superficial lymph node enlargement. Peripheral
blood count results included a hemoglobin level of 40 g/l, a PLT
count of 6×109/l, and a WBC count of
55.59×109/l [2.5% segmented neutrophils, 4% lymphocytes
and 93.5% leukemic blast cells (shown in the hypercellular bone
marrow aspirate)]. The cytochemical staining and immunological
analysis were consistent with AML. The FAB classification M1 was
established. Morphology and cytochemical staining of leukemic cells
are shown in Table I.
Hemophagocytosis and vacuolation were observed in the leukemic
cells (Fig. 1). Blast antigens are
shown in Table II. The karyotype was
46,XX,t(16;21)(p11;q22)(20) (Fig.
2B). The TLS/FUS-ERG fusion gene was positive and the other
genes were all negative. The patient received nine days of
daunorubicin and etoposide chemotherapy and was in a critical
condition from an infection, resulting in mortality after 1
month.
Patient 3
Patient 3 was a 54-year-old female who had a history
of epilepsy of >20 years and was on scheduled antiepileptic
medications. At 15 days prior to presentation, the patient ceased
the use of the antiepileptic medications due to a sustained severe
headache. The patient then exhibited weakness, and leg ecchymoses
were found. Upon physical examination, the patient was revealed to
have clear mental status, normal development, pallor, ecchymoses in
the two lower limbs and no superficial lymph node enlargement.
Peripheral blood count results included a hemoglobin level of 86
g/l, PLT count of 46×109/l, and WBC count of
2.0×109/l [18% segmented neutrophils, 13% lymphocytes,
7% monocytes and 62% leukemic blast cells (shown in the
hypercellular bone marrow aspirate)]. The cytochemical staining and
immunological analysis were consistent with AML. FAB classification
M2 was established. Morphology and cytochemical staining of
leukemic cells are shown in Table I.
Hemophagocytosis and vacuolation were observed in the leukemic
cells (Fig. 1). Blast antigens are
shown in Table II. The karyotype was
46,XX,t(16;21)(p11;q22) (20) (Fig.
2C). The TLS/FUS-ERG fusion gene was positive and the other
genes were all negative. The patient was treated with DA and
cytarabine plus mitoxantrone, and subsequently received three
courses of chemotherapy, without attaining remission. The patient
survived for two years following the initial diagnosis
Discussion
t(16;21)(p11;q22) is a unique subtype of AML. For
three patients reported previously, the age at diagnosis had a
range of 1–81 years, with a median age of 26 years (1), and had a poor prognosis.
t(16;21)(p11;q22) results in the chimeric transcript TLS/FUS-ERG
(4). This translocation causes the
replacement of the RNA-binding domain of FUS with the DNA-binding
domain of ERG (5,6). This fusion gene is thought to be
responsible for the leukemogenesis of AML harboring t(16;21)
(7). Four transcripts found in AML
with t(16;21) have been designated as types A, B, C and D,
corresponding to the chimeric products of 255, 211, 179 and 349 bp,
respectively. The t(16;21) translocation has been reported in
different types of leukemia (5,7). FAB
classifications M3, M2 and M5 are the most common, and M1 and M4
are the next most common. These classifications included chronic
myeloid leukemia, acute lymphoblastic leukemia and myelodysplastic
syndrome (7–10). This result indicates that
t(16;21)(p11;q22) and the TLS/FUS-ERG chimeric transcript do not
occur exclusively in AML (11).
Of the published karyotypes of AML with the
TLS/FUS-ERG chimeric transcript, some were t(16;21)(pll;q22), while
others had additional abnormities, including +10, +l2, +8, +6, −9,
ins (7;2), del(9)(ql3;q33), +der (21) and del(15)(qll;ql5)
(1). In the present report, the
karyotype of patient 1 had +21 as an additional abnormality. This
combination has not been reported in previous studies. The small
chromosome 21, harboring ∼300 genes, may be involved in numerous
structural aberrations, including translocations, deletions and
amplifications in leukemia and lymphoma. Genes located on
chromosome 21 have been identified to play important roles in
tumorigenesis (12). Trisomy 21 is
the most common cytogenetic abnormality at birth and one of the
most recurrent aneuploidies in leukemia (13). Constitutional +21 of Down's syndrome
is associated with increased risk for childhood leukemia (14). The elevated incidence of acute
megakaryocytic leukemia in young children with +21 is estimated at
∼500-fold (13,15).
Immunophenotyping results have been inconsistent for
AML with t(16;21). Marosi et al (16) found that the leukemic cells expressed
CD7, CD71, CD38, CD15, HLA-DR, CDw65, CD13, CD33 and CD42b
(17); however, Nobbs et al
(17) reported that the leukemic
cells mainly expressed CD34, HLA-DR, CD7, CD13 and CD33, and did
not express CD2, CD10, CD19, CD20, CD14 and terminal
deoxynucleotidyl transferase. Tan et al (18) reported a 54-year-old man whose
leukemic cells mainly expressed CD7, CD13, CD33, CD34, CD117, CD56,
CD64, HLA-DR and cytoplasmic (c)MPO, with positive percentages of
89.9, 53.5, 75.8, 96.7, 99.0, 41.4, 19.9, 98.4 and 97.5%,
respectively, while CD11b, CD14, CD15, CD19, CD3, CD45e and CD79a
were not expressed (19). In the
present three cases, the leukemic blast cells all highly expressed
CD7, CD13, CD34, CD56 and CD38. Additionally, patient 1 expressed
HLA-DR and cMPO; patient 2 expressed CD33 and CD15; and patient 3
expressed CD33, CD15 and HLA-DR. This indicates that the blast
cells of AML with t(16;21) originate from an earlier stage of
myeloid cell differentiation. Granulocytes, mononuclear cells,
megakaryocytes and red blood cells may be involved.
Jekarl et al (2) reported that the average percentage of
CD56 positive blasts in AML with t(16;21) was 45%. Imashuku et
al (9) suggested that the
morphology of bone marrow aspirate of patients with AML and
t(16;21) was unique. Leukemic cells phagocytose WBCs, red blood
cells, PLTs and other leukemic cells. The cytoplasms of leukemic
cells have pseudopodia and one or more, occasionally
alveolate-like, vacuoles. Increased eosinophilia was observed in
the bone marrow or peripheral blood of certain patients, but Auer
rods were uncommon. Hemophagocytosis and vacuolation are closely
associated with the CD56 expression of blast cells (9). In the present cases, hemophagocytosis
and vacuolation of the blast cells were typical, Auer rods were not
observed and eosinophilia was absent. These findings were
consistent with the reports of Imashuku et al (9), but not with that of Wu et al, who
reported that the other five patients in China did not exhibit the
aforementioned characteristics (19).
Therefore, it has been suggested that heterogeneity exists in the
bone marrow aspirate morphology of patients with AML and
t(16;21).
The progression of AML is faster in patients with
t(16;21)(p11;q22) than in patients with other subtypes of AML. With
conventional chemotherapy, complete remission is difficult to
achieve, and the duration of remission is short. Early relapse is
common, and the median survival time is 16 months (7). Therefore, t(16;21)(p11;q22) can be used
as an independent marker for poor prognosis (19). In the present case report, Patient 1
succumbed after 2 years, Patient 2 succumbed after 1 month, and
Patient 3 did not sustain remission despite three courses of
chemotherapy. Therefore, the treatment results were not adequate
compared with conventional chemotherapy regimens, and hematopoietic
stem cell transplantation should be performed (7).
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (no. 81000731) and the
Promotive Research Fund for Excellent Young and Middle-Aged
Scientists of Shandong Province (no. BS2010YY045).
References
|
1
|
Kim J, Park TS, Song J, et al: Detection
of FUS-ERG chimeric transcript in two cases of acute myeloid
leukemia with t(16;21)(p11.2;q22) with unusual characteristics.
Cancer Genet Cytogenet. 194:111–118. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jekarl DW, Kim M, Lim J, et al: CD56
antigen expression and hemophagocytosis of leukemic cells in acute
myeloid leukemia with t(16;21) (p11;q22). Int J Hematol.
92:306–313. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Park TS, Lee ST, Song J, et al: A tandem
triplication, trp (1) (q21q32), in a patient with follicular
lymphoma: a case study and review of the literature. Cancer Genet
Cytogenet. 189:127–131. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ismael O, Shimada A, Elmahdi S, et al:
RUNX1 mutation associated with clonal evolution in relapsed
pediatric acute myeloid leukemia with t(16;21) (p11;q22). Int J
Hematol. 99:169–174. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ichikawa H, Shimizu K, Hayashi Y and Ohki
M: An RNA-binding protein gene, TLS/FUS, is fused to ERG in human
myeloid leukemia with t(16;21) chromosomal translocation. Cancer
Res. 54:2865–2868. 1994.PubMed/NCBI
|
|
6
|
Panagopoulos I, Aman P, Fioretos T, et al:
Fusion of the FUS gene with ERG in acute myeloid leukemia with
t(16;21) (p11;q22). Genes Chromosomes Cancer. 11:256–262. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kong XT, Ida K, Ichikawa H, Shimizu K, et
al: Consistent detection of TLS/FUS-ERG chimeric transcripts in
acute myeloid leukemia with t(16;21) (p11;q22) and identification
of a novel transcript. Blood. 90:1192–1199. 1997.PubMed/NCBI
|
|
8
|
Oh SH, Park TS, Choi JR, et al: Two
childhood cases of acute leukemia with t(16;21) (p11.2;q22): second
case report of infantile acute lymphoblastic leukemia with unusual
type of FUS-ERG chimeric transcript. Cancer Genet Cytogenet.
200:180–183. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Imashuku S, Hibi S, Sako M, et al:
Hemophagocytosis by leukemic blasts in 7 acute myeloid leukemia
cases with t(16;21)(p11;q22): common morphologic characteristics
for this type of leukemia. Cancer. 88:1970–1975. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kawashima N, Shimada A, Taketani T, et al:
Childhood acute myeloid leukemia with bone marrow eosinophilia
caused by t(16;21) (q24;q22). Int J Hematol. 95:577–580. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Huang Z, Chai YH, He HL, Li JQ, Lu J and
Shao XJ: The clinical and laboratory study of TLS-ERG fusion gene
in seven cases of childrens' acute leukemia. Journal of Leukemia
& Lymphoma. 16:352–354. 2007.[(In Chinese)].
|
|
12
|
Fonatsch C: The role of chromosome 21 in
hematology and oncology. Gene's chromosomes cancer. 49:497–508.
2010.
|
|
13
|
Klusmann JH, Creutzig U, Zimmermann M, et
al: Treatment and prognostic impact of transient leukemia in
neonates with down syndrome. Blood. 111:2991–2998. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Izraeli SI, Rainis L, Hertzberg L, Smooha
G and Birger Y: Trisomy of chromosome 21 in leukemogenesis. Blood
Cells Mol Dis. 39:156–159. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Roy A, Roberts I, Norton A and Vyas P:
Acute megakaryoblastic leukaemia (AMKL) and transient
myeloproliferative disorder (TMD) in down syndrome: a multi-step
model of myeloid leukaemogenesis. Br J Haematol. 147:3–12. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Marosi C, Bettelheim P, Geissler K, et al:
Translocation (16;21)(p11;q22) in acute monoblastic leukemia with
erythrophagocytosis. Cancer Genet Cytogenet. 54:61–66. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nobbs MC, Chan-lam D, Howell RT, Kitchen C
and Copplestone JA: Acute nonlymphocytic leukemia with t(16;21).
Cancer Genet Cytogenet. 70:144–145. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tan L, Tan H, Liu WD and Li HM: Clinical
and laboratory investigation of hematological malignancies with
t(16;21)(p11;q22) translocation. Laboratory Medicine and Clinic.
8:2440–2441. 2011.[(In Chinese)].
|
|
19
|
Wu Y, Xue Y, Pan J and Ma Q: Clinical and
experimental studies on five cases of acute myeloid leukemia with
translocation t(16;21)(p11;q22). Zhonghua Yi Xue Yi Chuan Xue Za
Zhi. 20:171–173. 2003.[(In Chinese)]. PubMed/NCBI
|